Abstract
The medial collateral ligament (MCL) is a major stabilizer of the knee joint. It is the most common ligament injured in the knee, particularly in athletes, and has been reported to be torn in 7.9% of all knee injuries.2 The MCL has a complex, layered anatomy with multiple insertions and functions. Minor trauma can cause tearing of the superficial portion whereas higher energy mechanisms can disrupt both the deep and superficial layers. History and physical are often adequate, but the gold standard for diagnosis is MRI. Lesser injuries to the MCL can often be treated conservatively with early rehabilitation, but more significant tears often necessitate surgery. A thorough understanding of the MCL and associated injuries is essential for proper diagnosis and treatment.
Keywords: Knee, Medial collateral ligament, MCL, Anatomy, Pellegrini-stieda, Sports injury, Valgus stress
1. Introduction
The medial collateral ligament is one of four major ligaments that support the knee. The MCL is the prime static stabilizer of the medial side of the knee joint, and is important for providing support against valgus stress, rotational forces, and anterior translational forces on the tibia. A discussion on the topic of knee injuries, specifically MCL injuries, is important because medial collateral ligament injuries are the most common ligamentous injury to the knee, with ligament injuries accounting for up to 40% of all knee injuries.1 It is also likely that many low grade MCL injuries go unreported. In a 10-year observational study in athletes, it was found that MCL tears accounted for 7.9% of all the knee injuries.2 MCL injuries occur commonly in athletes, either through trauma or sudden changes in direction or speed. The valgus stress or rotational forces associated with these events can either strain or tear the ligament, as well as affect other structures of the knee such as the ACL, PCL, and menisci.
2. Anatomy
The medial collateral ligament is part of the capsuloligamentous complex of the medial knee. This region of the knee is divided into three layers: the superficial layer, middle layer, and deep layer. The superficial layer is comprised sartorius and the investing fascia which forms part of the patellar retinaculum. The middle layer includes semimembranosus, the superficial MCL, the medial patellofemoral ligament, and the posterior oblique ligament. The deep layer includes the deep MCL, the posterior medial capsule, and the meniscotibial ligament.3
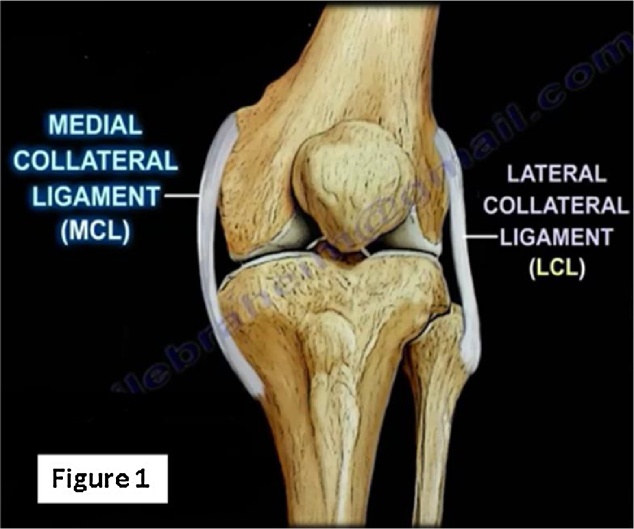
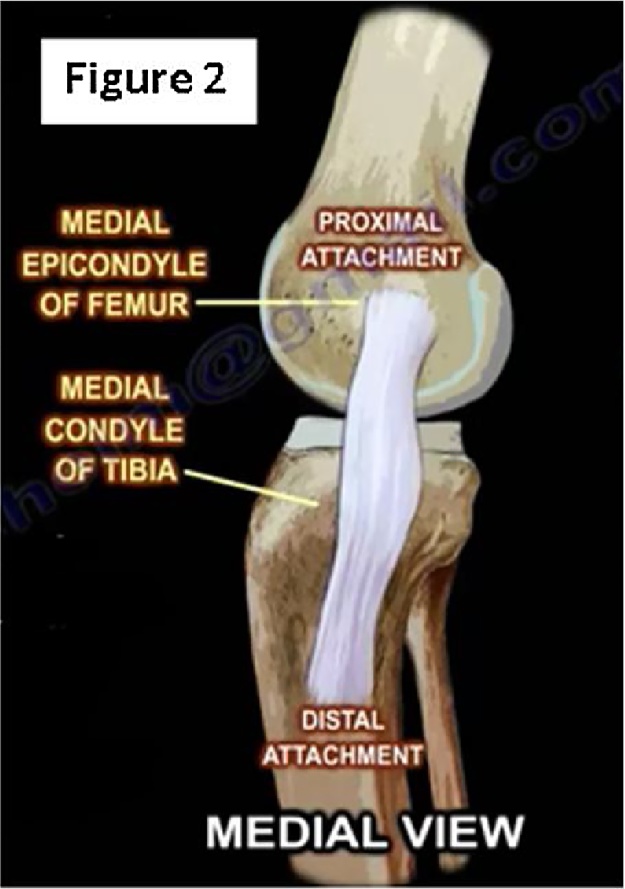
The MCL, an 8 to 10 cm ligament in length, is the largest structure found on the medial aspect of the knee joint (Fig. 1). It is comprised of both a superficial and deep component. The superficial MCL, also known as the tibial collateral ligament, is composed of fibers that originate proximally from the posterior aspect of the medial femoral epicondyle and attach distally to the medial condyle of the tibia 5–7 cm below the joint line near the level of, but posterior to, the pes anserinus insertion (Fig. 2, Fig. 3).3, 4 It is considered the primary static stabilizer to valgus stress of the knee. There is some controversy as to whether the posterior oblique ligament, which is a portion of the semimembranosus that has capsular attachments to the medial knee, is a part of the superficial medial collateral ligament, or if it is a distinct structure. This ligament resides on the posterior aspect of the superficial portion of the MCL and provides additional static and dynamic stabilization for the medial aspect of the knee.5 The deep portion of the MCL, also known as the mid-third capsular ligament, is a major secondary restraint to anterior translation of the tibia, and also provides minor static stabilization against valgus stress. It can be thought of as a thickening of the medial joint capsule, and is divided into meniscofemoral (ligaments of Humphrey and Wrisberg) and meniscotibial (coronary ligament) components.4 The meninscofemoral ligament is longer than the meniscotibial ligament, with its origin being just distal to that of the superficial portion of the MCL, and inserting into the medial meniscus. The shorter and thicker meniscotibial ligament originates from the medial meniscus and attaches to the medial tibial plateau.
Fig. 1.
Anterior view of the left knee with the medial collateral ligament (MCL) and Lateral Collateral ligament (LCL) highlighted to demonstrate their relationship to the osseous structures of the knee.
Fig. 2.
Represents a medial view of the right knee highlighting the proximal and distal attachments of the MCL on the femur and tibia respectively.
Fig. 3.
Medial view of the right knee displaying the muscular attachments of several muscles in relation to the insertion of the distal MCL.
3. Clinical presentation/grades/classification/associated conditions
Injury to the MCL usually presents as an acute trauma with a high number of injuries acquired as a result of trauma during sport. MCL injuries are often the result of a valgus stress applied to a stationary knee, which puts enormous strain on the ligament. The lateral aspect of the knee is usually the most exposed during sport, for this reason, MCL injuries are the most common ligamentous injury of the knee. Minor trauma may result in tearing of the superficial portion (Fig. 5) of the MCL, while more severe injuries can result in complete tears of both the deep and superficial portions (Fig. 4). The patient often describes a sensation of the knee “giving out” at the moment of injury, followed by a rapid filling of the joint with blood, which becomes acutely painful.6 Pain to palpation is usually worse over the course of the MCL and most often near its proximal insertion site. When complete tear is suspected, sedation may be needed to fully examine the injured knee.
Fig. 5.
Similar view representing a distal MCL tear.
Fig. 4.
Medial view of the right knee displaying a proximal tear of the medial collateral ligament (MCL).
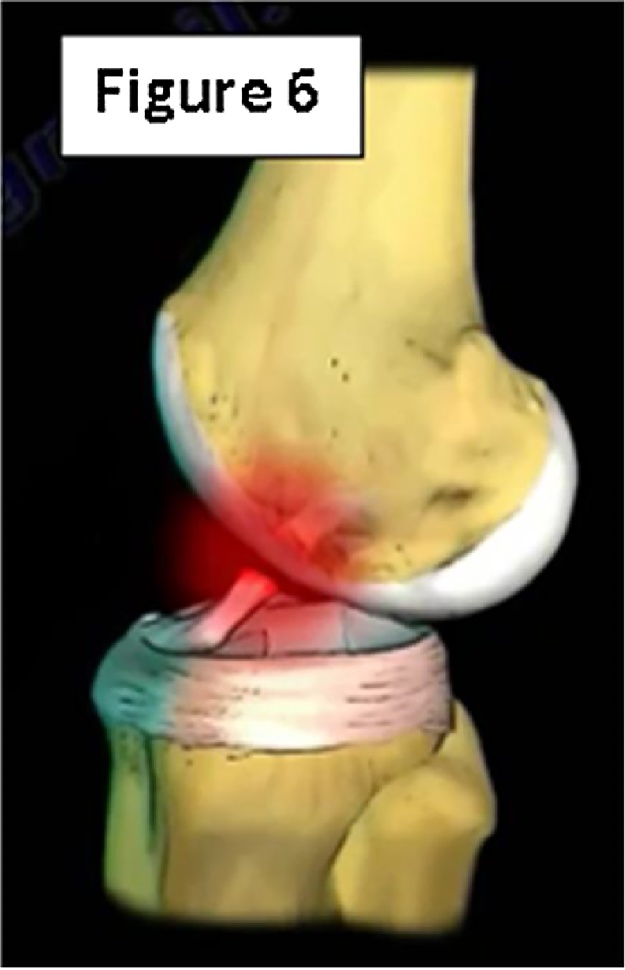
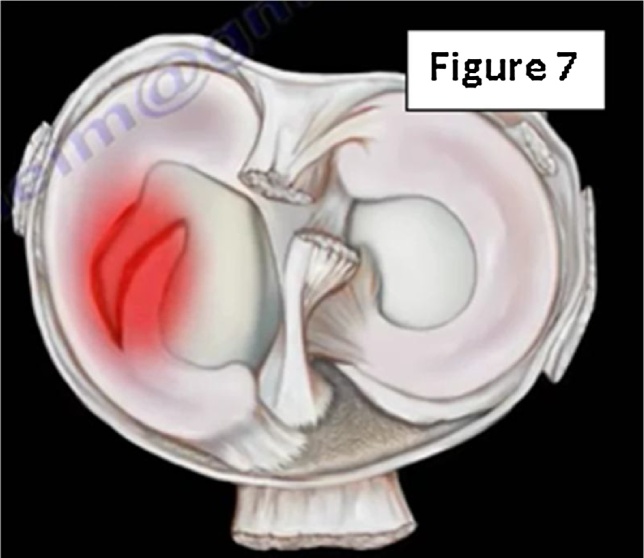
Clinical exam of the knee in patients suspected of having an MCL tear should be done within 20–30 min if possible to avoid complications related to the injury such as pain, swelling, and muscle spasm, using the contralateral leg as a control. In order to isolate the MCL, the knee should be flexed to 30°. This can be accomplished by raising the leg manually, or in larger patients, the thigh can rest on the table while the lower leg hangs over the side of table with the foot and ankle supported. The examiner will then apply a valgus force to the knee and even a small 5–8 mm medial joint opening is indicative of MCL injury.7 In addition to testing the MCL, it is important to test for associated injuries including: ACL, PCL, or medial meniscus (Fig. 6, Fig. 7). Combined injuries to the ACL and MCL are the most common multi-ligament knee injuries in the general population and are usually associated with grade 3 MCL tears.8 Partial or complete tears in the ligament increases the load on the ACL with 30° of flexion, valgus load, or internal rotational torque.9
Fig. 6.
Lateral view of the knee illustrating the increased strain placed on the ACL when the medial collateral ligament (MCL) is torn.
Fig. 7.
Superior view of the knee joint showing a medial meniscus tear, a common injury occurring concurrently with MCL tears.
The extent of MCL injury is graded through clinical history and physical exam. Grade 1 tears involve a few fibers of the MCL with localized tenderness to the medial knee and no instability. Grade 2 tears involve disruption of more fibers, commonly fibers of the superficial MCL with preservation of the deep MCL, more generalized tenderness to palpation, and no instability. A grade 3 MCL tear is a complete tear of the MCL, both deep and superficial portions, with instability of the knee. Grade 3 tears are further classified based on their laxity with respect to valgus stress in 30° of knee flexion. Grade 1+ refers to 3–5 mm of laxity, grade 2+ 5–10 mm of laxity and grade 3+ is defined as >10 mm of laxity to valgus stress.
4. Diagnosis/testing/imaging
The gold standard for diagnosing an MCL injury is diagnostic arthroscopy and surgical exploration, however, this is rarely done. Diagnosis of an MCL injury can reliably be done with clinical history and physical exam. The history will describe a recent trauma in which valgus stress was placed on the lateral knee or a non-contact sensation of the knee “giving away” and “popping” while the patient attempted to change direction rapidly. Positive findings on physical exam will be a medial opening to valgus stress and tenderness to palpation over the medial aspect of the knee. Physical exam findings are a reliable and accurate way of both diagnosing and grading MCL injuries.10 Imaging with MRI is usually reserved for cases of severe trauma or where suspected multi-ligament injury occurred.11 Chronic pain and tenderness over the medial tibiofemoral joint line in a patient with a history of falls or knee trauma may indicate a condition called Pellegrini-Stieda Syndrome (Fig. 8). The pathogenesis of this disease is thought to involve calcification of a posttraumatic hematoma, is diagnosed by a frontal x-ray view of the knee which will show calcification of the medial collateral ligament, and may also show ossifications superiorly on the medial femoral condyle.12
Fig. 8.
AP radiograph of the right knee with superior calcification of the medial collateral ligament (MCL) near the proximal attachment to the medial femoral condyle. This finding is often found in cases of Pellegrini-Stieda Syndrome.
5. Treatment/complications
The mainstay of treatment for grade 1 and grade 2 injuries (Hughston's Classification System) is conservative treatment, with early rehabilitation and ROM exercises with progressive strength training.13 Early joint motion is a central concept of rehabilitation as animal models have found that immobilized joints lead to weaker ligament healing and poorer outcomes.14 Early use of a hinged knee brace can also be used to prevent further valgus injury. Weight bearing is encouraged once pain has subsided and rehabilitation with strengthening of the quadriceps and hamstrings follows. Adjunctive therapy with ultrasound and NSAIDs is often employed to control symptoms and possibly accelerate healing. Prognosis of grade 1 and grade 2 tears is generally favorable with early return to sport/work likely. In one study, high school football players with grade 1 tears returned to sport an average of 10.6 days post-injury and those with grade 2 tears returned an average of 19.5 days post-injury.15
Grade 3 tears are managed similarly to grade 1 and 2 tears if they are injured in isolation to any other ligaments of the knee. Unlike anterior cruciate ligament tears, most MCL tears are either proximal or distal, and have a good blood supply for healing.16 However, most grade 3 MCL injuries are severe, and the risk of an associated ligament injury is 78%, with the anterior cruciate ligament being the associated injury 95% of the time.17 It is recommended that chronic MCL tears are repaired surgically with reconstruction, as non-operative treatment may lead to chronic valgus or rotatory instability with subsequent arthritis.6 Associated injuries such as ACL tears should be repaired after MCL rehabilitation, which may take up to 8 weeks.
Complications with grade 1 MCL injuries are uncommon. In grade 2 or 3 injuries, instability is a common sequela. This can persist and limit participation in athletic activities. Pain is also expected, and rarely can result in complex regional pain syndrome. The most clinically significant complication of an MCL tear is the recurrence of injury. In a group of patients with isolated grade 3 MCL injuries, the recurrence of MCL injury was 23%.18 Scarring and adhesions can be reduced or avoided with early mobilization of the joint.
6. Summary
MCL injuries are the most common ligamentous injuries of the knee. It usually presents as an acute trauma in the athlete involved in sports that require many changes in direction or contact that results in valgus stress to the knee. A good history and physical exam is often enough to diagnose MCL injuries, while imaging can be done when chronic (Pellegrini-Stieda Sydnrome) or multi-ligamentous injuries are suspected. The extent of MCL injury varies greatly as does the treatment. Mild grade 1 or grade 2 MCL tears are treated conservatively with early rehabilitation and generally have a favorable long-term prognosis with return to sport/work in a few weeks. Grade 3 tears are more complicated and often co-exist with other ligamentous injury, such as ACL, PCL or medial meniscus injuries, making surgical treatment sometimes necessary.
Conflict of interest
None.
Contributor Information
Kyle Andrews, Email: kyle.andrews3@utoledo.edu.
Alex Lu, Email: alex.lu2@rockets.utoledo.edu.
Lucas Mckean, Email: lucas.mckean@rockets.utoledo.edu.
Nabil Ebraheim, Email: nabil.ebraheim@utoledo.edu.
References
- 1.Bollen S. Epidemiology of knee injuries: diagnosis and triage. Br J Sports Med. 2000;34(3) doi: 10.1136/bjsm.34.3.227-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Majewski M., Susanne H., Klaus S. Epidemiology of athletic knee injuries: a 10-year study. Knee. 2006;13(3):184–188. doi: 10.1016/j.knee.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 3.Warren L.F., Marshall J.L. The supporting structures and layers on the medial side of the knee. J Bone Joint Surg. 1979;61(1):56–62. [PubMed] [Google Scholar]
- 4.Laprade R.F. The anatomy of the medial part of the knee. J Bone Joint Surg (Am) 2007;89(9):2000. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 5.Lind M., Jakobsen B.W., Lund B., Hansen M.S., Abdallah O., Christiansen S.E. Anatomical reconstruction of the medial collateral ligament and posteromedial corner of the knee in patients with chronic medial collateral ligament instability. Am J Sports Med. 2009;37(6):1116–1122. doi: 10.1177/0363546509332498. [DOI] [PubMed] [Google Scholar]
- 6.Salter R.B. Williams Wilkins; Baltimore: 1999. Textbook of Disorders and Injuries of the Musculoskeletal System: An Introduction to Orthopaedics, Fractures and Joint Injuries, Rheumatology, Metabolic Bone Disease and Rehabilitation. [Google Scholar]
- 7.Chen L., Kim P.D., Ahmad C.S., Levine W.N. Medial collateral ligament injuries of the knee: current treatment concepts. Curr Rev Musculoskelet Med. 2007;1(2):108–113. doi: 10.1007/s12178-007-9016-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyasaka K.C., Daniel D.M., Stone M.L., Hirshman P. The incidence of knee ligament injuries in the general population. Am J Knee Surg. 1991;4:3–8. [Google Scholar]
- 9.Battaglia M.J., Lenhoff M.W., Ehteshami J.R. Medial collateral ligament injuries and subsequent load on the anterior cruciate ligament: a biomechanical evaluation in a cadaveric model. Am J Sports Med. 2009;37(2):305–311. doi: 10.1177/0363546508324969. [DOI] [PubMed] [Google Scholar]
- 10.Rasenberg E.I., Lemmens J.A., van Kampen A. Grading medial collateral ligament injury: comparison of MR imaging and instrumented valgus-varus laxity test-device. A prospective double-blind patient study. Eur J Radiol. 1995;21(1):18–24. doi: 10.1016/0720-048x(95)00660-i. [DOI] [PubMed] [Google Scholar]
- 11.Phisitkul P., James S.L., Wolf B.R., Amendola A. MCL injuries of the knee: current concepts review. Iowa Orthop J. 2006;26:77–90. [PMC free article] [PubMed] [Google Scholar]
- 12.Majjhoo A., Sagar H. Pellegrini-Stieda disease. JCR: J Clin Rheumatol. 2011;17(8):456. doi: 10.1097/RHU.0b013e31820568db. [DOI] [PubMed] [Google Scholar]
- 13.Miyamoto R.G., Bosco J.A., Sherman O.H. Treatment of medial collateral ligament injuries. J Am Acad Orthop Surg. 2009;17(3):152–161. doi: 10.5435/00124635-200903000-00004. [Retrieved April 6 2017] [DOI] [PubMed] [Google Scholar]
- 14.Creighton R.A., Spang J.T., Dahners L.E. Basic science of ligament healing. Sports Med Arthrosc Rev. 2005;13(3):145–150. [Google Scholar]
- 15.Derscheid G.L., Garrick J.G. Medial collateral ligament injuries in football: nonoperative management of grade I and grade II sprains. Am J Sports Med. 1981;9:365–368. doi: 10.1177/036354658100900605. [DOI] [PubMed] [Google Scholar]
- 16.Robins A.J., Newman A.P., Burks R.T. Postoperative return of motion in anterior cruciate ligament and medial collateral ligament injuries. The effect of medial collateral ligament rupture location. Am J Sports Med. 1993;21:20–25. doi: 10.1177/036354659302100104. [DOI] [PubMed] [Google Scholar]
- 17.Fetto J.F., Marshall J.L. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978:206–218. [undefined] [PubMed] [Google Scholar]
- 18.Reider B., Sathy M.R., Talkington J., Blyznak N., Kollias S. Treatment of isolated medial collateral ligament injuries in athletes with early functional rehabilitation. Am J Sports Med. 1994;22(4):470–477. doi: 10.1177/036354659402200406. [DOI] [PubMed] [Google Scholar]
Further reading
M.N. Ebraheim. Medial Collateral Ligament Injuries 2017; [(2017, March 31) Retrieved April 01, 2017, from http://www.huffingtonpost.com/entry/medial-collateral-ligament-injuries_us_58dea7c9e4b03c2b30f6a604].