Abstract
Background
Chronic low back pain (LBP) is a common health problem, with a large potential for primary prevention. Health utilities (HU) reflect which proportion of their expected remaining life time individuals would hypothetically trade to be alleviated of a health condition of interest. A value of 0 means “prefer to die immediately”, a value of 1 means “not willing to trade any life time”. The aim of this cross-sectional study was to assess HU for LBP patients and for healthy participants and to examine whether HU for LBP are useful indicators to substantiate preventive and therapeutic decision making.
Methods
Healthy participants (n = 126) and LBP patients (n = 32) were recruited mainly among the employees of a tertiary care hospital in Germany. Standardized LBP scenarios were presented to all participants and HU values were assessed using the time-trade-off method.
Results
Median HU for LBP were 0.90 (IQR 0.31) for participants and 0.93 (IQR 0.10) for LBP patients. Measurements were consistent across illness severity ratings with HU and with a visual analogue scale (VAS); in the healthy sample the intraclass correlation coefficient (ICC) was 0.61 (95% CI 0.23–1.00, F(1125) = 190, p < .001), in the patient sample the ICC was 0.66 (95% CI = 0.24–1.00, F(1,31) = 62, p < .001). 8% of participants reported HU of 1. There was no statistically significant relation between HU and age, income, or gender.
Conclusion
On average, participants chose a 7 to 10% shorter life expectancy to avoid LBP, but almost 1 in 10 participants were not willing to trade any life years. The results indicate a certain stability of HU due to the comparability of HU ratings across patients and healthy participants, the measurement consistency when comparing VAS and HU ratings, and the lack of association between demographic variables and HU. This underlines the usefulness of HU for measuring illness severity in comparative health economics evaluations of preventive and therapeutic measures that address chronic LBP or other pain-characterized diseases. Future studies should focus on different LBP intensities and derive stratified HU that reflect the distribution of pain intensity in the population.
Keywords: Chronic Low back pain, Health utilities, Health economics, Time-trade-off
Background
Chronic low back pain (LBP) is a common health problem. The global 1-month prevalence of LBP has been estimated to be 23.2 ± 2.9% [1]. Assessing and addressing chronic LBP – commonly defined as LBP of more than 12 weeks duration [2] – is highly relevant not only to general medicine and orthopedics, but also to occupational medicine [3, 4]. Chronic LBP is a leading cause of work absence worldwide which puts a massive economic burden on both the society and individuals [5–7]. It is related to the working conditions in many different job sectors, since it is associated with physically straining work-tasks (e.g. heavy lifting, forward bending, whole-body vibration) and psychosocial work factors (e.g. high demand and low control) [8]. A review of occupational LBP and preventive approaches found that there is high potential for work-related primary prevention of chronic LBP [9]. Decision making concerning occupational prevention measures and treatments for chronic LBP requires health economic evaluations and cost-utility analyses. A systematic review of previous cost utility studies for LBP identified a need for additional studies [10].
Health utilities (HU) are a measure of illness severity that are widely used to facilitate cost-effectiveness analyses and health-related policy making [11]. HU assessed with the time-trade-off method provide a measure of health-related quality of life based on decision-making theory: a value of 0 would mean “prefer to die immediately”, a value of 1 would mean “not willing to trade any life time”. HU scores reflect which proportion of their life time affected patients and non-affected healthy individuals would hypothetically trade to be alleviated of a respective condition [12]. For instance, a score of 0.6 indicates that an individual would choose to live 60% of their (hypothetical) remaining life time in perfect health over living their full remaining life time with the respective condition. HU can be used to assess trade-offs relevant for resource allocation [13] and they allow for a direct comparison of disease outcomes across different health conditions [14]. HU for chronic LBP could provide a tool to conduct cost-utility analyses for treatments and occupational prevention measures and to compare the cost-utility of occupational health promotion targeting chronic LBP to occupational health promotion addressing different diseases such as mental illnesses [15–17].
A previous study assessing patient utilities for LBP found an average utility of 0.93 for mild, 0.65 for moderate, and 0.18 for severe back pain [18]. However, the sample was highly selective; it consisted of 41 LBP patients in a tertiary care hospital. The derived HU are likely to not represent generalizable views on chronic LBP and might thus not be suitable for work-related as well as lifestyle-related primary preventive interventions for healthy individuals. Due to the high potential of occupational preventative approaches targeting healthy individuals, it is important to assess health utility values in this healthy target group. Another previous study examined HU in a healthy sample for chronic pain in general but not chronic LBP specifically [19]. The authors found mean HU of 0.84 for mild, 0.72 for moderate, 0.04 for severe and −0.15 for very severe chronic pain; the negative value indicates that participants would prefer death to suffering these pain. However, the usefulness of HU varies across disease type [20]. While the cited study gives important information on healthy individuals’ ratings of chronic pain and shows that the HU are sensitive to severity of pain, it remains unclear whether these general values are transferable to chronic LBP.
The primary aim of the current study was to assess HU for chronic LBP in a sample of LBP patients and a healthy sample. The secondary aim was to examine whether HU for chronic LBP are useful indicators to substantiate decision making generally and in preventive (e.g. occupational) medicine specifically by assessing: how HU compare to a standard measure of pain severity (VAS-scale) and other severity measures; whether there are many individuals not willing to trade any life years; and whether HU derived with the time-trade-off method are influenced by other variables (age, gender, and own level of pain).
Methods
Participants
The data for this cross-sectional study were collected between October 2011 and August 2015 at the Institute and Policlinic of Occupational and Social Medicine and the Center for Evidence-Based Healthcare, Faculty of Medicine of the TU Dresden. The study population included two groups of participants: 126 healthy participants and 32 patients with chronic LBP. Eligible for inclusion were only participants that: were at least 18 years old; were affiliated with University Hospital and Faculty of Medicine Dresden; and that gave informed consent to participate in the study. Exclusion criteria were: lack of willingness to co-operate and lack of understanding of the study questions. Individuals were eligible for inclusion as patients if an ICD-10 code M54.5 was specified by a careful medical examination and anamnesis and if they reported a LBP duration of more than 3 months, which is in accordance with a widely accepted definition of chronic LBP [2, 9]. Patients with specific lumbar spine diseases (e.g. disc herniation, lumbago with sciatica) were excluded. The healthy participants were working in health-related sectors, to ensure the ability to make informed judgements about LBP. The healthy sample was considered the primary study population to derive HU for healthy individuals as recommended for health economic analyses [17]. The patient group was interviewed to specifically assess the influence of being personally affected by chronic LBP on HU.
The sample was recruited from the employees at the University Hospital and Faculty of Medicine Dresden, and through the social media presence and the intranet of the University Hospital and Faculty of Medicine. The study protocol was approved by the responsible ethics committee of the University Clinic Dresden. This manuscript follows the STROBE Statement for cross-sectional studies [21].
Data collection and measures
Data were collected through a standardized computer-assisted interview. Firstly, participants’ age, sex, and income group were assessed. For employees of the University Hospital no direct information on income was available, their income was thus estimated based on their occupational role. After assessing this demographic information, a standardized scenario for chronic LBP was presented to all participants to assess HU using the time-trade-off method (see Table 1). Participants were given the choice between living for their remaining life expectancy (calculated by the software based on participants’ age and sex) with the described chronic LBP or for a shorter duration in perfect health. The shorter duration in perfect health was a randomly chosen duration based on a normal distribution with mean (± SD) = participant’s remaining life expectancy × 0.8 (±0.05) to avoid a starting point bias [22]. The duration of life in perfect health was then altered until the individual’s preferences were equal. HU were calculated by taking the ratio between the duration of life in perfect health and the duration of life with chronic LBP. Additionally, participants were asked to rate the severity of the standardized LBP scenario on a visual analogue scale (VAS) with 0 reflecting perfect health and 100 reflecting worst imaginable condition. Willingness to pay (WTP) was assessed by asking participants how much they would be willing to pay monthly to not suffer from chronic LBP, and how much they think health insurances should spend monthly so people do not have to suffer from chronic LBP.
Table 1.
Health state scenario
| Unspecified chronic low back pain | |
|---|---|
| Disease Duration | >3 months |
| Affected Regions | Low back, one-or-two sided, can radiated to other body regions |
| Pain Sensations | Pain, sensory disturbances, sometimes numbness and tingling sensations in the legs |
| Causes/Detoriation | Overstraining, lack of exercise, relieving postures, psychosocial factors, being overweight, smoking |
| Treatment | Symptom-oriented: Physical activity (e.g. physiotherapy), possibly analgesics |
| Impact on Life | Occupational impacts, limitations everyday activities and interpersonal relationships |
The patient group suffering from chronic LBP rated their current pain with the time-trade-off method and on a VAS scale; their level of disability was assessed using the Roland Morris disability index [23]. Impairment and productivity were assessed using the Work Productivity and Activity Impairment (WPAI) questionnaire [24]. Furthermore, patients completed the Center for Epidemiological Studies Depression Scale (CES-D) [25] to measure depressive symptoms that may systematically influence HU ratings [26].
We conducted a sample size calculation assuming a standard deviation of 0.1 for the patient sample and of 0.2 for the healthy sample. A sample size of 32 LBP patients and 126 healthy individuals was necessary to obtain 95% confidence intervals with a width of 0.1.
Statistical analysis
Descriptive statistics were calculated for all variables. Arithmetic means with standard deviations, and medians with interquartile range were calculated to derive average disease severity values for HU, VAS and WTP. The key variables were not normally distributed. Thus, robust Spearman correlation analysis and robust regression analysis were applied to assess relations between the disease severity measures and third variables. Measurement consistency between HU and VAS values was tested by calculating two-way random effect intraclass correlation coefficients (ICCs). T-tests were performed to assess group differences. Welsh t-tests were applied when Levene Tests revealed that the variances were not homogenous. All analyses were performed using the open-source software R [27].
Results
Sociodemographic and disease specific characteristics of study participants are shown in Table 2. There were no missing data for any individuals or variables. The mean age of patients with chronic LBP was 41 years (SD = 13), they were thus considerably older than the group of healthy participants (mean age: 30 years, SD = 9). Furthermore, a slightly higher percentage of LBP patients were in the lower income groups compared to the healthy participants (see Table 2). Chronic LBP was a well-known disease in the group of healthy participants (that were mainly health professionals) not suffering from LBP: The vast majority (94%) had a good idea of what chronic LBP is, and 62% had friends or relatives suffering from LBP.
Table 2.
Sociodemographics and disease-specific characteristics of study participants
| Variable | Healthy participants n = 126 | Patients with chronic low back pain n = 32 |
|---|---|---|
| Sex (% female) | 54% | 59% |
| Age in years (mean, SD) | 29.95 (9.25) | 41.03 (12.85) |
| Income group (%) | ||
| <1000 €/month | 10% | 16% |
| 1000–2000 €/month | 2% | 13% |
| 2000–3000 €/month | 56% | 48% |
| 3000–4000 €/month | 30% | 19% |
| >4000 €/month | 2% | 3% |
| Having idea of what low back pain is (%) | 94% | 100% |
| Friends/family members with low back pain (%) | 62% | 66% |
| Family history of LBP (positive, %) | - | 56% |
| Disease duration in years (mean, SD) | - | 15.48 (9.48) |
| Roland Morris disability index | ||
| light (%) | - | 72% |
| moderate (%) | - | 25% |
| severe (%) | - | 3% |
| Degree health affected productivity while working (0 to 1) (WPAI) (mean, SD) | - | 0.18 (0.18) |
| Degree health affected regular activities (0 to 1) (WPAI) (mean, SD) | - | 0.28 (0.24) |
| Depressive Symptoms (CES-D) (mean, SD) |
- | 12.06 (7.52) |
| HU own disease (0 to 1) (mean, SD) | - | 0.93 (0.13) |
| Pain own disease (100 mm VAS) (mean, SD) | - | 22.25 (21.60) |
SD Standard Deviation, WPAI Work Productivity and Activity Impairment Questionnaire, CES-D Center for Epidemiological Studies Depression Scale, VAS Visual Analogue Scale, − not applicable
For the group suffering from chronic LBP, the mean disease duration was 15.48 (SD = 9.48; range 1–40) years. According to the Roland Morris Disability index, the degree of disability was light for 72% (n = 23), moderate for 25% (n = 8), and severe for 3% (n = 1) of the patients. This relatively light impairment for most LBP patients is also reflected in the HU for their current pain assessed with the time-trade-off method (median = 0.96, IQR = 0.06), and in the ratings of current pain on a VAS scale (mean = 22.25, SD = 21.60). The mean VAS of LBP patients with a light degree of disability (according to the Roland Morris Disability index) was 14.78 (median 11.0), the mean VAS of patients with a moderate degree of disability was 39.75 (median 32.5), the only patient with a severe degree of disability had a VAS of 54.
HU values for healthy participants and LBP patients
Median HU for the standardized chronic LBP scenario were 0.90 (IQR = 0.31) as rated by healthy participants and 0.93 (IQR = 0.10) as rated by LBP patients. They were thus comparable between the groups. The mean difference between healthy individuals (M = 0.81, SD = 0.19) and LBP patients (M = 0.88, SD = 0.14) was statistically significant (t(63.64) = −2.48, p = 0.02). However, the less pronounced median difference indicates that the mean difference is related to more extreme ratings in the healthy group (see Table 3 and Fig. 1).
Table 3.
HU and VAS values for standardized chronic low back pain scenario for different groups
| Group | HU | VAS | WTP own money | WTP health insurance | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | Mean (SD) | Median (IQR) | |
| Healthy (n = 126) | 0.81 (0.19) | 0.90 (0.31) | 44.34 (20.84) | 48.00 (34.00) | 236.03 (314.98) | 150.00 (200.00) | 664.93 (945.21) | 300.00 (500.00) |
| Low Back Pain (n = 32) | 0.88 (0.14) | 0.93 (0.10) | 40.91 (19.64) | 47.00 (30.50) | 180.78 (269.78) | 100.00 (150.00) | 785.31 (1234.48) | 300.00 (410.00) |
| Total (n = 156) | 0.83 (0.18) | 0.91 (0.25) | 43.65 (20.59) | 47.00 (33.75) | 224.84 (306.36) | 150.00 (170.00) | 689.94 (1008.83) | 300.00 (528.75) |
HU Health Utilities, VAS 100 mm Visual Analogue Scale Values, WTP Willingness to Pay Monthly in Euros, SD Standard Deviation, IQR Interquartile Range
Fig. 1.
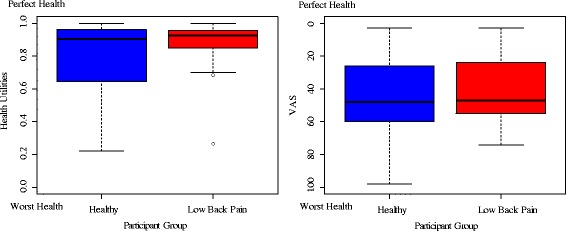
Median and interquartile range of Health Utilities and VAS values by participant group
Relation of HU to VAS and other severity measures
Mean, standard deviation, median and interquartile range for the HU, VAS, and WTP scores for the standardized scenarios are shown in Table 3. There was a good reliability across VAS and HU, the two-way random effects ICC was .61 (95% CI = 0.23–1.00, F(1125) = 190, p < .001) for the healthy sample, and .66 (95% CI = 0.24–1.00, F(1,31) = 62, p < .001) for the patient sample. Correlations between the different measures of rated illness severity are shown in Table 4. HU and VAS are moderately correlated, interestingly, the correlation between HU and VAS is stronger for the group of healthy participants (r = −.53, p < .001) than for the patient group (r = −.31, p = .09). VAS and HU show a stronger correlation and thus seem to be more related constructs than VAS and WTP or HU and WTP.
Table 4.
Spearman correlation coefficients for different measures of illness severity for different groups
| Group | HU ↔ VAS |
HU ↔ Own WTP |
HU ↔ Insurance WTP |
VAS ↔ Own WTP |
VAS ↔ Insurance WTP |
Own WTP ↔ Insurance WTP |
|---|---|---|---|---|---|---|
| Healthy (n = 126) | −.53*** | −.29*** | −.15 | .22* | .20* | .67*** |
| Low Back Pain (n = 32) | −.31+ | −.20 | −.10 | −.11 | −.04 | .73*** |
| Total (n = 156) | −.50*** | −.30*** | −.15+ | .18* | .16* | .68*** |
HU Health Utilities, VAS 100 mm Visual Analogue Scale Values, WTP Willingness to Pay, + = p < .01, * = p < .05, ** = p < .01, *** = p < .001
Individuals not willing to trade any life years
As shown in Fig. 1, ten of the healthy participants (8%), were not willing to hypothetically trade any life years to be relieved of the presented standardized scenario of chronic LBP (and thus received HU of 1). In comparison, no healthy participant rated chronic LBP as equal to perfect health on a VAS scale, and only one healthy participant was not willing to pay any money to be relieved of LBP. Similarly, three of the LBP patients (9%) had HU values of 1, but no LBP patient rated the disease as equal to perfect health on a VAS scale, and no patient was not willing to pay any money to be relieved of LBP.
Demographic factors, own pain, and HU
In the sample, younger people were willing to trade a higher proportion of life years (since they reported lower HU), however, this association was not statistically significant (r(156) = .10, p = .24). VAS and age do not seem to be related in the sample, if anything, younger people rated chronic LBP as less severe (r = .05, p = .55). Males were willing to trade slightly more life years (M male = 0.81, SD male = 0.19, M female = 0.83, SD female = 0.18), but again this difference was not statistically significant (t(156) = −0.67, p = .50). There was no sex difference for VAS (M male = 44.24, SD male = 21.38, M female = 43.16, SD female = 20.02, t(156) = 0.33, p = .74). There was a tendency (albeit not statistically significant) for individuals in the higher income group to report higher HU (r = .12, p = .14), while income group did not influence VAS ratings (r = −.01, p = .92). As shown in Fig. 2, there was a positive relation for chronic LBP patients between HU for their own LBP, and HU for the standardized description of LBP (r = .57, p < .001).
Fig. 2.
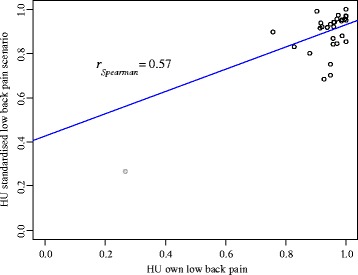
Association between Health Utilities rating of own LBP and Health Utilities rating of standardized LBP scenario
Discussion
This study derived HU values with the time-trade-off method for a sample of patients with chronic LBP and a sample of healthy participants. Median HU for chronic LBP in the healthy sample were 0.90, while median HU in the LBP patient sample were 0.93. HU derived with the time-trade-off method were related to other severity measures and particularly VAS, and there was good measurement consistency when comparing HU and VAS. This indicates that HU for chronic LBP reflect a fairly direct severity rating of LBP and are thus a useful indicator of illness severity. The usefulness of HU is also supported by the lack of statistically significant associations between HU and demographic variables (age, gender, and income). However, almost one in ten participants (in both the healthy and the patient sample) was not willing to trade any life years to be relieved of chronic LBP, while no participant rated chronic LBP as equivalent to being perfectly healthy on a VAS scale.
This observed ceiling effect that exists in HU derived with the time-trade-off method but not in other severity measures has previously been reported for other diseases but not for chronic LBP [20]. On the one hand, this effect impairs the interpretability of HU, as it is not possible to differentiate between ‘perfect health’ and ‘condition not worse enough to trade life years’. It also impairs the direct comparability between HU and other measures of disease severity [20]. On the other hand, the ceiling effect provides useful information for the planning of prevention and intervention measures: It indicates that measures against chronic LBP including the risk of a reduced life expectancy or of other adverse side effects would not be accepted by some individuals since some individuals would not trade any life years to not suffer LBP.
The assessed associations between HU and potential influencing factors (e.g. age or sex) were stronger than the assessed associations between VAS and these factors. While none of these associations were statistically significant, this may have been due to the small sample size, since previous studies did find significant associations: Dolan & Roberts [20] used the time-trade-off method to assess health preferences for different health states (but not LBP) and found that age, sex and marital status influenced the derived values. HU increased up to the age of 45 and then started to fall until the age of 70. Men, and married or cohabiting individuals showed higher HU compared to women and individuals living alone. Additionally, mental health states such as depression have previously been shown to influence HU for cancer patients [26]. It is likely, that mental health states also influence HU for chronic LBP, since depression changes people’s outlooks on life and death (which the extreme case of suicidality illustrates).
Generally, death is a very vague concept and may mean something different to each individual. The perception of life and death possibly largely influences whether an individual would be willing to trade life years and if so how many to be relieved from a disease. A reason for this may be that people with depression place a lower value on life, while it may not reflect perceived severity of the illness. This is related to the finding that there are inconsistencies in HU values that can be attributed to loss aversion, the idea that people are more sensitive to losses than to gains [28]. There is strong evidence showing a higher prevalence of depression among chronic LPB patients [29, 30], it is thus possible that co-morbid depression might also influence HU ratings. These findings pose two difficulties. Firstly, it is difficult to interpret whether differences between population groups result from differing evaluations of the respective health state or of differing evaluations of the value of a life year. For instance, a married or cohabiting person may live a happier life and thus be less likely to trade these happy life years, despite judging the respective health state similarly severe as a person living alone. Secondly, HU being influenced by individual characteristics makes them less informative for cost-effectiveness analyses that concern the general population since it reduces their generalizability.
The HU for chronic LBP found with the time-trade-off method in this study are comparable to the mean HU of 0.93 for mild LBP found in a previous study with a patient sample [18], and they are slightly higher than HU assessed in a healthy sample for general mild chronic pain that were on average 0.84 [19]. This indicates that the LBP scenario used in this study to describe chronic LBP was perceived as a fairly mild type of pain. This is in line with a study comparing the perceived severity of different illnesses, showing that LBP is perceived as comparably moderate [31].
A strength of this study is that HU were assessed for both healthy participants and patients with chronic LBP. Looking at those two different samples is particularly useful for this particular disease: chronic LBP is often addressed in preventive health promotion programs. Because healthy individuals are the target of these programs, it is their rating that is relevant to inform decision makers, while for therapeutic interventions patient ratings are more relevant. Furthermore, this design allows a comparison between these two groups allowing for a judgement on the influence of perspective on HU. There were no drop-outs or missing values for any of the core variables (HU, VAS, WTP, age, gender). The risk of interviewer bias was minimized since all the interviews were conducted by the same well-trained interviewer, and the interviews were computer-assisted to standardize the testing procedure. The concept of chronic LBP was well known to the vast majority of healthy participants, reducing the risk of arbitrary values.
A major limitation to this study is that the sample is not representative of the general population. The average Roland Morris disability index of the current sample was lower (5.34) than that of a population-representative sample of LBP patients in a Greek survey (average Roland Morris disability index 10.01) [32]. This principally impacts the generalizability of the results. However, the mentioned Greek study gives the mean Roland Morris disability index of all individuals that suffered from LBP at the time of the survey, whereas the present sample also includes patients with chronic LBP that are currently free of pain (or almost free of pain). If only looking at individuals in our sample that are currently suffering from LBP (defined as pain levels of at least 20 out of 100 on a VAS scale), the mean Roland Morris disability index of this subsample was 9.09, and is thus comparable to the population-representative Greek study. Moreover, we found similar values for healthy participants and patients, this indicates a certain stability of the derived HU.
Furthermore, the use of a restricted sample of mainly health professionals ensures that healthy participants were informed about chronic LBP. Pain is a hard concept to grasp for someone not suffering from it, since it is invisible and hard to describe. Health professionals are likely to have better insight to this illness since they encounter people suffering from it and are likely to have factual knowledge on chronic LBP and its implications. They are therefore likely to be able to make more informed judgements. The sample size was too small to precisely assess the influence of potential covariates on HU ratings. Future studies should use larger and population-based samples. There was an age difference of 11 years between healthy participants and patients which may have introduced systematic differences to the HU ratings of the two groups. However, this concern is slightly alleviated by the finding that there was no statistically significant association between age and HU ratings.
For health economic evaluations of (primarily) preventable disorders like chronic LBP a reflection of the disease expression in the general population is of particular importance. In the chronic LBP description used in this study, we did not give explicit indications of pain intensity. However, the description seems to reflect moderate pain intensity since the mean VAS as rated by all LBP patients for the standardized chronic LBP scenario was 40.91 which is comparable to the mean VAS of 39.75 that LBP patients with a moderate degree of disability attributed to their own complaints. The advantage of not giving explicit indications of pain intensity is that it reflects how the intensity of chronic LBP varies in the population. The disadvantage of this approach is that it impedes the concrete description of an illness that is primarily pain based. This problem becomes clear when comparing the patient and the population group in our sample: On average, healthy participants rated chronic LBP as more severe than patients with chronic LBP did (note that most chronic LBP patients in our sample reported only light pain intensities). Furthermore, patients with more severe LBP rated the standardized chronic LBP scenario as more severe than patients with less severe LBP (Fig. 2). Consequently, future studies should incorporate explicit descriptions of a range of different pain intensities in their chronic LBP scenarios and derive HU for different levels of pain intensity. HU could then be weighted with respect to the distribution of pain intensities in the general population to derive values that can be used for a health economic evaluation of primary prevention programs. Pain-intensity stratified HU could also be useful for the health economics evaluations of therapeutic treatments, since often chronic LBP cannot be cured completely, but it can be eased. Ideally, these stratified values would be supplemented by HU for a pain reduction from strong to moderate and from moderate to light to optimize the evaluation of curative measures. Overall, deriving HU stratified by pain intensity should be the next step to improve the applicability of HU values to evaluate preventive and pain reduction measures for chronic LBP.
Conclusion
The present study shows that on average chronic LBP patients chose a 7% shorter life expectancy and healthy participants chose a 10% shorter life expectancy to avoid chronic LBP, but almost 1 in 10 participants were not willing to trade any life years. Since LBP is one of the most common diseases in the population and has high preventive potential, these HU can give decision makers in preventive health promotion and health care valuable insight to how patients and healthy individuals perceive chronic LBP. Furthermore, the results indicate a certain stability of HU due to the comparability of HU ratings across patients and healthy participants, the measurement consistency and association between VAS and HU, and the lack of association between demographic variables and HU. The results point towards an applicability of HU for assessing illness severity of LBP specifically and the applicability of HU for diseases that are mainly characterized through pain in general. Future studies looking at pain-characterised diseases should include explicit descriptions of pain intensities in their disease scenarios and independently assess HU for these different pain intensities ideally in a sample that is representative of the population of interest.
Acknowledgments
Not applicable.
Funding
The study was supported by the German Social Accident Insurance Institution for the Health and Welfare Service (BGW). We acknowledge support by the German Research Foundation and the Open Access Publication Funds of the TU Dresden.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CES-D Scale
Center for Epidemiological Studies Depression Scale
- HU
Health Utilities
- ICC
Intraclass Correlation Coefficient
- IQR
Interquartile Range
- LBP
Low Back Pain
- Mfemale
Mean Among Females
- Mmale
Mean Among Males
- r
Correlation Coefficient
- SD
Standard Deviation
- VAS
Visual Analogue Scale
- WPAI Scale
Work Productivity and Activity Impairment Scale
- WTP
Willingness to Pay
Authors’ contributions
ALS analyzed and interpreted the data and drafted the manuscript. CR performed the data elevation. JS participated in the development of the epidemiological concept and in the interpretation of the study results. AN participated in the interpretation of the study results. AS coordinated the study and participated in the development of the epidemiological concept and the drafting of the manuscript. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Ethics approval and consent to participate
The study protocol was approved by the local ethics committee and all study subjects gave written informed consent before study participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, Woolf A, Vos T, Buchbinder R. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 2.Violante FS, Mattioli S, Bonfiglioli R. Low-back pain. Handb Clin Neurol. 2015;131:397–410. doi: 10.1016/B978-0-444-62627-1.00020-2. [DOI] [PubMed] [Google Scholar]
- 3.Hoy D, Brooks P, Blyth F, Buchbinder R. The Epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–781. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Steenstra I, Verbeek J, Heymans M, Bongers P. Prognostic factors for duration of sick leave in patients sick listed with acute low back pain: a systematic review of the literature. Occup Environ Med. 2005;62(12):851–860. doi: 10.1136/oem.2004.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo H-R, Tanaka S, Halperin WE, Cameron LL. Back pain prevalence in US industry and estimates of lost workdays. Am J Public Health. 1999;89(7):1029–1035. doi: 10.2105/AJPH.89.7.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maetzel A, Li L. The economic burden of low back pain: a review of studies published between 1996 and 2001. Best Pract Res Clin Rheumatol. 2002;16(1):23–30. doi: 10.1053/berh.2001.0204. [DOI] [PubMed] [Google Scholar]
- 7.Wynne-Jones G, Cowen J, Jordan JL, Uthman O, Main CJ, Glozier N, van der Windt D. Absence from work and return to work in people with back pain: a systematic review and meta-analysis. Occup Environ Med. 2014;71(6):448–456. doi: 10.1136/oemed-2013-101571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sterud T, Tynes T. Work-related psychosocial and mechanical risk factors for low back pain: a 3-year follow-up study of the general working population in Norway. Occup Environ Med. 2013;70(5):296–302. doi: 10.1136/oemed-2012-101116. [DOI] [PubMed] [Google Scholar]
- 9.Seidler A, Liebers F, Latza U. Prävention von Low-Back-Pain im beruflichen Kontext. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2008;51(3):322–333. doi: 10.1007/s00103-008-0463-3. [DOI] [PubMed] [Google Scholar]
- 10.Dagenais S, Roffey DM, Wai EK, Haldeman S, Caro J. Can cost utility evaluations inform decision making about interventions for low back pain? Spine J. 2009;9(11):944–957. doi: 10.1016/j.spinee.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Longworth L, Yang Y, Young T, Mulhern B, Hernández Alava M, Mukuria C, et al. Use of generic and condition-specific measures of health-related quality of life in NICE decision-making: a systematic review, statistical modelling and survey. Health Technol Assess. 2014;18(9). [DOI] [PMC free article] [PubMed]
- 12.Torrance GW, Feeny D. Utilities and quality-adjusted life years. Int J Technol Assess Health Care. 1989;5(04):559–575. doi: 10.1017/S0266462300008461. [DOI] [PubMed] [Google Scholar]
- 13.Gold M, Siegel J, Russell L, Weinstein M. Cost-effectiveness in health and medicine. New York: Oxford Univ Press; 1996. [Google Scholar]
- 14.Doth AH, Hansson PT, Jensen MP, Taylor RS. The burden of neuropathic pain: a systematic review and meta-analysis of health utilities. Pain®. 2010;149(2):338–344. doi: 10.1016/j.pain.2010.02.034. [DOI] [PubMed] [Google Scholar]
- 15.Seidler A, Thinschmidt M, Deckert S, Then F, Hegewald J, Nieuwenhuijsen K, Riedel-Heller SG. The role of psychosocial working conditions on burnout and its core component emotional exhaustion–a systematic review. J Occupat Med Toxicol. 2014;9(1):10. doi: 10.1186/1745-6673-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. JAMA. 1996;276(14):1172–1177. doi: 10.1001/jama.1996.03540140060028. [DOI] [PubMed] [Google Scholar]
- 17.Drummond MF, Sculpher MJ, Claxton K, Stoddart GL, Torrance GW: Methods for the economic evaluation of health care programmes. Oxford, UK: Oxford University Press; 2015.
- 18.Lai KC, Provenzale JM, Delong D, Mukundan S. Assessing patient utilities for varying degrees of low back pain. Acad Radiol. 2005;12(4):467–474. doi: 10.1016/j.acra.2004.11.031. [DOI] [PubMed] [Google Scholar]
- 19.Eldabe S, Lloyd A, Verdian L, Meguro M, Maclaine G, Dewilde S. Eliciting health state utilities from the general public for severe chronic pain. Eur J Health Econ. 2010;11(3):323–330. doi: 10.1007/s10198-009-0178-x. [DOI] [PubMed] [Google Scholar]
- 20.Robinson A, Dolan P, Williams A. Valuing health status using VAS and TTO: What lies behind the numbers? Soc Sci Med. 1997;45(8):1289–1297. doi: 10.1016/S0277-9536(97)00057-9. [DOI] [PubMed] [Google Scholar]
- 21.Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M, Initiative S. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med. 2007;4(10) doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schmitt J, Meurer M, Klon M, Frick K. Assessment of health state utilities of controlled and uncontrolled psoriasis and atopic eczema: a population-based study. Br J Dermatol. 2008;158(2):351–359. doi: 10.1111/j.1365-2133.2007.08354.x. [DOI] [PubMed] [Google Scholar]
- 23.Roland M, Fairbank J. The Roland–Morris disability questionnaire and the Oswestry disability questionnaire. Spine. 2000;25(24):3115–3124. doi: 10.1097/00007632-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 24.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4(5):353–365. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 25.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 26.Fujisawa D, Inoguchi H. Impact of depression on health utility value in cancer patients. Psycho-Oncology. 2016;25(5):491–495. [DOI] [PubMed]
- 27.R Core Team: R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing. 2017. https://www.R-project.org/.
- 28.Bleichrodt H, Pinto JL, Maria Abellan-Perpiñan J. A consistency test of the time trade-off. J Health Econ. 2003;22(6):1037–1052. doi: 10.1016/S0167-6296(03)00046-8. [DOI] [PubMed] [Google Scholar]
- 29.Pinheiro MB, Ferreira ML, Refshauge K, Maher CG, Ordoñana JR, Andrade TB, Tsathas A, Ferreira PH. Symptoms of depression as a prognostic factor for low back pain: a systematic review. Spine J. 2016;16(1):105–116. doi: 10.1016/j.spinee.2015.10.037. [DOI] [PubMed] [Google Scholar]
- 30.Sagheer MA, Khan MF, Sharif S. Association between chronic low back pain, anxiety and depression in patients at a tertiary care centre. J Pak Med Assoc. 2013;63(6):688–690. [PubMed] [Google Scholar]
- 31.Mo F, Choi BC, Li FC, Merrick J. Using Health Utility Index (HUI) for measuring the impact on health-related quality of life (HRQL) among individuals with chronic diseases. Sci World J. 2004;4:746–757. doi: 10.1100/tsw.2004.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Billis E, Koutsojannis C, Matzaroglou C, Gliatis J, Fousekis K, Gioftsos G, Tsepis E. Association of low back pain on physical, sociodemographic and lifestyle factors across a general population sample within Greece. J Back Musculoskelet Rehab. 2017;30(2):279–290. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


