Abstract
Background
Clinical outcomes after surgical treatment of mitral regurgitation (MR) are worse if intervention occurs after deterioration of left ventricular (LV) size and function. Trans-thoracic echocardiographic (TTE) surveillance of patients with MR is indicated to avoid adverse ventricular remodeling. Overly frequent TTEs can impair patient access and reduce value in care delivery. This balance between timely surveillance and over-utilization of TTE in valvular disease provides a model to study variation in the delivery of health care services. We investigated patient and provider factors contributing to variation in TTE utilization, and hypothesized that variation was attributable to provider practice even after adjustment for patient characteristics.
Methods and Results
We obtained records of all TTEs from 2001–2016 ordered at a large echocardiography laboratory. The outcome variable was time interval between TTEs. We constructed a mixed-effects linear regression model with the individual physician as the random effect in the model, and used intra-class correlation coefficient (ICC) to assess the proportion of outcome variation due to provider practice.
Our study cohort was 55,773 TTEs corresponding to 37,843 intervals ordered by 635 providers. The mean interval between TTEs was 12.4 months, 17.0 months, 18.3 months, and 17.4 months for severe, moderate, mild, and trace MR respectively, with 20% of providers deemed over-utilizers of TTEs, and 25% under-utilizers.
Conclusions
We conclude that there is substantial variation in follow-up intervals for TTE assessment of MR, despite risk-adjustment for patient variables, likely due to provider factors.
Keywords: Mitral Regurgitation, Quality of Care and Outcomes, Variation, Echocardiography
Introduction
Valvular heart disease is a significant burden to the U.S. population, and is likely to increase over the next several decades given an aging population.1 Asymptomatic valvular lesions such as aortic stenosis (AS), aortic insufficiency (AI), and mitral regurgitation (MR) are followed with serial trans-thoracic echocardiograms (TTEs) to monitor severity.2 Visual severity, evidence of deteriorating ventricular function and pulmonary hypertension, and other data acquired with echocardiography, along with clinical evaluation, can identify ventricular decompensation and determine clinical decisions about intervention.2 This surveillance is critical, as the clinical window for intervention can be narrow.3–5 This is especially true of MR, the most common degenerative valve disease, which portends greater mortality and poor cardiovascular outcomes unless repaired before ventricular remodeling.1, 3 Guidelines for those with a normal ejection fraction, recommend TTE surveillance of mild MR every 3–5 years and every 1–2 years for moderate MR.2 If MR is severe, TTE is recommended every 6–12 months, and more frequently if the left ventricle (LV) is enlarging.2 In prior iterations of valvular disease management guidelines, little guidance has been provided for surveillance of mild or moderate MR except to discourage yearly surveillance in asymptomatic patients.6, 7 Recommendations for the surveillance of severe MR have been consistent since 1998.6, 7
However, unnecessarily frequent testing can increase costs without improving quality. Concern over the over-use of TTE led to the development of appropriate use criteria for echocardiography.8 While the majority of TTEs are ordered appropriately, a proportion of TTEs are indeed ordered inappropriately.9, 10 In addition, even when appropriate, many TTEs sometimes do not change clinical decisions.10 Examining these issues is critical since echocardiography is performed at continually increasing rates.11–13
The delivery of a variety of health services has been shown to vary significantly across providers and patients.11, 14–16 Given the balance between timeliness of surveillance and possible over-utilization of TTE in valvular disease, we assessed the association of surveillance frequency for MR with specific provider factors. The variation in performance of all-cause TTEs has been associated with local practice patterns and urban and rural settings, but little is known about specific causes of variation.11, 17, 18 To understand how to improve quality and value in echocardiography for patients with MR, we sought to determine the degree of variation in patient care, and to investigate patient and provider factors contributing to variation in TTE utilization. We hypothesized that there was variation attributable to provider practice even after adjustment for patient characteristics.
Methods
Data Source
The Massachusetts General Hospital (MGH) is the largest hospital in New England. The MGH Echocardiography Laboratory maintains a database of all echocardiograms performed in the main and satellite laboratories, including ordering provider, patient identifiers, and granular clinical data such as MR severity and LV size. This database was linked with hospital billing data for patient demographic characteristics.
Study Population
The study population included all patients over 18 years old who underwent at least two inpatient or outpatient TTEs between 2001 and March 2016. All TTEs are visible to all care providers within the system through a shared electronic health record. TTEs are ordered through the electronic medical system, and results are automatically sent to the ordering provider.
Outcomes and Covariates
The primary outcome was the number of months (“intervals”) between two consecutive studies done on a given patient. For a given patient, TTEs were assessed sequentially. The interval in months was calculated between TTEs, associated with the severity of MR in the initial TTE of each interval, and attributed to the provider who ordered the later study.
Intervals for patients in the echocardiography database not in the billing database were excluded from the analysis, as demographic data could not be linked with the patient. Studies done on patients with an ejection fraction less than 50% were excluded, to eliminate those not represented by the ACC/AHA guidelines.2 We excluded those with dilated left ventricles, any wall motion abnormalities, and those with MR mechanisms of incomplete closure or tethering without mitral valve prolapse to exclude those with secondary MR.19 To exclude studies on patients following valve replacement or repair, we excluded any interval marked by a persistent decrease in severity of valvular disease after moderate or severe disease. The validity of this strategy to exclude patients with interval surgery was confirmed by direct physician chart review of a selection of patients excluded by this algorithm. To exclude intervals during which patients may have been receiving echocardiography outside our hospital, we also excluded any echo intervals greater than 72 months. Consecutive inpatient TTEs and intervals with a single inpatient TTE following an outpatient TTE were also excluded. All ordering providers were identified as a cardiologist, primary care physician (PCP), or other specialist as of the time of the analysis by linkage with an administrative database. Missing data on provider type were adjudicated manually by physicians at the hospital (V.K.T. and J.H.W.). Most physicians are employed faculty physicians and very few (approximately 1%) are in private practice. Five providers for whom a field of practice could not be identified were excluded from the study. Providers who had ordered fewer than 5 tests were excluded from the initial cohort, as these providers were unlikely to be providing longitudinal care. When additional exclusion criteria were applied, additional providers were seen to have ordered fewer than 5 TTEs. TTEs ordered by these providers were aggregated and grouped under a dummy provider.
Demographic variables included age, gender, self-reported race, estimated income, and distance from the echocardiography facility. Race was recorded as white, non-Hispanic black, Hispanic, Asian, and other. Patient age was calculated as the difference between date of birth and the test date. Age was assessed as a categorical variable divided by decade starting at age 45 given a non-linear distribution. Estimated income was used as a continuous variable, and distance from MGH was specified per 10 miles. The most recent zip code was used to estimate distance and income. For missing values of distance, the median distance was used, and for distances greater than 90 miles, 90 miles was used. Income was inferred from zip code by US census data.20 For missing income, we used the median income for the entire sample. Clinical variables included the change in LV end systolic dimension (LVESD) of the two prior TTEs, right ventricular systolic pressure (RVSP), left atrial (LA) size, presence of other valvular disease (moderate or severe aortic stenosis or insufficiency, and severity of MR (trace, mild, moderate, severe). Change in LVESD, RVSP, and LA size were used as continuous variables. In addition, secular trend was measured by number of years starting from 2001 and specified as a continuous variable to account for trends over time. Provider factors were specialization, and experience (estimated by the number of years a provider ordered TTEs).
Statistical Analysis
The length of interval TTE follow up was modeled as a function of patient and provider factors. Frequencies and percentages were used to summarize the distribution of patients by categorical demographics. Means with standard deviations were used to summarize continuous variables. The outcome variable was right-skewed, so a generalized mixed-effects linear regression model with gamma distribution and log link was used.
Patient factors of age, gender, race, estimated income, distance from the echocardiography facility, RVSP, LA size, presence of multiple valvular disease, and change in LVESD were controlled for. Provider specialty and provider experience were the variables of interest. Regression results are reported as rate ratios (RRs) with 95% confidence intervals (CIs).
The contribution of the individual provider on the outcome variable was assessed by shrinkage estimates from a model with only patient factors to assess providers in comparison to the “average” provider. A standard deviation and 95% CI was constructed around the shrinkage estimate for a given provider. If significantly higher than average, the provider was assigned to a group of providers with longer intervals, and if the estimate was significantly lower than average, the provider was assigned to a group of providers with shorter intervals.
An intra-class correlation coefficient (ICC) was calculated to estimate how much of the variation in intervals were due to provider factors. The ICC was compared from two models, one including patient factors and secular trend alone, and another adding provider factors.
All statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, North Carolina). This study was performed for the purposes of quality improvement, so was considered exempt from review by the Institutional Review Board (IRB) at Partners Healthcare per the IRB’s policies. As a retrospective analysis of clinical data, informed consent was not required.
Sensitivity and Supplementary Analyses
To assess the robustness of our results with respect to care outside this health care system, we performed the same analysis in a cohort of patients predicted to receive the majority of their care at MGH. This “loyalty cohort” was determined by a logistic regression model that includes patient age, time since most recent visit, in-state residency, physician practice style, and PCP or primary care practice association. The resulting model has been previously validated with a specificity of 93.7% and positive predictive value of 96.5%.21 Additional sensitivity analyses were performed excluding inpatient TTEs and excluding patients with multiple valve disease. To examine the possibility that other imaging tests such as trans-esophageal echocardiograms (TEEs), magnetic resonance imaging (MRI), stress echocardiography, or invasive catheterization could have replaced some TTEs in following MR, we also conducted a direct physician chart review of a random sample of 100 patients in the analysis to determine how often other tests were ordered to follow MR.
Results
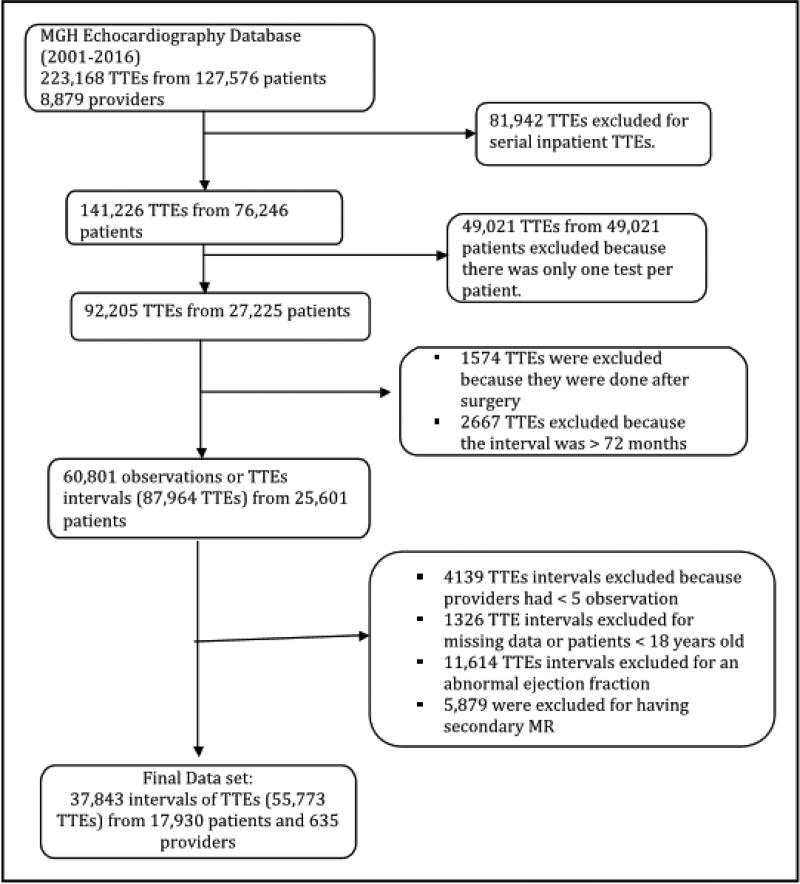
We initially evaluated 127,576 patients with 223,168 TTEs and 8,879 providers. After application of the inclusion and exclusion criteria, 55,773 TTEs remained, resulting in 37,843 intervals in 17,930 patients ordered by 635 providers were in the analytic cohort (Figure 1). Characteristics of the echocardiograms and providers are in Table 1. Trace MR was seen in 23,150 study intervals (61.2%), mild MR in 10,348 (27.3%), moderate MR in 3,678 (9.7%), and severe MR in 667 (1.8%). Seventeen percent of patients were seen to have vegetations, leaflet thickening, mitral valve prolapse, or rheumatic valve disease, as markers of primary MR. Patients with moderate or severe MR were older, but other demographic variables were similar amongst different degrees of MR. The mean interval between TTEs was 12.4 months, 17.0 months, 18.3 months, and 17.4 months for severe, moderate, mild, and trace MR respectively. Most studies done on patients with trace or mild MR were done sooner than would be indicated by the valvular disease (86.7% and 86.2%, respectively). Cardiologists ordered the majority of tests in our study population, and especially in patients with severe MR, ordering 89.5% of those studies, and 80.1%, 69.9%, and 62.4%, in those with moderate, mild, and trace MR respectively.
Figure 1.
Cohort Patients and Study Design. Massachusetts General Hospital (MGH), Trans-Thoracic Echo (TTE), Mitral Regurgitation (MR)
Table 1.
Characteristics of Interval Patient TTEs. (N = number of observations). Guideline recommendations used were 3–5 years for mild and trace MR, 1–2 years for moderate MR, and 6–12 months for severe MR.2
| Variables | All Studies (N=37,843) |
Trace MRa (N=23,150) |
Mild MR (N=10,348) |
Moderate MR (N=3,678) |
Severe MR (N=667) |
|
|---|---|---|---|---|---|---|
| Male (N, %) | 18784 (49.6) | 11799 (51.0) | 4941 (47.8) | 1619 (44.0) | 425 (63.7) | |
| Age Category | ||||||
| < 45 Yrs (N, %) | 6200 (16.4) | 5055 (21.8) | 776 (7.5) | 326 (8.9) | 43 (6.5) | |
| 45 to 54 Yrs (N, %) | 5403 (14.3) | 4052 (17.5) | 1000 (9.7) | 264 (7.2) | 87 (13.0) | |
| 55 to 64 Yrs (N, %) | 7543 (19.9) | 4971 (21.5) | 1826 (17.7) | 605 (16.5) | 141 (21.1) | |
| 65 to 74 Yrs (N, %) | 8795 (23.3) | 5025 (21.7) | 2731 (26.4) | 886 (24.1) | 153 (22.9) | |
| 75 to 84 Yrs (N, %) | 7160 (18.9) | 3151 (13.5) | 2803 (27.1) | 1045 (28.4) | 197 (29.5) | |
| > 84 Yrs (N, %) | 2742 (7.3) | 932 (4.0) | 1212 (11.7) | 552 (15.9) | 46 (6.9) | |
| Race | ||||||
| Black (N, %) | 1409 (3.7) | 929 (4.0) | 325 (3.1) | 128 (3.5) | 27 (4.1) | |
| Hispanic (N, %) | 1515 (4.0) | 1098 (4.7) | 302 (2.9) | 103 (2.8) | 12 (1.8) | |
| White (N, %) | 32724 (86.5) | 19711 (85.1) | 9168 (88.6) | 3263 (88.7) | 582 (87.3) | |
| Asian (N, %) | 1209 (3.2) | 772 (3.3) | 300 (2.9) | 121 (3.3) | 16 (2.4) | |
| Others | 986 (2.6) | 640 (2.8) | 253 (2.4) | 63 (1.7) | 30 (4.5) | |
| Patients with multiple valve diseases (N, %) | 4890 (12.9) | 2577 (11.1) | 1781 (17.2) | 489 (13.3) | 43 (6.5) | |
| Median distance from echo center (IQR) | 12.1(23) | 12.3 (24.3) | 10.5 (20.4) | 10.5 (20.0) | 12.1 (20.6) | |
| Mean estimated income (in $1000) (SD) | 80.1 (29.7) | 79.7 (29.0) | 80.3 (30.8) | 80.8 (30.7) | 83.6 (27.6) | |
| Mean change in LVESDb (SD) | −0.06 (3.5) | −0.12 (3.4) | 0.005 (3.6) | 0.16(3.9) | 0.15 (3.4) | |
| Mean LAc Size (SD) | 37.9 (7.4) | 36.4 (6.6) | 39.5 (7.8) | 42.2 (7.5) | 44.5 (7.4) | |
| RVSPd (SD) | 30.2 (19.1) | 27.0 (18.8) | 34.5 (18.1) | 37.4 (18.6) | 37.2 (21.4) | |
| Provider Specialty | ||||||
| Cardiology (N, %) | 25218 (66.6) | 14437 (62.4) | 7237 (69.9) | 2947 (80.1) | 597 (89.5) | |
| PCPe (N, %) | 4512 (11.9) | 2571 (11.1) | 1462 (14.1) | 441 (12.0) | 38 (5.7) | |
| Other Specialties (N, %) | 8113 (21.4) | 6142 (26.5) | 1649 (15.9) | 290 (7.9) | 32 (4.8) | |
| Mean years of TTEf ordering experience (SD) | 11.65(3.7) | 11.3 (3.7) | 11.6 (3.6) | 11.8 (3.6) | 12.0 (3.7) | |
| Mean interval length (months) (SD) | 17.5 (15.5) | 17.4 (15.9) | 18.3 (15.5) | 17.1 (13.6) | 12.4 (10.5) | |
| Intervals longer than guideline recommendations | 703 (3.0) | 303 (2.9) | 854 (23.2) | 290 (43.5) | ||
| Intervals shorter than guideline recommendations | 20062 (86.7) | 8925 (86.2) | 1508 (41.0) | 152 (22.8) | ||
Mitral Regurgitation (MR),
Left Ventricular End Systolic Dimension (LVESD),
Left Atrial (LA),
Right-Ventricular Systolic Pressure (RVSP),
Primary Care Physician (PCP),
Trans-Thoracic Echocardiogram (TTE)
Association with Patient and Provider Factors
With increased severity of MR, there was a decrease in the interval between TTEs (p < 0.0001). (Table 2) Patient age was associated with longer intervals (Ages 65–74 and 75–84 years old relative to those younger than 45) (RR 1.074; 95% CI 1.014 – 1.139 and RR 1.116; 95% CI 1.041–1.197). Hispanic race was associated with longer intervals between TTEs (RR 1.117; 95% CI 1.000–1.248). Over time, intervals became longer (RR 1.034; 95% CI 1.026–1.042). Distance from the echo facility per 10 miles was significantly associated with TTE intervals (RR 0.986; 95% CI 0.985–0.987; p < 0.0001). Those with multiple valvular diseases had shorter intervals between TTEs (RR 0.833; 95% CI 0.785–0.885).
Table 2.
Association of Patient and Provider Factors with Study Interval
| Predictors | Rate Ratio | Pr > |t| | |||
|---|---|---|---|---|---|
| Mean | [95% CI] | ||||
| MRa Severity Level (relative to trace MR) | |||||
| Mild MR | 0.987 | 0.962 | 1.012 | 0.31 | |
| Moderate MR | 0.892 | 0.851 | 0.936 | <0.0001 | |
| Severe MR | 0.664 | 0.610 | 0.724 | <0.0001 | |
| Male Gender | 0.989 | 0.965 | 1.014 | 0.40 | |
| Age Group (relative to Below 45) | |||||
| 45 to 54Yrs | 0.997 | 0.957 | 1.039 | 0.89 | |
| 55 to 64Yrs | 1.041 | 0.985 | 1.099 | 0.15 | |
| 65 to 74Yrs | 1.074 | 1.014 | 1.139 | 0.0158 | |
| 75 to 84Yrs | 1.116 | 1.041 | 1.197 | 0.002 | |
| > 84Yrs | 1.087 | 0.985 | 1.200 | 0.10 | |
| Race (relative to white patients) | |||||
| Black | 1.042 | 0.983 | 1.105 | 0.17 | |
| Hispanic | 1.117 | 1.000 | 1.248 | 0.049 | |
| Asian | 1.061 | 0.991 | 1.137 | 0.09 | |
| Others | 0.666 | 0.600 | 0.739 | <0.0001 | |
| Distance from Echo Lab (per 10mi) | 0.986 | 0.985 | 0.987 | <0.0001 | |
| Estimated Income (in $1000) | 1.000 | 0.999 | 1.000 | 0.32 | |
| Change in LVESDb | 0.997 | 0.995 | 1.000 | 0.0258 | |
| LAc Size | 0.998 | 0.997 | 1.000 | 0.021 | |
| RVSPd | 0.999 | 0.998 | 0.999 | <0.0001 | |
| Multiple Valve Diseases | 0.833 | 0.785 | 0.885 | <0.0001 | |
| Secular Trend | 1.034 | 1.026 | 1.042 | <0.0001 | |
| Provider Specialty (relative to Cardiologists) | |||||
| Other Specialty | 0.843 | 0.656 | 1.084 | 0.18 | |
| PCPe | 1.492 | 1.396 | 1.596 | <0.0001 | |
| TTEf ordering Experience | 1.012 | 1.001 | 1.023 | 0.0261 | |
Mitral Regurgitation (MR),
Left Ventricular End Systolic Dimension,
Left Atrial (LA),
Right-Ventricular Systolic Pressure (RVSP),
Primary Care Physician (PCP),
Trans-Thoracic Echo (TTE)
Regarding provider factors, relative to cardiologists, TTEs ordered by PCPs were of longer intervals (RR 1.492; 95% CI 1.396–1.596). Non-cardiology specialists trended towards shorter intervals, but did not reach statistical significance (RR 0.843; 95% CI 0.656–1.084). The greater the providers’ experience, the longer the intervals between TTEs (RR 1.012; 95% CI 1.001–1.023). Full results are reported in Table 2.
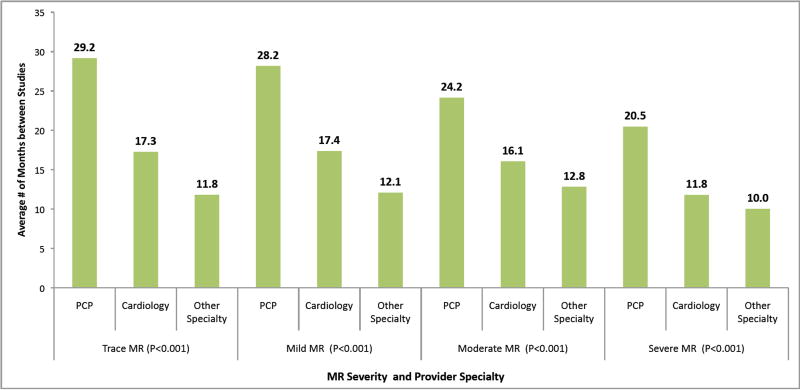
For mild MR, PCPs ordered TTEs every 28.2 months, cardiologists ordered TTEs every 17.4 months, and non-cardiology specialists ordered TTE every 12.1 months (p < 0.001) (Figure 2). For moderate MR, PCPs ordered TTEs every 24.2 months, cardiologists ordered TTEs every 16.1 months, and non-cardiac specialists ordered TTEs every 12.8 months (p <0.001). For severe MR, PCPs ordered TTEs every 20.5 months, whereas cardiologists ordered TTEs at a mean interval of every 11.8 months, and other specialists ordered studies every 10.0 months (p<0.001). For non-cardiac specialists, mean time interval between studies trended less with MR severity (12.1 months for mild, 12.8 months for moderate, and 10.0 months for severe). For both cardiologists and PCPs, MR severity trended with shorter time intervals.
Figure 2.
Average Number of Months between Studies by MR Level and Provider Specialty. Guidelines recommend TTE surveillance of mild MR every 3–5 years and every 1–2 years for moderate MR. If MR is severe, TTE is recommended every 6–12 months, and more frequently if the left ventricle is enlarging. 2
Sensitivity Analyses
A sensitivity analysis replicating the model in our loyalty cohort showed results that were largely consistent with the main findings of the primary analysis. When excluding inpatient studies, the ordering patterns of non-cardiology specialists became significant. They were seen to order studies more frequently (RR 0.781; CI 0.631–0.966). Other results were consistent and supported the main conclusions. Exclusion of those with multiple valve diseases showed results in keeping with the primary analysis. Full results are reported in the Supplementary Appendix.
Supplementary Analyses
A direct physician chart review of a selection of 100 random patients at each severity of MR was conducted to assess the effect of TEEs, stress echocardiograms, cardiac catheterization, and MRIs. We were reassured to see that 1/100 had a stress echocardiogram that may have contributed to surveillance, and 1/100 had a TEE that may have been used in surveillance. No patients received MRIs. Most TEEs and all cardiac catheterizations were performed immediately before operations, and post-op TTEs were excluded from our study.
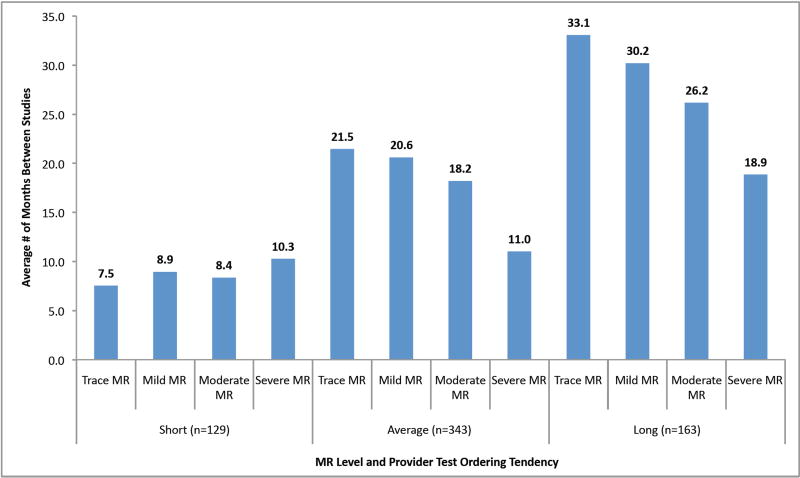
Association Between Individual Provider and TTE Interval
Providers grouped by case-mix adjusted time intervals are shown in Figure 3. High-frequency providers, or those with on average short intervals between TTEs, ordered TTEs at 8.9 month intervals for mild MR and 10.3 month intervals for severe MR, thus independent of MR severity. Average frequency providers ordered TTEs at 20.6 months for mild MR and 11.0 months for severe MR, trending with MR severity. Low frequency providers ordered TTEs for patients with mild MR every 30.2 months but for patients with severe MR every 18.9 months. While mean intervals were all longer, intervals maintained correlation with severity of MR.
Figure 3.
Average Length of Study Interval by MR Severity and Provider Test Ordering Tendency. (n = number of providers) “Short” refers to short-interval providers, or over-utilizers, and “long” refers to long-interval providers, or under-utilizers.
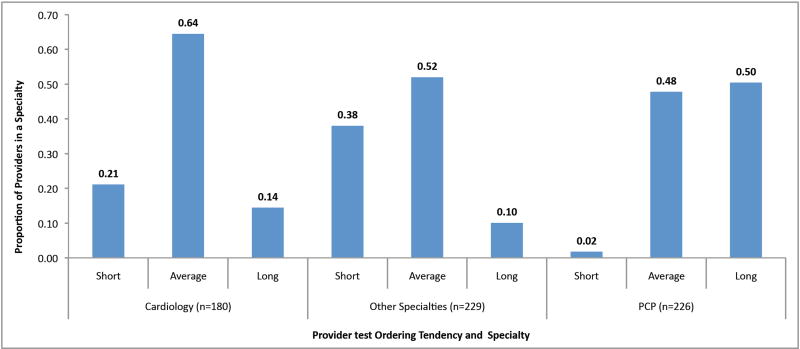
The proportions of high and low frequency providers by specialty are in Figure 4. Among cardiologists, 25.2 out of 180 (14%) had intervals longer than the mean for all providers, and 38 out of 180 (21%) had intervals that were shorter. Among non-cardiac specialists, 87 of 229 (38%) had intervals shorter than the mean and 23 of 229 (10%) had longer intervals. Among PCPs, 5 out of 226 providers (2%) had intervals shorter than the mean and 113 out of 226 providers (50%) had longer intervals.
Figure 4.
Proportion of Providers by Test Ordering Tendency and Specialty. (n = number of providers) “Short” refers to short-interval providers, or over-utilizers, and “long” refers to long-interval providers, or under-utilizers.
The ICC for the unadjusted data was 0.35 (Table 3). When adjusted for patient factors alone, the ICC increased to 0.36. When adjusted for both patient factors and provider specialty and experience, the ICC decreased to 0.27.
Table 3.
Measuring Variation in Study Interval due to Physicians. Patient factors include, age, gender, race, distance from the echo center, and estimated income, LA size, RVSP, and having multiple valve disease. Provider factors include specialty and years of experience ordering TTEs.
| Metric | Unadjusted Model |
Adjusted for Patient Factors |
Adjusted for Patient and Provider Factors* |
|---|---|---|---|
| Variation due to providers (P-value) | 0.0.3417 (<0.0001) | 0.3355 (<0.0001) | 0.2296 (<0.0001) |
| Variation due to Patients (P-value) | 0.6282 (<0.0001) | 0.6078 (<0.0001) | 0.6091 (<0.0001) |
| Intra-class Correlation (ICC) | 0.35 | 0.36 | 0.27 |
Discussion
The surveillance of patients with chronic mitral regurgitation has both the potential for overutilization and underutilization and, as such, is an important case to study variation in the delivery of health care services.3, 9 In this work, we demonstrate substantial variation in the receipt of surveillance TTEs and the association of individual provider practice patterns with interval TTE surveillance of patients with MR. Specifically, cardiologists were seen to order more frequent TTEs in general, whereas PCPs were seen to order TTEs less frequently than indicated, and in both fields specific providers consistently tracked as over- or under-utilizers.
Cardiologists were associated with the majority of the observations (66.6%). Mean imaging intervals for cardiology patients with moderate and severe MR were within guideline recommendations, but trace MR and mild MR were imaged more frequently than recommended.2 Although we cannot determine the indications for all of these studies, it is unlikely that all of the observations ordered by cardiologists in patients with trace or mild MR, can be accounted for by other illnesses requiring TTEs approximately every 18 months. (Figure 2) Within cardiologists, there is also significant variation. Most cardiologists (64%) ordered within the average interval, but 21% of cardiologists fall into the provider group of those ordering TTEs with shorter intervals, and 14% of cardiologists ordered TTEs with longer intervals. (Figure 4) This left-shift of interval distribution and overall higher frequency than PCPs even after adjusting for patient factors is consistent with prior findings that specialists order more diagnostic testing.22 While a greater portion of cardiologists’ tests were ordered for severe MR than the PCPs’ practice panel, this increased frequency when compared to PCPs is maintained after controlling for disease severity.
In comparison to cardiologists, PCPs ordered TTEs at nearly 50% longer intervals for all degrees of MR. (Table 2) Studies for those with trace or mild MR remained outside of guideline recommended windows, but were less frequent than those ordered by cardiology.2 However, patients with severe MR were also imaged less frequently than guideline recommendations.2 (Figure 2) Few PCPs had patients with studies that were done more frequently than the mean provider with only 2% of PCPs falling into the provider group with shorter intervals. Most PCPs (98%) ordered within the average range or at longer intervals. (Figure 4)
In contrast, other specialists, including infectious disease specialists, oncologists, and pulmonologists, ordered TTEs at stable, and overall shorter, intervals despite MR severity. (Figure 2) This suggests that these specialists may not have been ordering studies to assess MR, but rather to answer a different question with an independent time frame. These nearly yearly intervals suggest that these TTEs were spaced around yearly office visits, rather than on clinically guided intervals.
Provider experience was associated with ordering TTEs less frequently. (Table 2) A limitation to assessing provider experience is that we are only capturing ordering practice at MGH during our study period. We are unable to account for experience a provider may have had at another institution or if a provider’s clinical volume changed drastically over time.
Variance related to providers was much more substantial that variance related to patient factors. (Table 3) The association of interval echo imaging with experience and specialty provides guidance to reduce unwanted practice variation. For example, cardiologists can share educational resources with non-cardiology providers. Point of care decision support tools could be used to decrease the ordering of unnecessary TTEs. Additional support for newer physicians may alleviate variation due to experience, and sharing provider behavior in comparison to peers can be used to encourage both over- and under-utilizers to examine ordering behavior.
One notable strength of our study is that by linking demographic data to an echocardiography database, we were able to assess granular information about patient characteristics that possibly influenced time intervals. Although a significant proportion of the observed variation was associated with provider factors, some patient factors were also significant. (Table 2) For example, Hispanic patients had longer imaging intervals than white patients, which warrants further investigation. The source of this variation, whether related to bias in ordering behavior, patient access to TTEs, or other factors, is unclear, but warrants additional investigation as a patient’s care should be consistent between providers. Secular trend noted that intervals elongated slightly over time, which suggests that initiatives to decrease over-use of TTE may be contributing to ordering patterns. Of note, increased distance from the hospital was significantly associated with longer surveillance interval, but the magnitude of that association effect was very small. Since this association was not statistically significant in the loyalty cohort sensitivity analysis, this very small effect may have been related to patients who live far away from the hospital receiving TTEs outside our system.
Our analysis should be interpreted in the setting of important limitations. First, due to the need for granular information regarding severity of valvular disease, the analysis was performed within a single health care center. However, we believe that since the MGH is a large general hospital, our results are likely generalizable to other settings. Second, since we are unable to capture TTEs performed at other hospitals, patients with fragmented care, who travel south during winter, or simply outside cardiologists, may receive echocardiography at different medical centers causing overestimation of time intervals for those patient and provider groups. Nevertheless, we are reassured that a sensitivity analysis performed in a validated “loyalty cohort” supported our main study findings. Third, we did not include a comorbidity index. However, there is no data to reliably suggest how comorbidities would affect the ordering of outpatient TTEs. Specifically, our analysis did not include information about atrial fibrillation, which could have changed ordering patterns. To adjust the conclusions of our analysis, patients with atrial fibrillation would have had to be distributed unequally among physicians with different ordering patterns. In addition, we are unable to assess the addition of medications for treatment of the sequelae MR due to limitations of our data sources. We are reassured that cardiologists, most likely to add these medications, still have frequent testing, suggesting that adding medications may not have had a significant effect on decreasing the frequency of testing. Other imaging, including TEEs, stress echocardiograms, and MRIs, that might have been used for MR surveillance was not part of our database leading to falsely elongated intervals. However, we are reassured by the results of our supportive direct chart review which demonstrated only a trivial number of instances in which another test was used intermittently to follow MR. We are therefore reassured that these other studies did not have a significant effect on our results. Last, it is possible that studies deemed to have been ordered sooner than indicated for valvular assessment were ordered for alternative assessments. However, while these indications, such as device adjustment, other valvular disease, or aortic aneurysms may be over-represented in indications for TTEs ordered by cardiologists, they are unlikely to have a differential effect within each specialty. We are reassured that differences in provider practices persisted in patients with severe MR, who were most likely imaged primarily for their valvular disease. Finally, a sensitivity analysis excluding those with multiple valvular diseases further supported our main findings.
In conclusion, there is substantial variation the frequency of TTE assessment of MR among different physicians even after adjustment for patient factors. Ordering TTEs too frequently may reduce value in echocardiography, and ordering TTEs not often enough may lead to poor patient outcomes because of ventricular remodeling. We believe these findings offer opportunities to improve both quality and value in echocardiography. In our study, provider-related variation is associated with specialization and provider experience, which are fortunately practical targets to minimize unwanted variation in patient care. These results may provide guidance for tactics to improve quality and value in the care of patients with mitral regurgitation, and suggests the need for further investigation into the causes of practice variation.
Supplementary Material
Clinical Perspective.
Clinical outcomes after surgical treatment of mitral regurgitation (MR) are worse if intervention occurs after deterioration of left ventricular (LV) size and function. Trans-thoracic echocardiographic (TTE) surveillance of patients with MR is indicated to avoid adverse ventricular remodeling, but overly frequent TTEs can impair patient access and reduce value in care delivery. To study variation in the delivery of surveillance echocardiography for primary MR, we investigated patient and provider factors contributing to variation in TTE utilization, and hypothesized that variation was attributable to provider practice even after adjustment for patient characteristics.
To do so, we obtained records of all TTEs from 2001–2016 ordered at a large echocardiography laboratory. The outcome variable was time interval between TTEs. We constructed a mixed-effects linear regression model with the individual physician as the random effect in the model, and used intra-class correlation coefficient (ICC) to assess the proportion of outcome variation due to provider practice.
Our study cohort was 55,773 TTEs corresponding to 37,843 intervals ordered by 635 providers. The mean interval between TTEs was 12.4 months, 17.0 months, 18.3 months, and 17.4 months for severe, moderate, mild, and trace MR respectively, with 20% of providers deemed over-utilizers of TTEs, and 25% under-utilizers. Provider factors of specialization and experience were significantly correlated with intervals between TTEs.
We concluded that there is substantial variation in follow-up intervals for TTE assessment of MR, despite risk-adjustment for patient variables, likely due to provider factors.
Acknowledgments
Jason H. Wasfy MD MPhil: Dr. Wasfy was supported by a career development award from the National Institutes of Health through Harvard Catalyst (KL2 TR001100).
Footnotes
Disclosures
Varsha K. Tanguturi MD: None
Michael K. Hidrue PhD: None
Michael H. Picard MD: None
Steven J. Atlas MD MPH: None
Jeffrey B. Weilburg MD: None
Timothy G. Ferris MD MPH: None
Katrina Armstrong MD MPH: Dr. Armstrong was a consultant for Glaxo Smith Kline
References
- 1.Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 2.Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP, 3rd, Guyton RA, O'Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM, 3rd, Thomas JD. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:e521–643. doi: 10.1161/CIR.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 3.Delahaye JP, Gare JP, Viguier E, Delahaye F, De Gevigney G, Milon H. Natural history of severe mitral regurgitation. Eur Heart J. 1991;12(Suppl B):5–9. doi: 10.1093/eurheartj/12.suppl_b.5. [DOI] [PubMed] [Google Scholar]
- 4.Enriquez-Sarano M, Tajik AJ, Schaff HV, Orszulak TA, Bailey KR, Frye RL. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation. Circulation. 1994;90:830–837. doi: 10.1161/01.cir.90.2.830. [DOI] [PubMed] [Google Scholar]
- 5.Ghoreishi M, Evans CF, DeFilippi CR, Hobbs G, Young CA, Griffith BP, Gammie JS. Pulmonary hypertension adversely affects short- and long-term survival after mitral valve operation for mitral regurgitation: implications for timing of surgery. J Thorac Cardiovasc Surg. 2011;142:1439–1452. doi: 10.1016/j.jtcvs.2011.08.030. [DOI] [PubMed] [Google Scholar]
- 6.Bonow RO, Carabello BA, Chatterjee K, de Leon AC, Jr, Faxon DP, Freed MD, Gaasch WH, Lytle BW, Nishimura RA, O'Gara PT, O'Rourke RA, Otto CM, Shah PM, Shanewise JS, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Nishimura R, Page RL, Riegel B. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing Committee to Revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardiovascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2006;48:e1–148. doi: 10.1016/j.jacc.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 7.ACC/AHA guidelines for the management of patients with valvular heart disease. A report of the American College of Cardiology/American Heart Association. Task Force on Practice Guidelines (Committee on Management of Patients with Valvular Heart Disease) J Am Coll Cardiol. 1998;32:1486–1588. doi: 10.1016/s0735-1097(98)00454-9. [DOI] [PubMed] [Google Scholar]
- 8.Douglas PS, Khandheria B, Stainback RF, Weissman NJ, Brindis RG, Patel MR, Alpert JS, Fitzgerald D, Heidenreich P, Martin ET, Messer JV, Miller AB, Picard MH, Raggi P, Reed KD, Rumsfeld JS, Steimle AE, Tonkovic R, Vijayaraghavan K, Yeon SB, Hendel RC, Peterson E, Wolk MJ, Allen JM. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Coll Cardiol. 2007;50:187–204. doi: 10.1016/j.jacc.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Ballo P, Bandini F, Capecchi I, Chiodi L, Ferro G, Fortini A, Giuliani G, Landini G, Laureano R, Milli M, Nenci G, Pizzarelli F, Santoro GM, Vannelli P, Cappelletti C, Zuppiroli A. Application of 2011 American College of Cardiology Foundation/American Society of Echocardiography appropriateness use criteria in hospitalized patients referred for transthoracic echocardiography in a community setting. J Am Soc Echocardiogr. 2012;25:589–598. doi: 10.1016/j.echo.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Matulevicius SA, Rohatgi A, Das SR, Price AL, DeLuna A, Reimold SC. Appropriate use and clinical impact of transthoracic echocardiography. JAMA Intern Med. 2013;173:1600–1607. doi: 10.1001/jamainternmed.2013.8972. [DOI] [PubMed] [Google Scholar]
- 11.Papolos A, Narula J, Bavishi C, Chaudhry FA, Sengupta PP. U.S. Hospital Use of Echocardiography: Insights From the Nationwide Inpatient Sample. J Am Coll Cardiol. 2016;67:502–511. doi: 10.1016/j.jacc.2015.10.090. [DOI] [PubMed] [Google Scholar]
- 12.Pearlman AS, Ryan T, Picard MH, Douglas PS. Evolving trends in the use of echocardiography: a study of Medicare beneficiaries. J Am Coll Cardiol. 2007;49:2283–2291. doi: 10.1016/j.jacc.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 13.Andrus BW, Welch HG. Medicare services provided by cardiologists in the United States: 1999–2008. Circ Cardiovasc Qual Outcomes. 2012;5:31–36. doi: 10.1161/CIRCOUTCOMES.111.961813. [DOI] [PubMed] [Google Scholar]
- 14.Haymart MR, Banerjee M, Yang D, Stewart AK, Sisson JC, Koenig RJ, Doherty GM, Griggs JJ. Variation in the management of thyroid cancer. J Clin Endocrinol Metab. 2013;98:2001–2008. doi: 10.1210/jc.2012-3355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wasfy JH, Hidrue MK, Yeh RW, Armstrong K, Dec GW, Jr, Pomerantsev EV, Fifer MA, Ferris TG. Differences Among Cardiologists in Rates of Positive Coronary Angiograms. J Am Heart Assoc. 2015;4:e002393. doi: 10.1161/JAHA.115.002393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aragam KG, Dai D, Neely ML, Bhatt DL, Roe MT, Rumsfeld JS, Gurm HS. Gaps in referral to cardiac rehabilitation of patients undergoing percutaneous coronary intervention in the United States. J Am Coll Cardiol. 2015;65:2079–2088. doi: 10.1016/j.jacc.2015.02.063. [DOI] [PubMed] [Google Scholar]
- 17.Kini V, McCarthy FH, Rajaei S, Epstein AJ, Heidenreich PA, Groeneveld PW. Variation in use of echocardiography among veterans who use the Veterans Health Administration vs Medicare. Am Heart J. 2015;170:805–811. doi: 10.1016/j.ahj.2015.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lucas FL, Wennberg DE, Malenka DJ. Variation in the use of echocardiography. Eff Clin Pract. 1999;2:71–75. [PubMed] [Google Scholar]
- 19.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39. e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 20.Burstin HR, Lipsitz SR, Brennan TA. Socioeconomic status and risk for substandard medical care. JAMA. 1992;268:2383–2387. [PubMed] [Google Scholar]
- 21.Atlas SJ, Chang Y, Lasko TA, Chueh HC, Grant RW, Barry MJ. Is this "my" patient? Development and validation of a predictive model to link patients to primary care providers. J Gen Intern Med. 2006;21:973–978. doi: 10.1111/j.1525-1497.2006.00509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harrold LR, Field TS, Gurwitz JH. Knowledge, patterns of care, and outcomes of care for generalists and specialists. J Gen Intern Med. 1999;14:499–511. doi: 10.1046/j.1525-1497.1999.08168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seeburger J, Eifert S, Pfannmuller B, Garbade J, Vollroth M, Misfeld M, Borger M, Mohr FW. Gender differences in mitral valve surgery. Thorac Cardiovasc Surg. 2013;61:42–46. doi: 10.1055/s-0032-1331583. [DOI] [PubMed] [Google Scholar]
- 24.Tran A, Ruel M, Chan V. Gender differences in outcomes following cardiac surgery: implications for managing patients with mitral valve disease. Curr Opin Cardiol. 2015;30:151–154. doi: 10.1097/HCO.0000000000000150. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.