Abstract
Refugees frequently experience symptoms of post-traumatic stress and depression, which impede their acculturation in the new host country where they are re-settling. There are few longitudinal studies investigating predictors of mental health and acculturation during the early post-migration period. We conducted a longitudinal study of 298 Iraqi refugees, assessing them upon arrival to the U.S. and 1 year after migration. Pre-migration trauma was associated with increased PTSD and depressive symptoms at baseline, and with acculturation 1 year later. Resilience was associated with depressive symptoms at 1-year follow-up, but not with other resettlement outcomes (PTSD symptoms, English-language skills, or acculturation). PTSD and depressive symptoms at baseline predicted the same symptoms at 1-year follow-up, but not any other re-settlement outcomes. The number of chronic diseases at baseline predicted worse PTSD and depressive symptoms, acculturation, and English language skills at 1-year follow up. Post-migratory exposure to daily stressors and less social support predicted worse 1-year outcomes. Results suggest that interventions that aim to improve mental health and promote acculturation among refugees should assess their history of trauma, chronic disorders, and psychological symptoms soon after migration, and promptly provide opportunities for social support.
Keywords: refugees, mental health, acculturation, structural equation models
Refugees are defined as people who are unable to return to their home countries for fear of serious harm. They constitute about half of the 34 million people forcibly displaced worldwide (Brown & Scribner, 2014; United Nations High Commission on Refugees, 2010). The health of refugees is often compromised by pre-migration conflict, physical and sexual trauma, and social losses (Lindert, Ehrenstein, Priebe, Mielck, & Brahler, 2009; Lipson, 1993; Steel et al., 2009). As might be expected, refugees usually have higher rates of depressive and post-traumatic symptoms than other migrants from their own ethnic groups as well as the populations of the host countries in which they are re-settled (Cummings, Sull, Davis, & Worley, 2011; Lindert et al., 2009; Lipson, 1993; Steel et al., 2009). Psychiatric disability occurs in both tortured and non-tortured refugees, indicating that even in the absence of torture, refugee populations have an elevated risk for impairment (Thapa & Hauff, 2005).
There are several major limitations in our knowledge about the relationship between pre- and post-migration exposures and the problems that refugees experience during the months following migration (i.e., the “post-migration period”). First, investigations since the 1980s have studied asylum seekers and others who have experienced trauma, such as those in post-conflict and other displaced populations. These studies initially explored the relationship between refugees’ demographic characteristics or exposure to trauma and later psychological symptoms. (Beisser & Hou, 2001; Westermeyer, Neider, & Callies, 1989). They usually relied, however, on self-report instruments collected long after the initial exposure; further, most studies used a cross-sectional design and examined refugees who had already resided in their host country for some time (Fazel, Wheeler, & Danesh, 2005; Lindert et al., 2009; Steel et al., 2009). This approach limits one’s ability to discriminate the effects of pre- vs. post-migration stressors on refugees’ health (Rechel, Mladovsky, Ingleby, Mackenbach, & McKee, 2013). The inter-relationship of these factors and how they change over time during the post-migration period is culturally, socially, and psychologically complex, and thus not easily characterized by cross-sectional studies (Bhopal, 2014). For example, post-migratory “daily stressors” may impede acculturation and increase refugees’ risk for developing mental health problems (Carlsson, Mortensen, & Kastrup, 2006). Conversely, social support from refugees’ communities is associated with successful acculturation (Barry, 2005), which may also be promoted by resilience; that is, protective responses after trauma exposure that reduce its impact, promote self-esteem and self-efficacy, and may prevent subsequent adverse psychological distress and disorders (Arnetz et al., 2013; Edward & Warelow, 2005; Hoge, Austin, & Pollack, 2007; Rutter, 1987).
Second, most studies have focused on risk due to pre-migration trauma but have not explored the interplay of other factors that may influence refugees’ health and well-being in the post-migration period. Such factors include not only resilience, but also pre-existing mental health and physical health at the time of migration (Beiser & Hou, 2014; Butow et al., 2013; Sorkin, Tan, Hays, Mangione, & Ngo-Metzger, 2008), as well as the effects of post-migration daily stressors and social support, whether from a refugee’s community of origin or the host community (Berry, Kim, Minde, & Mok, 1987; Huijts, Kleijn, van Emmerik, Noordhof, & Smith, 2012; Morris, Popper, Rodwell, Brodine, & Brouwer, 2009). These effects can be explored using path analysis, particularly with structural equation modeling, which is a statistical approach that allows for this interplay. The few studies that have explored refugee psychological outcomes using this approach have usually depended solely on retrospective or cross-sectional data (Steel, Silove, Bird, McGorry, & Mohan,1999; Beiser & Hou, 2001).
Third, pre-existing chronic disorders present at the time of migration may also impact refugees’ re-settlement outcomes. Early U.S. studies among Hmong refugees found that older refugees with medical problems had persistent psychological symptoms including depression, somatization, phobia, anxiety, hostility and paranoia (Westermeyer et al., 1989). More recent cross-sectional analyses have found a prevalence of non-communicable chronic diseases in up to 50% of refugees, significantly more than among other immigrants from similar backgrounds (Doocy, Sirois, Tileva, Storey, & Burnham, 2012; Yun, Fuentes-Afflick, & Desai, 2012 ;Yun, Hebrank, et al., 2012).
Finally, prior studies investigating outcomes during the post-migration period have often failed to test a specific theoretical model that posits relationships between pre- or post-migration exposures and outcomes (Arnetz, Rofa, Arnetz, Ventimiglia, & Jamil, 2013). Grove and Torbiorn (1985) proposed a longitudinal model that described the effect of refugees’ pre- and post-migratory stressors on their psychological symptoms and behavior during the re-settlement period, positing that refugees progress through a series of four stages: early arrival stability, psychological destabilization, exploration and re-stabilization, and finally return to normal life. Grove and Torbiorn proposed that in the early arrival stage, refugees become cognitively aware of cultural expectations in the host country and of their incapacity to behave appropriately. In the destabilization stage, refugees attempt to make sense out of the new culture; some refugees interact only with others from their culture of origin, some remain hostile to the host culture, and some assimilate uncritically to the host culture. In the re-stabilization stage, refugees progressively explore different cultural learning strategies, gradually adapting to their new culture, until at last the host country feels like an adequate venue for daily life (Grove & Torbiorn, 1985). Gonsalves (1992) appended to Grove and Torbiorn’s model an additional stage, de-compensation, to describe the incapacity of some refugees to acculturate, resulting in a chronic state of being overwhelmed and unable to adapt to the demands of the new host country. This suggests that at some point during re-settlement, divergence may occur between refugees who are adapting well and those who decompensate. Gonsalves postulated that post-migration outcomes were due to refugees’ pre-migration personality traits, the impact of pre-migration trauma and/or post-migration stressors, or some combination of these; however, he did not test this proposal empirically. The model, including Gonsalves’ addition, suggests the need for longitudinal studies elucidating temporal processes in refugee health before and after migration, and how the relationship between pre- and post-migration stressors affects subsequent acculturation and mental health. In the more than two decades since Gonsalves published his work, we are aware of no studies that have explored the proposed associations among refugees in the early post-migration period. In particular, we are unaware of studies exploring the relationship between chronic disease, trauma, and resilience on the persistence of psychological symptoms and the development of acculturation using methods such as path analysis.
To test Grove and Torbiorn’s (1985) model empirically and identify factors that influence refugees’ mental health and acculturation, we conducted a prospective, longitudinal cohort study of Iraqi refugees who were newly arrived in the U.S. These refugees are a representative population that has experienced significant pre-and post-migratory trauma and are at increased risk of anxiety and mood disorders, compared to other refugees (Gorst-Unsworth & Goldenberg, 1998). We measured multiple potential pre- and post-migration factors and outcomes relevant to refugees’ mental health and acculturation, both cross-sectionally at baseline, and prospectively, 1 year later. We tested four hypotheses:
Greater exposure to pre-migratory trauma would be associated with greater PTSD and depressive symptoms and worse acculturation 1 year after re-settlement.
Higher resilience at baseline would be associated with lower PTSD and depressive symptoms and better acculturation at 1-year follow-up.
Higher PTSD and depressive symptoms and a greater number of chronic disorders at baseline would be associated with poorer re-settlement outcomes at 1-year follow-up, i.e. psychological symptoms and acculturation.
Exposure to post-migratory stressors would be the strongest mediator of change in mental health symptoms and acculturation during the first year post-arrival.
Methods
Participants and Procedures
In 2010, a community-based sample of newly-arrived Iraqi refugees was interviewed upon arrival to the U.S. and then again, 1 year later. Refugees resettling in the U.S. must attend orientation meetings during the early post-arrival period. These mandatory meetings are organized by local resettlement agencies and occur every few weeks. To recruit refugees for the study, a contact person at seven local collaborating resettlement agencies notified the research team when orientation meetings with the newly-arrived refugees were held. An Arabic-speaking researcher attended each meeting and described the study to the refugees. During an 11-month recruiting period (October 2010 through August 2011), a total of 501 refugees provided written consent for the researchers to contact them. To achieve our preplanned sample size of 300 refugees, a computer-generated random sampling of those who were interested was selected each week. In total, we contacted 306 refugees and informed them fully about the study; 98% of them (n = 298) chose to participate and provided written consent to the protocol, which was approved by our university Human Investigation Committee.
A trained Arabic-speaking interviewer assessed participants in a location of their choosing (e.g., home, workplace, coffee shop) using instruments described below. Each interview session lasted approximately 2 hours. Baseline interviews for refugees took place immediately following their arrival in the U.S. (M = 1.00 month post-arrival, SD = 1.09). All follow-up interviews took place approximately 1 year after the baseline interview; thus, each participant was interviewed twice (at arrival and 1 year later). Participants received US $35 per phase.
Measures
Participants responded to one survey at baseline and a similar survey 1 year later. To validate our measures culturally and linguistically, all questions that were not already available in Arabic were translated into Arabic by a bilingual psychiatrist and back-translated to English by a separate bilingual Arabic language expert to check for discrepancies with the original measures. Translation discrepancies were resolved during discussions among the research team, which included a co-investigator fluent in Arabic (HJ), until consensus was achieved (Arnetz et al., 2013). Included measures are described below, and we report internal consistencies (alpha) where appropriate.
We examined the following predictors in our model:
Demographics and chronic diseases
At baseline, participants reported their gender, age, religion (Christian or Muslim), marital status, education, number of children, and whether they had been diagnosed by a physician with any of 12 chronic illnesses (high blood pressure, any heart disease, headaches, high cholesterol, sleep apnea or narcolepsy, asthma, diabetes, arthritis or rheumatism, diseases of the muscles or tendons, skin problems, and ear, nose and throat disorders). The total number of chronic diseases was analyzed.
Pre-migration trauma
At baseline, participants were asked about exposure to potentially traumatic events that occurred prior to arrival in the U.S. using the traumatic events section of the Iraqi version of the Harvard Trauma Questionnaire (Shoeb, Weinstein, & Mollica, 2007), which was already validated in Arabic. Participants reported whether or not they were exposed to each of 39 possible traumatic events (e.g., “murder or violent death of family member–child, spouse or friend”). Trauma exposure scores were calculated by summing affirmative responses.
Depressive symptoms
The depression subscale of the Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983) was completed at both baseline and 1-year follow-up. This 7-item measure assesses the symptoms of depression (e.g., “I feel as if I am slowed down”) on a scale from 0 (not at all) to 3 (nearly all the time), and a sum was calculated. Scores less than 8 are considered normal, scores from 8 to 10 indicate mild depression, and scores greater than 10 indicate moderate to severe depression (Breeman, Cotton, Fielding, & Jones, 2015). This scale showed high internal consistency at baseline (α = .93).
PTSD symptoms
The civilian version of the PTSD Checklist (PCL-C) assessed PTSD symptoms at baseline and 1-year follow-up (Adkins, Weathers, McDevitt-Murphy, & Daniels, 2008). This 17-item measure assesses the degree to which individuals are troubled by each of the DSM-IV symptoms of PTSD in the past month (e.g., “Repeated, disturbing memories, thoughts, or images of a stressful experience from the past”) on a scale from 1 (not at all) to 5 (extremely). We assessed total PTSD symptoms by summing up all item responses. The National Center for PTSD suggests a cut-point score between 30 and 35 when used in civilian populations and populations of individuals who are hesitant to disclose such information. Internal consistency was high in this sample (α = .91).
Resilience
The 8-item Resilience Scale (Wagnild & Young, 1993) assessed cognitive and behavioral abilities to cope adaptively with adversity (Lazarus & Folkman, 1984). Participants were asked to rate statements such as “When I’m in a difficult situation, I can usually find my way out of it.” from 1 (strongly agree) to 5 (strongly disagree). The scale exhibited high internal consistency (α = .87), and we created a total score by summing the item ratings; higher scores reflect higher resilience.
We assessed two post-migratory processes as potential mediators at the 1-year follow-up:
Daily stressors
Participant exposure to daily stressors was assessed with a modified version of the Hassles Scale (Kanner, Coyne, Schaefer, & Lazarus, 1981). This 10-item scale assessed the frequency that individuals were exposed to daily stressors (e.g., “problems with transportation”) on a scale from 1 (almost never) to 5 (almost always). The measure had acceptable internal consistency (α = .74), and we created a total score by summing the ratings to the items, with higher scores reflecting more daily stress exposure.
Social support
Social support was assessed with five items from the Interpersonal Support Evaluation Checklist (Cohen & Hoberman, 1983). Items reflect a participant’s interpersonal connection to others (e.g., “When I feel lonely, there are several people I can talk to.”) and were rated from 1 (strongly agree) to 5 (strongly disagree). Items were internally consistent (α = .89), and we created scale scores by summing item responses; higher scores reflect greater social support.
We examined these outcomes:
Acculturation
Participants responded to a modified, 7-item version of the Arab Acculturation Scale (Barry, 2005) at 1-year follow-up only. The scale items measure 2 dimensions of acculturation: separation/assimilation, which included “Most of my friends are from Arab-speaking countries.”, and integration/marginalization, which included “I am equally at ease socializing with Arab-speaking individuals and Americans.”. Items were rated from 1 (strongly agree) to 5 (strongly disagree) Ratings were summed, and higher scores reflect greater adjustment to the host culture.
Language abilities
Participants were asked about their English language skills both at baseline and at follow-up using two items: (1) “How well do you speak English?” and (2) “How well do you write in English?” Item responses ranged from 1 (not at all) to 4 (very well) and were analyzed separately.
PTSD and Depressive symptoms measured at 1-year follow-up were also examined as outcomes.
Data Analyses
Initially, we calculated descriptive statistics for measures at baseline (means and SDs). Data were analyzed using maximum likelihood estimation methods in LISREL 8.80 (Joreskog & Sorbom, 1993). We used structural equation modeling to conduct a path analysis in which error terms for multi-item scales were estimated from the internal consistency measures using the following formula: error = (1−αx)*σx2 (Williams & Hazer, 1986). Any missing data (maximum of seven cases) were deleted in pairwise fashion. All cases were included in the model, and each pathway was simultaneously estimated adjusting for all other variables in the model. The fit of the resulting mediation model was assessed using absolute (chi-square) and incremental fit indices; that is, the root mean square error approximation (RMSEA) and the comparative fit index (CFI). Although non-significant chi-square values indicate superior fit, a significant value was expected in the present study due to a sample size greater than 200 (Bentler & Bonett, 1980; Schumacker & Lomax, 1996). For incremental fit indices, RMSEA values below 0.10 indicate that the model fits well (Browne & Cudeck, 1992), whereas for CFI values, which compare the test model to a null model, a value above 0.90 indicates acceptable fit (Millsap, 2002).
In addition to model fit statistics, direct and indirect pathways were assessed within the model. We examined associations for which prior evidence suggested a predictive association, as described in the Introduction. Significant direct pathways can be interpreted in predictive terms, similar to regression weights. We identified such pathways as negative (an inverse relationship between the predictor and outcome) or positive (a direct relationship between predictor and outcome). The significance of indirect pathways was examined using the product of coefficients test (Sobel, 1987; Preacher & Leonardelli, 2001). A significant indirect pathway between a predictor and outcome variable indicated that the association between these variables did not exist independently of another variable, known as a mediator. A significant indirect association in the absence of a significant direct association indicated that the association between the predictor and outcome was fully mediated by this other variable, suggesting that the relationship between the predictor and the outcome was fully driven by the mediator. Significance for all analyses was set at a 2-tailed alpha of .05.
Results
At baseline, 298 refugees provided data, and fully 291 of these refugees (98%) provided 1-year follow-up data. Table 1 shows baseline descriptive statistics. Below, we address each of our four study hypotheses. Figure 1 and Tables 2, 3, and 4 show additional results described below, including the path analyses. Results reported below are statistically significant unless otherwise noted. For complete results, please refer to the tables and Figure 1.
Table 1.
Descriptive Statistics for Model Variables
| Characteristic | Baseline
|
Follow-up
|
|---|---|---|
| (n = 298) M (SD) |
(n = 291) M (SD) |
|
| Age (years) | 33.4 (11.3) | 34.3 (11.4) |
| Trauma | 12.5 (3.5) | — |
| Depression symptoms | 1.9 (3.5) | 3.4 (4.3) |
| PTSD symptoms | 19.2 (5.3) | 19.6 (5.8) |
| Social support | 19.7 (2.2) | 19.1 (2.6) |
| Perceived hassles | 20.8 (2.6) | 16.8 (3.3) |
| Acculturation | 16.8 (2.1) | 17.5 (3.0) |
| Resilience | 30.9 (3.3) | 30.6 (3.3) |
| Co-morbid diseases* | 0.9 (1.4) | 1.1 (1.6) |
| English speaking skills | 1.9 (0.6) | 2.1 (0.6) |
| English writing skills | 2.0 (0.6) | 2.0 (0.6) |
Total number of the following: high blood pressure, any heart disease, headaches, high cholesterol, sleep apnea or narcolepsy, asthma, diabetes, arthritis or rheumatism, diseases of the muscles or tendons, skin problems, and ear, nose and throat disorders
Figure 1.
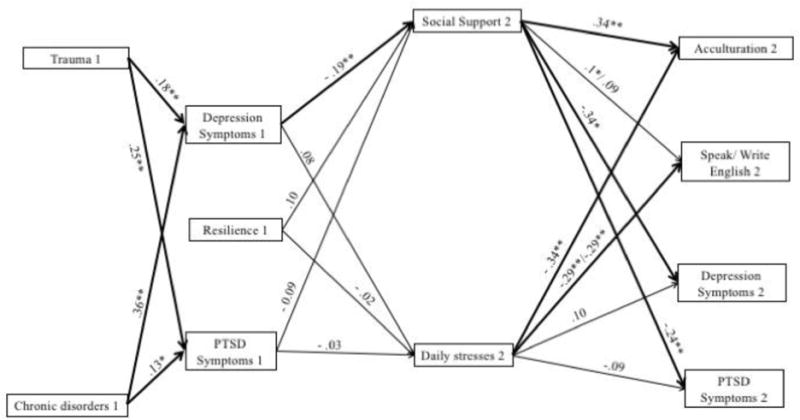
Path Analysis The model fit the data well (RMSEA = .077; 95% CI = 0.06–0.09; CFI = .96; Chi-Square = 242.53, p<.001). Not all pathways are shown in the model. Additional pathways are reported in Tables 2 and 3. Path beta-coefficients indicate negative (−) and positive associations. Time in study measure was collected: 1=baseline, 2= 1-year follow-up *=P<0.05, **=P<0.01.
Table 2.
Standardized Direct and Indirect Effect Pathways
| Outcomes at 1-year Follow-up | |||||||
|---|---|---|---|---|---|---|---|
| Social Support | Daily Stressors | Acculturation | Speak English | Write English | Depression | PTSD | |
| Direct Predictors | |||||||
| Trauma | 0.15* | −0.05 | 0.14** | — | — | −0.04 | 0.05 |
| Resilience | 0.1 | −0.02 | 0.06 | 0.1 | 0.1 | −0.1* | 0.01 |
| Depression (baseline) | −0.19** | 0.08 | −0.17** | — | — | 0.23** | −0.03 |
| PTSD (baseline) | −0.09 | −0.03 | −0.04 | — | — | 0.04 | 0.37** |
| Chronic diseases | — | 0.26** | −0.02 | — | — | 0.31** | 0.16** |
| Male gender | — | 0.06 | 0.15** | 0.07 | 0.05 | −0.07 | −0.05 |
| Education | −0.24** | 0.01* | 0.13* | 0.15** | 0.04 | 0.02* | |
| Age | 0.06 | −0.15 | −0.16 | −0.16 | 0.13 | 0.10 | |
| Married | 0.26** | 0.11 | −0.06 | −0.08 | −0.02 | 0.004 | |
| Indirect Predictors | |||||||
| Trauma | 0.007 | 0.02 | 0.01 | 0.01 | 0.07* | ||
| Resilience | 0.04 | 0.01 | 0.01 | −0.04 | −0.02 | ||
| Chronic diseases | −0.19** | −0.09** | −0.09** | 0.15** | 0.03 | ||
| Depression (baseline) | −0.09** | −0.04 | −0.04 | 0.07** | 0.04 | ||
| PTSD (baseline) | −0.02 | −0.004 | 0.01 | 0.02 | 0.02 | ||
= p< .05,
p<.01. Dashes indicate pathways that were not estimated.
Table 3.
Estimated Significant Correlations between Model Variables
| Depression (Baseline) | Acculturation | Depression (1-year) | Speak English (1-year) | |
|---|---|---|---|---|
| PTSD (baseline) | 0.84** | |||
| Depression (baseline) | −0.11** | |||
| PTSD (1-year) | 0.26** | |||
| Speak (1-year) | 0.20** | |||
| Write (1-year) | 0.20** | 0.57** |
= p< .05,
p<.01
Table 4.
Specific Indirect Effects for Significant Total Indirect Effect Pathways
| Predictor | Mediator | Outcome | SIE | Sobel Test | p |
|---|---|---|---|---|---|
| Trauma | Depression 1 | Social Support 2 | −0.024 | −2.10 | .036 |
| PTSD 1 | −0.015 | −1.21 | .23 | ||
| Depression 1 | Daily Stresses 2 | 0.013 | 1.11 | .27 | |
| PTSD 1 | −0.006 | −0.43 | .67 | ||
| Depression 1 | Social Support 2 | PTSD 2 | 0.08 | 2.36 | .018 |
| Daily Stresses 2 | −0.013 | −0.90 | .37 | ||
| PTSD 1 | Social Support 2 | PTSD 2 | 0.025 | 1.21 | .23 |
| Daily Stresses 2 | 0.003 | 0.41 | .68 | ||
|
| |||||
| Diseases | Depression 1 | Social Support 2 | −0.12 | −2.55 | .011 |
| PTSD 1 | 0.02 | −1.10 | .27 | ||
| Depression 1 | Daily Stresses 2 | 0.06 | 1.16 | .25 | |
| PTSD 1 | −0.01 | −0.42 | .67 | ||
| Depression 1 | Social Support 2 | Acculturation | −0.05 | −2.55 | .011 |
| Daily Stresses 2 | −0.02 | −1.15 | .25 | ||
| PTSD 1 | Social Support 2 | Acculturation | −0.02 | −1.23 | .22 |
| Daily Stresses 2 | 0.005 | 0.43 | .67 | ||
|
| |||||
| Diseases | Depression 1 | Social Support 2 | −0.12 | −2.55 | .011 |
| PTSD 1 | 0.02 | −1.10 | .27 | ||
| Depression 1 | Daily Stresses 2 | 0.06 | 1.16 | .25 | |
| PTSD 1 | −0.008 | −0.42 | .67 | ||
| Depression 1 | Social Support 2 | Speak English | −0.003 | −1.60 | .11 |
| Daily Stresses 2 | −0.004 | −1.15 | .25 | ||
| PTSD 1 | Social Support 2 | Speak English | −0.001 | −1.06 | .29 |
| Daily Stresses 2 | 0.001 | 0.43 | .67 | ||
|
| |||||
| Diseases | Depression 1 | Social Support 2 | −0.12 | −2.55 | .011 |
| PTSD 1 | 0.02 | −1.10 | .27 | ||
| Depression 1 | Daily Stresses 2 | 0.06 | 1.16 | .25 | |
| PTSD 1 | −0.008 | −0.42 | .67 | ||
| Depression 1 | Social Support 2 | Write English | −0.003 | −1.50 | .13 |
| Daily Stresses 2 | −0.004 | −1.15 | .25 | ||
| PTSD 1 | Social Support 2 | Write English | −0.001 | −1.03 | .31 |
| Daily Stresses 2 | 0.001 | 0.43 | .67 | ||
| Diseases | Depression 1 | Social Support 2 | −0.12 | −2.55 | .011 |
| PTSD 1 | 0.02 | −1.10 | .27 | ||
| Depression 1 | Daily Stresses 2 | 0.06 | 1.16 | .25 | |
| PTSD 1 | −0.008 | −0.42 | .67 | ||
| Depression 1 | Social Support 2 | Depression 2 | 0.08 | 2.61 | .009 |
| Daily Stresses 2 | 0.01 | 1.00 | .32 | ||
| PTSD 1 | Social Support 2 | Depression 2 | −0.02 | −1.24 | .22 |
| Daily Stresses 2 | −0.002 | −0.42 | .67 | ||
|
| |||||
| Depression 1 | Social Support 2 | Acculturation | −0.05 | −2.55 | .011 |
| Daily Stresses 2 | −0.02 | −1.15 | .25 | ||
|
| |||||
| Depression 1 | Social Support 2 | Depression 2 | 0.08 | 2.61 | .009 |
| Daily Stresses 2 | 0.01 | 1.00 | .32 | ||
As proposed in Hypothesis 1, pre-migration trauma assessed at baseline was both directly and positively associated with PTSD and depressive symptoms at baseline. Pre-migration trauma was also directly and positively associated with acculturation, but not with PTSD or depressive symptoms scores, at 1-year follow-up. The indirect effect of pre-migration trauma on acculturation, English language skills, and depressive symptoms at 1-year follow-up were non-significant; however, trauma was indirectly and positively associated with PTSD symptoms at 1-year follow-up.
Regarding Hypothesis 2, resilience at baseline was directly and negatively associated with depressive symptoms at 1-year follow up; however, resilience was not directly associated with PTSD symptoms, acculturation, or English language skills at 1-year follow-up. Resilience was not indirectly associated with any outcomes at 1-year follow-up.
As we proposed in Hypothesis 3, PTSD symptoms at baseline were directly, positively associated with PTSD symptoms at 1-year follow-up. PTSD symptoms at baseline, however, were neither directly nor indirectly associated with any other post-migratory mediators or outcomes at 1-year follow-up. PTSD symptoms at baseline were positively correlated with depressive symptoms at baseline (see Table 3). PTSD symptoms reported at 1-year follow-up were also correlated with depressive symptoms reported at the same point in time.
Similarly, depressive symptoms at baseline were both directly and indirectly positively associated with depressive symptoms at 1-year follow-up, but not with PTSD symptoms at 1-year follow-up. In contrast, depressive symptoms at baseline were directly and indirectly negatively associated with acculturation at 1-year follow-up. The number of chronic diseases at baseline was positively associated with depressive symptoms at 1-year follow-up (both directly and indirectly) and directly, positively associated with PTSD symptoms at 1-year follow-up. Indirectly, the number of diseases was negatively associated with acculturation and English language skills at 1-year follow-up.
Finally, regarding mediating associations (Hypothesis 4), exposure to daily stressors was directly associated with less acculturation and poorer English language skills at 1-year follow-up (see Figure 1), but not with 1-year follow-up PTSD or depressive symptoms. Social support was positively, directly associated with acculturation, and negatively associated with depressive and PTSD symptoms, after one year. A number of associations existed between baseline predictors and other baseline characteristics as well as post-migratory influences, and are reported in Table 2 and 3.
Discussion
In this longitudinal study of Iraqi refugees who were newly arrived in the U.S. during a time of multi-national war and ethnic conflict in Iraq, we found that pre-migration trauma predicted less acculturation after one year of resettlement (Hypothesis 1). Trauma also positively predicted refugees’ PTSD symptoms after 1 year, but only indirectly. This suggests that the relationship between trauma and PTSD symptoms is mediated by other exposures, perhaps by refugees’ social support (Ehlers & Clark, 2003; Huijts et al., 2012).
In partial confirmation of our hypotheses, higher baseline resilience was associated with fewer depressive symptoms 1 year after migration, but not with other resettlement outcomes (Hypothesis 2). In a similar population, Arnetz et al. (2013) found no association between resilience and PTSD symptoms, leading them to suggest that the effect of resilience was to foster pre-migratory processes during refugees’ development, which helped mitigate their response to subsequent trauma (Arnetz et al., 2013). A recently published longitudinal study investigating post-traumatic effects in a post-conflict, internally-displaced population (Sri-Lankan Muslims) found that although resilience promoted social interaction and support, it did not directly predict the occurrence of mental health disorders (Siriwardhana, Abas, Siribaddana, Sumathipala, & Stewart,2015). Maladaptive coping (e.g., denial, social isolation, substance abuse, self-blame) has, in contrast, been associated with worse physical and mental health and inadequate acculturation (Cummings et al., 2011; Matheson, Jorden, & Anisman, 2008; Morris et al., 2009; Noh & Kaspar, 2003). Our findings suggest that resilient coping skills by themselves are not adequate to help refugees re-settle well.
We found that PTSD and depressive symptoms at baseline predicted persistence of those symptoms at 1-year follow-up, but only depressive symptoms at baseline predicted less acculturation 1 year later (Hypothesis 3). Also, a greater number of chronic diseases at baseline predicted worse PTSD and depressive symptoms as well as less acculturation and English language skills after 1 year. A Canadian cross-sectional study reported that refugees with chronic health problems were less likely than native-born people to receive adequate healthcare for chronic diseases (Beiser & Hou, 2014). Also, a longitudinal study using path analysis among trauma-exposed internally displaced people in a number of conflict-affected countries found that mental health in the past year was the strongest predictor of future mental health, although economic growth (or lack thereof), was also an important predictor (Saragih Turnip, Sorbom, & Hauff, 2016). Clearly, there is a need to address somatic and mental health in tandem when assessing the health and wellbeing of refugees.
Mediating factors also appeared to impact re-settlement outcomes. As hypothesized, greater exposure to daily stressors over the follow-up year predicted worse acculturation (Hypothesis 4), but had no impact on PTSD or depressive symptoms. The sociopolitical and cultural contexts in which trauma occurs, and ongoing cumulative exposure to post-migration stressors, may be equally important in affecting re-settlement outcomes, especially for those who did not experience overt physical trauma (Steel, 2001; Summerfield, 1997).
On the other hand, social support had a strong effect on all re-settlement outcomes that we measured. Although our findings do not clarify whether social support originated from within or outside the refugee ethnic community, it appears that the more social support refugees receive, the better their acculturation will be, including lower levels of PTSD and depressive symptoms. In a study of 120 Arab men, Barry et al. (2005) reported that respondents with high levels of ethnic identity and interdependence with similar persons in their community of origin were more likely to use social supports within that community, and higher use of social support from a refugee’s ethnic community was associated with better acculturation. Collectivist versus individually-oriented decision-making may contribute to these effects. Among Middle Eastern communities, mental health problems may be viewed as social issues that need to be solved collectively. Refugees may view themselves as part of a cultural, relational web, from which they may seek social support, depending on their level of distress and resilience (Drozdek, 2007). Our social support results suggest that when refugees have a number of trusted family members and friends with whom to discuss their concerns, they are more likely to have a favorable resettlement trajectory.
To our knowledge, this is the first longitudinal study attempting to test the “stage” model proposed by Grove and Torbiorn (1995) and Gonsalves (1992). Our results suggest two main post-migratory trajectories for refugees. First, some refugees, for whatever reason (e.g., traumatic experiences, the presence of multiple chronic diseases, or high levels of depressive symptoms), do not experience social support post-migration and continue to experience adverse psychological symptoms similar to those experienced when they arrived. They are overwhelmed by daily stressors and make less progress in acculturation over the first year of resettlement. Second, refugees who obtain social support, even if they have mental health symptoms initially, are more likely to acculturate, have fewer mental health symptoms, and have better English language skills after the first year.
Although our findings support the basic Grove and Torbiorn model, we did not detect the post-migration de-compensatory stage that Gonsalves hypothesized may occur with some refugees (Gonsalves, 1992). Instead, our study suggests that pre-migration trauma, medical illness, and more depressive symptoms at baseline have adverse influences on refugees’ acculturation, at least through the end of their first post-migration year.
These findings are consistent with earlier research. A path analytic study found that pre-migration trauma and post-migration stress accounted for a similar proportion of PTSD symptoms among Tamil asylum seekers (Steel, Silove, Bird, McGorry, & Mohan, 1999). A more recent 6-year prospective study of 1022 adult survivors of the Timor Leste conflict found that PTSD symptoms and severe distress increased over time more among women, particularly among those with direct experience of severe trauma, and those with personal health problems or poverty (Silove et al., 2014). Unlike our study, however, they did not use path analysis to explore mediators of traumatic and other exposures on these outcomes. Our findings add to these studies by using longitudinal data to perform path analysis and including the simultaneous effects of positive characteristics such as resilience, along with mediating factors, such as social support and daily stressors.
This study has several limitations. First, we relied on refugees’ self-report for all measures, which can be biased in various ways. For example, social support may be over-reported (Henderson & Byrne, 1976; Henderson, Duncan-Jones, Byrne, & Scott, 1980), whereas some types of trauma (e.g., sexual trauma) and mental health problems may be under-reported, limiting accurate estimates of the relationship between such trauma and mental health (Drozdek, 2007), and leading to artificially low estimates of mental health problems. Furthermore, although we used recommended methods for translation and cultural validation of our measures (World Health Organization, 2016), most of the measures that we used were initially developed and validated on Western, non-refugee populations, and little psychometric information is available for these measures on Iraqi refugees. Thus, caution in interpretation is warranted. Second, Arnetz et al. (2014) found that some trauma subtypes accounted for more variation in PTSD and depressive symptoms than the cumulative number of traumas reported, which we used in this study and which is consistent with most refugee trauma studies. Our use of a cumulative trauma score may thus have underestimated the direct effect of trauma on PTSD and depression symptoms at 1-year follow up. Third, we followed the refugees for only 1 year post-migration. It is possible that changes in mental health and acculturation require longer follow-up. Fourth, although we tested a mediation model, it is possible that some variables, such as resilience, operate in a more complex manner than we tested, that is, they may moderate the various mediated longitudinal relationships. Finally, detecting more vulnerable subgroups would have required an even larger sample size.
Despite these limitations, this study advances the literature by using methods that, as noted by Hollifield (2002), are usually lacking in studies of refugee trauma and mental health (Hollifield et al., 2002). Our study assessed refugees at arrival, was conducted in a large, culturally homogeneous sample, used measures that were administered in a standardized fashion, and had a very low rate of attrition over the year. The latter is likely due to the fact that refugees were interviewed in Arabic by the same individual at both times, who scheduled and conducted interviews at times and places that were convenient for participants.
Our results imply that interventions to promote acculturation should be developed and rigorously evaluated in terms of their effects on and management of mental health symptoms and other diseases that refugees experience; and the degree to which an intervention promotes social support. Interventions that promote enhancement of refugees’ social environments (e.g., assistance in addressing mental health symptoms or management of chronic disorders) may assist refugees at highest risk of poor re-settlement outcomes (Drozdek, 2007). A recent cross-sectional study of traumatized refugees found that delayed access to mental health services after resettlement increased the risk of PTSD more than 3-fold, and of depression more than 4-fold, thus underscoring the importance of early intervention to prevent these outcomes (Song, Kaplan, Tol, Subica, & de Jong, 2015). Although refugees may gain skills to overcome barriers to accessing mental healthcare with longer duration of residence in a new country (Nose, Turrini, & Barbui, 2015), our results support expediting access via social support. A note of caution, however, comes from the intervention literature. A recent Cochrane review reported that psychological interventions for torture survivors showed, at most, moderate effects on PTSD and other psychological symptoms, and only after 6 months of participation (Patel, Kellezi, & Williams, 2014). This suggests that there may be a critical period after trauma exposure and symptom development and prior to migration when interventions might be most effective. Waiting until migration may be too late to intervene effectively, when the effect of poor social support or social isolation over an extended period prior to migration may lead to chronic disorders that negatively affect subsequent acculturation during post-migration settlement.
The findings reported here may have implications for refugee re-settlement programs in the US. Passage of the Refugee Act of 1980 established refugees’ rights to asylum in the U.S. and created a series of assistance programs that help refugees transition into life in the U.S. (Brown & Scribner, 2014). One of the central tenets of the U.S. Office of Refugee Resettlement administering the Act, however, is that refugees achieve “self-sufficiency,” which is interpreted as employment and economic independence (Brick et al., 2010). Emphasis on this aim has contributed to a progressive diminishment of funding for refugee support programs, and shortening of the duration of funding for individual refugees. In contrast, the policy of the U.S. State Department’s Bureau of Population, Refugees and Migration (PRM) is to re-settle the most vulnerable refugee populations, including those we have identified as being at high risk of poor outcomes. The PRM has recently mandated quarterly consultations between state and local governmental and voluntary agencies to arrange for newly arriving refugees’ financial and social support (Brown & Scribner, 2014). These consultations could provide an opportunity for improved coordination of service agencies to arrange for social support to newly arriving refugees, particularly if local agencies can gain access to relevant information to understand the needs of incoming refugees and make timely arrangements to provide that support (United Nations High Commissioner for Refugees, 2013). Future research should explore the size of the refugee population most at risk, and develop and test interventions to help those refugees overcome their barriers to re-settlement, as identified in this report.
Acknowledgments
This work was supported by the NIH / National Institute of Mental Health grants R01MH085793 and R34MH86943 (B. Arnetz, Principal Investigator). The content of this article is the sole responsibility of the authors and does not necessarily represent the views of NIMH. We gratefully acknowledge the following organizations that assisted us with recruitment: the Arab Community Center for Economic and Social Services (ACCESS), Lutheran Social Services of Michigan, the Arab American and Chaldean Council, the Chaldean Federation of America, the U.S. Commission on Resettlement and Immigration, Catholic Services of Macomb, and Kurdish Human Rights Watch. We are also in great appreciation of all our participants who, despite having suffered war trauma and life-challenging experiences, were willing to participate in this study.
Contributor Information
Joseph W. LeMaster, University of Kansas
Carissa L. Broadbridge, Wayne State University
Mark A. Lumley, Wayne State University
Judith E. Arnetz, Wayne State University
Cynthia Arfken, Wayne State University.
Michael D. Fetters, University of Michigan
Hikmet Jamil, Wayne State University.
Nnamdi Pole, Smith College.
Bengt B. Arnetz, Wayne State University
References
- Adkins JW, Weathers FW, McDevitt-Murphy M, Daniels JB. Psychometric properties of seven self-report measures of posttraumatic stress disorder in college students with mixed civilian trauma exposure. Journal of Anxiety Disorders. 2008;22(8):1393–1402. doi: 10.1016/j.janxdis.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Arnetz BB, Broadbridge CL, Jamil H, Lumley MA, Pole N, Barkho E, Arnetz JE. Specific trauma subtypes improve the predictive validity of the Harvard Trauma Questionnaire in Iraqi refugees. Journal of Immigrant Minority Health. 2014;16(6):1055–1061. doi: 10.1007/s10903-014-9995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnetz J, Rofa Y, Arnetz B, Ventimiglia M, Jamil H. Resilience as a protective factor against the development of psychopathology among refugees. Journal of Nervous and Mental Disease. 2013;201(3):167–172. doi: 10.1097/NMD.0b013e3182848afe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry DT. Measuring acculturation among male Arab immigrants in the United States: an exploratory study. Journal of Immigrant Health. 2005;7(3):179–184. doi: 10.1007/s10903-005-3674-9. [DOI] [PubMed] [Google Scholar]
- Beiser M, Hou F. Language acquisition, unemployment and depressive disorder among Southeast Asian refugees: a 10-year study. Social Science and Medicine. 2001;53(10):1321–1334. doi: 10.1016/s0277-9536(00)00412-3. doi.org/10.1016/S0277-9536(00)00412-3. [DOI] [PubMed] [Google Scholar]
- Beiser M, Hou F. Chronic health conditions, labour market participation and resource consumption among immigrant and native-born residents of Canada. International Journal of Public Health. 2014;59(3):541–547. doi: 10.1007/s00038-014-0544-z. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett D. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88(3):388–406. [Google Scholar]
- Berry J, Kim U, Minde T, Mok D. Comparative stuides of acculturative stress. International Migration Review. 1987;21(3):491–511. [Google Scholar]
- Bhopal RS. Migration, ethnicity, race and health in multi-cultural societies. 2. London: Oxford University Press; 2014. Assessing the health and health-care needs of migrant, racial and ethnic minorities using quantitative and qualitative data; pp. 118–162. [Google Scholar]
- Breeman S, Cotton S, Fielding S, Jones GT. Normative data for the hospital anxiety and depression scale. Quality of Life Research. 2015;24(2):391–398. doi: 10.1007/s11136-014-0763-z. [DOI] [PubMed] [Google Scholar]
- Brick K, Cusing-Savvi A, Elshafie S, Krill A, McGlynn Scanlon M, Stone M. Refugee Resettlement in the United States: An Examination of Challenges and Proposed Solutions. New York, NY: Columbia University School of International and Public Affairs; 2010. [Google Scholar]
- Brown A, Scribner T. Unfulfilled promises, future possibilities: The refugee resettlement system in the United States. Journal on Migration and Human Security. 2014;2(2):101–120. http://dx.doi.org/10.14240/jmhs.v2i2.27. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of asseessing model fit. Sociological Methods Research. 1992;21:230–258. [Google Scholar]
- Butow PN, Aldridge L, Bell ML, Sze M, Eisenbruch M, Jefford M, Goldstein D. Inferior health-related quality of life and psychological well-being in immigrant cancer survivors: a population-based study. European Journal of Cancer. 2013;49(8):1948–1956. doi: 10.1016/j.ejca.2013.01.011. [DOI] [PubMed] [Google Scholar]
- Carlsson JM, Mortensen EL, Kastrup M. Predictors of mental health and quality of life in male tortured refugees. Nordic Journal of Psychiatry. 2006;60(1):51–57. doi: 10.1080/08039480500504982. [DOI] [PubMed] [Google Scholar]
- Cohen S, Hoberman H. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology. 1983;13:99–125. [Google Scholar]
- Cummings S, Sull L, Davis C, Worley N. Correlates of depression among older Kurdish refugees. Social Work. 2011;56(2):159–168. doi: 10.1093/sw/56.2.159. [DOI] [PubMed] [Google Scholar]
- Doocy S, Sirois A, Tileva M, Storey JD, Burnham G. Chronic disease and disability among Iraqi populations displaced in Jordan and Syria. International Journal of Health Planning and Management. 2012;28(1):e1–e12. doi: 10.1002/hpm.2119. [DOI] [PubMed] [Google Scholar]
- Drozdek B. The re-birth of contextual thinking in psychotraumatology. In: Drozdek B, Wilson JP, editors. Voices of trauma: Treating psychological trauma across cultures. New York, NY: Springer; 2007. pp. 1–25. [Google Scholar]
- Edward L, Warelow P. Resilience: when coping is emotionally intelligent. Journal of the American Psychiatric Nurses Assocociation. 2005;11:101–102. doi: 10.1177/1078390305277526. [DOI] [Google Scholar]
- Ehlers A, Clark D. Early psychological interventions for adult survivors of trauma: a review. Biological Psychiatry. 2003;53(9):817–826. doi: 10.1016/s0006-3223(02)01812-7. doi.org/10.1016/S0006-3223(02)01812-7. [DOI] [PubMed] [Google Scholar]
- Fazel M, Wheeler J, Danesh J. Prevalence of serious mental disorder in 7000 refugees resettled in western countries: a systematic review. Lancet. 2005;365(9467):1309–1314. doi: 10.1016/s0140-6736(05)61027-6. [DOI] [PubMed] [Google Scholar]
- Gonsalves CJ. Psychological stage of the refugee process: a model for therapeutic interventions. Professional Psychology: Research and Practice. 1992;23(5):382–389. [Google Scholar]
- Gorst-Unsworth C, Goldenberg E. Psychological sequelae of torture and organised violence suffered by refugees from Iraq. Trauma-related factors compared with social factors in exile. British Journal of Psychiatry. 1998;172:90–94. doi: 10.1192/bjp.172.1.90. [DOI] [PubMed] [Google Scholar]
- Grove CL, Torbiorn I. A new conceptualization of intercultural adjustment and the goals of training. International Journal of Intercultural Relations. 1985;9:205–233. [Google Scholar]
- Henderson S, Byrne DG. Towards a method for assessing social support systems. Mental Health and Society. 1976;4:163–170. [PubMed] [Google Scholar]
- Henderson S, Duncan-Jones P, Byrne DG, Scott R. Measuring social relationships The Interview Schedule for Social Interaction. Psychological Medicine. 1980;10:723–734. doi: 10.1017/S003329170005501X. [DOI] [PubMed] [Google Scholar]
- Hoge EA, Austin ED, Pollack MH. Resilience: research evidence and conceptual considerations for posttraumatic stress disorder. Depression and Anxiety. 2007;24(2):139–152. doi: 10.1002/da.20175. [DOI] [PubMed] [Google Scholar]
- Hollifield M, Warner TD, Lian N, Krakow B, Jenkins JH, Kesler J, Westermeyer J. Measuring trauma and health status in refugees: a critical review. Journal of the American Medical Association. 2002;288(5):611–621. doi: 10.1001/jama.288.5.611. [DOI] [PubMed] [Google Scholar]
- Huijts I, Kleijn WC, van Emmerik AA, Noordhof A, Smith AJ. Dealing with man-made trauma: the relationship between coping style, posttraumatic stress, and quality of life in resettled, traumatized refugees in the Netherlands. Journal of Traumatic Stress. 2012;25(1):71–78. doi: 10.1002/jts.21665. [DOI] [PubMed] [Google Scholar]
- Joreskog KG, Sorbom D. LISREL 8 user’s guide. Chicago, IL: Scientific Software; 1993. [Google Scholar]
- Kanner AD, Coyne JC, Schaefer C, Lazarus RS. Comparison of two modes of stress measurement: daily hassles and uplifts versus major life events. Journal of Behavioral Medicine. 1981;4(1):1–39. doi: 10.1007/BF00844845. [DOI] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, appraisal and coping. New York: Springer; 1984. [Google Scholar]
- Lindert J, Ehrenstein OS, Priebe S, Mielck A, Brahler E. Depression and anxiety in labor migrants and refugees: A systematic review and meta-analysis. Social Science and Medicine. 2009;69(2):246–257. doi: 10.1016/j.socscimed.2009.04.032. [DOI] [PubMed] [Google Scholar]
- Lipson JG. Afghan refugees in California: mental health issues. Issues in Mental Health Nursing. 1993;14(4):411–423. doi: 10.3109/01612849309006903. [DOI] [PubMed] [Google Scholar]
- Matheson K, Jorden S, Anisman H. Relations between trauma experiences and psychological, physical and neuroendocrine functioning among Somali refugees: mediating role of coping with acculturation stressors. Journal of Immigrant Minority Health. 2008;10(4):291–304. doi: 10.1007/s10903-007-9086-2. [DOI] [PubMed] [Google Scholar]
- Millsap RE. Structural equation modeling: a user’s guide. In: Drasgow F, Schmitt N, editors. Measuring and analyzing behavior in organizations: advances in measurement and data analysis. San Francisco, CA: Jossey-Bass; 2002. pp. 257–301. [Google Scholar]
- Morris MD, Popper ST, Rodwell TC, Brodine SK, Brouwer KC. Healthcare barriers of refugees post-resettlement. Journalof Community Health. 2009;34(6):529–538. doi: 10.1007/s10900-009-9175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. American Journal of Public Health. 2003;93(2):232–238. doi: 10.2105/ajph.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nose M, Turrini G, Barbui C. Access to mental health services and psychotropic drug use in refugees and asylum seekers hosted in high-income countries. Epidemiology and Psychiatric Sciences. 2015;24(5):379–381. doi: 10.1017/s2045796015000578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel N, Kellezi B, Williams AC. Psychological, social and welfare intervenitions for psychological health and well-being of torture survivors. Cochrane Database of Systematic Reviews. 2014;11:CD009317. doi: 10.1002/14651858.CD009317.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Leonardelli GJ. Calculation for the Sobel test: An interactive calculation tool for mediation tests. 2001 Retrieved from http://quantpsy.org/sobel/sobel.htm.
- Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381(9873):1235–1245. doi: 10.1016/s0140-6736(12)62086-8. [DOI] [PubMed] [Google Scholar]
- Rutter M. Psychosocial resilience and protective mechanisms. American Journal of Orthopsychiatry. 1987;57(3):316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. doi.org/10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- Saragih Turnip S, Sorbom D, Hauff E. Predicting positive mental health in internally displaced persons in Indoneisa: the roles of economic development and exposure to violent conlict. Psychol Health Med. 2016;21(3):286–294. doi: 10.1080/13548506.2015.1051554. [DOI] [PubMed] [Google Scholar]
- Schumacker RE, Lomax RG. A beginner’s guide to structural equation modeling. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1996. pp. 119–137. [Google Scholar]
- Shoeb M, Weinstein H, Mollica R. The Harvard Trauma Questionnaire: adapting a cross-cultural instrument for measuring torture, trauma and posttraumatic stress disorder in Iraqi refugees. International Journal of Social Psychiatry. 2007;53(5):447–463. doi: 10.1177/0020764007078362. [DOI] [PubMed] [Google Scholar]
- Silove D, Liddell B, Rees S, Chey T, Nickerson A, Tam N, Zwi AB, Brooks R, Sila LL, Steel Z. Effects of recurrent violence on post-traumatic stress disorder and severe distress in conflict-affected Timor-Leste: a 6-year longitudinal study. Lancet Global Health. 2014;2(5):e293–300. doi: 10.1016/S2214-109X(14)70196-2. [DOI] [PubMed] [Google Scholar]
- Siriwardhana C, Abas M, Siribaddana S, Sumathipala A, Stewart Dynamics of resilience in forced migration: a 1-year follow-up study of lingitudinal associations with mental health in a conflict-affected, ethnic Muslim population. BMJ Open. 2015;5(2):e006000. doi: 10.1136/bmjopen-2014-006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel ME. Direct and indirect effects in linear structural equation models. Sociological Method Research. 1987;16:155–176. [Google Scholar]
- Song SJ, Kaplan C, Tol WA, Subica A, de Jong J. Psychological distress in torture survivors: pre- and post-migration risk factors in a US sample. Social Psychiatry and Psychiatric Epidemiology. 2015;50(4):549–560. doi: 10.1007/s00127-014-0982-1. [DOI] [PubMed] [Google Scholar]
- Sorkin D, Tan AL, Hays RD, Mangione CM, Ngo-Metzger Q. Self-reported health status of vietnamese and non-Hispanic white older adults in California. Journal of the American Geriatric Society. 2008;56(8):1543–1548. doi: 10.1111/j.1532-5415.2008.01805.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel Z, Silove D, Bird K, McGorry P, Mohan P. Pathways from war trauma to posttraumatic stress symptoms among Tamily asylm seekers, refugees and immigrants. Journal of Traumatic Stress. 1999;12(3):421–35. doi: 10.1023/A:1024710902534. [DOI] [PubMed] [Google Scholar]
- Steel Z. Beyond PTSD: towards a more adequate understanding of the multiple effects of complex trauma. In: Moser C, Verwey M, editors. Traumatisierungen von Fluchtlingen und Asyl Suchenden: einfluss des politischen, sozialen und medizinischen Kontextes. Zurich: Seismo; 2001. pp. 66–84. [Google Scholar]
- Steel Z, Chey T, Silove D, Marnane C, Bryant RA, van Ommeren M. Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: a systematic review and meta-analysis. Journal of the American Medical Association. 2009;302(5):537–549. doi: 10.1001/jama.2009.1132. [DOI] [PubMed] [Google Scholar]
- Summerfield D. The impact of war and atrocity on civilian populations. In: Black D, Newman M, Harris-Hendriks J, Mezey G, editors. Psychological trauma: a developmental approach. London: Gaskell; 1997. pp. 148–155. [Google Scholar]
- Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Social Psychiatry and Psychiatric Epidemiology. 2005;40(8):672–679. doi: 10.1007/s00127-005-0943-9. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs, National Center for PTSD. Using the PTSD checklist (PCL) 2012 Retrieved from http://www.ptsd.va.gov/professional/pages/assessments/ptsd-checklist.asp.
- United Nations High Commission on Refugees. Statistical Yearbook 2010: Ten years of statistics. 2010 Retrieved from http://www.unhcr.org/4ef9c8d10.html.
- United Nations High Commissioner for Refugees. Resettlement and Women at Risk: Can the Risk Be Reduced? 2013 Retrieved from http://www.unhcr.org/51de6e929.html.
- Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. Journal of Nursing Measurement. 1993;1(2):165–178. [PubMed] [Google Scholar]
- Westermeyer J, Neider J, Callies A. Psychosocial adjustment of Hmong refugees during their first decade in the United States. A longitudinal study. Journal of Nervous and Mental Disorders. 1989;177(3):132–139. doi: 10.1097/00005053-198903000-00002. [DOI] [PubMed] [Google Scholar]
- Williams LJ, Hazer JT. Antecedents and consequences of satisfaction and commitment in turnover models: a re-analysis using latent variable structure equation models. Journal of Applied Psychology. 1986;71(2):219–231. [Google Scholar]
- World Health Organization. Process of translation and adaptation of instruments. 2016 http://www.who.int/substance_abuse/research_tools/translation/en/. Accessed October 10, 2016.
- Yun K, Fuentes-Afflick E, Desai MM. Prevalence of chronic disease and insurance coverage among refugees in the United States. Journal of Immigrant and Minority Health. 2012;14(6):933–940. doi: 10.1007/s10903-012-9618-2. [DOI] [PubMed] [Google Scholar]
- Yun K, Hebrank K, Graber LK, Sullivan MC, Chen I, Gupta J. High prevalence of chronic non-communicable conditional among adult refugees: implications for policy and practice. Journal of Community Health. 2012;37(5):1110–1118. doi: 10.1007/s10900-012-9552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]


