Abstract
The objectives were to determine the incidence of hearing impairment in a standardized population of neonates and to determine the significance of association of epidemiological and risk factors with neonatal hearing loss. A cohort of 600 newborns was selected for study and divided into two groups—525 in ‘No Risk’ group and remaining 75 in ‘At Risk’ group. The study protocol was carried out in three steps: (a) Screening of Hearing Loss with TOAE, done from 36 h after birth to 28 days of life, (b) Re-screening of hearing loss in newborns (of 4–12 weeks of age), who were tested positive for hearing loss in the first screening, done with DPOAE, (c) Confirmation of hearing loss with BERA, in those who were tested positive in both the first and second screening. In the study the incidence of hearing impairment in 600 infants screened was 6.67 per 1000 screened; 3.81 per 1000 screened in the Not at Risk group and 26.67 per 1000 screened in At Risk group. In At Risk group, admitted to the NICU, severe birth asphyxia and hyperbilirubinemia were found to be major risk factors. Loss to follow up was more in Not at Risk group and False Positive cases with TEOAE were more than DPOAE. BERA was found to be must for confirmation of hearing loss. Neonatal Hearing Screening of only At Risk population is likely to miss some hearing loss. Universal Hearing Screening should be the preferred strategy. Good follow up in the ‘At Risk’ group suggests that initial interventions in NICU had sensitized the parents for the possibility of hearing loss. This study recommends the introduction of two stage neonatal screening–rescreening protocol, using OAE and BERA, in the country in phased manner.
Keywords: Universal Hearing Screening, Otoacoustic Emissions, Brain-stem evoked response audiometry
Introduction
Normal hearing is necessary for development of expressive language and consequent social, emotional and intellectual development of a child. Hearing impairment during the critical phase of infancy and childhood affect the development of speech and language. Early detection of hearing impairment and energetic intervention thereafter in children has significant psycho-social, linguistic and educational repercussions. Intervention at or before 6 months of age allows a child with hearing impairment to develop normal speech and language, like his or her hearing peers.
The study was performed in Command Hospital, Lucknow; in a selective group of population. Our aim was to evaluate the efficacy of various strategies of screening for hearing loss in neonates. Our objectives were to determine the incidence of hearing impairment in a standardized population of neonates, comparative efficacy of the screening protocols used in detecting hearing loss and significance of association of epidemiological and risk factors with neonatal hearing loss.
Materials and Methods
It was a non-randomized prospective multiple cohort study conducted in Command Hospital, Lucknow for the period of 1 year. The study population was divided into two groups, “At Risk” and “No Risk” groups as per criteria adapted from the American Joint Committee statement on Infant hearing screening (JCIH), 2007 [1].
Children of Eastern Uttar Pradesh territory, between 36 h and 28 days of age without gender bias, born in hospital or elsewhere, but attending the hospital during the period of study, or admitted to Neonatal Intensive Care Unit, were included. Neonates having evidence of middle ear pathology, meatal atresia, fatal event before the completion of the study or refusal by the parents; were excluded.
A voluntary informed written consent of the parent or legal guardian for the conduct of the study on the subject was taken. Complete ENT examination to exclude congenital anomaly or active ear infection, was done. The test Equipment was Audio Screener Analyzer manufactured by Messers Grason Stadler Instrument (GSI), USA; having provision for screening OAEs as well as screening BERA (Fig. 1).
Fig. 1.
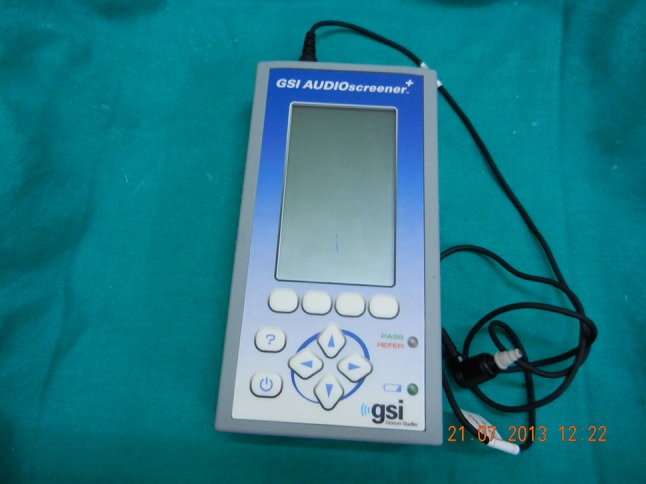
The audioscreening device used in the study
Initial Screening with Transient Evoked Otoacoustic Emissions (TOAE) for both At Risk and Not at Risk neonates was done. Re-screening with Distortion Product Otoacoustic Emission (DPOAE) for those who failed with TOAE test was done after 1 month of the test. Confirmation of hearing loss with BERA for those who failed with DPOAE test was done.
Results
In the study cohort male to female ratio was 1.07:1.00. The incidence of hearing impairment in 600 infants screened was 4 (6.67 per 1000 screened); 2 (3.81 per 1000 screened) in the 525 infants (No Risk) and 2 (26.67 per 1000 screened) in 75 infants (At Risk). So the incidence of hearing loss in At Risk group was higher than No Risk group.
In At Risk group, 63 newborns were admitted to the NICU, of which two newborns were found to have confirmed hearing loss. They were having severe birth asphyxia and hyperbilirubinemia respectively, as major risk factors identified.
In 525 Not at Risk neonates, on initial screening with TEOAE screening protocol, 24 (4.5%) were referred signifying the possibility of hearing loss. On re-screening, only 13 out of 24 reported for follow up (fall out rate of 45.8%); Of these 13, 5 (38.4%) were found to have hearing loss on re-screening DPOAE, remaining 8 constituted false positives for the initial screening with TEOAE. In At Risk group, on initial screening with TEOAE, 8 out of 75 (10.7%) were referred signifying the possibility of hearing loss. On re-screening, all 8 reported for follow up (0% fall out rate). Of these 8, 3 constituting 37.50% were found to have hearing loss on re-screening DPOAE (62.50% constituted false positives for the initial screening with TEOAE). On BERA testing, 2 out of these 3 were confirmed to have hearing loss. Therefore loss to follow up was more in No Risk group and False Positive cases with TEOAE were more than DPOAE. BERA was found to be must for confirmation of hearing loss.
Discussion
Energetic attempts are required to detect congenital and acquired anomalies that are hard to prevent. Neonatal hearing loss is supposed to be one such clinical entity. Screening procedures form the core component of this process. Early identification, before significant handicap accrues, offer the best opportunity to initiate effective interventions. When primary prevention is difficult, the early identification and treatment with appropriate and early rehabilitation of hearing loss becomes the main priority, rather to correct disability at a later stage.
Universal Neonatal Hearing Screening (UNHS) was initially attempted using instruments such as Crib-o-gram and risk registers [2]. Development of OAE and ABR technologies in the 1980s made it feasible to use an objective, non-invasive instrument that could be administered to all infants.
Data from the newborn hearing screening program in Rhode Island [3], Colorado [4] and Hawai [5] show that 2–4 of every 1000 neonates having hearing loss. In a retrospective study, it was found that 1 in every 811 infant without risk factors and 1 in every 75 infant with risk factor were having hearing loss [6]. In another study, the prevalence of hearing loss through Universal Neonatal Hearing Screening program was found variable between 1.4/1000 and 6/1000. For population with audiologic risk factor this value reached 3–5% [7–10]. The report of the 58th round of the National Sample Survey Organization of India (NSSO, 2002) estimates that 18.49 million (1.8% of the total population of the country) are disabled. According to this survey the estimated incidence of hearing loss in India stands at 3.1 in rural areas and 2.36 in urban areas [11]. Recent reports from India suggest the incidence of hearing impairment in infants screened was 5.65 per 1000 screened [12].
In our study, we preferred to use OAE as the initial screening method over ABR because the studies which compare screening technologies, rate OAE screening methods higher than the traditional ABR screening. The two most common OAE screening methods currently available are Transient Evoked OAE and Distortion Product OAE. Although both have been successfully employed in hearing screening, majority of the large studies have preferred TEOAEs over DPOAE.
Screening at birth with OAEs and later confirming the hearing loss by sixth month was taken as the standard. It was studied that, though cochlea is fully developed at birth, the myelination of VIII nerve and maturation of brainstem takes nearly 6 months. This is why in most of the screening and rescreening protocols, final confirmation of hearing loss is made only at around 6 months of age. This factor is also responsible for any possible false positive results that may result from immature central connections of cochlea [13, 14].
Neonates in our study in the At Risk group had exposure in all cases to more than one risk factor. Sharing of multiple risk factors is common experience noted in other studies. One of such studies found 20% incidence of hearing impairment at high risk neonates [15]. The other one found bilateral hearing loss in 9.7% of very low birth weight infants and 16.7% in infants who survived neonatal seizures [16].
Hypoxia associated SNHL in neonates is mainly related to Persistent Pulmonary Hypertension (PPHN) and Extra-corporeal Membrane Oxygenation (ECMO). PPHN occurs in full term infants, as a result of failure of the circulatory adaptation at birth causing a right to left shunt and is associated with hypoxemia. 12 out of 80 children were found to have SNHL in a study of such type, constituting 15% [17, 18].
Along with asphyxia, the second major association in our study of hearing loss in neonates was with hyperbilirubinemia. Hyperbilirubinemia is known to cause specific changes in ABR waveforms, which disappear after reversion to normal bilirubin levels through exchange transfusion.
The sensitivity and specificity of TEOAEs as a screening test for neonatal hearing loss has been extensively studied in several community projects. One study found the specificity of 70% in initial screening with TEOAEs in the Rhode Island Hearing Assessment Project [19]. Another study reported 84% specificity for TEOAE in NICU Population [20]. We have intentionally not reported specificity and sensitivity of this screening tool as this was meant to be a pilot study and no significant statistical conclusions can be derived with the small sample size we have in this study. A larger multi-centric study would be in order to report this important data.
Conclusion
Neonatal Hearing Screening of only At Risk population is likely to miss some hearing loss. Universal Hearing Screening should be the preferred strategy.
Because of small numbers specificity/sensitivity of tests could not be studied. Cost benefit analysis of two strategies could not be performed.
Ambient noise in labour rooms and NICU was high, so-test results were some times not consistent.
Good follow up in the ‘At Risk’ group suggests that initial interventions in NICU had sensitized the parents for the possibility of hearing loss.
We recommend introduction of universal neonatal hearing screening programme in the country in phased manner. Screen–Rescreen-Confirmation protocol should be by using OAE and BERA. Screening should be within the first 4 weeks, re-screening with immunization within 6 months and to start appropriate intervention within 6 months.
Compliance with Ethical Standards
Conflict of interest
There is no conflict of interest between the authors of this manuscript.
Ethical Approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from parents of all individual participants included in the study.
References
- 1.Joint Committee on Infant Hearing Year 2007 position statement: principles and guidelines for early hearing detection and intervention programs. Pediatrics. 2007;120:898. doi: 10.1542/peds.2007-2333. [DOI] [PubMed] [Google Scholar]
- 2.Downs MP. Universal newborn hearing screening—the Colorado story. Int J Pediatr Otorhinolaryngol. 1995;32:257–259. doi: 10.1016/0165-5876(95)01183-C. [DOI] [PubMed] [Google Scholar]
- 3.Vohr BR, Carty L, Moore P, Letourneau K. The Rhode Island hearing assessment program: experience with statewide hearing screening (1993–1996) J Pediatr. 1998;128:710–714. doi: 10.1016/S0022-3476(96)80143-0. [DOI] [PubMed] [Google Scholar]
- 4.Colorado Department of Education (2001) A blueprint for closing the gap. http://www.cde.state.co.us/cdesped/download/pdf/dhh-blueprint.pdf
- 5.Johnson JL, Kuntz NL, Sia CC, White KR, Johnson RL. Newborn hearing screening in Hawaii. Hawaii Med J. 1997;56(12):352–355. [PubMed] [Google Scholar]
- 6.Connolly JL, Carron JD, Roark SD. Universal newborn hearing screening: are we achieving the Joint Committee on Infant Hearing (JCIH) objectives. Laryngoscope. 2005;115(2):232–236. doi: 10.1097/01.mlg.0000154724.00787.49. [DOI] [PubMed] [Google Scholar]
- 7.Gravel JS (2005) Evidence-based pediatric audiology. In: Seewald RC, Bamford JM (eds) A sound foundation through early amplification 2004: proceedings of the 3rd international conference. Immediate Proceedings, London, pp 17–26
- 8.Gravel J, Berg A, Bradley M, Cacace A, Campbell D, Dalzell L, et al. New York State universal newborn hearing screening demonstration project: effects of screening protocol on inpatient outcome measures. Ear Hear. 2000;21:131–140. doi: 10.1097/00003446-200004000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Gravel J, White K, Johnson J, et al. A multisite study to examine the efficacy of the otoacoustic emission/automated auditory brainstem response newborn hearing screening protocol: results of visual reinforcement audiometry. Am J Audiol. 2005;14(2):S200–S216. doi: 10.1044/1059-0889(2005/023). [DOI] [PubMed] [Google Scholar]
- 10.Gravel J, Roberts J, Roush J, Grose J, Besing J, Burchinal M, Neebe E, Wallace I, Zeisel S. Early otitis media with effusion, hearing loss, and auditory processes at school age. Ear Hear. 2006;27(4):353–368. doi: 10.1097/01.aud.0000224727.45342.e9. [DOI] [PubMed] [Google Scholar]
- 11.National Sample Survey Organisation. A publication of Department of Statistics, Government of India, New Delhi. DDI-IND-MOSPI-NSSO-58Rnd- Sch26-July2002-Dec2002
- 12.Nagapoornima P, Ramesh A, Srilakshmi, Rao S, Patricia PL, Gore M, Dominic M, Swarnarekha Universal hearing screening. Indian J Pediatr. 2007;74(6):545–549. doi: 10.1007/s12098-007-0105-z. [DOI] [PubMed] [Google Scholar]
- 13.Fujikawa SM, Weber BA. Effects of increased stimulus rate on brainstem electric response (BER) audiometry as a function of age. J Am Audiol Soc. 1977;3(3):147–150. [PubMed] [Google Scholar]
- 14.Lai Y, van Drongelen W, Ding L, Hecox KE, Towle VL, Frim DM, He B. Estimation of in vivo human brain-to-skull conductivity ratio from simultaneous extra- and intra-cranial electrical potential recordings. Clin Neurophysiol. 2005;116(2):456–465. doi: 10.1016/j.clinph.2004.08.017. [DOI] [PubMed] [Google Scholar]
- 15.Stein LK. Factors influencing the efficacy of universal newborn hearing screening. Pediatr Clin N Am. 1999;46(1):95–105. doi: 10.1016/S0031-3955(05)70084-5. [DOI] [PubMed] [Google Scholar]
- 16.Bergman I, Hirsch RP, Fria TJ, et al. Cause of hearing loss in the high-risk premature infant. J Pediatr. 1985;106:95–101. doi: 10.1016/S0022-3476(85)80476-5. [DOI] [PubMed] [Google Scholar]
- 17.Desai NS, Rutherford LC, Turrigiano GG. Plasticity in the intrinsic excitability of cortical pyramidal neurons. Nat Neurosci. 1999;2:515–520. doi: 10.1038/9165. [DOI] [PubMed] [Google Scholar]
- 18.Desai NS, Cudmore RH, Nelson SB, Turrigiano GG. Critical periods for experience-dependent synaptic scaling in visual cortex. Nat Neurosci. 2002;5:783–789. doi: 10.1038/nn878. [DOI] [PubMed] [Google Scholar]
- 19.White KR, Vohr BR, Meyer S, Widen JE, Johnson JL, Gravel JS, et al. A multisite study to examine the efficacy of the otoacoustic emission/automated auditory brainstem response newborn hearing screening protocol: research design and results of the study. Am J Audiol. 2005;14:S186–S199. doi: 10.1044/1059-0889(2005/021). [DOI] [PubMed] [Google Scholar]
- 20.Stevens J, Wood S (2004) NHSP in England: screening equipment. Paper presented at the international newborn hearing screening symposium, Como, Italy, May 2004


