Abstract
Rhinoplasty is one of the oldest known surgeries to the human kind. However, being a cosmetic of surgery of utmost importance, it has been an attractive and fascinating surgery for the otolaryngologists and plastic surgeons. Along with the evolution of improved techniques and better surgical modalities, this surgery has been growing in panorama including its indications, needs and techniques. We present our experience with rhinoplasty in a tertiary care center of north India. We have included all cases operated with septorhinoplasty from 2001 to 2014 by the senior author in the manuscript. We reviewed their presentations, investigations, preoperative counselling records, operative details and post-operative clinical records to audit our results and hence to document our experiences in septorhinoplasties. A total of 53 cases including 37 males and 16 females had undergone rhinoplasty surgeries. The most common reason of disfigurement was road traffic accident (58.5%). All these patients included different deformities and required varied corrections. There were no major post-operative complications except persistent edema with longest lasting for 23 weeks. Thermal splints gave a better patient satisfaction in post-op compared to POP splints. Results were completely and partially satisfying for 50 patients and not satisfying for three. Unrealistic expectations from the procedure might be the reason for non-satisfactory results in rhinoplasty. Rhinoplasty is a delicate procedure and has greater aesthetic implications in planning surgical techniques and approaches. For better satisfaction of patients, adequate preoperative counseling and realistic expectations are warranted. Skillful surgical techniques null chances of complications.
Keywords: Septoplasty, Rhinoplasty, Septorhinoplasty, Revision rhinoplasty, Augmentation rhinoplasty, External nasal deformity, Sports injury
Introduction
Among the aesthetic surgical procedures performed in the world, rhinoplasty is the oldest performed in the history. It was initially developed in ancient Greece and India (Sushruta Samhita). Sushruta is considered as the father of rhinoplasty surgery in the world [1]. The first documented evidence of the available records regarding rhinoplasty comes from Edwin smith papyrus [2]. This surgery has varied indications ranging from functional obstructions in the nasal cavity to pure cosmetic reasons and these include asymmetry of the alar cartilages or upper lateral cartilages, nasal tip with lack of support, rotation or projection, over projected nose, nasal tip asymmetry or deformities, crooked nose, saddle nose, cleft lip nose or other congenital anomalies, septal perforations and revision rhinoplasty [3].
Detailed knowledge of the intricacies of nasal anatomy, analysis of the anatomy including its variations and goal directed surgical planning in each individual case is the key to a successful rhinoplasty [4]. Detailed analysis should include individual consideration of skin and soft tissues, nasal bones and bony alterations, facial muscular attachments, septum, lower and upper lateral cartilages, turbinates, internal and external nasal valves and adequacy of nasal airway [5]. Facial aesthetic measurements like tip projection, proportional length of the nose, radix projection, naso-labial angle and naso-facial angle and tip rotation, projection and domal definition points play important role in determining the changes that need to be achieved objectively in order to attempt for the desired target in primary rhinoplasty [4, 6].
Though a commonly performed procedure now days, rhinoplasty has definite legalities associated with it. Hence, detailed counseling of the patient in terms of realistic expectations, outcomes and possible complications is an integral part of any rhinoplasty procedure. It should be associated with detailed photographic documentation and evaluation including right and left lateral and oblique views along with anterior, inferior(basal) and superior views for analyzing the target, outcomes and for discussing the surgical and aesthetic issues with the patient [7, 8].
We, at our tertiary care institute tried to evaluate outcome of cases done by the senior author in order to analyze our experience of rhinoplasty as a part of internal audit and to through light upon an otolaryngologists’ perspective in rhinoplasty cases. We present our experience in this paper.
Materials and Methods
Retrospective chart review of all individuals of external nasal deformity who underwent rhinoplasty by the senior author from 2001 to 2014 in our tertiary care institute was done. We evaluated all the treatment records including clinical presentation, routine blood investigations, skiagrams of the nose and paranasal sinuses (PNS) and nasal bones, high resolution CT images of the nose, PNS with 3D reconstruction of face in posttraumatic cases along with analysis of photographs of all the patients in all 6 views were analyzed. All such patients under went detailed facial photography in frontal or anterior profile view, basal or inferior view, superior view, right and left oblique view and right and left lateral views as per protocol. All patients had undergone detailed facial analysis including objective measurement of facial angles, target oriented realistic psychological assessment and counseling prior to pre anesthetic checkup and surgical planning. Type of deformity, etiology, surgical procedures performed, grafts and splints used were analyzed and studied. Among the surgical procedures; in closed rhinoplasty, ipsilateral or bilateral inter cartilaginous incisions were made and in open rhinoplasty, inverted sea-gull wing incision was used. Flap was elevated over nasal dorsum in supra perichondrial and sub periosteal plane. Humps was reduced with rasps and for saddle deformity iliac crest bone graft and septal bone or cartilage were used. Osteotomies had been done in cases of crooked or deviated noses. Tip corrections as required were done. After achieving hemostasis, merocel nasal packs were used followed by nasal splints. Anterior nasal packs were removed after 48–72 h and splints were removed after 7 days after surgery. Antibiotics, analgesics and decongestant were given for 7 days.
Results
A total of 53 cases were operated by the senior author in these years. There were 37 males and 16 females among the patients with a male to female ratio of 2.31 to 1. The mean age was 31.5 years with age ranged between 15 and 48 years among those who presented to the author for rhinoplasty. This suggests that adults of all age groups visit ENT clinics for rhinoplasty (Table 1).
Table 1.
Age and sex distribution of patients who were taken for rhinoplasty
| Age range/mean age | ||
|---|---|---|
| Total no. of patients | 53 | 15–48 years/31.56 years |
| Male | 37 | 15–48 years/31.99 years |
| Female | 16 | 18–41 years/29.45 years |
History and cause for which they underwent rhinoplasties were noted in patients. The most common reasons for which our patients attended the clinic for rhinoplasty were results of trauma mostly after road traffic accidents. 31 out of 53 (58.5%) patients in the present analysis had developed the deformities after road traffic accidents. Sports injuries were responsible in 4/53(7.5%) cases including 3 cases of cricket ball injury and one case of boxing injury. Three patients had history of septal abscess and two patients had history of septoplasty as the cause of their deformities. Rest 13/53(24.5%) cases had developmental cause as the reason for their deformities (Table 2).
Table 2.
Etiological causes of external nasal deformity in patients who underwent rhinoplasty
| Attributable causes from history | No. of patients | Percentage |
|---|---|---|
| Road traffic accidents | 31 | 58.5% |
| Sports Injury | 4 | 7.5% |
| Cricket ball injury | 3 | |
| Boxing injury | 1 | |
| Post septal abscess | 3 | 5.67% |
| Post septoplasty | 2 | 3.78% |
| Developmental | 13 | 24.52% |
| Total patients | 53 |
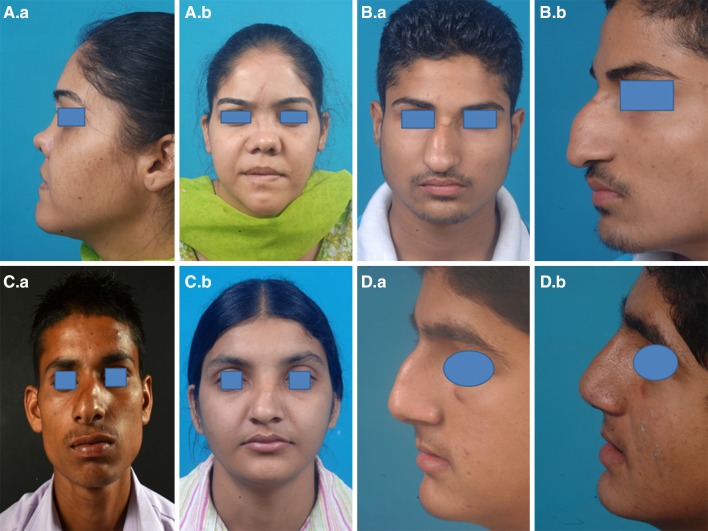
Out of 53 cases, 24 persons (45.28%) had presented with saddle nose deformity and requested for the correction. Ten patients had hump deformity and 18 patients had crooked/deviated nose with multiple deformities which made them to visit our outpatient clinic. One patient who had a history of boxing injury had an open roof deformity. Associated septal deviations necessitating corrections was required in 42 out of 53 patients with rest requiring only nasal corrections (Table 3). Figure 1(A.a, A.b) shows a patient with saddle nose deformity. Figure 1(B.a, B.b) shows a patient with hump deformity and deviation of external nasal pyramid which had developed after cricket ball injury. Figure 1(C.a, C.b) shows crooked nose in two patients who had presented to the clinic.
Table 3.
Type of deformities observed in rhinoplasty patients
| Type of deformity | No. of patients |
|---|---|
| Saddle nose deformity | 24 |
| Hump deformity | 10 |
| Crooked nose (Multiple deformities) |
18 |
| Open roof deformity (Boxing injury patient) |
1 |
| Associated deviated nasal septum | 42 |
| Deformities of tip | 14 |
Fig. 1.
A (a, b) A patient with saddle nose deformity. B (a, b) A patient with hump deformity and deviation of external nasal pyramid which had developed after cricket ball injury. C (a, b) Crooked nose in 2 patients who presented to the clinic. D (a, b) A patient with humped nose post hump reduction surgery
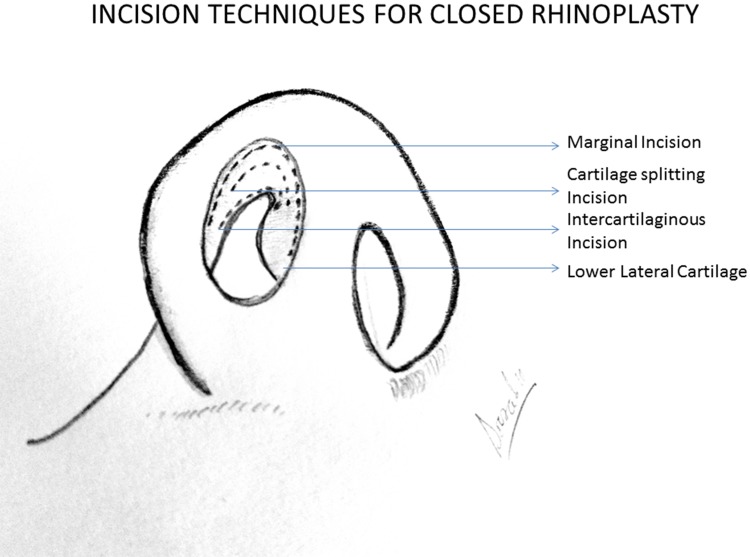
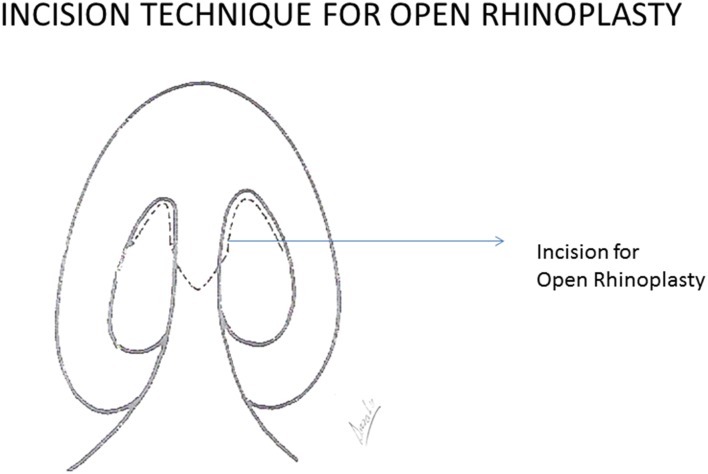
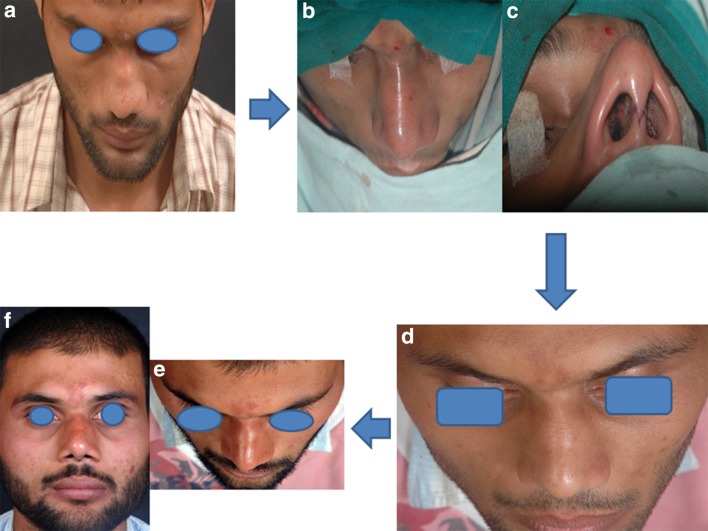
We also reviewed the details of the surgical techniques that the patients had undergone to determine the extent of surgical work that was required. 24 patients under went closed rhinoplasty surgeries using Marginal and Intercartilaginous incisions (Fig. 2) and open rhinoplasty (Figs. 3 and 5c) had to be performed 29 cases. Supra perichondrial and sub periosteal plane of dissection (Fig. 4 A.b) was used in both the techniques of rhinoplasty for elevation of the soft tissue. 43 patients required septorhinoplasty as the surgical procedure. 24 patients required augmentation and 14 patients required tip plasty techniques during the surgery for adequate corrections to be achieved. Of the 24 persons who required augmentation, septal bone and cartilage was used in 14 patients and 10 patients required iliac crest bone as grafts to be put. Mean hospital stay was 9.5 days (5–14 days). Splints were used in all patients after surgery. Thermal external nasal splints were used in 41 patients and POP cast splints were used in 12 patients. There was no difference in the post-operative outcome between the patients in terms of the splint used, however patients’ satisfaction concerned with splints and immediate post-operative aesthetic appearance as per patients was poor with POP cast splints. Figure 1(D.a and D.b) shows a patient with humped nose post hump reduction surgery. Figure 4(A.a, A.b and A.c) shows a patient with saddle nose deformity where iliac crest bone grafting was done. Figure 4B shows a case of tip-plasty inpre-op period (B.a) and in the post op period with a more defined tip (B.b). Figure 5 shows a patient with crooked nose with left deviation of external nasal pyramid being straightened with open rhinoplasty.
Fig. 2.
Incision techniques used for closed rhinoplasty surgeries. Marginal and Intercartilaginous incisions were used in our series
Fig. 3.
The Incision used for Open Rhinoplasty surgeries in the present series. (combination of bilateral marginal and midline columella incision)
Fig. 5.
A patient with crooked nose with left deviation of external nasal pyramid being straightened with open rhinoplasty
Fig. 4.
A (a, b and c) A patient with saddle nose deformity where iliac crest bone grafting was done. B (a, b) A case of tip-plasty in the post op period with a more defined tip
There was no intraoperative and post-operative complication noticed among our cases. However, short term anesthesia over nose was seen in 3 patients which resolved by 3–4 weeks in the post-operative period. 5 patients did present to us with persistent swelling and edema over nasal dorsum which persisted more than 6 weeks and took longer to resolve. All these patients got resolution of their persistent edema in due course of time with the longest persisting upto approximately 23 weeks in one patient.
Patients’ satisfaction levels from the procedures were routinely documented in the post op visits. 45 patients were satisfied with the results with 5 patients being partially satisfied. Three persons were not satisfied with the results of the surgical procedures. Patients who had shown partial satisfaction with the results were advised for revision surgeries however none of those patients had consented for a revision surgery. Donor site morbidity was not reported among the cases.
Discussion
Rhinoplasty is the second most common plastic surgery of the face that is routinely performed. Although rhinoplasty is a common procedure to be performed, it should involve delicate and detailed surgical planning as this surgery and the anatomical and aesthetic details play a major role in the facial appearance of a person. Open approach to rhinoplasty does have certain advantages such as detailed and wide exposure of nasal shape defining structures, easy suturing and avoidance of distortion of anatomy for planning the reconstruction along with certain definite disadvantages of a trans-columellar scar, increased chances of post op edema in the tip and dorsum and need of fixation for graft placement which could be done without fixation in the closed technique [9]. Detailed anatomical and anthropometric analysis of dimensions and individualized surgical planning are needs for surgical plan of rhinoplasty. This includes precise planning of the need and amount of cartilage resection, suturing and osteotomies [10] along with consideration of dynamics of nasal anatomy [11, 12].
Open surgical technique does produce increased supra tip edema than closed rhinoplasty [13] but use of both hands for sculpting leads to ease of work and better results in the surgical process [14]. Precise techniques do help in making the columella scar less conspicuous [15]. In this analysis, out of the 29 cases of open rhinoplasty five patients developed edema over the tip; however, those resolved with time. We had to do tip plasty in 14 patients and with open approach, correction of tip was much easier than that of closed approach. Putting a spreader graft (Fig. 4A) helps to prevent narrowing of internal nasal valve, preserve the dorsal aesthetic lines, and stabilize the septum [16, 17]. We had resorted to autologous bony and cartilaginous grafts in view of evidences of lesser complication rates with autologous grafts compared to the synthetic implants. [18] Along with the status of the nasal anatomy, cause of injury is a major concern as sports injuries might require extensive bony work compared to those having developmental etiology. For grade III or IV nasal deformity and for cases of sports injury, help of an imaging computational technique might help in deciding an objectively more precise surgical plan with better results [19, 20].
Three persons in our analysis were not satisfied with the results of the surgery. We consider the reason of dissatisfaction in those three patients to be expectations which were beyond the realistic limitations. Hence we propose preoperative discussion and counseling regarding the realistic expectations is an important factor in improving patient satisfaction with rhinoplasty surgery. Surgery should not be planned in children before completion of the development of facial skeleton. Hence timing of surgery has to be planned and discussed with the patient in detail.
Conclusion
Rhinoplasty is an aesthetic procedure involving finer surgical details and requires good surgical skills and planning. It is the most commonly performed and chosen facial plastic procedure [21]. Otolaryngologists have detailed knowledge of anatomy and physiological dynamics of nose and accordingly should consider each rhinoplasty procedure in accordance with the knowledge of anatomy along with addressing the needs of the patient.
Acknowledgments
Funding
This study is a retrospective chart review and was not funded by any funding agency. There are no financial disclosures to be made by the authors.
Compliance with Ethical Standards
Conflict of interests
We the authors namely, Prof Jaimanti Bakshi and Dr. Sourabha K. Patro declare that we have no conflicts of interests among ourselves.
Ethical Approval
This study being a retrospective chart review of our experience this work is exempted from the ethical committee approval required for any trial on humans. For this type of retrospective study formal consent of institute ethical committee is not required.
Informed Consent
Written informed consent for treatment purposes were obtained from all individual participants who presented to our OPD for rhinoplasty during treatment and surgeries. Additional informed consents were obtained from all individual participants whose identifying information such as photographs have been included in this article.
References
- 1.Sorta-Bilajac I, Muzur A. The nose between ethics and aesthetics: sushruta’s legacy. Otolaryngology–head and neck surgery : official journal of American Academy of Otolaryngology-Head and Neck. Surgery. 2007;137(5):707–710. doi: 10.1016/j.otohns.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 2.Whitaker IS, Karoo RO, Spyrou G, Fenton OM. The birth of plastic surgery: the story of nasal reconstruction from the Edwin Smith Papyrus to the twenty-first century. Plast Reconstr Surg. 2007;120(1):327–336. doi: 10.1097/01.prs.0000264445.76315.6d. [DOI] [PubMed] [Google Scholar]
- 3.Whitaker EG, Johnson CM., Jr The evolution of open structure rhinoplasty. Arch Fac Plast Surg. 2003;5(4):291–300. doi: 10.1001/archfaci.5.4.291. [DOI] [PubMed] [Google Scholar]
- 4.Byrd HS, Hobar PC. Rhinoplasty: a practical guide for surgical planning. Plast Reconstr Surg. 1993;91(4):642–654. doi: 10.1097/00006534-199304000-00011. [DOI] [PubMed] [Google Scholar]
- 5.Oneal RM, Beil RJ, Jr, Schlesinger J. Surgical anatomy of the nose. Clin Plast Surg. 1996;23(2):195–222. [PubMed] [Google Scholar]
- 6.Daniel RK. The nasal tip: anatomy and aesthetics. Plast Reconstr Surg. 1992;89(2):216–224. doi: 10.1097/00006534-199202000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Guyuron B. Precision rhinoplasty. Part I: the role of life-size photographs and soft-tissue cephalometric analysis. Plast Reconstr Surg. 1988;81(4):489–499. doi: 10.1097/00006534-198804000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Zijlker TD, Vuyk H, Adamson PA. Rhinoplasty: preoperative photographic analysis. Clin Otolaryngol Allied Sci. 1992;17(4):361–369. doi: 10.1111/j.1365-2273.1992.tb01014.x. [DOI] [PubMed] [Google Scholar]
- 9.Sajjadian A, Guyuron B. Primary rhinoplasty. Aesthetic Surg J Am Soc Aesthetic Plast Surg. 2010;30(4):527–539. doi: 10.1177/1090820X10380388. [DOI] [PubMed] [Google Scholar]
- 10.Ghanaatpisheh M, Sajjadian A, Daniel RK. Superior rhinoplasty outcomes with precise nasal osteotomy: an individualized approach for maintaining function and achieving aesthetic goals. Aesthetic Surg J Am Soc Aesthetic Plast Surg. 2015;35(1):28–39. doi: 10.1093/asj/sju013. [DOI] [PubMed] [Google Scholar]
- 11.Guyuron B. Dynamic interplays during rhinoplasty. Clin Plast Surg. 1996;23(2):223–231. [PubMed] [Google Scholar]
- 12.Guyuron B. Dynamics in rhinoplasty. Plast Reconstr Surg. 2000;105(6):2257–2259. doi: 10.1097/00006534-200005000-00057. [DOI] [PubMed] [Google Scholar]
- 13.Sporri S, Simmen D, Briner HR, Jones N. Objective assessment of tip projection and the nasolabial angle in rhinoplasty. Arch Fac Plast Surg. 2004;6(5):295–298. doi: 10.1001/archfaci.6.5.295. [DOI] [PubMed] [Google Scholar]
- 14.Petropoulos I, Karagiannidis K, Kontzoglou G. Our experience in open rhinoplasty. Hippokratia. 2007;11(1):35–38. [PMC free article] [PubMed] [Google Scholar]
- 15.Constantian MB. Differing characteristics in 100 consecutive secondary rhinoplasty patients following closed versus open surgical approaches. Plast Reconstr Surg. 2002;109(6):2097–2111. doi: 10.1097/00006534-200205000-00048. [DOI] [PubMed] [Google Scholar]
- 16.Sheen JH. Tip graft: a 20-year retrospective. Plast Reconstr Surg. 1993;91(1):48–63. doi: 10.1097/00006534-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Sajjadian A, Rubinstein R, Naghshineh N. Current status of grafts and implants in rhinoplasty: part I Autologous grafts. Plast Reconstr Surg. 2010;125(2):40e–49e. doi: 10.1097/PRS.0b013e3181c82f12. [DOI] [PubMed] [Google Scholar]
- 18.Lee MR, Unger JG, Rohrich RJ. Management of the nasal dorsum in rhinoplasty: a systematic review of the literature regarding technique, outcomes, and complications. Plast Reconstr Surg. 2011;128(5):538e–550e. doi: 10.1097/PRS.0b013e31822b6a82. [DOI] [PubMed] [Google Scholar]
- 19.Mahajan AY, Shafiei M, Marcus BC. Analysis of patient-determined preoperative computer imaging. Arch Fac Plast Surg. 2009;11(5):290–295. doi: 10.1001/archfacial.2009.61. [DOI] [PubMed] [Google Scholar]
- 20.Mehta U, Mazhar K, Frankel AS. Accuracy of preoperative computer imaging in rhinoplasty. Arch Fac Plast Surg. 2010;12(6):394–398. doi: 10.1001/archfacial.2010.96. [DOI] [PubMed] [Google Scholar]
- 21.Larrabee WF., Jr In praise of rhinoplasty. Arch Fac Plast Surg. 2010;12(6):371–372. doi: 10.1001/archfacial.2010.94. [DOI] [PubMed] [Google Scholar]