Abstract
Although a childhood diagnosis of attention-deficit/hyperactivity disorder (ADHD) is known to be linked to psychotic experiences and psychotic disorders in later life, the developmental trajectories that could explain this association are unknown. Using a sample from the prospective population-based Avon Longitudinal Study of Parents and Children (ALSPAC) (N = 8247), we hypothesized that the previously reported association of ADHD combined subtype in childhood and psychotic experiences in early adolescence is mediated by traumatic events and by involvement in bullying. Moreover, we expected this mediation to be specific to ADHD and tested this by comparison with specific phobia. Children with ADHD combined subtype at age 7 were more often involved in bullying at age 10 (OR 3.635, 95% CI 1.973–6.697) and had more psychotic experiences at age 12 (OR 3.362, 95% CI 1.781–6.348). Moreover, children who were involved in bullying had more psychotic experiences (2.005, 95% CI 1.684–2.388). Bullying was a significant mediator between ADHD and psychotic experiences accounting for 41%–50% of the effect. Traumatic events from birth to age 11 were also significantly associated with ADHD combined subtype and psychotic experiences; however, there was no evidence of mediation. Specific phobia was significantly associated with psychotic experiences, but not with bullying. To conclude, bullying is a relevant translating mechanism from ADHD in childhood to psychotic experiences in early adolescence. Interventions that eliminate bullying in children with ADHD could potentially reduce the risk of having psychotic experiences in later life by up to 50%. Clinicians should thus screen for bullying in routine assessments of children with ADHD.
Keywords: ADHD, risk factor, victimization, aggression, traumatic experiences, ALSPAC
Introduction
Attention-deficit/hyperactivity disorder (ADHD), that is prevalent in approximately 3%–5% of children,1,2 has been found to be a common precursor of psychotic disorders in medical register studies3–5 as well as in retrospective6–9 and prospective studies.10,11 A recent study found childhood ADHD not only to be more frequent in patients with a first-episode psychosis than in the general population but also to predict poorer response to treatment.12 However, the developmental trajectories and mechanisms behind the association between ADHD and psychotic disorders are unknown. Longitudinal designs including mediation analysis can help to shed light on them.
Consistent with traditional developmental models of psychosis,13 our conceptualization is that ADHD represents a risk indicator in the premorbid phase of psychosis that is associated with an increased likelihood of psychotic experiences in the prodrome that in turn precede the full-blown disorder. Despite promising interventions to prevent the “late” transition from the prodrome to the disorder, their outcomes to date are limited and there still is a substantial amount of transition to psychosis.14,15 Therefore, the “early” transition from the premorbid phase to the prodrome is a worthy target of examination.16,17
One possible mediator between ADHD and psychotic experiences is childhood trauma. Children with ADHD are inattentive, impulsive, and have a tendency towards risk and sensation seeking with the consequence that they are more prone to accidents18,19 and to being injured than the general population.20 In a representative study, adults diagnosed with ADHD in childhood retrospectively reported more physical and sexual abuse than adults without ADHD.21 Similarly, posttraumatic stress disorder was more common in adolescents with ADHD than in adolescents without the disorder.22 Childhood trauma is also a common experience in individuals with psychotic disorders.23–25 According to the traumagenic neurodevelopmental model of psychosis, traumatic experiences disturb stress regulation mechanisms and establish an enduring oversensitivity to stress which renders people vulnerable to future psychosis.26,27 Putting the pieces together, ADHD may increase the risk of traumatic experiences in childhood which in turn increases the likelihood of psychotic experiences.
Another possible mediator between ADHD and psychotic experiences is bullying. Compared to their nonaffected peers, children and adolescents with ADHD are more likely to be bullied as well as to bully others.28,29 Factors that contribute to being bullied by peers are being different in some way and having poor relationships with teachers and peers.30 Studies find that children with ADHD are less liked and more often rejected by peers, have fewer close friends, and are more likely to have friends who exhibit deviant behavior.31,32 Having been a victim of bullying in childhood is also frequent in people with psychotic disorders.33,34 Consequences of bulling have been found in emerging psychotic experiences and symptoms, not only in pure victims but also in those who are both victims and perpetrators (bully/victims) and in pure bullies.35–37 Summing up, children with ADHD are more likely to be involved in bullying compared to children without ADHD and children who are involved in bullying are more likely to have psychotic experiences in adolescence.
To conclude, there is evidence that ADHD is associated with trauma and bullying and that trauma and bullying are associated with psychotic experiences. However, so far, no study has tested whether trauma and bullying explain the association between ADHD and psychosis that has been found in previous research. In a prior study on data from the Avon Longitudinal Study of Parents and Children (ALSPAC), we found the combined subtype of ADHD assessed at age 7 to be strongly associated with psychotic experiences at age 12 even when potential confounders and the occurrence of other disorders were controlled for (OR 3.35, 95% CI 1.59–7.07; Hennig et al38). Moreover, although the full range of possible childhood disorders was assessed, the only other comparably frequent childhood disorder significantly associated with psychotic experiences at age 12 after controlling for other disorders was specific phobia.
In the present study, we further investigated the connection between ADHD combined subtype and psychotic experiences by testing whether it is, at least partially, mediated by traumatic experiences or involvement in bullying. As there is evidence that all childhood disorders are associated with an increased risk for psychotic disorders,5 we repeated the analyses with specific phobia to investigate whether the mediation is specific to ADHD or represents a general feature of childhood psychopathology.
Methods
Sample
We analyzed data from participants from the ALSPAC (www.bristol.ac.uk/alspac). Initially, the children from 14541 pregnancies with an expected date of delivery between 1 April 1991 and 31 December 1992 were recruited. These resulted in 14775 live births and 14701 children who were alive at 1 year of age.39 The initial sample was bolstered with eligible cases who had failed to join the study originally, which after 8 years of age resulted in data being available for a total of 15 247 pregnancies. The children and their parents and teachers were followed up over a period of more than 20 years and repeatedly interviewed, tested, and asked to complete questionnaires on developmental and health-related topics. The study website contains details of all the data that are available through a fully searchable data dictionary: http://www.bris.ac.uk/alspac/researchers/data-access/ data-dictionary/. For the present study, all participants with data available on mental disorder status in childhood were selected, resulting in a sample of N = 8247. Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees. Written consent was provided by all participants.
Instruments
Mental Disorders.
When the children were 7.6 years old, the ALSPAC team sent questionnaires from the Development and Well-Being Assessment (DAWBA)40 to carers and teachers. The DAWBA contains closed and open-ended questions that are used to screen mental disorders according to the DSM-IV.41 In an initial evaluation of the answers, a computer algorithm estimated the probability of fit between reported symptoms and disorders as defined by the DSM-IV. Afterwards, trained clinical raters reviewed all information according to a manual, rechecked the results of the computerized evaluation, and finally assigned the diagnoses. Good validity of the diagnoses assigned with the DAWBA has been confirmed.42
Psychotic Experiences.
At the mean age of 12.8 years, participants were interviewed following the semistructured Psychosis-Like Symptom Interview (PLIKS)43 which is based on the Schedule for Clinical Assessment in Neuropsychiatry44 and on the Diagnostic Interview Schedule for Children.45 The interview starts with 6 questions on unusual experiences followed by 11 questions on psychotic experiences covering hallucinations, delusions, and thought interference during the past 6 months. The interrater reliability of the PLIKS has been found to be satisfying43 with κ = 0.72. Trained psychology graduates from the ALSPAC team administered the interviews and rated every experience as not present, suspected, or definitely present, with the latter requiring a concrete example of a clearly psychotic experience. We used the classifications from a prior publication46 on the ALSPAC data. Psychotic experiences were coded as present when at least 1 symptom was rated as suspected or definitely present and the symptoms were not attributable to the effects of sleep or fever.
Traumatic Events.
From study child age 0.5–11.2 years, the carers were sent a total of 14 event-exposure checklists as described in another publication on the ALSPAC data.47 Four checklists were sent when the children were in toddlerhood (age 0.5–2.8 y), 6 in early childhood (age 2.5–6.1 y), and 4 in middle childhood (age 5–11.1 y). From the events in the checklists, severe exposures were identified, namely physical and sexual abuse, death of a parent or sibling, and being taken into care. Following the procedure used in a previous study,47 we composed a binary variable with a traumatic event being coded present vs not present when at least 1 severe exposure was reported from toddlerhood to middle childhood.
Bullying.
At a mean age of 10.7 years, children attended the Bullying and Friendship Interview Schedule (BFIS).48 The children answered 5 questions on whether they had experienced overt bullying (eg, physical aggression) and 4 questions on whether they had experienced relational bullying (eg, exclusion from a group). If they reported bullying, they were also asked if they had only received it (pure victims), or if they had only provided it (pure bullies), or if they had received as well as provided it (bully/victims). We used a derived variable on bullying status that was composed for the ALSPAC data in a previous study.38 Bullying was coded as present when at least 1 experience had occurred 4 or more times in the past 6 months.
Statistical Analyses
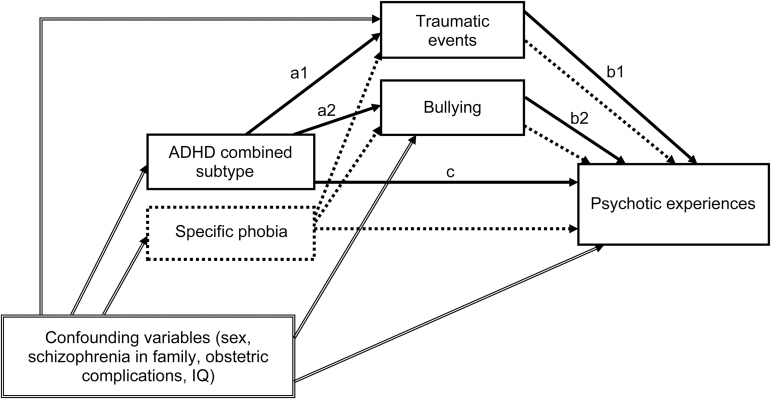
All analyses were carried out using SPSS 24. Figure 1 shows the overall model that was examined. In a first step, we tested bivariate associations between the exposure variable, potential mediators, and the outcome. As all of the variables of interest were dichotomous (present vs not present), we calculated ORs to test the associations between ADHD combined subtype and psychotic experiences (path c), ADHD and traumatic events (path a1), ADHD and bullying (path a2), traumatic events and psychotic experiences (path b1), and bullying and psychotic experiences (path b2). We also calculated adjusted ORs by using logistic regression to control for the influence of sex, schizophrenia in parents or grandparents, maternal diabetes in pregnancy as an indicator of obstetric complications, and IQ49 as these have been found to be associated with ADHD and psychotic disorders.3,11,50,51
Fig. 1.
Examined model of the mediation between ADHD combined subtype and psychotic experiences. ADHD, attention-deficit/hyperactivity disorder.
In a second step, we conducted mediation analyses for those potential mediators that showed significant associations both with the exposure variable and the outcome. The mediation analyses were performed following the principles of Baron and Kenny52 and an extension in regard to dichotomous outcomes.53 The analyses were conducted using an SPSS macro that was developed for this purpose.53 We also conducted additional mediation analyses by adjusting for the abovementioned covariates. Moreover, we calculated the proportion of the mediated effect as an indicator of effect size.54
In a third step, we repeated the analyses with specific phobia instead of ADHD to evaluate whether the effects were specific to ADHD combined or a shared feature of childhood mental disorders.
Results
Participant Characteristics
Participant characteristics are shown in table 1. Complete data were available from 5497 children on DAWBA, PLIKS, and trauma and from 4950 children on DAWBA, PLIKS, and BFIS. Children with incomplete data in the trauma subsample were more likely to be male (OR 1.275, 95% CI 1.163–1.398), affected by a mental disorder (OR 1.255, 95% CI 1.052–1.497), and to be from families receiving income support (OR 2.106, 95% CI 1.730–2.564). Children with incomplete data in the bullying subsample were more likely to be male (1.289, 95% CI 1.179–1.408), affected by a mental disorder (OR 1.423, 95% OR 1.119–1.688), to be from families receiving income support (OR 2.327, 95% CI 1.908–2.837), to be non-White (1.364, 95% CI 1.082–1.720), to have psychotic experiences (OR 1.664, 95% CI 1.312–2.112), and to be affected by ADHD combined subtype (OR 1.772, 95% CI 1.139–2.755).
Table 1.
Participant Characteristics
| Characteristics and Measures | n | % |
|---|---|---|
| Female | 4005 | 48.6 |
| Non-White | 301 | 3.6 |
| Urban upbringing | 7031 | 85.3 |
| Parent or grandparent with schizophrenia | 103 | 1.2 |
| Diabetes in pregnancy | 105 | 1.3 |
| Family receiving income support | 493 | 6.0 |
| Highest maternal education | ||
| CSE | 848 | 11.0 |
| Vocational | 712 | 9.3 |
| O-level | 2800 | 36.5 |
| A-level | 2050 | 26.7 |
| University degree | 1271 | 16.5 |
| IQ (M, SD) | 105.14 | 16.27 |
| DAWBA | 8247 | |
| ADHD | 175 | 2.1 |
| Inattentive subtype | 70 | 0.9 |
| Hyperactive-impulsive subtype | 25 | 0.3 |
| Combined subtype | 80 | 1.0 |
| Specific phobia | 86 | 1.0 |
| Number of disorders | ||
| 0 | 7649 | 92.7 |
| 1 | 448 | 5.4 |
| 2 | 122 | 1.5 |
| 3 | 25 | 0.3 |
| >3 | 13 | 0.2 |
| Traumatic event | 5467 | |
| Present | 345 | 6.3 |
| BFIS | 7248 | |
| Overt bullying | 1627 | 22.4 |
| Pure bully | 67 | 0.9 |
| Pure victim | 1183 | 16.3 |
| Bully/victim | 377 | 5.2 |
| Neutral | 5621 | 77.6 |
| Relational bullying | 592 | 8.2 |
| Pure bully | 20 | 0.3 |
| Pure victim | 519 | 7.2 |
| Bully/victim | 53 | 0.7 |
| Neutral | 6632 | 91.8 |
| PLIKS | 6792 | |
| Psychotic experiences | 786 | 11.6 |
| Suspected | 467 | 6.9 |
| Definite | 319 | 4.7 |
Note: A-level, advanced level; CSE, certificate of secondary education; O-level, ordinary level. ADHD, attention-deficit/hyperactivity disorder; BFIS, Bullying and Friendship Interview Schedule; DAWBA, Development and Well-Being Assessment; PLIKS, Psychosis-Like Symptom Interview.
Bivariate Comparisons
As can be seen from table 2, the bivariate associations between all variables were significant. Children with ADHD combined subtype compared to children without had a more than 3-fold increased risk of psychotic experiences at age 12 (OR 3.362, 95% CI 1.781–6.348; path c). Moreover, children with ADHD combined subtype had a 2-fold risk of experiencing a traumatic event (OR 2.199, 95% CI 1.119–4.325; path a1) and a more than 3-fold risk of being involved in bullying (OR 3.635, 95% CI 1.973–6.697; path a2). Children who experienced a traumatic event compared to those who did not had an increased risk of psychotic experiences at age 12 (OR 1.567, 95% CI 1.187–2.068; path b1) and children who were involved in bullying compared to those who were not had a 2-fold risk of psychotic experiences at age 12 (OR 2.005, 95% CI 1.684–2.388; path b2).
Table 2.
Associations of ADHD Combined Subtype, Traumatic Events, Bullying, and Psychotic Experiences
| Path/Exposure | Outcome | OR | Adjusted ORa | |||
|---|---|---|---|---|---|---|
| Path c | Psychotic Experiences | |||||
| No | Yes | Total | 3.257 (1.738, 6.103) | 3.362 (1.781, 6.348) | ||
| ADHD combined subtype | No | 4856 | 614 | 5470 | ||
| Yes | 34 | 14 | 48 | |||
| Total | 4890 | 628 | 5518 | |||
| Path a1 | Traumatic Events | |||||
| No | Yes | Total | 2.202 (1.127, 4.304) | 2.199 (1.119, 4.325) | ||
| ADHD combined subtype | No | 7563 | 505 | 8068 | ||
| Yes | 68 | 10 | 78 | |||
| Total | 7631 | 515 | 8146 | |||
| Path a2 | Bullying | |||||
| No | Yes | Total | 4.558 (2.491, 8.339) | 3.635 (1.973, 6.697) | ||
| ADHD combined subtype | No | 4320 | 1369 | 5689 | ||
| Yes | 18 | 26 | 44 | |||
| Total | 4338 | 1395 | 5733 | |||
| Path b1 | Psychotic Experiences | |||||
| No | Yes | Total | 1.592 (1.208, 2.099) | 1.567 (1.187, 2.068) | ||
| Traumatic events | No | 5311 | 663 | 5974 | ||
| Yes | 332 | 66 | 398 | |||
| Total | 5643 | 729 | 6372 | |||
| Path b2 | Psychotic Experiences | |||||
| No | Yes | Total | 2.019 (1.699, 2.401) | 2.005 (1.684, 2.388) | ||
| Bullying | No | 4083 | 403 | 4486 | ||
| Yes | 1189 | 237 | 1426 | |||
| Total | 5272 | 640 | 5912 | |||
Note: ADHD, attention-deficit/hyperactivity disorder. Numbers in brackets are 95% CIs of the estimates.
aAdjusted for sex, schizophrenia in parent or grandparent, maternal diabetes in pregnancy, and IQ.
Mediation Analyses
Five or fewer (exact cells counts below 5 cannot be given due to ALSPAC privacy protection regulations) of the children who fulfilled criteria for both ADHD combined subtype and psychotic experiences also had a traumatic experience. As shown in table 3, there was no evidence of mediation through traumatic events as the indirect effect (path a1–b1) was not significant. Nine of the 14 (64.3%) children with both ADHD combined subtype and psychotic experiences were also involved in bullying. There was evidence of mediation through bullying as the indirect effect (path a2–b2) was significant. When the mediating effect of bullying was controlled for, ADHD no longer had an effect on psychotic experiences as indicated by the nonsignificant controlled direct effect. The proportion of mediated effect through bullying was 49.72% in the model without covariates and 41.28% in the adjusted model. However, there was only a trend effect (P = .060) for the significance of the indirect effect in the second mediation model that was adjusted for confounders.
Table 3.
Direct and Indirect Effects of ADHD Combined Subtype on Psychotic Experiences Mediated by Traumatic Events and Bullying
| Traumatic Eventsa (Path a1–b1) | Bullyingb (Path a2–b2) | |||||||
|---|---|---|---|---|---|---|---|---|
| Effects | Estimates | P | Adjusted Estimatesc | P | Estimates | P | Adjusted Estimatesc | P |
| Direct | 3.381 (1.766, 6.472) | <.001 | 3.643 (1.828,7.260) | <.001 | 3.054 (1.455, 6.411) | .003 | 3.516 (1.663, 7.430) | <.001 |
| Indirect | 0.996 (0.892, 1.111) | .938 | 0.994 (0.893, 1.107) | .915 | 1.665 (1.053, 2.635) | .029 | 1.503 (0.983, 2.297) | .060 |
| Controlled direct | 3.491 (1.765, 6.472) | <.001 | 3.643 (1.828,7.260) | <.001 | 2.092 (0.602, 7.263) | .245 | 2.172 (0.621, 7.596) | .224 |
| Total | 3.366 (1.789, 6.336) | <.001 | 3.510 (1.850, 6.659) | <.001 | 5.087 (2.240, 11.550) | <.001 | 5.283 (2.335, 11.953) | <.001 |
Note: ADHD, attention-deficit/hyperactivity disorder. Numbers in brackets are 95% CIs of the estimates.
aBased on n = 5497 complete cases.
bBased on n = 4950 complete cases.
cAdjusted for sex, schizophrenia in parent or grandparent, maternal diabetes in pregnancy, and IQ.
We conducted additional exploratory analyses to investigate which confounder was responsible for the reduction in the indirect effects. Adjusting for any single confounder or any combination of confounders without sex resulted in the significant indirect effect. However, adjusting for sex along with any other confounder reduced the indirect effect to trend level, indicating that sex was the most influential confounder to the mediation. As there were fewer females than males among the 9 children affected by all 3 conditions (ADHD combined subtype, bullying, and psychotic experiences), we repeated the adjusted mediation analysis with boys only and found the indirect effect to be significant.
Comparison With Specific Phobia
As can be seen from table 4, children with specific phobia compared to children without had a more than 2-fold increased risk of psychotic experiences at age 12 (OR 2.217, 95% CI 1.155–4.259). However, they did not have a significantly increased risk of being involved in bullying (OR 1.231, 95% CI 0.666–2.275).
Table 4.
Associations of Specific Phobia, Bullying, and Psychotic Experiences
| Exposure | Outcome | OR | Adjusted ORa | |||
|---|---|---|---|---|---|---|
| Psychotic Experiences | ||||||
| No | Yes | Total | 2.288 (1.196, 4.376) | 2.217 (1.155, 4.259) | ||
| Specific phobia | No | 4854 | 621 | 5475 | ||
| Yes | 41 | 12 | 53 | |||
| Total | 4895 | 633 | 5528 | |||
| Bullying | ||||||
| No | Yes | Total | 1.336 (0.728, 2.454) | 1.231 (0.666, 2.275) | ||
| Specific phobia | No | 4309 | 1382 | 5691 | ||
| Yes | 35 | 15 | 50 | |||
| Total | 4344 | 1397 | 5741 | |||
Note: Numbers in brackets are 95% confidence intervals of the estimates.
aAdjusted for sex, schizophrenia in parent or grandparent, maternal diabetes in pregnancy, and IQ.
Discussion
As expected, ADHD combined subtype at age 7 was significantly associated with bullying at age 10 and bullying was significantly associated with psychotic experiences at age 12. These bivariate associations were not just due to the children’s sex, IQ, or indicators of genetic liability and obstetric complications. In line with our expectations, bullying significantly mediated between ADHD and psychotic experiences, accounting for up to half of the effect. By controlling for confounders, we aimed to further corroborate the postulated causal pathways. Although the model adjusting for sex reduced the indirect effect to trend level, this indirect path nevertheless rendered the direct path insignificant, indicating mediation. Moreover, the indirect effect was significant when analyzing the boys only. As there were very few girls with ADHD who had experienced both bullying and psychotic experiences, no meaningful analyses could be conducted for the subsample of girls. Thus, we need to remain open to the possibility that being involved in bullying as an explanation for the trajectory from ADHD to psychosis could be restricted to boys who more likely are to be affected by ADHD combined subtype.1
Specific phobia at age 7 was significantly associated with psychotic experiences at age 12, but not with bullying at age 10, thus, there was no evidence of mediation. Specific phobia was the only disorder at age 7 that was significantly correlated with psychotic experiences at age 12 aside from pervasive developmental disorder that was too rare to include it into the analysis.38 Thus, our findings indicate that the mediation through bullying could be specific to ADHD. Nevertheless, the question of specificity needs further investigation in other, and if possible larger, samples, before firm conclusions can be drawn.
ADHD combined subtype was also significantly associated with the occurrence of a traumatic event between birth and age 11 and traumatic events were significantly associated with psychotic experiences at age 12. Again, these associations were not explicable by potential confounders. In contrast to our expectation, we did not find evidence of mediation between ADHD combined subtype and psychotic experiences through traumatic events. This seems to indicate that ADHD and traumatic events have independent influences on psychotic experiences. However, as the numbers in the cells were small, there may be a small mediation effect that can only be detected in larger samples. Moreover, we cannot rule out the possibility that early traumatic experiences, that occurred prior to the assessment of ADHD at age 7, contributed to the development of ADHD and not vice versa. As the combination of ADHD combined subtype and traumatic events between 0.5 to 11.1 years was rare, we could not further subdivide the age span in order to focus exclusively on traumatic events in middle childhood.
This study is the first to show that bullying mediates between ADHD combined subtype in childhood and psychotic experiences in early adolescence. There are several possible mechanisms for the mediating role of bullying: Children with ADHD tend to be impulsive and strive for immediate rewards. Bullying might serve to directly satisfy their needs and induce a feeling of power and peer regard they cannot attain in a socially acceptable way. In the long term, however, children who bully others fail to establish positive social relationships and are at an increased risk of various adversities including criminality and drug misuse.55 Children with ADHD are also more likely to become victims of bullying as they lack friends31,32 who could help them to defend themselves against being bullied. Consistent with cognitive models of delusions,56,57 social exclusion promotes the manifestation of psychotic ideas due to a lack of social correction to misinterpretations of anomalous experiences. This process is accompanied by feelings of anxiety, depression, and negative beliefs about oneself that have also been found to mediate between bullying and psychotic experiences.58 To conclude, we assume that social exclusion along with negative affect and dysfunctional self-related beliefs are key mechanisms in translating ADHD to psychotic experiences.
Based on our findings, we expect the prevention of bullying to reduce the risk of psychotic experiences in children with ADHD combined subtype by up to 50%. Even though most adolescents with psychotic experiences do not develop psychotic disorders in later life,46,59 our finding is clinically relevant because psychotic experiences nevertheless represent one of the strongest risk factor for psychosis we know of so far.46,60 Moreover, there is evidence that the occurrence of psychotic experiences is not only a specific risk factor for psychotic disorders but also a general risk indicator of nonpsychotic disorders.61,62
In contrast to genetic or biological influences, bullying is susceptible to psychological and psychosocial treatment. Interventions to prevent bullying should be implemented at the school, class, and individual level and include parents, teachers, and peers.63 There is evidence that training teachers to improve the peer regard of children with ADHD can ameliorate social problems64 and thus might be a promising intervention to prevent bullying. This approach might not only prevent students from bulling their classmates with ADHD but also prevent children with ADHD from bulling their peers in order to achieve peer regard.
Limitations
Three limitations regarding our study should be mentioned: First, it is reasonable to assume that more children experienced a traumatic event than were identified, because only children’s carers were asked. Sexual abuse frequently takes place within the family environment65 and carers are unlikely to report events they were involved in themselves. Moreover, children might not have reported all incidents to their carers as traumatic events are often accompanied by feelings of shame and self-blame.65
Second, there was attrition from the assessments at age 7–12. There was more missing data in children with ADHD combined subtype and psychotic experiences who as a consequence were underrepresented in the bullying mediation analysis. As ADHD combined subtype and psychotic experiences were the variables of interest, the power of the analysis was thus reduced and the effect might be underestimated. Despite this selective drop out and the resulting reduction of statistical power, we found the hypothesized mediation effect for bullying. Moreover, a simulation study of the ALSPAC data found that even though there was selective drop out, the validity of regression models was only marginally affected.66 It would have been interesting to additionally include ALSPAC data from a second assessment of psychotic experiences conducted at age 18. However, there was substantial selective drop out for this time-point that made meaningful analyses impossible.
Third, we cannot rule out that psychotic experiences preceded ADHD and bullying. However, the pathway we postulated is in line with generally accepted developmental models of psychopathology. ADHD is thought of as a neurodevelopmental disorder with strong genetic and biological underpinnings that are expressed early in behavioral symptoms.67 Consistent with the pathway proposed by us, there is evidence that bullying contributes to psychotic experiences even when previous psychotic experiences are controlled for.68 We also planned to examine the impact of the bullying role (ie, pure bully vs pure victim vs bully/victim) on the mediation. However, the cell counts were too small—especially for pure bullies—to perform this type of analysis. Future research should investigate the relevance of the bullying role as there is evidence that bullies, victims, and bully/victims differ in their adult psychopathological outcomes.55
Conclusions
Our findings corroborate the notion that bullying is a central translating mechanism between ADHD and psychotic experiences that in turn are risk indicators for psychotic and nonpsychotic disorders. Thus, in agreement with other researches,69 we suggest that healthcare professionals are well advised to include screening and interventions aimed at bullying in their routine assessments and treatment of children with ADHD. In addition, schools and other social institutions should engage more strongly in protecting children from bullying and other forms of aggression from an early age on in order to prevent serious consequences on mental health and well-being.70,71
Funding
The UK Medical Research Council and the Wellcome Trust (grant ref: 102215/2/13/2) and the University of Bristol provided core support for ALSPAC. E.S.J. received a research grant from the German Academic Exchange Service (DAAD, 91540971).
Acknowledgments
We are grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses. This publication is the work of the authors and all the authors will serve as guarantors for the contents of this paper. The authors like to thank the researchers who provided their derived variables on the ALSPAC data37,46,47 and Linda Valeri for her support with the mediation macro. The authors declare no conflict of interest associated with the manuscript.
References
- 1. Willcutt EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 2012;9:490–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. 2015;56:345–365. [DOI] [PubMed] [Google Scholar]
- 3. Larsson H, Rydén E, Boman M, Långström N, Lichtenstein P, Landén M. Risk of bipolar disorder and schizophrenia in relatives of people with attention-deficit hyperactivity disorder. Br J Psychiatry. 2013;203:103–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chen MH, Wei HT, Chen LC, et al. Autistic spectrum disorder, attention deficit hyperactivity disorder, and psychiatric comorbidities: a nationwide study. Res Autism Spectr Disord. 2015;10:1–6. [Google Scholar]
- 5. Maibing CF, Pedersen CB, Benros ME, Mortensen PB, Dalsgaard S, Nordentoft M. Risk of schizophrenia increases after all child and adolescent psychiatric disorders: a nationwide study. Schizophr Bull. 2015;41:963–970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alaghband-Rad J, McKenna K, Gordon CT, et al. Childhood-onset schizophrenia: the severity of premorbid course. J Am Acad Child Adolesc Psychiatry. 1995;34:1273–1283. [DOI] [PubMed] [Google Scholar]
- 7. Dalteg A, Zandelin A, Tuninger E, Levander S. Psychosis in adulthood is associated with high rates of ADHD and CD problems during childhood. Nord J Psychiatry. 2014;68:560–566. [DOI] [PubMed] [Google Scholar]
- 8. Rubino IA, Frank E, Croce Nanni R, Pozzi D, Lanza di Scalea T, Siracusano A. A comparative study of axis I antecedents before age 18 of unipolar depression, bipolar disorder and schizophrenia. Psychopathology. 2009;42:325–332. [DOI] [PubMed] [Google Scholar]
- 9. Elman I, Sigler M, Kronenberg J, et al. Characteristics of patients with schizophrenia successive to childhood attention deficit hyperactivity disorder (ADHD). Isr J Psychiatry Relat Sci. 1998;35:280–286. [PubMed] [Google Scholar]
- 10. Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. 2003;60:709–717. [DOI] [PubMed] [Google Scholar]
- 11. Dalsgaard S, Mortensen PB, Frydenberg M, Maibing CM, Nordentoft M, Thomsen PH. Association between attention-deficit hyperactivity disorder in childhood and schizophrenia later in adulthood. Eur Psychiatry. 2014;29:259–263. [DOI] [PubMed] [Google Scholar]
- 12. Rho A, Traicu A, Lepage M, Iyer SN, Malla A, Joober R. Clinical and functional implications of a history of childhood ADHD in first-episode psychosis. Schizophr Res. 2015;165:128–133. [DOI] [PubMed] [Google Scholar]
- 13. McGlashan TH, Johannessen JO. Early detection and intervention with schizophrenia: rationale. Schizophr Bull. 1996;22:201–222. [DOI] [PubMed] [Google Scholar]
- 14. van der Gaag M, Smit F, Bechdolf A, et al. Preventing a first episode of psychosis: meta-analysis of randomized controlled prevention trials of 12 month and longer-term follow-ups. Schizophr Res. 2013;149:56–62. [DOI] [PubMed] [Google Scholar]
- 15. National Institute for Health and Care Excellence. Psychosis and Schizophrenia in Children and Young People. London: The British Psychological Society and The Royal College of Psychiatrists; 2013. [Google Scholar]
- 16. Keshavan MS, DeLisi LE, Seidman LJ. Early and broadly defined psychosis risk mental states. Schizophr Res. 2011;126:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Seidman LJ, Nordentoft M. New targets for prevention of schizophrenia: is it time for interventions in the premorbid phase? Schizophr Bull. 2015;41:795–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pastor PN, Reuben CA. Identified attention-deficit/hyperactivity disorder and medically attended, nonfatal injuries: US school-age children, 1997-2002. Ambul Pediatr. 2006;6:38–44. [DOI] [PubMed] [Google Scholar]
- 19. Tai YM, Gau SS, Gau CS. Injury-proneness of youth with attention-deficit hyperactivity disorder: a national clinical data analysis in Taiwan. Res Dev Disabil. 2013;34:1100–1108. [DOI] [PubMed] [Google Scholar]
- 20. Chou IC, Lin CC, Sung FC, Kao CH. Attention-deficit-hyperactivity disorder increases risk of bone fracture: a population-based cohort study. Dev Med Child Neurol. 2014;56:1111–1116. [DOI] [PubMed] [Google Scholar]
- 21. Fuller-Thomson E, Lewis DA. The relationship between early adversities and attention-deficit/hyperactivity disorder. Child Abuse Negl. 2015;47:94–101. [DOI] [PubMed] [Google Scholar]
- 22. Biederman J, Petty CR, Spencer TJ, et al. Examining the nature of the comorbidity between pediatric attention deficit/hyperactivity disorder and post-traumatic stress disorder. Acta Psychiatr Scand. 2013;128:78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. van Dam DS, van Nierop M, Viechtbauer W, et al. Childhood abuse and neglect in relation to the presence and persistence of psychotic and depressive symptomatology. Psychol Med. 2015;45:1363–1377. [DOI] [PubMed] [Google Scholar]
- 25. Muenzenmaier KH, Seixas AA, Schneeberger AR, Castille DM, Battaglia J, Link BG. Cumulative effects of stressful childhood experiences on delusions and hallucinations. J Trauma Dissociation. 2015;16:442–462. [DOI] [PubMed] [Google Scholar]
- 26. Read J, Fosse R, Moskowitz A, Perry B. The traumagenic neurodevelopmental model of psychosis revisited. Neuropsychiatry. 2014;4:65–79. [Google Scholar]
- 27. Read J, Perry BD, Moskowitz A, Connolly J. The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry. 2001;64:319–345. [DOI] [PubMed] [Google Scholar]
- 28. Holmberg K, Hjern A. Bullying and attention-deficit- hyperactivity disorder in 10-year-olds in a Swedish community. Dev Med Child Neurol. 2008;50:134–138. [DOI] [PubMed] [Google Scholar]
- 29. Chou W-J, Liu T-L, Yang P, Yen C-F, Hu H-F. Bullying victimization and perpetration and their correlates in adolescents clinically diagnosed with ADHD [published online ahead of print November 17, 2014]. J Atten Disord. doi: 10.1177/1087054714558874. [DOI] [PubMed] [Google Scholar]
- 30. Brock SE, Nickerson AB, O’Malley MD, Chang Y. Understanding children victimized by their peers. J Sch Violence. 2006;5:3–18. [Google Scholar]
- 31. Normand S, Schneider BH, Lee MD, Maisonneuve MF, Kuehn SM, Robaey P. How do children with ADHD (mis)manage their real-life dyadic friendships? A multi-method investigation. J Abnorm Child Psychol. 2011;39:293–305. [DOI] [PubMed] [Google Scholar]
- 32. Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA. What aspects of peer relationships are impaired in children with attention-deficit/hyperactivity disorder? J Consult Clin Psychol. 2005;73:411–423. [DOI] [PubMed] [Google Scholar]
- 33. Trotta A, Di Forti M, Mondelli V, et al. Prevalence of bullying victimisation amongst first-episode psychosis patients and unaffected controls. Schizophr Res. 2013;150:169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Catone G, Marwaha S, Kuipers E, et al. Bullying victimisation and risk of psychotic phenomena: analyses of British national survey data. Lancet Psychiatry. 2015;2:618–624. [DOI] [PubMed] [Google Scholar]
- 35. Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kelleher I, Harley M, Lynch F, Arseneault L, Fitzpatrick C, Cannon M. Associations between childhood trauma, bullying and psychotic symptoms among a school-based adolescent sample. Br J Psychiatry. 2008;193:378–382. [DOI] [PubMed] [Google Scholar]
- 37. Wolke D, Lereya ST, Fisher HL, Lewis G, Zammit S. Bullying in elementary school and psychotic experiences at 18 years: a longitudinal, population-based cohort study. Psychol Med. 2014;44:2199–2211. [DOI] [PubMed] [Google Scholar]
- 38. Hennig T, Jaya ES, Koglin U, Lincoln TM. Associations of attention-deficit/hyperactivity and other childhood disorders with psychotic experiences and disorders in adolescence [published online ahead of print September 13, 2016]. Eur Child Adolesc Psychiatry. doi: 10.1007/s00787-016-0904-8. [DOI] [PubMed] [Google Scholar]
- 39. Boyd A, Golding J, Macleod J, et al. Cohort profile: the ‘children of the 90s’–the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol. 2013;42:111–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41:645–655. [PubMed] [Google Scholar]
- 41. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV. Washington, DC: APA; 1994. [Google Scholar]
- 42. Goodman A, Heiervang E, Collishaw S, Goodman R. The ‘DAWBA bands’ as an ordered-categorical measure of child mental health: description and validation in British and Norwegian samples. Soc Psychiatry Psychiatr Epidemiol. 2011;46:521–532. [DOI] [PubMed] [Google Scholar]
- 43. Horwood J, Salvi G, Thomas K, et al. IQ and non-clinical psychotic symptoms in 12-year-olds: results from the ALSPAC birth cohort. Br J Psychiatry. 2008;193:185–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. World Health Organization. Schedules for Clinical Assessment in Neuropsychiatry. Washington, DC: American Psychiatric Research; 1994. [Google Scholar]
- 45. Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. [DOI] [PubMed] [Google Scholar]
- 46. Zammit S, Kounali D, Cannon M, et al. Psychotic experiences and psychotic disorders at age 18 in relation to psychotic experiences at age 12 in a longitudinal population-based cohort study. Am J Psychiatry. 2013;170:742–750. [DOI] [PubMed] [Google Scholar]
- 47. Crane C, Heron J, Gunnell D, Lewis G, Evans J, Williams JM. Childhood traumatic events and adolescent overgeneral autobiographical memory: findings in a U.K. cohort. J Behav Ther Exp Psychiatry. 2014;45:330–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wolke D, Schreier A, Zanarini MC, Winsper C. Bullied by peers in childhood and borderline personality symptoms at 11 years of age: a prospective study. J Child Psychol Psychiatry. 2012;53:846–855. [DOI] [PubMed] [Google Scholar]
- 49. Wechsler D, Golombok S, Rust J. Wechsler Intelligence Scale for Children (WISC-IIIUK). Sidcup, UK: The Psychological Corporation; 1992. [Google Scholar]
- 50. Peralta V, de Jalón EG, Campos MS, Zandio M, Sanchez-Torres A, Cuesta MJ. The meaning of childhood attention-deficit hyperactivity symptoms in patients with a first-episode of schizophrenia-spectrum psychosis. Schizophr Res. 2011;126:28–35. [DOI] [PubMed] [Google Scholar]
- 51. Hickie IB, Hermens DF, Naismith SL, et al. Evaluating differential developmental trajectories to adolescent-onset mood and psychotic disorders. BMC Psychiatry. 2013;13:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. [DOI] [PubMed] [Google Scholar]
- 53. Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18:137–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. VanderWeele TJ, Vansteelandt S. VanderWeele and Vansteelandt respond to “decomposing with a lot of supposing” and “mediation”. Am J Epidemiol. 2010;172:1355–1356. [Google Scholar]
- 55. Klomek AB, Sourander A, Elonheimo H. Bullying by peers in childhood and effects on psychopathology, suicidality, and criminality in adulthood. Lancet Psychiatry. 2015;2:930–941. [DOI] [PubMed] [Google Scholar]
- 56. Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41:331–347. [DOI] [PubMed] [Google Scholar]
- 57. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. [DOI] [PubMed] [Google Scholar]
- 58. Fisher HL, Schreier A, Zammit S, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr Bull. 2013;39:1045–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43:1133–1149. [DOI] [PubMed] [Google Scholar]
- 60. Kaymaz N, Drukker M, Lieb R, et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med. 2012;42:2239–2253. [DOI] [PubMed] [Google Scholar]
- 61. Kelleher I, Keeley H, Corcoran P, et al. Clinicopathological significance of psychotic experiences in non-psychotic young people: evidence from four population-based studies. Br J Psychiatry. 2012;201:26–32. [DOI] [PubMed] [Google Scholar]
- 62. Fusar-Poli P, Yung AR, McGorry P, van Os J. Lessons learned from the psychosis high-risk state: towards a general staging model of prodromal intervention. Psychol Med. 2014;44:17–24. [DOI] [PubMed] [Google Scholar]
- 63. Leff SS, Waasdorp TE. Effect of aggression and bullying on children and adolescents: implications for prevention and intervention. Curr Psychiatry Rep. 2013;15:343. [DOI] [PubMed] [Google Scholar]
- 64. Mikami AY, Griggs MS, Lerner MD, et al. A randomized trial of a classroom intervention to increase peers’ social inclusion of children with attention-deficit/hyperactivity disorder. J Consult Clin Psychol. 2013;81:100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Pinheiro P. World Report on Violence Against Children. Geneva, Switzerland: United Nations; 2006. [Google Scholar]
- 66. Wolke D, Waylen A, Samara M, et al. Selective drop-out in longitudinal studies and non-biased prediction of behaviour disorders. Br J Psychiatry. 2009;195:249–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 68. Kelleher I, Keeley H, Corcoran P, et al. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013;170:734–741. [DOI] [PubMed] [Google Scholar]
- 69. Holmberg K. The association of bullying and health complaints in children with attention-deficit/hyperactivity disorder. Postgrad Med. 2010;122:62–68. [DOI] [PubMed] [Google Scholar]
- 70. Halpern J, Jutte D, Colby J, Boyce WT. Social dominance, school bullying, and child health: what are our ethical obligations to the very young? Pediatrics. 2015;135(suppl 2):S24–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Arseneault L, Bowes L, Shakoor S. Bullying victimization in youths and mental health problems: ‘much ado about nothing’? Psychol Med. 2010;40:717–729. [DOI] [PubMed] [Google Scholar]