Abstract
Introduction
The mechanism linking childhood trauma (CT) to the functional deficits observed in early psychosis (EP) patients is as yet unknown. We aim to examine the potential mediating effect of depressive symptoms in this well-established association.
Methods
Two hundred nine EP subjects aged 18–35 were assessed for functioning and psychopathology after 2, 6, 12, 18, 24, 30, and 36 months of treatment. Patients were classified into early trauma if they had faced at least one experience of abuse (physical, sexual, or emotional) or neglect (physical or emotional) before age 12, and late trauma if the exposure had occurred between ages 12 and 16. Diagnosis was based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition). Psychopathology was assessed with the Positive and Negative Syndrome Scale and the Montgomery-Asberg Depression Rating Scale. Functioning was measured with the Global Assessment of Functioning (GAF) and the Social and Occupational Functioning Assessment Scale (SOFAS). Mediation analyses were performed in order to study whether the relationship between CT and functioning was mediated by depressive symptoms.
Results
When compared with nonexposed patients, early but not late trauma patients showed lower levels of GAF and SOFAS scores over all the time points, excepting after the first assessment. After 30 and 36 months, the effect of early trauma on functioning was completely mediated by depressive symptoms. No mediating effect of positive or negative symptoms was highlighted at those time points.
Conclusion
Mild depressive symptoms mediated the impact of early trauma on long-term functional outcome. Intensifying pharmacologic and/or psychotherapeutic treatment, focused on the depressive dimension, may help traumatized EP patients to improve their functioning.
Keywords: childhood trauma, first episode psychosis, psychopathology, depression, functional outcome, mediation, prospective
Introduction
Functional impairment can be observed at all stages of psychotic disorders and remains a major challenge for treatment.1 Currently, available medication have significant impact on positive symptoms, but improvement in this domain unfortunately do not correlate well with functional recovery.2–4 Functional impairment is a broad term that covers activities of daily living, vocational activities, social relationships, and degree of independence; it is a key element of outcome in psychotic disorders which greatly impacts the burden of social disability.5,6 We therefore need to develop a better understanding of the mechanisms contributing to these impairments, in order to improve current treatments. This remains one of the most difficult challenges for clinicians in this field.7
Recent research suggests that exposure to childhood trauma (CT) is a potential determinant of functional impairments in both chronic8,9 and first episode of psychosis (FEP) patients.10,11 Previous research has suggested that a better understanding of the psychological processes that link social adversity with functional impairments could provide new insights, with possible therapeutic implications.12 Along these lines, it has been recently suggested that so-called “ancillary symptoms”13 of psychosis (depression, anxiety, dissociation) might operate as mediators between social risk factors and psychotic symptoms, thus providing targets for psychological therapy in psychosis.14–19 None of these studies, however, do comment on how social environmental risk factors lead to functional impairments in psychotic patients. Exploring potential mediators between CT and this important outcome may pave the way for helpful interventions in this domain.
Some studies in psychotic patients have linked CT to higher depressive symptoms,20,21 full-blown depression22–24 and to a lack of response or remission in depression during psychotherapeutic and pharmacological treatments.25 On the other hand, literature has shown that patients suffering from schizophrenia with concurrent depressive symptoms have poorer long-term functional outcomes compared to nondepressed patients,26 and that depressive symptoms are indicator of poor prognosis regarding recovery and integration in the community.27 Connecting these findings with previous considerations highlighting the potential mediating role of “ancillary symptoms” in the psychotic processes,13 we hypothesize that depressive symptoms may also operate as mediators between CT and functional deficits in patients suffering from psychosis.
A recently published article by Palmier-Claus et al.,28 explored this question in a sample of 44 patients. Its results suggest that childhood adversity acts on social functioning by increasing levels of depression, which is in line with our hypothesis. However, in addition to its limited sample size, this study was performed in a heterogeneous sample combining ultra high risk, FEP, and chronic patients. Moreover, its cross-sectional and retrospective design did not enable exploration of the dynamic aspects of this interaction. These factors limit the conclusiveness of these promising results, which therefore need to be replicated in a larger, prospective, and more homogeneous sample of EP patients.
Based on these elements we hypothesized, in a sample of 209 EP patients treated in a specialized program for 3 years, that severity of depressive symptoms would mediate the impact of CT on the functional level of patients at different time points of the follow-up. We have recently shown that only patients exposed to trauma before the age of 12 (and not later) show functional impairments during the three years of follow-up compared to nonexposed patients.12 According to these findings, we also stratified patients according to their age at the time of exposure to the initial traumatic event.
Methods
Procedure and Subjects
TIPP (Treatment and Early Intervention in Psychosis Program), a specialized early psychosis program, was launched in 2004 at the Department of Psychiatry CHUV, in Lausanne, Switzerland.29,30 Entry criteria to the program are: (I) age between 18 and 35; (II) residing in the catchment area (Lausanne and surroundings; population about 300000); (III) meeting threshold criteria for psychosis, as defined by the “Psychosis threshold” subscale of the Comprehensive Assessment of At Risk Mental States (CAARMS31) Scale. Patients are referred to other treatment programs if they have been taking antipsychotic medication for more than a total of 6 months, have psychosis related to intoxication or organic brain disease, or have an intelligence quotient below 70. In the TIPP program, each patient is followed up by a psychiatrist and a Case manager. The program offers an integrated bio-psycho-social treatment based on psychotherapy, psycho-education, family support, cognitive assessment and remediation (when needed), social support, assistance in finding employment, psychological interventions for cannabis use, and pharmacological treatment. The last is applied based on international guidelines and favors atypical antipsychotic. Any side effects due to medication are prospectively monitored.30
A specially designed questionnaire is completed for all patients enrolled in the program by their case managers who have up to one hundred instances of contact with patients during the 3 years of treatment. It assesses demographic characteristics, past medical history, exposure to life events as well as symptoms and functioning. It is completed on the basis of information gathered with patients and their family over the first few weeks of treatment and can be updated during follow-up if new information emerges. Follow-up assessments, exploring various aspects of treatment and co-morbidities (such as the level of insight; the treatment adherence; the presence or absence of forensic history and substance use; intermittent exposure to trauma; suicide attempts; and forensic events) as well as evolution of psychopathology and functional level, are conducted by a research psychologist (for psychopathology) and by case managers (for functional measures) after 2, 6, 12, 18, 24, 30, and 36 months of treatment.
The Research and Ethics Committee of the Faculty of Biology and Medicine of Lausanne University granted access to TIPP clinical data for research purposes. Therefore, every patient that takes part in TIPP automatically participates in this study, without exception. This is a prospective study based on the first 221 patients who had been enrolled in the program and who had been in treatment for 36 months.
Diagnostic Assessment
Diagnosis is the result of an expert consensus and is based on the following elements: (1) Diagnosis based on DSM-IV criteria32 reported by a treating psychiatrist in all medical documents and at the end of any hospitalization; (2) Longitudinal assessment by psychiatrist and clinical case manager over the 3 years of treatment. The consensus diagnosis procedure is realized by a senior psychiatrist (LA and PB) and the senior psychologist (CF) in charge of scale-based assessment over the treatment period. They both review the entire file once after 18 months and again after 36 months (or at the end of treatment), and conduct a diagnostic process discussing any unclear issue with the clinical case manager. In this study, we considered the diagnostic consensus conducted after 36 months. In case of changes between the 18- and the 36-month evaluation, the 36-month diagnosis was considered. In order to determine the overall rates of depression, we considered diagnosis of depression as a primary diagnosis of major depression with psychotic feature and/or as a co-morbidity.
Assessment of History of Past Trauma
Clinicians at TIPP are trained to conduct an extensive assessment of patients, including evaluation of exposure to traumatic life events. Case managers meet patients frequently over the treatment period, which provides the framework to establish a trusting relationship, where extensive knowledge of patients’ history can be gathered. If patients agree, information can also be completed with family. In the case of inconsistency between the patient’s and the family’s report or in case of doubt regarding the exposure to trauma or the age at the time of exposure, patients were not included in the study.12,21
Case managers complete a table during the patients’ 3 years of treatment, where exposure to traumatic life events can be recorded as follows: (1) Type of traumatic life event, rated as present or absent (sexual abuse, physical abuse, emotional and physical neglect, emotional abuse, among others…); (2) time of occurrence in relation to psychosis stage (during the premorbid phase, during the prodrome or after onset of psychosis); (3) age at the time of first exposure to each one of the traumas that occurred; and (4) single or repeated exposure to each one of the traumas that occurred. Considering that the clinicians who assessed exposure to life events did not rate the subjective perception of severity of the different forms of stressful events, patients were considered traumatized if they had been exposed to at least one experiences of abuse (physical, sexual, or emotional) or neglect (physical or emotional). The consideration was that such events would undoubtedly be considered as highly traumatizing by anyone, and have been shown to be associated with risk for psychosis and functional deficits in psychotic samples.20,33–35 Sexual abuse refers to sexual molestation and/or rape. Physical abuse refers to physical attack or assault, or being repetitively beaten by parents, relatives, or caregivers. Emotional abuse was defined as verbal assaults on a child’s sense of worth or well-being or any humiliating or demeaning behavior directed toward a child by an adult or older person. Physical neglect was defined as the failure of caretakers to provide for a child’s basic physical needs, including food, shelter, clothing, safety, and health care. Emotional neglect was defined as the failure of caretakers to meet children’s basic emotional and psychological needs, including love, belonging, nurturance, and support.36
Age at the time of first exposure was categorized as follows (1) early trauma refers to exposure between birth and age 12, according to conventions applied elsewhere,37–39 (2) late trauma refers to exposure between ages 12 and 16. Patients who were exposed to trauma after age 16 were excluded from this study, according to other studies40 suggesting that they may already have been in the prodromal phase of their first psychotic episode.
Level of Functioning
The level of functioning during follow-up was assessed with the Global Assessment of Functioning (GAF; APA, 199432) Scale and the Social and Occupational Functioning Assessment Scale (SOFAS; APA, 199432). While the SOFAS only takes the social and occupational functioning into account, the GAF also includes the level of symptoms. The GAF scale is a one dimension scale rated from zero to 100 on the basis of anchor definitions: indeed, it provides a very global rating of mixing functional and symptomatic elements. For this reason, we have also conducted ratings on the basis of the SOFAS which is very similar to the GAF except that it does not include psychopathological elements in the definition of the various anchors. As such, these 2 dimensions were rated separately. The psychometric properties of these instruments have been attested.41,42 All patients were assessed on the basis of the GAF and SOFAS scales at each time-point of the follow up (after 2, 6, 12, 18, 24, 30, and 36 months). Instead of relying on a categorical definition of functional recovery (which is dependent on one or several cut-off scores), theses scale were taken as continuous variables when comparing the 3 groups of patients nontrauma, early trauma, and late trauma).
Level of Depressive, Positive, and Negative Psychotic Symptoms
Depressive, positive, and negative symptoms were evaluated at each measurement occasion (after 2, 6, 12, 18, 24, 30, and 36 months of follow-up). Depressive symptoms were assessed using the total score of the Montgomery-Asberg Depression Rating Scale (MADRS43). The MADRS is a 10-item scale commonly used to measure the severity of depressive symptoms. The 10 MADRS items were selected for their ability to detect changes due to antidepressant treatment and their high correlations with overall change in depression. The level of positive and negative symptoms was assessed using the total score of the positive and negative components of the Positive and Negative Syndrome Scale (PANSS44,45). PANSS is a scale which is used to measure psychotic symptoms. It is composed of 30 items (1–7 severity scale) divided into 3 sections: the positive (7 items), the negative (7 items), and the general section (16 items).
Statistical Analysis
Mediation analysis was performed in order to study whether the relationship between trauma and functioning was mediated by depressive symptoms. For each measurement occasion, a series of path analysis models were estimated with early/late trauma as 2 independent dummy variables and MADRS scores as the mediating variable. Because GAF and SOFAS scores were highly correlated (<.90) at each time point, the GAF and SOFAS scores were introduced simultaneously as the 2 dependent variables. These models are allowed to determine whether significant indirect effects between trauma and functioning variables could be observed. Such indirect effect indicates the amount of mediation. Partial mediation is the situation in which the path between trauma and functioning (also called the direct effect) is reduced but still statistically significant when the mediator is introduced. Complete mediation describes the case were the path between trauma and functioning is no longer significant after the introduction of the mediating variable. To verify whether depressive symptoms only could mediate the relationship between trauma and functioning, positive and negative symptoms were also considered as potential mediators in two series of alternate models. Theses path analysis models were estimated using maximum likelihood estimation and bootstrapped standard errors using the Mplus v7.4 software.46 All statistical tests were two-tailed and significance was determined at the .05 level. Considering indices of fit indicated perfect fit, we did not report these values.
Results
Patient Sample
Of the first 221 patients consecutively admitted to TIPP between 2004 and 2012 and for which data was available at the time of the study, 12 patients were excluded for the following reasons: (I) Age at exposure to trauma was not available, or there was a doubt about the exactly age (n = 2); (II) First exposure to trauma occurred during their prodromal phase (n = 4), after psychosis onset (n = 3) or after age 16 (n = 3); (III). Therefore, analysis was carried out on the data of 209 patients.
Rates of Trauma, Demographic Characteristics
The diagnostic breakdown, the baseline and demographic characteristics of the sample, the treatment adherence, the program commitment and the number of hospitalizations are described in table 1. Among the 209 patients, 72 (34.4% of total patients) had a history of trauma. Within the trauma group, 52 (72.2% of exposed patients) had been exposed before age 12 (early trauma) and 20 (27.8% of exposed patients) between age 12 and 16 (late trauma). There were no differences in terms of diagnostic distribution, demographic and baseline characteristics, neither between exposed and nonexposed patients, nor between those exposed early and late. There were only 43 (20.6%) patients with a diagnosis of depression in the entire sample. Among the nontrauma patients, 22 (16.1% of this group) had a diagnosis of depression; among the early trauma patients, 17 (32.7% of this group) had a diagnosis of depression; and among the late trauma patients only 4 (20.0% of this group) had a diagnosis of depression.
Table 1.
Demographic and Baseline Factors Related to Early or Late Exposure to Sexual, Physical, and/or Emotional Abuse and/or Emotional and Physical Neglect (Trauma)
| Total, N = 209 | Nontrauma, N = 137 | Early Trauma, N = 52 | Late Trauma, N = 20 | Nontrauma Vs Trauma (P value) | Early Trauma Vs Late Trauma (P value) | |
|---|---|---|---|---|---|---|
| Age in years, M (SD) | 24.67 (4.76) | 24.31 (4.74) | 25.42 (4.57) | 25.25 (5.30) | .169 | .890 |
| Sex, male, % (N) | 66.0 (138) | 70.1 (96) | 61.5 (32) | 50.0 (10) | .094 | .430 |
| SES, % (N) | ||||||
| Low | 15.8 (33) | 16.8 (23) | 17.3 (9) | 5.0 (1) | .834 | .182 |
| Intermediate | 47.8 (100) | 48.2 (66) | 50.0 (26) | 40.0 (8) | ||
| High | 36.4 (76) | 35.0 (48) | 32.7 (17) | 55.0 (11) | ||
| GAF baseline, M (SD) | 37.72 (15.84) | 38.00 (15.43) | 39.09 (17.37) | 32.85 (14.49) | .426 | .143 |
| SOFAS baseline, M (SD) | 39.99 (15.27) | 40.28 (14.71) | 40.44 (16.40) | 37.05 (16.50) | .529 | .407 |
| Insight at presentation, % (N) | ||||||
| Absent | 32.8 (65) | 35.2 (45) | 28.0 (14) | 30.0 (6) | .290 | .823 |
| Partial | 46.5 (92) | 42.2 (54) | 56.0 (28) | 50.0 (10) | ||
| Complete | 20.7 (41) | 22.7 (29) | 16.0 (8) | 20.0 (4) | ||
| Diagnostic, % (N) | ||||||
| Schizophrenia | 58.9 (123) | 58.4 (80) | 59.6 (31) | 60.0 (12) | .473 | .118 |
| Schizophreniform/BPE | 11.5 (24) | 13.1 (18) | 11.5 (6) | 0.0 (0) | ||
| Schizoaffectif disorder | 10.0 (21) | 10.2 (14) | 5.8 (3) | 20.0 (4) | ||
| Major depressionª | 2.4 (5) | 1.5 (2) | 5.8 (3) | 0.0 (0) | ||
| Biopolar disorder | 6.7 (14) | 8.0 (11) | 1.9 (1) | 10.0 (2) | ||
| Others | 10.5 (22) | 8.8 (12) | 15.4 (8) | 10.0 (2) | ||
| Hospitalizations during program, % (N) | ||||||
| None | 19.1 (40) | 20.4 (28) | 13.5 (7) | 25.0 (5) | .451 | .333 |
| One | 38.3 (80) | 40.1 (55) | 32.7 (17) | 40.0 (8) | ||
| Several | 42.6 (89) | 39.4 (54) | 53.8 (28) | 35.0 (7) | ||
| Complete adherence to treatment, % (N) | ||||||
| After 12 months | 77.0 (161) | 75.9 (104) | 76.9 (40) | 85.0 (17) | .730 | .534 |
| After 24 months | 86.6 (181) | 89.8 (123) | 78.8 (41) | 85.0 (17) | .086 | .744 |
| After 36 months | 90.0 (188) | 92.7 (127) | 82.7 (43) | 90.0 (18) | .089 | .716 |
| Program commitment, % (N) | ||||||
| Interruption > 2 months | 19.1 (29) | 20.6 (21) | 19.4 (7) | 7.1 (1) | .661 | .414 |
| Lost from sight | 10.6 (16) | 11.9 (12) | 8.3 (3) | 7.1 (1) | .581 | .690 |
Note: Analyses between nontrauma vs trauma and early trauma vs late trauma were performed with planned contrasts for one-way independent ANOVA for continuous variables and Fisher’s exact test for categorical variables. BPE, brief psychotic episode; SES, socioeconomic status.
ªWith psychotic features.
Effect of Early- and Late-Trauma on the Level of Functioning of Patients During Follow-up
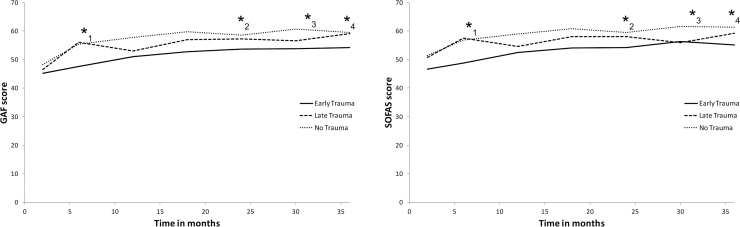
At the 2 months time-point, early- and late-trauma were not significantly related to functioning as assessed by the GAF (early trauma: B = −3.412, P = .205; late trauma: B = −2.010, P = .542). Early-Trauma was related to the SOFAS (early trauma: B = −5.126, P = .044) but not late trauma (B = −1.011, P = .754). Most importantly, at all the other time points, as illustrated in figure 1 (left for GAF scores and right for SOFAS scores), early trauma was significantly related to functioning, while this was not the case for late trauma.
Fig. 1.
Level of functioning measured with the Global Assessment of Functioning Scale (GAF; left) and the Social and Occupational Assessment of functioning Scale (SOFAS; right) with assessments after 2, 6, 12, 18, 24, 30, and 36 months of treatment. Note: At the 2-month time point, there were no differences in terms of Global Assessment of Functioning (GAF) and the Social and Occupational Assessment Scale (SOFAS) scores between early or late trauma patients, and no trauma patients. At the 6, 12, 18, 24, 30, and 36 time points, early trauma patients showed lower levels of GAF score, while this was not the case for late trauma patients. (*1) At the 6 months time point a partial mediation of depressive symptoms between early trauma and GAF scores was observed. (*2) At the 24 months time point a total mediation of positive symptoms between early trauma and GAF scores was observed. At the 30 (*3) and 36 (*4) months time points a total mediation of depressive symptoms between early trauma and GAF scores was observed.
Mediating Effects of Depressive Symptoms on the Link Between Trauma and the Level of Functioning of Patients During Follow-up
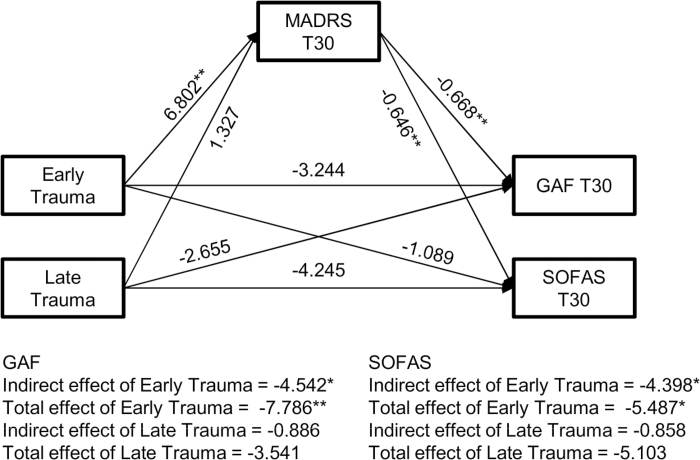
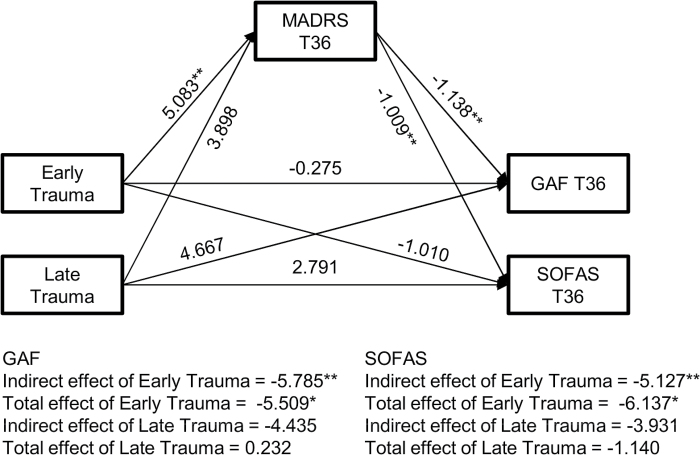
As there was no effect of early or late trauma on the level of functioning (GAF) after 2 months, accordingly, no mediating effect from depressive symptoms could be expected. For the SOFAS, there was no mediating role of depressive symptoms between early trauma and functioning. After 6 months of follow-up, the effect of early trauma was only partially mediated by depressive symptoms (figures 1 left [for GAF] and right [for SOFAS]). Although there was a significant indirect effect of depressive symptoms between early trauma and functioning assessed by the GAF (B = −3.678, P = .031), the direct effect of early trauma was still significant (B = −5.209, P = .039). The same pattern of results could be observed when functioning was assessed by the SOFAS (figure 1 right; indirect effect: B = −3.448, P = .027; direct effect: B = −5.885, P = .014). For the 12, 18, and 24 month’s time-points, depressive symptoms did not play any mediating role between trauma and functioning. After 30 (figure 2) and 36 months (figure 3) of follow-up, the effect of early trauma on functioning was completely mediated by depressive symptoms. There was a significant indirect effect between early trauma and functioning measured by the GAF after 30 months (indirect effect: B = −4.542, P = .015) and 36 months (indirect effect: B = −5.785, P = .003). The direct effect of early trauma was not significant anymore indicating that the overall effect of early trauma could completely be accounted for by depressive symptoms. Results when functioning was measured with the SOFAS were exactly the same after 30 months (indirect effect: B = −4.398, P = .014) and 36 months (B = −5.127, P = .004).
Fig. 2.
Analyses showing the mediating effect of depressive symptoms between trauma and functional outcomes after 30 months of follow-up. Note: *P < .05, **P < .01; MADRS, Montgomery Asberg Depression Rating Scale; GAF, Global Assessment of Functioning; SOFAS, Social and Occupational Assessment Scale.
Fig. 3.
Analyses showing the mediating effect of depressive symptoms between trauma and functional outcomes after 36 months of follow-up. Note: *P < .05, **P < .01; MADRS, Montgomery Asberg Depression Rating Scale; GAF, Global Assessment of Functioning; SOFAS, Social and Occupational Assessment Scale.
It is worth noting that after 3 years of follow-up, nontrauma patients scored on average 8.14 points (SD = 6.41) to the MADRS Scale which corresponds to mild depression levels (7–19 points47). early trauma patients scored on average 5.08 points higher (P = .003) and late trauma patients scored 3.90 points higher (P = .162) than nontrauma patients which also falls into the mild depression category. Earlier in the follow-up (2 months) nontrauma patients scored on average 14.19 (SD = 9.04) while early trauma patients scored 5.56 points higher (P = .009) and late trauma patients scored 3.31points higher (P = .304). After 18 months, nontrauma patients scored on average 11.79 (SD = 9.18) while early trauma patients scored 1.97 points higher (P = .340) and late trauma patients 0.61 points higher (P = .844). In other words, overall depressive symptom levels were low and decreasing over time.
Mediating Effects of Positive and Negative Symptoms on the Link Between Trauma and the Level of Functioning
Positive and negative symptoms measured with the PANSS were next considered as potential mediators in order to verify whether depression only could mediate the relationship between trauma and functioning. As illustrated in figure 1, positive symptoms had a total mediating effect at 24 months of follow-up for GAF and SOFAS. For all others time-points (2, 6, 12, 18, 30, and 36 months), impact of trauma on functional outcome was mediated neither by positive nor by negative symptoms.
Discussion
The current study demonstrates, in a sample of EP patients, that poorer functional levels at 30 and 36 months in patients exposed to CT when compared to of nonexposed patients, is completely mediated by the severity of depressive symptoms. Long-term effects of early trauma on functioning were not accounted for by positive and/or negative symptomatology at those time points. This reveals an important mediating role of depression in this association at the end of the treatment period. Our study also shows that the mediating role of depressive symptoms exists only in patients exposed to CT before the age of 12; this is understandable, considering that patients exposed to trauma at a later age, as previously shown,12 have a better outcome at 30 and 36 months and do not display lower functional level than nonexposed patients.
The mediating role of depressive symptoms between early adversity and the onset and persistence of psychotic experiences has been highlighted recently in different studies.13,16,17,48 However, to our knowledge, Palmier-Claus et al.28 study and ours are the only two studies addressing the potential mediating role of depression on the link between early adversity and the functional outcomes in patients suffering from psychosis. Our results confirm findings reported by Palmier-Claus et al.28 in a larger, more homogeneous sample of EP patients followed-up in a prospective setting.
These results have important therapeutic implications and open new avenues for future research. They suggest that mild depressive symptoms, even if they are below the diagnostic threshold for depression, may be a useful target to aim at with pharmacological and/or psychotherapeutic treatment in patients exposed to severe trauma, particularly in those exposed prior to the age of 12. They also suggest that psychotherapy focusing on the negative perceptions of self, anxiety, insomnia, and depressive mood—symptoms that are part of the depressive syndrome—may also help patients to improve some of their social and vocational difficulties. In addition, in future prospective studies it would be very interesting to stratify patients according to the time at exposure to trauma, and examine whether depressive symptoms (but also some other possible factors such as anxiety, dissociation, insomnia…) may mediate the link between trauma and positive symptoms. If our results are confirmed, it would be important to try and develop interventions and explore in the frame of a randomized controlled trial, if the treatment of subthreshold depression would improve outcome in such patients.
Primary diagnosis of depression with psychotic features was rare in our sample (2.4%), and an additional 18.2% of patients displayed co-morbid depression. However, using depressive symptoms based on the MADRS’s score as a continuous variable, we could show that subdiagnostic depressive symptoms were determinant regarding outcome. This provides additional support to the utility of a dimensional approach of psychiatric disorders49–51 and highlights the importance of exploring subdiagnostic nonpsychotic symptom in EP patients.
Our data showed in addition that while positive symptoms mediated the link between trauma and functional level, they did so only at the 24-months follow-up. This limited impact of positive psychotic symptoms is in line with Palmier-Claus et al.28, who did not find any mediating effect of paranoia between childhood adversity and social functioning. This observation may explain why treatments aimed mainly at the resolution of positive symptoms are not sufficient to improve patients’ functioning level2,3,7 and again highlights the importance of addressing other potential mediators13 such as attachment styles52,53 or social cognition.54 Besides these elements, the fact that we only found this significant mediating effect of positive symptoms at one time point is intriguing and needs to be further explored in future studies.
It is important to mention that the mediating effect of depressive symptoms between CT and functional outcome was only found in patients exposed to trauma before the age of 12, which provide additional evidence for a differential impact of trauma according to age at the time of exposure.39,55 This may be linked to the neuro-developmental stage of patients at the time of exposure to trauma which may be linked to different degree of brain vulnerability.56–60 Taking this into account, and stratifying patients cohorts according to age of exposure to stress may be important in future research in order to better understand the link between trauma and patient’s outcome.
The absence of a mediating effect of depressive symptoms before the 30th month time point in traumatized patients may be linked to the progressive development of insight over time in our sample.61 As mentioned by others,62–65 the development of insight often goes along with the emergence of depressive affects, which may in turn impact functional levels. It is therefore critical to explore this process in patients and to offer support and psychological approaches that promote integration of the episode along with psycho-education, in order to prevent self-stigmatization and pessimism.
Our study has various limitations. Firstly, exposure to CT was assessed retrospectively, which may be particularly problematic for patients suffering from psychosis due to recall bias.66 However, exposure to trauma was assessed on the basis of information obtained from patients and their families in the context of a 3-year therapeutic relationship.67 This reduces the risk of recall bias existing in other forms of self-report or cross-sectional research interviews.68 Secondly, we did not explore some aspects of trauma exposure, such as repetition, length of exposure or the nature of the perpetrator, variables that have all been shown to modulate the impact of trauma on later outcomes39,69 and that may have played a role in our results. Thirdly, the mediation models being cross-sectional, they assume that functioning is mediated by mood, while mood could actually also be mediated by functioning. While this may suggest reciprocal interactions between depressive symptoms and functioning, it is worth noting that when depressive symptoms and functioning were to permutated in the mediation models, we did not observe a complete mediation of the effect of early trauma on depressive symptoms. Finally, the fact that patients have received specialized comprehensive treatment may have influenced the results, possibly reducing the size of the difference between groups.
Despite these limitations, this study shows that the persistence of the impact of trauma on functional outcome in patients who were exposed to trauma in early childhood is completely determined by depressive symptoms. This suggests not only that clinicians should explore this dimension very carefully in such patients but also that even at subdiagnostic levels these symptoms may have a significant impact on functional recovery. If confirmed, these results may pave the way for the development of specific interventions that may contribute to improve this aspect of outcome, which so far has resisted to most of the approaches which can be offered to these patients.
Funding
Swiss National Science Foundation (#320030_122419 to Drs Do and Conus), National Center of Competence in Research “SYNAPSY—The Synaptic Bases of Mental Diseases” from the Swiss National Science Foundation (#51AU40_125759 to Dr Do), and Avina Foundation.
Acknowledgments
We thank the Case Managers from the TIPP Program for collecting these data over the years. Most of all, we express our gratitude to all patients for their participation. The authors have declared that there are no conflicts of interest in relation to the subject of the study.
References
- 1. Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophr Res. 2008;99:119–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hamilton S, Edgell E, Revicki D, Breier A. Functional outcomes in schizophrenia: a comparison of olanzapine and haloperidol in a European sample. Int Clin Psychopharmacol. 2000;15:245–255. [DOI] [PubMed] [Google Scholar]
- 3. Bond GR, Kim H-W, Meyer PS, et al. Response to vocational rehabilitation during treatment with first-or second-generation antipsychotics. Psychiatr Serv. 2004;55:59–66. [DOI] [PubMed] [Google Scholar]
- 4. Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry. 2006. [DOI] [PubMed] [Google Scholar]
- 5. Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26:119–136. [DOI] [PubMed] [Google Scholar]
- 6. Cornblatt BA, Carrion RE, Addington J, et al. Risk factors for psychosis: impaired social and role functioning. Schizophr Bull. 2012;38:1247–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Menezes NM, Arenovich T, Zipursky RB. A systematic review of longitudinal outcome studies of first-episode psychosis. Psychol Med. 2006;36:1349–1362. [DOI] [PubMed] [Google Scholar]
- 8. Lysaker PH, Meyer PS, Evans JD, Clements CA, Marks KA. Childhood sexual trauma and psychosocial functioning in adults with schizophrenia. Psychiatr Serv. 2001;52:1485–1488. [DOI] [PubMed] [Google Scholar]
- 9. Lysaker PH, Nees MA, Lancaster RS, Davis LW. Vocational function among persons with schizophrenia with and without history of childhood sexual trauma. J Trauma Stress. 2004;17:435–438. [DOI] [PubMed] [Google Scholar]
- 10. Trotta A, Murray RM, David AS, et al. Impact of different childhood adversities on 1-year outcomes of psychotic disorder in the genetics and psychosis study. Schizophr Bull. 2016;42:464–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stain HJ, Bronnick K, Hegelstad WT, et al. Impact of interpersonal trauma on the social functioning of adults with first-episode psychosis. Schizophr Bull. 2013;40:1491–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alameda L, Ferrari C, Baumann PS, Gholam-Rezaee M, Do KQ, Conus P. Childhood sexual and physical abuse: age at exposure modulates impact on functional outcome in early psychosis patients. Psychol Med. 2015;45:2727–2736. [DOI] [PubMed] [Google Scholar]
- 13. Bebbington P. Unravelling psychosis: psychosocial epidemiology, mechanism, and meaning. Shanghai Arch Psychiatry. 2015;27:70–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fisher HL, Schreier A, Zammit S, et al. Pathways between childhood victimization and psychosis-like symptoms in the ALSPAC birth cohort. Schizophr Bull. 2013;39:1045–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Varese F, Barkus E, Bentall R. Dissociation mediates the relationship between childhood trauma and hallucination-proneness. Psychol Med. 2012;42:1025–1036. [DOI] [PubMed] [Google Scholar]
- 16. Morgan C, Gayer-Anderson C. Childhood adversities and psychosis: evidence, challenges, implications. World Psychiatry. 2016;15:93–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Murray RM, Sideli L, La Cascia C, La Barbera D. Bridging the gap between research into biological and psychosocial models of psychosis. Shanghai Arch Psychiatry. 2015;27:139–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Freeman D, Stahl D, McManus S, et al. Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol 2012;47:1195–1203. [DOI] [PubMed] [Google Scholar]
- 19. Fisher HL, Appiah-Kusi E, Grant C. Anxiety and negative self-schemas mediate the association between childhood maltreatment and paranoia. Psychiatry Res. 2012;196:323–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van Nierop M, Viechtbauer W, Gunther N, et al. Childhood trauma is associated with a specific admixture of affective, anxiety, and psychosis symptoms cutting across traditional diagnostic boundaries. Psychol Med. 2014;45:1–12. [DOI] [PubMed] [Google Scholar]
- 21. Alameda L, Golay P, Baumann PS, Ferrari C, Do KQ, Conus P. Age at the time of exposure to trauma modulates the psychopathological profile in patients with early psychosis. J Clin Psychiatry. 2016;77:e612–e618. [DOI] [PubMed] [Google Scholar]
- 22. Sachs-Ericsson N, Kendall-Tackett K, Hernandez A. Childhood abuse, chronic pain, and depression in the National Comorbidity Survey. Child Abuse Negl. 2007;31:531–547. [DOI] [PubMed] [Google Scholar]
- 23. Vreeburg SA, Hoogendijk WJ, van Pelt J, et al. Major depressive disorder and hypothalamic-pituitary-adrenal axis activity: results from a large cohort study. Arch Gen Psychiatry. 2009;66:617–626. [DOI] [PubMed] [Google Scholar]
- 24. Brown GW, Craig TK, Harris TO, Handley RV, Harvey AL. Validity of retrospective measures of early maltreatment and depressive episodes using the Childhood Experience of Care and Abuse (CECA) instrument—a life-course study of adult chronic depression—2. J Affect Disord. 2007;103:217–224. [DOI] [PubMed] [Google Scholar]
- 25. Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry. 2012;169:141–151. [DOI] [PubMed] [Google Scholar]
- 26. Conley RR, Ascher-Svanum H, Zhu B, Faries DE, Kinon BJ. The burden of depressive symptoms in the long-term treatment of patients with schizophrenia. Schizophr Res. 2007;90:186–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Resnick SG, Rosenheck RA, Lehman AF. An exploratory analysis of correlates of recovery. Psychiatr Serv. 2004;55:540–547. [DOI] [PubMed] [Google Scholar]
- 28. Palmier-Claus J, Berry K, Darrell-Berry H, et al. Childhood adversity and social functioning in psychosis: exploring clinical and cognitive mediators. Psychiatry Res. 2016;238:25–32. [DOI] [PubMed] [Google Scholar]
- 29. Conus P, Bonsack C. Early intervention for the initial phase of psychotic disorders in Lausanne: what problems and what solutions?. Revue medicale de la Suisse romande. 2004;124:221–224. [PubMed] [Google Scholar]
- 30. Baumann PS, Crespi S, Marion-Veyron R, et al. Treatment and Early Intervention in Psychosis Program (TIPP-Lausanne): implementation of an early intervention programme for psychosis in Switzerland. Early Interv Psychiatry. 2013;7:322–328. [DOI] [PubMed] [Google Scholar]
- 31. Yung AR, Yuen HP, McGorry PD, et al. Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry. 2005;39:964–971. [DOI] [PubMed] [Google Scholar]
- 32. APA. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 33. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lysaker PH, Outcalt SD, Ringer JM. Clinical and psychosocial significance of trauma history in schizophrenia spectrum disorders. Expert Rev Neurother. 2010;10:1143–1151. [DOI] [PubMed] [Google Scholar]
- 35. Ucok A, Bikmaz S. The effects of childhood trauma in patients with first-episode schizophrenia. Acta Psychiatr Scand. 2007;116:371–377. [DOI] [PubMed] [Google Scholar]
- 36. Bernstein DP, Stein JA, Newcomb MD, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27:169–190. [DOI] [PubMed] [Google Scholar]
- 37. Thornberry TP, Ireland TO, Smith CA. The importance of timing: the varying impact of childhood and adolescent maltreatment on multiple problem outcomes. Dev Psychopathol. 2001;13:957–979. [PubMed] [Google Scholar]
- 38. Widom CS, Czaja SJ, Dutton MA. Childhood victimization and lifetime revictimization. Child Abuse Negl. 2008;32:785–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fisher HL, Jones PB, Fearon P, et al. The varying impact of type, timing and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psychol Med. 2010;40:1967–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. van Nierop M, Lataster T, Smeets F, et al. Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: analysis of a large, representative population-based sample. Schizophr Bull. 2014;40(suppl 2):S123–S130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Jones SH, Thornicroft G, Coffey M, Dunn G. A brief mental health outcome scale-reliability and validity of the Global Assessment of Functioning (GAF). Br J Psychiatry. 1995;166:654–659. [DOI] [PubMed] [Google Scholar]
- 42. Jovanović AA, GaSic MJ, Ivković M, Milovanović S, Damjanović A. Reliability and validity of DSM-IV Axis V scales in a clinical sample of veterans with posttraumatic stress disorder. Psychiatr Danub. 2008;20:286–300. [PubMed] [Google Scholar]
- 43. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. [DOI] [PubMed] [Google Scholar]
- 44. Emsley R, Rabinowitz J, Torreman M, Group R-I-EPGW The factor structure for the Positive and Negative Syndrome Scale (PANSS) in recent-onset psychosis. Schizophr Res. 2003;61:47–57. [DOI] [PubMed] [Google Scholar]
- 45. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 46. Muthen LK, Muthén L. Mplus [computer software]. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- 47. Snaith R, Harrop F, Newby TD, Teale C. Grade scores of the Montgomery-Åsberg Depression and the Clinical Anxiety Scales. Br J Psychiatry. 1986;148:599–601. [DOI] [PubMed] [Google Scholar]
- 48. Trotta A, Murray RM, Fisher HL. The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. Psychol Med. 2015;45:2481–2498. [DOI] [PubMed] [Google Scholar]
- 49. Van Os J, Gilvarry C, Bale R, et al. A comparison of the utility of dimensional and categorical representations of psychosis. UK700 Group. Psychol Med. 1999;29:595–606. [DOI] [PubMed] [Google Scholar]
- 50. Allardyce J, Suppes T, Van Os J. Dimensions and the psychosis phenotype. Int J Methods Psychiatr Res. 2007;16(suppl 1):S34–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. van Os J, Kapur S. Schizophrenia. Lancet. 2009;374:635–645. [DOI] [PubMed] [Google Scholar]
- 52. Berry K, Barrowclough C, Wearden A. Attachment theory: a framework for understanding symptoms and interpersonal relationships in psychosis. Behav Res Ther. 2008;46:1275–1282. [DOI] [PubMed] [Google Scholar]
- 53. MacBeth A, Schwannauer M, Gumley A. The association between attachment style, social mentalities, and paranoid ideation: an analogue study. Psychol Psychother. 2008;81:79–93. [DOI] [PubMed] [Google Scholar]
- 54. Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. 2006;32(suppl 1):S44–S63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Keiley MK, Howe TR, Dodge KA, Bates JE, Petti GS. The timing of child physical maltreatment: a cross-domain growth analysis of impact on adolescent externalizing and internalizing problems. Dev Psychopathol. 2001;13:891–912. [PMC free article] [PubMed] [Google Scholar]
- 56. Steullet P, Cabungcal JH, Kulak A, Kraftsik R, Chen Y, Dalton TP, Cuenod M, Do KQ. Redox dysregulation affects the ventral but not dorsal hippocampus: impairment of parvalbumin neurons, gamma oscillations, and related behaviors. J Neurosci. 2010;30:2547–2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Perry BD. Childhood experience and the expression of genetic potential: what childhood neglect tells us about nature and nurture. Brain Mind. 2002;3:79–100. [Google Scholar]
- 58. De Bellis MD. The psychobiology of neglect. Child Maltreat. 2005;10:150–172. [DOI] [PubMed] [Google Scholar]
- 59. Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–445. [DOI] [PubMed] [Google Scholar]
- 60. Andersen SL, Tomada A, Vincow ES, Valente E, Polcari A, Teicher MH. Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. J Neuropsychiatry Clin Neurosci. 2008;20:292–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Klaas HS, Clémence A, Marion-Veyron R, et al. Insight as a social identity process in the evolution of psychosocial functioning in the early phase of psychosis. Psychol Med. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Crumlish N, Whitty P, Kamali M, et al. Early insight predicts depression and attempted suicide after 4 years in first‐episode schizophrenia and schizophreniform disorder. Acta Psychiatr Scand. 2005;112:449–455. [DOI] [PubMed] [Google Scholar]
- 63. McEvoy JP, Johnson J, Perkins D, et al. Insight in first-episode psychosis. Psychol Med. 2006;36:1385–1393. [DOI] [PubMed] [Google Scholar]
- 64. Buchy L, Bodnar M, Malla A, Joober R, Lepage M. A 12‐month outcome study of insight and symptom change in first‐episode psychosis. Early Interv Psychiatry. 2010;4:79–88. [DOI] [PubMed] [Google Scholar]
- 65. Cotton S, Lambert M, Schimmelmann B, et al. Depressive symptoms in first episode schizophrenia spectrum disorder. Schizophr Res. 2012;134:20–26. [DOI] [PubMed] [Google Scholar]
- 66. Howard LM. Allegations of abuse in psychotic patients. Am J Psychiatry. 1993;150:839–840. [DOI] [PubMed] [Google Scholar]
- 67. Conus P, Cotton S, Schimmelmann BG, McGorry PD, Lambert M. Pretreatment and outcome correlates of sexual and physical trauma in an epidemiological cohort of first-episode psychosis patients. Schizophr Bull. 2010;36:1105–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Morgan C, Fisher H. Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma—a critical review. Schizophr Bull. 2007;33:3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Shevlin M, Houston JE, Dorahy MJ, Adamson G. Cumulative traumas and psychosis: an analysis of the national comorbidity survey and the British Psychiatric Morbidity Survey. Schizophr Bull. 2008;34:193–199. [DOI] [PMC free article] [PubMed] [Google Scholar]