Abstract
Problem Most patients with advanced lung cancer currently receive much of their health care, including chemotherapy, as outpatients. Patients have to deal with the complex and time consuming logistics of ambulatory cancer care. At the same time, members of staff often waste considerable time and energy in organisational aspects of care that could be better used in direct interaction with patients.
Design Quality improvement study using direct observation and run and flow charts, and focus group meetings with patients and families regarding perceptions of the clinic and with staff regarding satisfaction with working conditions.
Setting Thoracic oncology outpatient clinic at a Norwegian university hospital where patients receive chemotherapy and complementary palliative care.
Key measures for improvement Waiting time and time wasted during consultations; calmer working situation at the clinic; satisfaction among patients.
Strategies for change Rescheduled patients' appointments, automated retrieval of blood test results, systematic reporting in patients' files, design of an information leaflet, and refurnishing of the waiting area at the clinic.
Effects of change Interventions resulted in increased satisfaction for patients and staff, reduced waiting time, and reduced variability of waiting time.
Lessons learnt Direct observation, focus groups, questionnaires on patients' satisfaction, and measurement of process time were useful in systematically improving care in this outpatient clinic. The description of this experience can serve as an example for the improvement of a microsystem, particularly in other settings with similar problems.
Context
Improving the quality of ambulatory care for patients with lung cancer is challenging. Oncologists, who generally have little time available,1 need to help patients find the right balance between chemotherapy and radiotherapy and supportive care2 in ambulatory clinics, where the infrastructure and organisation is not adequate to deal with increasingly sick patients who traditionally have been admitted as inpatients.3 Under such circumstances, effective and timely services are essential to allow for informed patient centred decisions.4 Furthermore, the evaluation of system and process changes in this setting is difficult because of interdisciplinary care, complex treatments, and the inevitable deterioration in most patients' medical condition.5
In Bergen the outpatient clinic for patients with lung cancer is at the department of thoracic medicine. Each year in this clinic6 about 150 patients with advanced lung cancer receive chemotherapy and about 300 patients attend for their regular follow up visits at the unit. Chest radiographs are taken at the unit. Blood samples are also taken and analysed at a central laboratory. Results are available through a password protected computer system. Two consultants and three nurses work in the clinic four days a week.
Outline of the problem
The unit was started in 1995 to reduce costs of ambulatory chemotherapy. Because of their weekly visits for chemotherapy and their need for ancillary hospital facilities and oncological expertise, however, patients became attached to the unit, which became a primary provider of care.
At baseline, neither the infrastructure nor the organisation of our clinic was well designed to meet the task of providing chemotherapy and supportive care. Signals that alerted us of problems included complaints from team members about constant time pressure. Paradoxically, while members of the oncology team constantly felt a lack of time, patients were spending many hours each visit waiting for their chemotherapy. The fact that most of the patients only had a few months to live aggravated the problem of waiting time.
Because of these problems we embarked on a project with the long term goal of improving the palliative care for lung cancer patients at the clinic.
Key measures of improvement
We defined the following aims for the project:
Reducing waiting time by at least 30 minutes
Reducing the waste of time during consultations
Calming the work situation at the clinic.
Process of gathering information
Eight patients and six spouses participated in a focus group. All patients had received at least one cycle ofchemotherapy at the clinic. The overall question for the group was, “What is your impression of the outpatient clinic?”
Box 1: Methods and key findings during process of gathering information
Table 1.
| Method | Findings |
| Patient focus group | Waiting time is too long |
| Explanations for waiting time should be given | |
| Doctors need to be updated on the patient; otherwise patients feels insecure | |
| Information given by different staff members and should not be contradictory | |
| Staff availability and time spent with staff are appreciated | |
| Furniture in waiting area is uncomfortable | |
| Information should be individualised | |
| Information should be actively offered | |
| Alternative medicine and psychological and nutritional problems should be discussed | |
| Direct observation | |
| Direct observation | Nurse has fragmented work situation due to retrieval of laboratory results |
| Waste of time during consultations | |
| Difficult to gain overview in electronic patient file | |
| “Walking the system” | Coordination between process at the clinic and the pharmacy causes delays |
| Flow chart | Process sequence causes delays |
To stimulate the discussion we also asked: “What is your best impression?” “What is your worst impression?” “What do you think about the quality of information and communication at the clinic?” “Do team members respond to non-medical problems?” and “Is there anything that has not been mentioned yet?” An external nurse facilitated the group and another nurse documented the conversation.
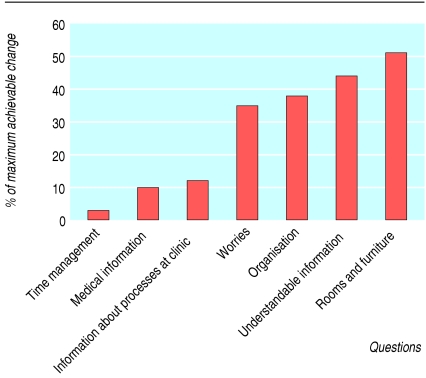
We designed a questionnaire to measure patients' views sequentially. The questions were based on topics that had been brought up in focus groups. Patients rated their answers on a scale, with 7 being best and 1 worst. For each question we calculated the mean of the maximum achievable improvement—that is, the best obtainable score (7) minus the actual score after the interventions. Then we calculated the actual differences between the mean scores for each question before and after the interventions. Finally, the achieved difference in percentage of the maximum achievable difference was plotted to show achievements of the project and potential for future improvements. Considering the short survival time for patients with advanced lung cancer, we accepted the need to sample different groups of patients before and after interventions.
Discussion, analysis, and planning took place at team meetings held twice a month during the project. Meetings followed a structured agenda; roles of leader, timekeeper, and recorder were designated. Conclusions were recorded in writing, distributed to all team members by email, and made available on the local bulletin board as the “latest news.” Staff satisfaction was documented in a focus group that was facilitated by an external nurse.
We created a flow chart after walking through the relevant hospital units, observing colleagues at work and following the patients' progress through the system. CvP observed the processes, and the observations were discussed in the team meetings. The nurse at the clinic registered waiting time, which was defined as time from registering at the front desk until chemotherapy was started.
Analysis and interpretation
Waiting time was a concern for patients and their families, and many patients often felt physically uncomfortable in the waiting area, particularly those with pain from bone metastases. Team discussions and direct observations showed that nurses often had to interrupt other tasks to check the computer for results of blood tests. These repeated checks added up to considerable amounts of time and fragmented work, particularly as nurses had to log on to the computer each time. On a busy day the nurse might need to look up results as many as 10 times during one hour.
Considerable time was used during consultations to get an overview of the patient's status and earlier treatment in the electronic file. In the focus group, patients mentioned that they felt insecure in these situations (box 1). Furthermore, uncertainty about the number of chemotherapy cycles had resulted in near errors and occasionally manifest errors.
Strategy of change
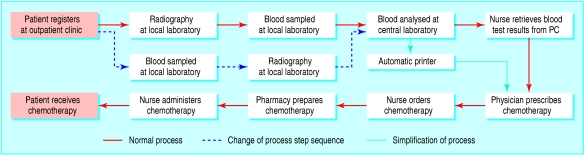
Box 2 shows an overview of the changes implemented. The flow chart (fig 1) suggested that patients could have their x ray pictures done while they waited for laboratory results. We also found that by installing a network printer in the doctor's office the results of blood tests could be printed automatically as soon as they were available in the laboratory, thus reducing the number of steps in the process and freeing up nurses' time.
Fig 1.
Movement through outpatient clinic for patient with lung cancer
We also found that the time required to prepare chemotherapy drugs for administration (pharmacy time) varied considerably depending on the time of day. A visit to the hospital pharmacy showed that chemotherapy orders arriving before 10 am could be completed within less than an hour, while later orders had to be postponed. To avoid unnecessary delays for drug preparation, we therefore scheduled patients for chemotherapy earlier than previously and ordered drugs early in the consultations, postponing talks and questions until later in the day.
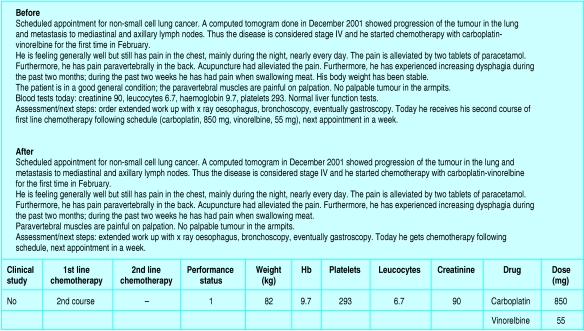
To increase clarity of the patient's file and save consultation time, the number of cycles of chemotherapy, haematological parameters, weight, World Health Organization performance status, and dose were reformatted in the electronic record in tabular form (fig 2). Physicians dictated their notes by following the structure of this table.
Fig 2.
Before and after example of a patient's notes showing use of standardised table to simplify presentation
To improve patients' understanding of their progress through the hospital, we wrote an information leaflet that explained the organisation of the clinic and reasons for possible delays. The leaflet also lists team members with contact information. It was produced locally and can easily be updated.
Initially, the clinic had a consultation room, a chemotherapy room, and a hallway. We opened a separate and more convenient room for talks with patients and families. Comfortable sofas that would allow patients to lie down were put in the waiting area.
The head of the department was kept informed. From the beginning the laboratory and the information technology department were involved in planning changes. CvP dedicated one day a week for three months to the project.
Effects of change
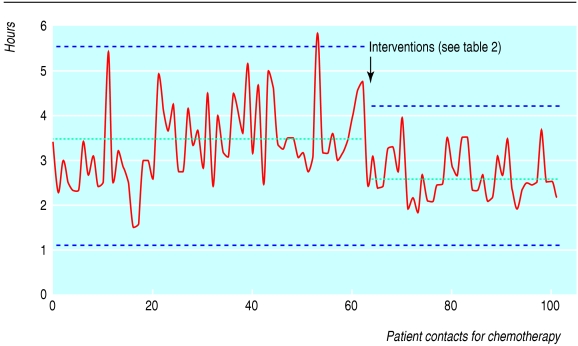
Measurements before and four months after interventions showed that absolute waiting time was reduced by nearly an hour and variation in waiting time had also decreased (from a mean of 3 hours 23 minutes (range 2 hours 19 minutes to 5 hours 42 minutes) to 2 hours 38 minutes (1 hour 32 minutes to 4 hours 10 minutes)) (fig 3). The reduction in waiting time seemed to be due to a combination of rescheduling appointments and simplifying the care process by installing a network printer.
Fig 3.
Time from registration at the outpatient clinic to start of chemotherapy. Time measurements were plotted as a run chart. Control limits (dotted blue lines) were calculated as: upper/lower control limit=mean waiting time±(2.66×average point to point variation—that is, moving range). Dotted green lines represent average waiting times
Twenty six patients completed the questionnaire the first time and 28 at the follow-up six months later, and five participated in both surveys. The mean score of patients' general satisfaction with the clinic before and after the interventions was 6.0 and 6.2, respectively. Figure 4 shows the patients' perceptions of the improvement of different aspects of the service as measured with the questionnaire: facilities at the clinic (51%), clarity of medical information (44%), organisation of the clinic (38%), opportunities to talk about non-medical problems (35%), orientation about the organisation of the clinic (12%), and the amount of information (10%). The least change wasfound in patients' perception of time management by members of staff (3%). Time management also scored lowest in questions before interventions with a mean score of 5.1, while all other questions scored above 5.4.
Fig 4.
Improvement in patients' views expressed as percentage of maximum possible change in score
Box 2: Overview of problems, improvement principles, and interventions
Table 2.
| Problem | Improvement principle | Intervention |
| Waiting time too long | Rearrange steps of process | X ray pictures taken during laboratory analysis time |
| Reduce number of process steps | Network printer installed at physicians office | |
| Coordinate with other units of system | Rescheduling of patient appointments | |
| Patient not aware of reason for waiting time | Explain processes of care | Local information leaflet |
| Fragmented work situation | Reduce number of process steps | Network printer installed at physicians office |
| Waste of time because of difficulty in gaining up to date information during consultations | Simplify presentation of information, use potential of information technology | Tabulate crucial patient information in electronic file |
A focus group meeting with team members at the end of the project showed that the working situation was more relaxed, allowing for better communication with patients; work had become more interesting because of the broader approach to treatment; and patients' records were easier to interpret. Physicians, however, found that routine procedures were still too time consuming.
Next steps
So far we have improved time management, work flow, the physical space at the clinic, and the documentation in patients' files. Having achieved this degree of improvement, we will incorporate more complex measurement dimensions into routine clinical practice.7 Beyond patients' satisfaction and assessment of process, we will also incorporate medical (symptom control, mortality) and functional (time spent at home) outcomes and an assessment of cost. For this purpose, we have begun to use the Edmonton symptom assessment system.8 Such a balanced combination of measurement dimensions has been called clinical value compass.9
Key learning points
Actively seeking feedback from patients in focus groups created ideas and momentum for improvement of this clinical microsystem
Observation, analysis, and illustration of the processes of care revealed interventions for improvement
Waiting time was reduced significantly and reliably by simple changes of scheduling and rearrangement of process steps
Clarity of medical information was improved by tabulation within existing electronic patient file
Reductions in waiting time seemed to be due to a combination of rescheduling patients' appointments and simplifying the care process by installing a network printer. Unfortunately, it was difficult to disentangle the influence of these two factors as they were introduced at the same time. Moreover, increased motivation of team members in the early phases of the project and enhanced awareness of process probably also contributed to the improvements. Increased motivation may, of course, wane with time, although precise knowledge about effective interventions may help to maintain enthusiasm and the gains. We plan to improve future measurements of change by restricting interventions to a single factor while performing repeated measurements.
While the changes were successful within the clinic, shortcomings of linkages to other units and the need for coordinating support from leadership in the hospital became obvious during the course of the study.10 Next steps in the improvement of the service will cover handovers between the outpatient clinic and other units and between different levels of care in the community.11
In the course of the project, we recognised that we often did not know when our patients had died and that we lacked opportunities to cope with our feelings of loss. Thus we established a monthly team meeting to talk about patients who had died and to reflect about their time at the clinic.
In summary, we addressed generally relevant aspects of outpatient oncology care for outpatients, such as waiting time, flow of patients, design of waiting areas, and documentation of chemotherapy. Feedback from patients and measurement of their views and the performance of process drove the changes. The novelty of the quality improvement approach was welcomed by patients and staff as a way to change the system.
We thank Frank Davidoff for his constructive reviewing of the manuscript, Gene Nelson for contributing ideas, Kerstin vonPlessen for detailed comments, and Alf Andreassen for supporting the project in the department of thoracic medicine. Contributors: CvP developed the project, wrote the paper, and is guarantor. AA guided the design of the project and reviewed the manuscript.
Funding: The project was supported by the Quality Improvement Fund of the Norwegian Medical Association. The Norwegian Heart and Lung Foundation sponsored new furniture for the waiting area at the clinic.
Competing interests: Astra-Zeneca, GlaxoSmithKline, and Boehringer have supported CvP to attend conferences on thoracic medicine. He is currently investigator in clinical studies initiated by AstraZeneca and ElyLilly. AA has received funding from the Norwegian Cancer Society and Medirad.
Ethical approval: The protocol was presented to the local ethical research committee and a formal review was not deemed necessary.
References
- 1.Benson RJ, Burnet NG, Williams MV, Tan LT. An audit of clinic consultation times in a cancer centre: implications for national manpower planning. Clin Oncol (R Coll Radiol) 2001;13: 138-43. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell G, Currow D. Chemotherapy and radiotherapy. When to call it quits. Aust Fam Physician 2002;31: 129-33. [PubMed] [Google Scholar]
- 3.Zimber J. [Managing oncological patients. It can also be done on an ambulatory basis]. MMW Fortschritte der Medizin 2001;143: 22-4. [PubMed] [Google Scholar]
- 4.Lock KK, Wilson B. Information needs of cancer patients receiving chemotherapy in an ambulatory-care setting. Can J Nurs Res 2002;34: 83-93. [PubMed] [Google Scholar]
- 5.Newell S, Sanson-Fisher RW, Girgis A, Ackland S. The physical and psycho-social experiences of patients attending an outpatient medical oncology department: a cross-sectional study. Eur J Cancer Care (Engl) 1999;8: 73-82. [DOI] [PubMed] [Google Scholar]
- 6.Nelson EC, Batalden PB, Huber TP, Mohr JJ, Godfrey MM, Headrick LA, et al. Microsystems in health care: Part 1. Learning from high-performing front-line clinical units. Jt Comm J Qual Improv 2002;28: 472-93. [DOI] [PubMed] [Google Scholar]
- 7.Nelson EC, Splaine ME, Batalden PB, Plume SK. Building measurement and data collection into medical practice. Ann Intern Med 1998;128: 460-6. [DOI] [PubMed] [Google Scholar]
- 8.Chang VT, Hwang SS, Feuerman M. Validation of the Edmonton symptom assessment scale. Cancer 2000;88: 2164-71. [DOI] [PubMed] [Google Scholar]
- 9.Nelson EC, Mohr JJ, Batalden PB, Plume SK. Improving health care. Part 1. The clinical value compass. Jt Comm J Qual Improv 1996;22: 243-58. [DOI] [PubMed] [Google Scholar]
- 10.Kleiner A. Health care. How hospitals can learn. In: Senge PM, Kleiner A, Roberts C, Ross RB, Smith BJ, eds. The fifth discipline fieldbook. New York: Doubleday, 1994: 479-84.
- 11.Batalden PB, Mohr JJ. Building knowledge of health care as a system. Qual Manag Health Care 1997;5: 1-12. [PubMed] [Google Scholar]