Abstract
Over the past six decades, the Chinese government made parasitoses with a high disease burden, including soil-transmitted nematode infections, malaria, leishmaniasis, filariasis, and schistosomiasis, a public health priority because they were seen to be crucial impediments to the development of rural areas. As a result, these debilitating parasitic diseases that used to be widely prevalent have been well controlled or eliminated. Consequently, less attention has been paid to parasitic infection during the rapid development of the economy, especially in developed areas. However, our investigations conducted in the parasitological laboratory of Sun Yat-sen University (Guangzhou, Guangdong, China) show that emerging parasitic diseases still threaten many people’s health, with 340 of 880 outpatients (38.6%) receiving a diagnosis of parasitic disease, among whom 201 (59.1%) had clonorchiasis and 120 (35.3%) had taeniasis/cysticercosis. Furthermore, our doctors are not equipped with sufficient parasitology knowledge because this discipline is not able to maintain attraction. Many parasitic infections that result in severe consequences are treatable and preventable, but the phenomena of misdiagnosis and missed diagnosis are common and merit attention.
Electronic supplementary material
The online version of this article (doi:10.1186/s40249-017-0332-0) contains supplementary material, which is available to authorized users.
Keywords: Parasitic diseases, Parasitology, Guangdong Province, P. R. China
Multilingual abstracts
Please see Additional file 1 for translations of the abstract into the five official working languages of the United Nations.
Background
China used to suffer greatly from parasitic infections [1, 2]. For example, lymphatic filariasis was highly prevalent in China 60 years ago, with 31 million cases and 330 million people at risk of endemic infection living in 864 counties of 16 provinces, autonomous regions, and municipalities. Its most spectacular symptom is elephantiasis — edema with thickening of the skin and underlying tissues that causes dramatic loss of labour to society, followed by tremendous economic loss [3, 4]. To enhance the population’s health, China spared no effort to fight against parasites over the past six decades, which led to great progress in parasitic disease control. For example, the conventional major parasitic diseases in China (soil-transmitted nematode infections, malaria, leishmaniasis, filariasis, and schistosomiasis) either have been eliminated or are well controlled [3–9]. Therefore, less attention is paid to parasite control than before. Instead, non-communicable chronic diseases such as cancer, diabetes, respiratory diseases, hypertension, and dementia are becoming common causes of disability and mortality [10, 11], and therefore, studies in this field are increasingly popular, and parasitology is no longer a hot discipline. Parasitology used to be a compulsory and key course for all medical students in China, but this is no longer the case. More and more medical schools have decided to devote fewer resources to the course. Hence, the scale of parasitology becomes smaller and smaller [12, 13]. As a result, departments of parasitology in China have been abrogated or integrated to pathogenic biology or pathogen and immunology [14]. Furthermore, the time spent studying parasitology has been significantly shortened in some medical schools in China [12, 15].
Parasitic infections are becoming neglected diseases, especially in well-developed areas with good sanitary and hygienic conditions, such as Shanghai, Beijing, and Guangdong Province in mainland China, because parasitoses are generally recognized as diseases of poverty [16] that will disappear as a result of higher standards of living and poverty alleviation. However, as a result of an unhealthy diet and lifestyle, an increasing number of people are willing to eat raw or undercooked vegetables and meat (pork, beef, fish, crab, snails, etc.), especially in highly developed cities like Guangzhou and Shenzhen in Guangdong. Thus, the prevalence of foodborne parasitic diseases is actually on a slight rise [17–20]. In addition, many urban families are keeping pets like cats (a known host of Toxoplasma gondii), which increases the risk of infection [21]. Furthermore, as national and international travel become more and more accessible and affordable, adventurous travellers will continue to return home with increasingly exotic infections, including parasitic infections [22]. This study aimed to investigate the parasitic infection situation in Guangdong, China, and to call attention to these ancient infectious diseases, especially in highly developed areas.
Patients and methods
The flowchart of this study is shown in Fig. 1. Between 1 Sept 2015 and 31 Aug 2016, blood and/or stool samples from 880 suspected cases were tested in the parasitological laboratory of Sun Yat-sen University (SYSU parasitic-clinic). The SYSU parasitic-clinic has gained a good reputation in the diagnosis of parasitic diseases, and experienced doctors generally refer suspected patients to the SYSU parasitic-clinic because their hospitals are not equipped with appropriate tests and skilled technicians. Each of the suspected patients was interviewed by a well-trained staff member. The information collected included the following.
Demographic characteristics: gender, age, education level, household income, and place of residence (i.e., city and province);
History of contact: drinking unclean water, consumption of raw or undercooked vegetables or meat (pork, beef, fish, crab, snails, etc.), keeping pets or contact with pets, contact with cecariae-infested water;
Symptoms and signs: stomachache, diarrhoea, jaundice, cough, expectoration, subcutaneous nodule, epilepsy, paralysis, impaired vision, or loss of vision.
Fig. 1.
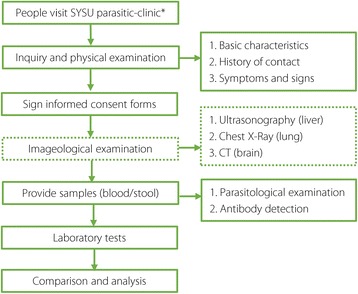
Flowchart. Full line: All participants took these steps. Dotted line: Not all participants took this step. * SYSU parasitic-clinic: Parasitological Laboratory of Sun Yat-sen University
Clinical diagnosis was made based on contact history, symptoms and signs, and laboratory findings. Imaging studies also helped in diagnosis, but not all suspected participants underwent such studies for many reasons, such as high cost and fear of radiation.
Parasitological examination
For patients in whom intestinal parasitic diseases were suspected, a single faecal sample was collected in a capped plastic polypot. Triplicate Kato-Katz microscope slides were then prepared and examined under a microscope at × 400 magnification by two experienced technicians within 2 h [23].
Antibody tests
Venous blood samples were drawn from each participant in aseptic conditions without stasis using vacuum blood collection tubes (no additive). Blood serum was obtained after rapid centrifugation for 10 min at 2000 g and then stored in 0.5 ml aliquots at −20 °C. The specific antibody for detection was chosen according to doctors’ advice based on the participant’s contact history and manifestations, and detection was then carried out by two skilled technicians in strict accordance with the manufacturers’ instructions. The antibody test kits were purchased from Yikang Co. Ltd., Guangzhou, China.
Statistical analysis
For continuous variables, data were expressed as mean (M) ± standard deviation (SD), and differences between groups were examined with Student’s t-test; for categorical variables, data were expressed as number (%), and differences between groups were examined with the chi-square or Fisher’s exact test. A P value of less than 0.05 (two-sided) was considered to indicate statistical significance. All data analyses were performed with SPSS 22.0 software (Chicago, IL).
Results and discussion
A significant difference in gender was seen between infected and non-infected participants, but little difference was observed in age, education level, household income, and place of residence (Table 1), which implies that these factors do not have significant effects on the morbidity of parasitic diseases. Women acquired fewer parasitic infections, partially due to better hygiene-related behaviours, because woman usually pay more attention to their own health condition.
Table 1.
Comparison of characteristics between infected and non-infected participants
| Factors | Infected | Non-infected | P value |
|---|---|---|---|
| Gender (%) | |||
| Male | 258 (75.9) | 265 (49.1) | 0.001 |
| Female | 82 (24.1) | 275 (50.9) | |
| Age (y) | 37.6 ± 14.4 | 42.4 ± 14.2 | 0.146 |
| Education Level (%) | |||
| Illiterate | 0 (0.0) | 15 (2.8) | 0.449 |
| Primary school | 13 (3.8) | 36 (6.6) | |
| Middle school | 128 (37.7) | 193 (35.8) | |
| College or above | 199 (58.5) | 296 (54.8) | |
| Household income (%) | |||
| < 10,000 RMB | 188 (55.2) | 246 (45.5) | 0.482 |
| 10,000 to 50,000 RMB | 45 (13.2) | 104 (19.3) | |
| 50,000 to 100,000 RMB | 18 (5.3) | 67 (12.4) | |
| > 100,000 RMB | 89 (26.3) | 123 (22.8) | |
| Place of residence (%) | |||
| Urban areas | 331 (97.4) | 506 (93.7) | 0.014 |
| Rural areas | 9 (2.6) | 34 (6.3) | |
As seen in Fig. 2, more than 94% of cases were from Guangdong; among these cases, around 60% were from Guangzhou, the provincial capital of Guangdong, and the others were from other cities, including Shenzhen, Dongguan, and Foshan. This distribution is understandable because the SYSU parasitic-clinic is located in Guangzhou and primarily provides health services to the local population. Of the 880 suspected cases, 340 participants were confirmed to have at least one of the six parasitic diseases (Fig. 3), and some even had co-infections. The leading parasitic disease was clonorchiasis, probably as a result of local eating habits. Many patients enjoy sashimi (raw fish), and this habit is difficult to change, even after long-term health education [19, 24]. However, many cases of clonorchiasis are asymptomatic or have mild symptoms, and the infection may go unrecognized or be misdiagnosed. Recent studies have shown that it is capable of causing cancer of the liver and bile duct, and in 2009 it was classified as a group 1 biological carcinogen that poses a remarkable threat to human health [25]. Taeniasis/cysticercosis, usually caused by ingestion of raw pork, is second only to clonorchiasis. Patients may show severe symptoms, such as epilepsy, paralysis, and impaired vision or loss of vision, leading to reduced physical functioning [2]. As a debilitating illness, paragonimiasis takes third place, manifesting as cough, bloody sputum, and chest pain [17] (Fig. 4).
Fig. 2.
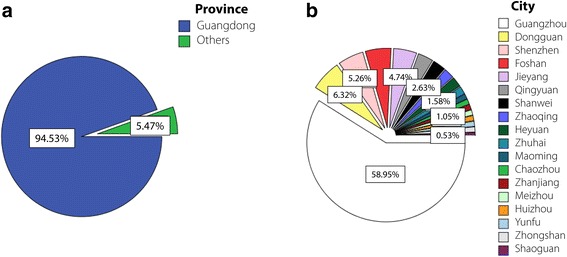
Geographic distribution (provinces, cities) of the 880 suspected cases in SYSU parasitic-clinic. a Distribution by province. b Distribution by city in Guangdong Province (picture drawn with SPSS 22)
Fig. 3.
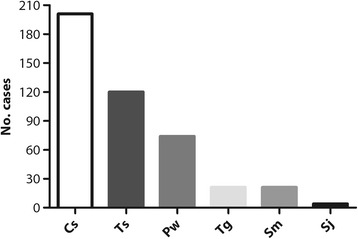
Number of clinically confirmed cases of the six parasitic diseases in SYSU parasitic-clinic. Cs: Clonorchis sinensis; Pw: Paragonimus westermani; Tg: Toxoplasma gondii; Ts: Taenia solium, Sm: Spirometra mansoni; Sj: Schistosoma japonica (picture drawn with GraphPad Prism 5)
Fig. 4.
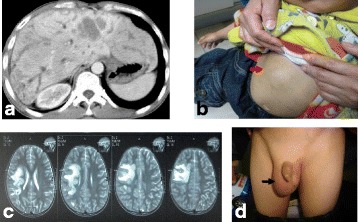
Damage caused by the main two parasitic infections. a CT image of intrahepatic biliary dilatations caused by Clonorchis sinensis infection. b MRI of brain cyst due to cerebral paragonimiasis. c Patient presented with a subcutaneous nodule in his right upper abdomen (red arrow) due to cutaneous paragonimiasis. d A patient presented with a mass in his right scrotum (black arrow) due to cutaneous paragonimiasis. All pictures are reproduced with the permission of the patient or that of his or her guardians
As shown in Fig. 5, patients with clonorchiasis had a much higher incidence of raw fish consumption than other participants (χ 2 = 22.53, P < 0.001), which means that ingestion of sashimi is a common risk factor that contributes to an accurate diagnosis. However, few patients with cysticercosis or paragonimiasis reported a contact history, which hindered an accurate diagnosis. As a result, clinical misdiagnosis and missed diagnosis often occurs.
Fig. 5.
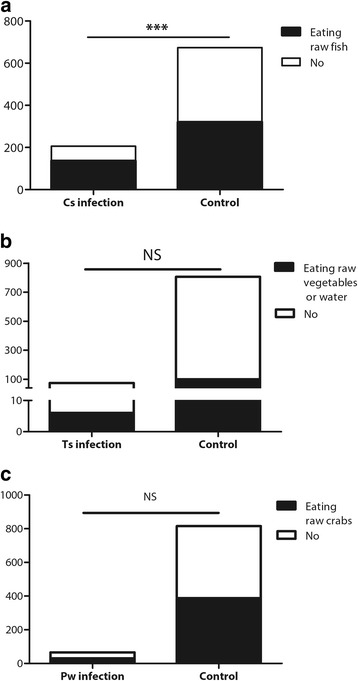
History contact frequencies between infected and non-infected participants. a Eating raw or undercooked fish. b Eating raw or undercooked crab or crayfish. c Eating raw or undercooked pork or vegetables or drinking unclean water. Cs: Clonorchis sinensis. Ts: Taenia solium. Pw: Paragonimus westermani. ***: P < 0.001. NS: not significant. (This picture was drawn with GraphPad Prism 5)
As ancient pathogens, human parasites have long been combated [2]. Because parasitic diseases are treatable and preventable, unremitting efforts have led to the control or elimination of the five main parasitic diseases in China [3–9]. Nationally, the annual incidences of schistosomiasis (0.2133/100000), malaria (0.2326/100000), filariasis (0), and leishmaniasis (0.0223/100000) are now very low according to the available 2016 official record [26]. Significant improvement has also been observed in the control of soil-transmitted nematode infection; the prevalence dropped from 20.88% in 2006 to 3.12% in 2013 [27]. However, other parasitic diseases that are less prevalent and relatively less harmful to humans have attracted little attention from the government. As a result of an unhealthy diet and lifestyle, an increasing number of people are willing to eat raw or undercooked vegetables and meat (pork, beef, fish, crab, snails, etc.), especially in highly developed cities like Guangzhou and Shenzhen. Hence, the prevalence of foodborne parasitic diseases is actually on a slight rise. The occurrence of emerging parasitic diseases is occasionally reported and has at times raised huge concern [1, 18, 28, 29]. For instance, an outbreak of eosinophilic angiostrongylaisis caused by the consumption of raw Ampullaria gigas in Beijing in 2006 caused panic, and at that time, many residents refused to eat freshwater snails (the intermediate host of Angiostrongylus cantonensis) for fear of acquiring infection [18]. However, this fear was soon forgotten.
Time has devalued the stature of parasitology, which seems unavoidable. Misdiagnosis and missed diagnosis of parasitic diseases are often seen in current practice [30–33], partially due to the lack of availability of deworming tablets and local expertise, especially in non-endemic settings [22]. For example, it was estimated that more than 6 million people in Guangdong Province had clonorchiasis, but only 1.8 million were treated, indicating a large number of missed diagnoses and misdiagnosed cases due to the non-specific symptoms and the lack of proper training of physicians [34, 35]. Hepatic clonorchiasis might be misdiagnosed as hepatitis B infection because of the geographic overlap and similar clinical features of these two diseases. Hence, diagnosis and treatment of clonorchiasis in a case of co-infection with hepatitis B virus is a great challenge [29, 36]. Those that parasitize in the human brain, such as juvenile Spirometra mansoni and Taenia solium, can lead to severe brain damage or death without timely anthelmintic treatment [2, 32, 37]; these are easily treatable diseases, but neurologists usually consider brain tumours instead of parasitic infections. In addition, it is quite difficult to differentiate from other diseases under the circumstance of ectopic parasitism. Thus, it is vital to equip doctors with knowledge of parasitology so that they are qualified to make an accurate diagnosis so that patients can receive timely treatment.
This study has some limitations. We only studied one-year data from one small clinic, even though it is the largest clinic of parasitology in Guangdong. However, it is only the tip of the iceberg and cannot represent the whole picture of the parasitic disease burden there. A great number of cases of parasitic diseases go undiagnosed because medical students’ or doctors’ knowledge of parasitology is far from satisfactory. Guangdong has the largest economy in China, and its gross domestic product has ranked 1st for 27 consecutive years, at over seven trillion RMB (around 1.1 trillion USD) in 2015 [38, 39]. Guangdong is one of the most developed areas in China, but parasitic diseases, usually recognized as a disease of poverty, remain a problem and pose a threat to human health. It is important to raise the awareness of both the public and medical personnel about parasitic diseases. Not only would it help to reduce the prevalence of parasitoses, but it would also decrease the rates of missed diagnosis or misdiagnosis.
Conclusions
Parasitic diseases still threaten many people’s health, not only in rural areas but also in urban areas. However, our doctors are not equipped with sufficient knowledge in parasitology because this discipline has not been able to maintain its attraction. Many parasitic infections that result in severe consequences are treatable and preventable, but the phenomena of misdiagnosis and missed diagnosis are common, which merits attention.
Acknowledgements
Not applicable.
Funding
This study was supported by National Research and Development Plan of China (No. 2016YFC1200500).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
Additional file
Multilingual abstracts in the five official working languages of the United Nations. (PDF 530 kb)
Authors’ contributions
ZD-W instructed and coordinated the study. XY-Z and DT-L were responsible for the interview and performed the experiments. LG-S analysed the data and wrote the first draft. GX-W provided some important information. XY-Z, DT-L, GX-W and ZD-Wu revised the manuscript. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Sun Yat-sen University (Guangzhou, Guangdong, China). All patients and guardians who participated signed informed consent forms before doing so.
Consent for publication
All images are reproduced with the permission of the patients.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s40249-017-0332-0) contains supplementary material, which is available to authorized users.
Contributor Information
Lan-Gui Song, Email: songlg@mail2.sysu.edu.cn.
Xiao-Ying Zheng, Email: zhengxy@mail.sysu.edu.cn.
Da-Tao Lin, Email: 1697084321@qq.com.
Guang-Xi Wang, Email: 2371966379@qq.com.
Zhong-Dao Wu, Email: wuzhd@mail.sysu.edu.cn.
References
- 1.Li T, He S, Zhao H, Zhao G, Zhu XQ. Major trends in human parasitic diseases in China. Trends Parasitol. 2010;26(5):264–270. doi: 10.1016/j.pt.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 2.Wang JL, Li TT, Huang SY, Cong W, Zhu XQ. Major parasitic diseases of poverty in mainland China: perspectives for better control. Infect Dis Poverty. 2016. doi: 101186/s40249-016-0159-0. [DOI] [PMC free article] [PubMed]
- 3.Sun DJ, Deng XL, Duan JH. The history of the elimination of lymphatic filariasis in China. Infect Dis Poverty. 2013;2(1):30. doi: 10.1186/2049-9957-2-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rebollo MP, Bockarie MJ. Can lymphatic filariasis be eliminated by 2020? Trends Parasitol. 2016. doi: 101016/jpt201609009. [DOI] [PubMed]
- 5.Lei ZL, Zhang LJ, Xu ZM, Dang H, Xu J, Lv S, et al. Endemic status of schistosomiasis in People's Republic of China in 2014. Chin J Schisto Control. 2015;27(6):563–569. [PubMed] [Google Scholar]
- 6.Lun ZR, Wu MS, Chen YF, Wang JY, Zhou XN, Liao LF, et al. Visceral leishmaniasis in China: an endemic disease under control. Clin Microbiol Rev. 2015;28(4):987–1004. doi: 10.1128/CMR.00080-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Song L, Wu X, Ren J, Gao Z, Xu Y, Xie H, et al. Assessment of the effect of treatment and assistance program on advanced patients with schistosomiasis japonica in China from 2009 to 2014. Parasitol Res. 2016;115(11):4267–4273. doi: 10.1007/s00436-016-5207-y. [DOI] [PubMed] [Google Scholar]
- 8.Song LG, Wu XY, Sacko M, Wu ZD. History of schistosomiasis epidemiology current status and challenges in China: on the road to schistosomiasis elimination. Parasitol Res. 2016;115(11):4071–4081. doi: 10.1007/s00436-016-5253-5. [DOI] [PubMed] [Google Scholar]
- 9.Xia ZG, Wang RB, Wang DQ, Feng J, Zheng Q, Deng CS, et al. China-Africa cooperation initiatives in malaria control and elimination. Adv Parasitol. 2014; doi: 101016/b978-0-12-800869-000012-3. [DOI] [PMC free article] [PubMed]
- 10.Hyseni L, Atkinson M, Bromley H, Orton L, Lloyd-Williams F, McGill R, et al. The effects of policy actions to improve population dietary patterns and prevent diet-related non-communicable diseases: scoping review. Eur J Clin Nutr. 2016. doi: 101038/ejcn2016234. [DOI] [PMC free article] [PubMed]
- 11.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yin YL. Thoughts on the current state of human parasitology teaching. Basic Med Educ. 2014;16(6):419–421. [Google Scholar]
- 13.Ji MJ, Wu GL. A historical reflect on the disciplinary development of human parasitology. Chin J Parasitol Parasit Dis. 2009;27(5):448–454. [PubMed] [Google Scholar]
- 14.Qin YH, Cui Y, Ren YX, Dai XD, Zheng LL. Discussion of scientific advances in parasitology and problems encountered during the integration of pathogenic biology in China. J Pathog Biol. 2013. doi: 1013350/jcjpb201303007. (in Chinese).
- 15.Cheng MS. Shorten class hours and deepen educational reform of parasitology. Chin J Med Educ. 1999;2:46. [Google Scholar]
- 16.World Health Organization. Global report for research on infectious diseases of poverty. 2012. http://apps.who.int/iris/bitstream/10665/44850/1/9789241564489_eng.pdf. Accessed 2 June 2015.
- 17.Hong Q, Feng J, Liu H, Li X, Gong L, Yang Z, et al. Prevalence of Spirometra mansoni in dogs, cats, and frogs and its medical relevance in Guangzhou, China. Int J Infect Dis. 2016;53:41–45. doi: 10.1016/j.ijid.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Lv S, Zhang Y, Steinmann P, Zhou XN. Emerging angiostrongyliasis in mainland China. Emerg Infect Dis. 2008;14(1):161–164. doi: 10.3201/eid1401.061529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tang ZL, Huang Y, Yu XB. Current status and perspectives of Clonorchis sinensis and clonorchiasis: epidemiology pathogenesis omics prevention and control. Infect Dis Poverty. 2016. doi: 101186/s40249-016-0166-1. [DOI] [PMC free article] [PubMed]
- 20.Zhou P, Chen N, Zhang RL, Lin RQ, Zhu XQ. Food-borne parasitic zoonoses in China: perspective for control. Trends Parasitol. 2008. doi: 101016/jpt200801001. [DOI] [PubMed]
- 21.Yan C, Liang LJ, Zheng KY, Zhu XQ. Impact of environmental factors on the emergence transmission and distribution of Toxoplasma gondii. Parasit Vectors. 2016. doi: 101186/s13071-016-1432-6. [DOI] [PMC free article] [PubMed]
- 22.Showler AJ, Wilson ME, Kain KC, Boggild AK. Parasitic diseases in travelers: a focus on therapy. Expert Rev Anti-Infect Ther. 2014;12(4):497–521. doi: 10.1586/14787210.2014.892827. [DOI] [PubMed] [Google Scholar]
- 23.Utzinger J, Becker SL, Knopp S, Blum J, Neumayr AL, Keiser J, et al. Neglected tropical diseases: diagnosis clinical management treatment and control. Swiss Med Wkly. 2012. doi: 104414/smw201213727. [DOI] [PubMed]
- 24.Qian MB, Utzinger J, Keiser J, Zhou XN. Clonorchiasis. Lancet. 2016;387(10020):800–810. doi: 10.1016/S0140-6736(15)60313-0. [DOI] [PubMed] [Google Scholar]
- 25.Bouvard V, Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, et al. A review of human carcinogens--Part B: biological agents. Lancet Oncol. 2009;10(4):321–322. doi: 10.1016/S1470-2045(09)70096-8. [DOI] [PubMed] [Google Scholar]
- 26.2016 Nationally Notifiable Infectious Diseases in China. 2017. http://www.nhfpc.gov.cn/jkj/s3578/201702/38ca5990f8a54ddf9ca6308fec406157.shtml. Accessed 23 Feb 2017. (in Chinses).
- 27.Chen YD, Zang P. Current situation of soil⁃transmitted nematodiasis monitoring in China and working keys in future. Chin J Schisto Control. 2015;02:111–114. [PubMed] [Google Scholar]
- 28.Cheng YZ, Xu LS, Chen BJ, Li LS, Zhang RY, Lin CX, et al. Survey on the current status of important human parasitic infections in Fujian province. Chin J Parasitol Parasit Dis. 2005;23(5):283–287. [PubMed] [Google Scholar]
- 29.Li L, Duan M, Jiang CD, et al. Analysis on misdiagnosis and missed diagnosis of 40 clonorchiasis cases. Ji Sheng Chong Bing Yu Gan Ran Xing Ji Bing. 2004;2:187–188. [Google Scholar]
- 30.Mandong BM, Madaki AJ. Missed diagnosis of schistosomiasis leading to unnecessary surgical procedures in Jos University Teaching Hospital. Trop Dr. 2005;35(2):96–97. doi: 10.1258/0049475054037011. [DOI] [PubMed] [Google Scholar]
- 31.Sun Q, Liu X, Hao Y, Li Y, Bai X, Wang F, et al. A misdiagnosis of clonorchiasis as gallstone leading to an unnecessary cholecystectomy: a case report. Am J Emerg Med. 2014. doi: 101016/jajem201404013. [DOI] [PubMed]
- 32.Xia Y, Ju Y, Chen J, You C. Cerebral paragonimiasis: a retrospective analysis of 27 cases. J Neurosurg Pediatr. 2015. doi: 103171/201410peds14208. [DOI] [PubMed]
- 33.Ye C, Tan S, Jiang L, Li M, Sun P, Shen L, et al. Endoscopic characteristics and causes of misdiagnosis of intestinal schistosomiasis. Mol Med Rep. 2013. doi: 103892/mmr20131648. [DOI] [PubMed]
- 34.Coordinating Office of the National Survey on the Important Human Parasitic Diseases A national survey on current status of the important parasitic diseases in human population. Chin J Parasitol Parasit Dis. 2005;23(Suppl 5):332–340. [PubMed] [Google Scholar]
- 35.Deng ZH, Fang YY. Epidemic situation and prevention and control strategy of clonorchiasis in Guangdong Province, China. Chin J Schisto Control. 2016;28(03):229–233. doi: 10.16250/j.32.1374.2016081. [DOI] [PubMed] [Google Scholar]
- 36.He FQ, Zhu SL. Treatment of 60 cases co-infected with hepatitis B virus and Clonorchis sinensis. Shi Yong Gan Zang Bing Za Zhi. 2000;5:114–115. [Google Scholar]
- 37.Harrington AT, Creutzfeldt CJ, Sengupta DJ, Hoogestraat DR, Zunt JR, Cookson BT. Diagnosis of neurocysticercosis by detection of Taenia solium DNA using a global DNA screening platform. Clin Infect Dis. 2009;48(1):86–90. doi: 10.1086/594128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.National Bureau Statistics of China. Annual national account by Province. 2015. http://data.stats.gov.cn/english/easyquery.htm?cn=E0103. Accessed Dec 2015.
- 39.Guangdong Provincial Statistics Bureau. 2015 Statistical Bulletin of National Economic and Social Development of Guangdong Province. 2016. http://www.gdstats.gov.cn/tjzl/tjgb/201605/t20160516_327975.html. Accessed 29 Feb 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.


