Abstract
Background
Scalp involvement is not directly evaluated in patients with dermatomyositis (DM). Therefore, the exact frequency of scalp dermatomyositis (SDM) and its clinical and trichoscopic characteristics have been poorly described.
Objective
The aim of this study was to determine the frequency and clinical and dermoscopic features of SDM in patients diagnosed with DM.
Methods
We performed a descriptive prospective, cross-sectional observational study that included all patients diagnosed with DM at a Mexican academic institute over the course of a year.
Results
Twenty-four out of 31 patients with DM had scalp involvement at clinical examination, with a prevalence of 77.4%. SDM was clinically characterized by erythema in all cases, scales in 20 (83.3%) patients, nonscarring alopecia in 21 (87.5%) patients, pruritus in 17 (70.8%) patients, and poikiloderma of the scalp in 16 (51.6%) patients. Twenty-eight patients were evaluated by trichoscopy. The most consistent finding was the presence of enlarged capillaries, found in 20 (71.4%) cases, followed by peripilar casts (57.1%) and tufting and interfollicular scales in 14 (50%) cases. Twenty-two patients also had positive nail fold capillaroscopic features similar to those observed by trichoscopy.
Limitations
The simple size was limited.
Conclusions
Scalp involvement and alopecia are common in patients with DM, and trichoscopy shows features similar to those found at capillaroscopy. Trichoscopy is a very important tool for diagnosis of scalp involvement in patients with DM.
Keywords: Dermatomyositis, Scalp dermatomyositis, Trichoscopy, Capillaroscopy, Alopecia, Itchy erythemato-squamous plaques
Introduction
Dermatomyositis (DM) is an autoimmune disease included in the inflammatory myopathies whose symptoms can be cutaneous, muscular, or systemic, and it can affect adults and children [1]. It is 2–3 times more common among females and has an incidence of 2–9 cases per million individuals [2, 3]. Hispanics have been found to have a higher frequency of DM compared to Caucasians, possibly because of their proximity to the equator and increased exposure to ultraviolet light [4].
Based on cutaneous findings and associations of DM with myopathy, neoplasms, or other connective tissue diseases, Stonecipher et al. [5] and Sontheimer [1] proposed a classification system that subdivides adult-onset DM into two entities: classic DM (CDM) and clinically amyopathic DM (CADM).
Both CDM and CADM have skin features that serve as classification criteria, including scalp dermatomyositis (SDM) [6]. To date, SDM with or without alopecia has been poorly characterized [7, 8]; however, SDM was shown to have a relatively high frequency, even if studies are relatively small (range: 28–82%) [9, 10, 11]. In addition to clinical changes that are observed by the naked eye, DM also causes vascular changes that have been extensively studied [12] by capillaroscopy of the proximal nail fold.
The aim of this study was to study the trichoscopic features of SDM, including the vascular patterns seen on the scalp.
Methods
The study was approved by the IRB committee (DER-1266-14/14-1). A prospective, cross-sectional observational study of 1 year duration was started at the Dermatology Department of the National Institute of Medical Sciences and Nutrition “Salvador Zubirán” in Mexico City. All patients with a diagnosis of CDM and CADM (with or without associated malignancy and/or other connective tissue diseases) fulfilling the criteria of Bohan's and Sontheimer's classification from June 2014 to June 2015 were included. Informed consent was obtained from all participants to participate in the study and have scalp clinical examination, scalp skin biopsy, and trichoscopic and capillaroscopic examination. A DermLite hybrid dermatoscope attached to an iPhone 6 camera was utilized to obtain scalp and proximal nail fold images.
Results
Thirty-one patients were included, with a mean age of 56 years (range: 27–68 years). Twenty-five patients were female (80.7%), and 6 patients were male (19.3%). The range of the duration of disease was 0–7 years, except for 1 patient, who was diagnosed with DM 14 years prior to enrollment in the study.
Twenty-seven patients were diagnosed with CDM, and the other 4 were diagnosed with CADM. In 5 patients, DM was associated with neoplasia (ovarian carcinoma in 2 patients, thyroid carcinoma in 2, and parathyroid adenoma in 1), and in 4 patients, DM was associated with connective tissue disease (systemic lupus erythematosus or mixed connective tissue disease).
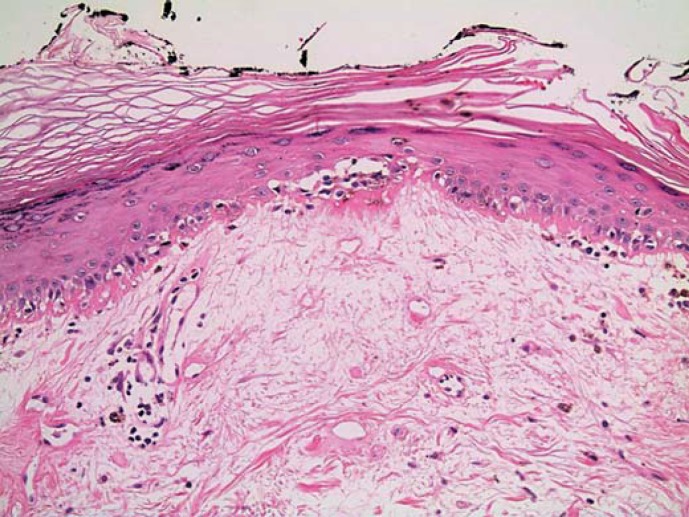
In 24 patients, SDM was evident on clinical examination, with a prevalence of 77.4%. SDM was characterized by erythema in all cases. Other symptoms included: scales (as erythemato-squamous plaques) in 20 (83.3%) patients, alopecia in 21 (87.5%) patients, pruritus in 17 (70.8%) patients, and scalp poikiloderma in 16 (51.6%) patients. No patient presented with calcinosis or ulceration. Eighteen patients (75%) had classical findings of a DM flare in association with SDM, and only 6 patients had scalp involvement as isolated symptom. Besides, 20 biopsies (64.5%) were performed, mostly finding interface dermatitis in all cases (Fig. 1).
Fig. 1.
Vertical skin biopsy, interface dermatitis; hyperkeratosis, atrophic epidermis, and telangiectasias.
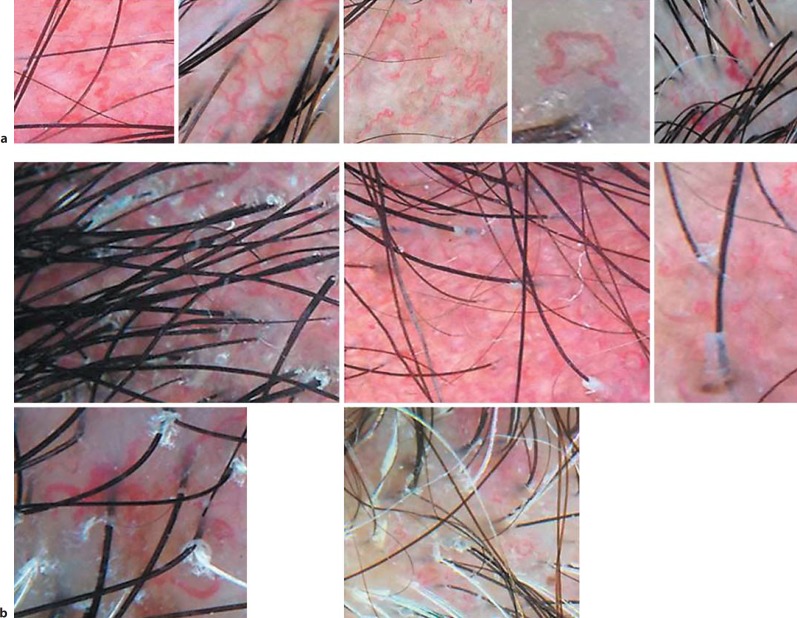
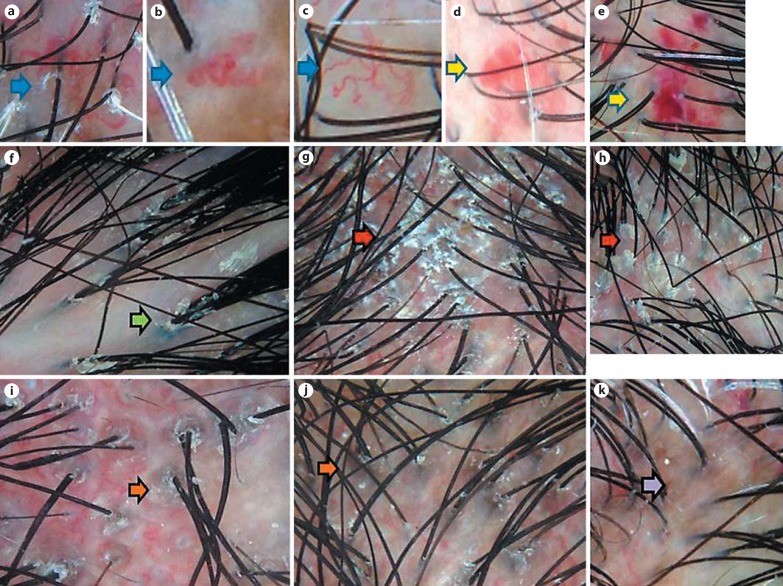
Trichoscopy images were available for 28 patients (see online supplementary Table 1, available at www.karger.com/doi/10.1159/000464469). The most common findings included enlarged tortuous capillaries and peripilar casts, which were both found in more than half of the cases (Fig. 2). Tufting with 3 or more hair shafts emerging together and interfollicular scales were also common. Other findings included bushy capillaries (similar to those observed in the proximal nail fold), interfollicular pigmentation, and perifollicular pigmentation. In 4 cases, we found vascular lake-like structures (defined as ectatic vascular structures filled with red blood cells) (Fig. 3).
Fig. 2.
Scalp dermatomyositis. Major trichoscopic features (seen in more than half of the cases). a Enlarged capillaries. b Peripilar cast.
Fig. 3.
Scalp dermatomyositis. Minor (less common) trichoscopic features. a-c Bushy capillaries (blue arrows). d, e Vascular, lake-like structures (yellow arrows). f Tufting (green arrow). g, h Interfollicular scale (red arrows). i, j Perifollicular pigmentation (orange arrows). k Interfollicular pigmentation (purple arrow).
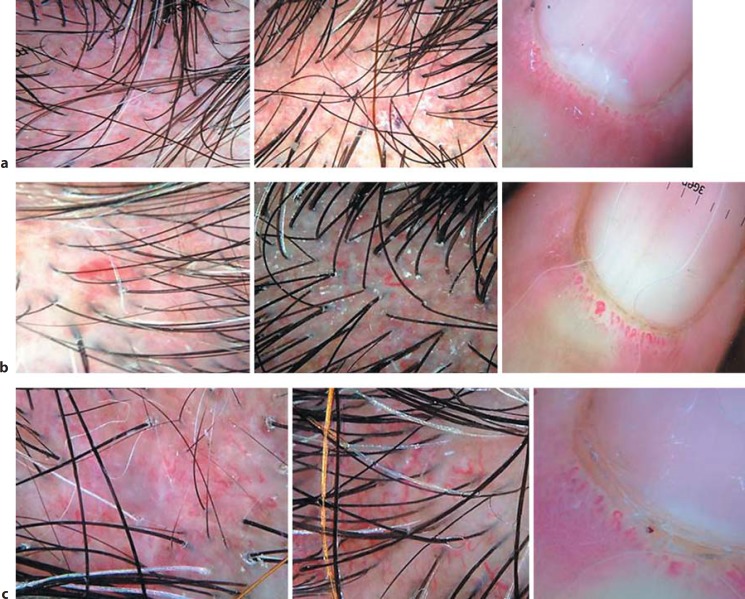
Capillaroscopy of the proximal nail fold showed capillary loss and enlarged and bushy capillaries in 22 patients (70%) (Fig. 4).
Fig. 4.
Trichoscopic and capillaroscopic correlation. a-c Trichoscopically enlarged capillaries and capillaroscopic lengthening.
Discussion
Although textbooks describe scalp itching and alopecia as important signs of DM, only a few studies focused on this topic. The first study on clinical features of SDM was published by Kasteler and Callen [10] in 1994. They described scalp involvement in 14 out of 17 patients with DM, defining SDM as diffuse erythematous and scaly plaques in addition to scalp poikiloderma and alopecia. Some patients had been previously diagnosed with psoriasis or seborrheic dermatitis (SD) because of scalp erythema and scaling. Six of the 14 patients had alopecia (43%), which was severe and nonscarring.
In 2009, Tilstra et al. [11] published a series of 24 patients with DM that included 15 patients with scalp involvement, among them 5 patients with nonscarring alopecia. There was female predominance for both the SDM and the nonscarring alopecia groups. This study included patients diagnosed with adult-onset DM, juvenile DM, and, particularly, CADM, which had a higher incidence of scalp involvement (66%). Additionally, some patients with SDM had associated connective tissue disorders, particularly lupus and scleroderma. They had no significant association with neoplasia (7–12%).
Gilliam and Prystowsky [13] reported focal and diffuse nonscarring alopecia in 10 out of 15 patients with mixed connective tissue disease.
There are no prospective studies on trichoscopy of SDM. However, books on scalp dermoscopy and reviews describe elongated and tortuous vessels with persistence of follicular openings and irregularly enlarged, giant vessels with root-like appearance and thick arborizing vessels with extravasations [14, 15].
In this study, we found that enlarged capillaries on trichoscopy are seen in most patients with DM regardless of the clinical evidence of scalp involvement. The enlarged scalp capillaries are often arborized with a tortuous shape. They may have the bushy appearance described in the nail fold. At pathology, enlarged capillaries correspond to vascular ectasia in the subpapillary dermis [14]. Other inflammatory diseases of the scalp may present prominent vessels, such as psoriasis and SD. However, the vascular patterns are very different. In psoriasis, vessels appear as red dots at low magnification and as twisted loops at high magnification. In SD, vessels have an arborizing pattern, similar to that seen in normal scalp, but are increased in number [14].
Peripilar casts appear as concentrically arranged scales encircling the hair shaft; these casts are commonly seen in dermoscopy of scarring alopecias including lichen planopilaris, frontal fibrosing alopecia, and discoid lupus erythematosus. SDM often shows this feature even if the alopecia is nonscarring. Patients with SDM may also present tufts of 2 or 3 hairs emerging together and surrounded by peripilar casts, as seen in lichen planopilaris or other scarring alopecia.
As SDM shows overlapping clinical features with SD, contact dermatitis, and psoriasis, it is possible that SDM patients are often misdiagnosed, especially those who do not have other signs of DM. Dermoscopy is very useful to indicate the right diagnosis in these cases.
Proximal nail fold capillaroscopy of our patients confirmed classical findings revealing capillary loss, altered capillary architecture, and presence of capillary hemorrhage [12]. It is interesting to notice the close similitudes between nail fold and scalp capillary changes, which have never been reported before. Proximal nail fold capillaroscopy abnormalities have been associated with disease activity and response to treatment [16], but we still do not know if the scalp capillary changes can also be modified by treatment.
SDM is an understudied manifestation of DM, as few reports have provided accurate information about its behavior. The number of patients included in previous studies in the literature is variable (10–24 patients, with the largest sample size in the study by Tilstra et al. [11]), and although our sample size was also small, our case series provides novel trichoscopic findings that are associated with SDM. In most SDM patients, cutaneous and flare disease was correlated with presence of positive trichoscopic features and pruritus was a symptom present in most patients (70.8%) on the other hand, 4 patients had positive trichoscopic features without clinical evidence of scalp involvement. In the experience of one of the authors (A.T.), trichoscopy findings suggested the diagnosis of DM in at least 3 patients who consulted for scalp itching, but they were not part of this study. Diagnosis was afterward confirmed by pathology.
Statement of Ethics
The study was approved by the IRB committee (DER-1266-14/14-1). Informed consent was obtained from all participants to participate in the study and have scalp clinical examination, scalp skin biopsy, and trichoscopic and capillaroscopic examination.
Disclosure Statement
The authors named above declare that they do not have any conflict of interest concerning this article.
Supplementary Material
Supplementary data
Acknowledgements
Project support/funding in part by The North American Hair Research Society.
References
- 1.Sontheimer R. Dermatomyositis: an overview of recent progress with emphasis on dermatologic aspects. Dermatol Clin. 2002;20:387–408. doi: 10.1016/s0733-8635(02)00021-9. [DOI] [PubMed] [Google Scholar]
- 2.Irazoque-Palazuelos F, Barragán-Navarro Y. Epidemiology, etiology and classification. Reumatol Clin. 2009;5((suppl 3)):2–5. doi: 10.1016/j.reuma.2009.09.007. [DOI] [PubMed] [Google Scholar]
- 3.Jorizzo JL. Dermatomyositis: practical aspects. Arch Dermatol. 2002;138:114–116. doi: 10.1001/archderm.138.1.114. [DOI] [PubMed] [Google Scholar]
- 4.Shamim EA, Rider LG, Pandey JP, O'Hanlon TP, Jara LJ, Samayoa EA, Burgos-Vargas R, Vazquez-Mellado J, Alcocer-Varela J, Salazar-Paramo M, Kutzbach AG, Malley JD, Targoff IN, Garcia-De la Torre I, Miller FW. Differences in idiopathic inflammatory myopathy phenotypes and genotypes between Mesoamerican Mestizos and North American Caucasians: ethnogeographic influences in the genetics and clinical expression of myositis. Arthritis Rheum. 2002;46:1885–1893. doi: 10.1002/art.10358. [DOI] [PubMed] [Google Scholar]
- 5.Stonecipher MR, Jorizzo JL, White WL, et al. Cutaneous changes of dermatomiositis in patients with normal muscle enzymes: dermatomiositis sine myositis? J Am Acad Dermatol. 1993;28:951–956. doi: 10.1016/0190-9622(93)70136-h. [DOI] [PubMed] [Google Scholar]
- 6.Yassaee M, Fiorentino D, Okawa J, Taylor L, Coley C, Troxel AB, Werth VP. Modification of the cutaneous dermatomyositis disease area and severity index, an outcome instrument. Br J Dermatol. 2010;162:669–673. doi: 10.1111/j.1365-2133.2009.09521.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dawkins MA, Jorizzo JL, Walker FO, et al. Dermatomyositis: a dermatology-based case series. J Am Acad Dermatol. 1998;38:397–404. doi: 10.1016/s0190-9622(98)70496-7. [DOI] [PubMed] [Google Scholar]
- 8.Oremovic L, Lugovic L, Vucic M, et al. Cicatricial alopecia as a manifestation of different dermatoses. Acta Dermatovenerol Croat. 2006;14:246–252. [PubMed] [Google Scholar]
- 9.Moghadam-Kia S, Franks AG., Jr Autoimmune disease and hair loss. Dermatol Clin. 2013;31:75–91. doi: 10.1016/j.det.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 10.Kasteler JS, Callen JP. Scalp involvement in dermatomyositis: often overlooked or misdiagnosed. JAMA. 1994;272:1939–1941. [PubMed] [Google Scholar]
- 11.Tilstra JS, Prevost N, Khera P. Scalp dermatomyositis revisited. Arch Dermatol. 2009;145:1062–1063. doi: 10.1001/archdermatol.2009.194. [DOI] [PubMed] [Google Scholar]
- 12.Hasegawa M. Dermoscopy findings of nail fold capillaries in connective tissue diseases. J Dermatol. 2011;38:66–70. doi: 10.1111/j.1346-8138.2010.01092.x. [DOI] [PubMed] [Google Scholar]
- 13.Gilliam JN, Prystowsky SD. Mixed connective tissue disease syndrome. Arch Dermatol. 1977;113:583–587. [PubMed] [Google Scholar]
- 14.Miteva M, Tosti A. Hair and scalp dermatoscopy. J Am Acad Dermatol. 2012;67:1040–1048. doi: 10.1016/j.jaad.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 15.Rudnicka L, Olszewska M, Rakowska A. Atlas of Trichoscopy. London: Springer; 2012. [Google Scholar]
- 16.Riccieri V, Vasile M, Macri V, Sciarra I, Stefanontoni K, De Luca N, Di Franco M, Spadaro A. Successful immunosuppressive treatment of dermatomyositis: a nailfold capillaroscopy survey. J Rheumatol. 2010;37:2. doi: 10.3899/jrheum.090841. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data