Abstract
Choriocarcinoma is a highly malignant neoplasm arising from the trophoblast of a human pregnancy, which may have distant spread to multiple organs, particularly to the lung. We report a case of a pulmonary arteriovenous fistula that developed after chemotherapy within a choriocarcinoma metastasis. A 24-year-old female with a history of uterine choriocarcinoma presented with multiple hypervascular pulmonary nodules on the initial chest computed tomography (CT) scan, consistent with lung metastases. Four months after chemotherapy, follow-up chest CT revealed a decrease in the size and vascularity of the lung metastases, except for 1 nodule that persisted with marked contrast enhancement and developed a communication with a pulmonary artery and vein. These findings were consistent with an acquired arteriovenous fistula. Physicians should be aware of the risk of acquired arteriovenous fistula in pulmonary metastases after chemotherapy because it can lead to a right-to-left shunt, pulmonary hemorrhage, and paradoxical emboli. It is also important for the definition of therapeutic planning, in order to avoid it being misdiagnosed as a site of disease progression.
Keywords: Choriocarcinoma metastasis, Acquired pulmonary arteriovenous fistula, Chemotherapy
Introduction
Choriocarcinoma is a rare malignant tumor, which may have distant spread to multiple organs, particularly to the lung. The most common thoracic manifestation of metastatic disease is multiple pulmonary nodules [1, 2]. Since the tumor has the potential to stimulate angiogenesis and other vascular changes, the metastases can show marked enhancement after intravenous contrast injection on computed tomography (CT) scans. In addition, metastatic nodules may be complicated by alveolar hemorrhage, which can be seen on CT as ground-glass opacities surrounding the pulmonary nodule.
These tumors are extremely sensitive to chemotherapy and have a high overall complete remission rate. The treatment response is monitored with serum human chorionic gonadotropin (HCG) levels, and the evaluation of distant metastases can be done with imaging examinations [1, 2]. We report a case of an acquired arteriovenous malformation in a pulmonary metastatic nodule from choriocarcinoma after favorable response to chemotherapy and normalization of HCG levels.
Case Presentation
A 24-year-old female with a history of uterine evacuation of a partial hydatidiform mole 2 months prior in another institution presented with an abdominal palpable mass and a progressively increasing serum HCG level. She had no other relevant medical history.
On admission, the serum HCG level was 110,925 mIU/mL. Pelvic magnetic resonance imaging (MRI) revealed a uterus didelphys with a heterogeneous, hypervascular, and T2-hyperintense mass in the endometrium of 1 of the uterine cavities, with invasion of the myometrium and extension to the left ovary. Chest CT revealed multiple metastatic hypervascular nodules in both lungs (Fig. 1), but no metastases were found in other organs on a positron emission tomography-CT scan and brain MRI.
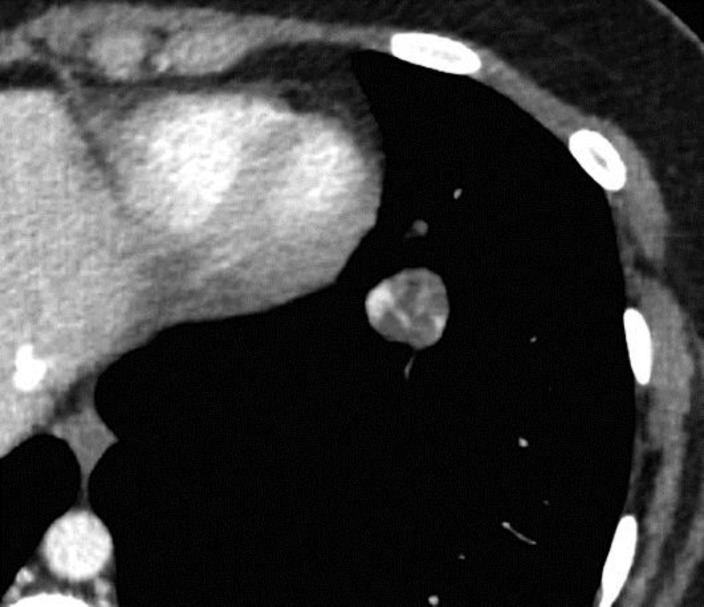
Fig. 1.
Axial chest computed tomography image in a 24-year-old female with metastatic choriocarcinoma. Initial enhanced chest computed tomography at presentation shows multiple solid pulmonary nodules with hyperenhancement after intravenous contrast.
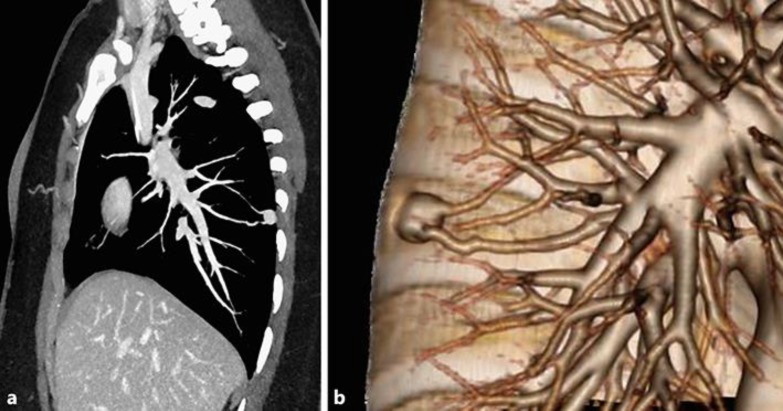
The patient started treatment with combined cisplatin and paclitaxel chemotherapy. Hysterectomy was performed 2 months after beginning the chemotherapy. After 5 months, she attained normal serum HCG levels (2 mIU/mL), with a normal physical examination and normal arterial oxygen saturation. Laboratory examination revealed a normal red and white cell count. At that time, the follow-up contrast-enhanced chest CT showed that the multiple metastatic pulmonary nodules had decreased in size and were no longer enhancing, except for 1 of them. This nodule also communicated with a subsegmental pulmonary artery and vein (Fig. 2a, Fig. 2b) suggesting an arteriovenous fistula, and the insignificant levels of serum HCG supported this diagnosis.
Fig. 2.
After 5 months of chemotherapy, the metastatic pulmonary nodules have decreased in size and are not enhancing, except for the nodule that developed arteriovenous fistula. A sagitally reformatted image with maximum intensity projection computed tomography (a) and a volume-rendered multidetector computed tomography image (b), showing communication of the nodule with the solitary feeding artery and a pulmonary draining vein, consistent with arteriovenous fistula.
Discussion
Gestational trophoblastic disease comprises a spectrum of disorders such as complete and partial hydatidiform moles, malignant invasive mole, choriocarcinoma, and placental site trophoblastic tumor/epithelioid trophoblastic tumor. The malignant forms are grouped under gestational trophoblastic neoplasia.
Choriocarcinoma usually develops months after the occurrence of a hydatidiform mole or abortion, or in intrauterine or ectopic pregnancies. The biomarker HCG is used for diagnosis and follow-up because levels are often elevated at initial diagnosis and in disease progression. The staging and prognosis of disease can be evaluated by a score, which considers features such as age, antecedent pregnancy, interval from index pregnancy, pretreatment HCG, tumor size, site and number of metastases, and prior failed chemotherapy. The detection of lung, liver, and brain metastasis is performed with chest X-ray or CT, abdominal ultrasound or CT, and brain MRI/CT [1, 2].
The lung is the most common site of metastatic disease [1], usually characterized by multiple rounded, hypervascular soft tissue density nodules, which can show surrounding ground-glass opacities (“halo sign”) on CT images reflecting alveolar hemorrhage due to the high vascularity of the lesions [3, 4]. It is also well documented that gestational trophoblastic diseases are associated with the development of uterine arteriovenous malformation [5], but the formation of arteriovenous shunts at another extrauterine site of spread, such as the lung, has been rarely reported [6, 7, 8, 9].
Choriocarcinomas are highly responsive to chemotherapy and have cure rates close to 100 and 75–90% in low-grade and high-grade tumors, respectively [1, 2]. There have been some cases of development of local arteriovenous shunts within or adjacent to metastases and persistence of these communications after treatment with chemotherapy [10, 11]. These patients can have complications such as right-to-left shunt, alveolar hemorrhage, hemoptysis, hemothorax, and paradoxical brain emboli. Arteriovenous malformations can be treated with angiographic procedures or surgery. After chemotherapy, residual nodules can be considered benign if the HCG levels are normal and no growth of the lesions is detected on serial imaging studies [12]. The identification of arteriovenous fistulas, although rare, is very important for the definition of clinical outcome of these patients and to avoid further complications.
Statement of Ethics
The authors have no ethical conflicts to declare.
Disclosure Statement
All authors declare that they have no conflicts of interest to disclose.
References
- 1.Hextan YS, Seckl MJ, Berkowitz RS, Xiang Y, Golfier F, Sekharan PK, Lurain JR. FIGO cancer report 2015: update on the diagnosis and management of gestational trophoblastic disease. Int J Gynecol Obstet. 2015;131:S123–S126. doi: 10.1016/j.ijgo.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Seckl MJ, Sebire NJ, Fisher RA, et al. Gestational trophoblastic disease: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24:vi39–vi50. doi: 10.1093/annonc/mdt345. [DOI] [PubMed] [Google Scholar]
- 3.Allen SD, Lim AK, Seckl MJ, Blunt DM, Mitchell AW. Radiology of gestational trophoblastic neoplasia. Clin Radiol. 2006;61:301–313. doi: 10.1016/j.crad.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 4.Martínez-Jiménez S, Rosado-de-Christenson ML, Walker CM, Kunin JR, Betancourt SL, Shoup BL, Pettavel PP. Imaging features of thoracic metastases from gynecologic neoplasms. Radiographics. 2014;34:1742–1754. doi: 10.1148/rg.346140052. [DOI] [PubMed] [Google Scholar]
- 5.Touhami O, Gregoire J, Noel P, Trinh XB, Plante M. Uterine arteriovenous malformations following gestational trophoblastic neoplasia: a systematic review. Eur J Obstet Gynecol Reprod Biol. 2014;181:54–59. doi: 10.1016/j.ejogrb.2014.07.023. [DOI] [PubMed] [Google Scholar]
- 6.Green JD, Carden TS, Jr, Hammond CB, Johnsru IS. Angiographic demonstration of arteriovenous shunts in pulmonary metastatic choriocarcinoma. Radiology. 1973;108:67–70. doi: 10.1148/108.1.67. [DOI] [PubMed] [Google Scholar]
- 7.McDonald-Burrows Z, Davies R, Goode E, Clarke C, Jackson J, Seckl M, Savage P. Haemoptysis from a pulmonary arteriovenous malformation in a post molar pregnancy gestational trophoblast tumour patient managed by radiological embolisation: a case report. J Med Case Rep. 2014;8:117. doi: 10.1186/1752-1947-8-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi SH, Goo JM, Kim H, Im J. Pulmonary Arteriovenous Fistulas Developed After chemotherapy of Metastatic Choriocarcinoma. AJR. 2003;181:1544–1546. doi: 10.2214/ajr.181.6.1811544. [DOI] [PubMed] [Google Scholar]
- 9.Bruzzi JF, Truong MT, Gladish GW, Wallace MJ, Moran CA, Munden RF. Development of pulmonary arteriovenous communications within pulmonary metastases after chemotherapy. J Thorac Oncol. 2007;2:243–246. doi: 10.1097/JTO.0b013e318031d086. [DOI] [PubMed] [Google Scholar]
- 10.Casson AG, McCormack D, Craig I, Inculet R, Levin L. A persistent pulmonary lesion after chemotherapy for metastatic choriocarcinoma. Chest. 1993;103:269–270. doi: 10.1378/chest.103.1.269. [DOI] [PubMed] [Google Scholar]
- 11.Murta EFC, Fatureto MC. Persisting metastatic pulmonar imaging after treatment of gestational trophoblastic disease. Rev Bras Ginecol Obstet. 1999;21:55–58. [Google Scholar]
- 12.Swett HA, Westcott JL. Residual non malignant pulmonary nodules in choriocarcinoma. Chest. 1974;65:560–562. doi: 10.1378/chest.65.5.560. [DOI] [PubMed] [Google Scholar]