Abstract
Context:
Women undergoing treatment for breast cancer often have psychological morbidity and body image difficulties. The risk factors for increased levels of stigma in women with breast cancer have not been adequately studied.
Aims:
This study aimed at investigating the associations of high levels of stigma in women with breast cancer.
Settings and Design:
This cross-sectional study was conducted in a comprehensive cancer center in India and recruited women (n = 134) undergoing surgical treatment for breast cancer.
Methods:
Body image difficulties, including stigma and affective symptoms, were quantified, alongside disease- and treatment-related variables using standardized questionnaires.
Statistical Analysis Used:
Univariate analysis followed by multivariate logistic regression was performed to find the risk factors of high levels of stigma related to body image.
Results:
In the univariate analysis, high levels of stigma were associated with lesser educational attainment (odds ratio [OR] =2.92, confidence interval [CI] 1.25–6.8, P = 0.01), breast conservation surgery (BCS) as opposed to mastectomy (OR = 4.78, CI 2.07–11.03, P < 0.001), having an anxiety disorder (OR = 2.4, CI 1.09–5.33, P = 0.03), and depression (OR = 3.08, CI 1.37–6.89, P < 0.01). On multivariate logistic regression, with stigma as the dependent variable, being less educated (adjusted OR [AOR] 3.08, CI 1.18–8.04, P = 0.02) and opting for BCS (AOR 6.12, CI 2.41–15.5, P < 0.001) were associated with higher stigma.
Conclusions:
Women with breast cancer should be screened for distress and stigma. Women opting for BCS may still have unmet emotional needs on completion of surgery and should have access to psychological interventions to address stigma, affective symptoms, and body image problems.
Keywords: Body image, breast cancer, cancer, depression, oncology, stigma
Introduction
The global burden of cancer study estimated that, in 2013, the incidence of breast cancer was 1.8 million worldwide. Although largely curable, breast cancer was the leading cause of disability-adjusted life years (DALYs, 13.1 million attributed to breast cancer).[1] Psychological stress, and its treatment in women with breast cancer, has been well studied.[2] However, the social construct of cancer varies enormously from one community to another, and sufferers, survivors, and family members may have different perceptions about the diagnosis of breast cancer and its potential impact on their lives, which may in turn influence choices about treatment.[3] Wide-ranging psychological issues which follow diagnosis of breast cancer include accepting the diagnosis, adjustment disorders, and anxiety, which may progress to clinical depression during treatment. Body image problems or stigma may persist even after treatment is completed.
Perceptions related to one's own body may impact on the woman's sense of identity, self-esteem, acceptance, sexuality, and also perceived stigma. More than half a century ago, Goffman defined stigma as an “attribute that is deeply discrediting.” Stigma reduces the person “from a whole and usual person to a tainted, discounted one.”[4] Over the years, experts have realized that stigma is not only related to society but also to the self-concept of the individual feeling stigmatized.[5] Body image dimensions of women with and without breast cancer are comparable, although it is likely that women with breast cancer have more distress.[6] In a study from the USA, on 546 women having breast cancer treatment, over half reported experiencing two or more body image problems some of the time, or at least one problem much of the time.[7] Two dimensions of body image after breast cancer have been described – affective and cognitive.[8] The affective dimension is associated with the feelings that a person has about her own body. The cognitive dimension, on the other hand, includes thoughts and beliefs associated with her body. These two dimensions can have a certain degree of overlap, and mismatch between the two can lead to stress and behavioral change and depression in women with breast cancer.[9] A study from Portugal reported that “shame” due to mastectomy increased over time.[10] A population-based study on public attitudes toward cancer survivors reported stigma related to the disease,[11] and stigma has also specifically been reported following breast cancer treatment in an Asian population.[3] However, this remains an understudied area. In this study, we report the findings of a research on perceived stigma and its associations with sociodemographic, affective symptoms, and treatment-related issues in women following surgery for breast cancer.
Methods
Setting
This study was conducted at a new cancer center in India with a multidisciplinary breast oncology team including surgeons, clinical and medical oncologists. A psycho-oncologist, psychologist, and a breast care nurse supported patients through the entire clinical course. The management of patients was discussed in weekly multidisciplinary meetings. If clinically feasible, patients and families were given a choice to opt for their preferred mode of surgical treatment to the breast, either breast conservation surgery (BCS) or mastectomy.
Participants
This study was approved by the Institutional Research Ethics Committee (EC/TMC/02/12) and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The study followed a cross-sectional study design. All women undergoing surgical treatment for breast cancer were eligible to be recruited. Potential study participants were approached, and the nature and purpose of the study were explained to them by the surgical team. All interviews were conducted by a trained registered clinical psychologist.
The only exclusion criterion was the presence of a significant medical condition other than cancer, which might unduly influence the outcome independent of cancer (e.g., previous cerebrovascular accident). Minor and chronic medical illnesses such as hypertension and diabetes were not considered to be reasons for exclusion, but the presence of such conditions was recorded.
Assessments
Assessments of stigma – The outcome variable
Stigma was quantified using body image using a breast cancer questionnaire,[12] which captures information on body image issues in women treated for breast cancer. The questionnaire has six subscales: stigma, vulnerability, transparency, arm concern, body concern, and limitation subscales.
Assessment of exploratory variables
Women were interviewed in the outpatient clinical setting, within the 1st month following surgery for breast cancer. Questionnaires were administered in private by the researcher, and data were collected in a predetermined sequence.
Personal information schedule: This included sociodemographic data regarding the patient's age, domicile, educational attainment, marital status, and being part of a joint versus a nuclear family
Disease- and treatment-related variables: Disease- and treatment-related variables were collected on a predesigned case report form. Medical comorbidities were also recorded for all participants
Hospital Anxiety and Depression Scale (HADS):[13] This is a well-validated instrument to quantify anxiety and depressive symptoms in medically ill patients. It has been used across cultures for patients suffering from breast cancer. A cutoff score on this scale of more than 8 (8/9) ensures inclusion of patients with possible anxiety and depression. The scale has been used by other researchers in India in the same language[14]
Body Image After Breast Cancer Questionnaire:[12] This questionnaire has been developed to capture body image issues in women with breast cancer. There are six subscales of this questionnaire: stigma, vulnerability, transparency, arm concern, body concern, and limitation subscales. Body Image After Breast Cancer Questionnaire was translated into the local vernacular language and back translated into English with permission of the author.
For patients who were unable to read, questions were read out by the researcher. This is an accepted research practice in the developing countries, ensuring that study participants are representative of the clinical population, which comes from a range of socioeconomic backgrounds.
Statistical analysis
Stigma score in the “Body Image After Breast Cancer” scale was predetermined as the main outcome variable. To explore the factors associated with high stigma, univariate analyses were conducted comparing “high perceived stigma” (top 25th percentile) as case group, with “lower perceived stigma,” in the bottom 75th percentile of the stigma score as control, giving a binary outcome. Exploratory variables tested for their association with stigma in the study were selected a priori. Multivariate logistic regression analysis was conducted with exploratory variables that were identified in univariate analysis and with the categorical stigma score as the dependent variable. Five domains were studied – (I) sociodemographic area, for example, age, level of education, domicile (rural vs. urban); (II) level of social support, for example, being in a marital relationship, being part of a joint/nuclear family system; (III) presence of other chronic medical conditions, for example, diabetes or hypertension; (IV) psychological health; and (V) cancer and its treatment-related factors.
Results
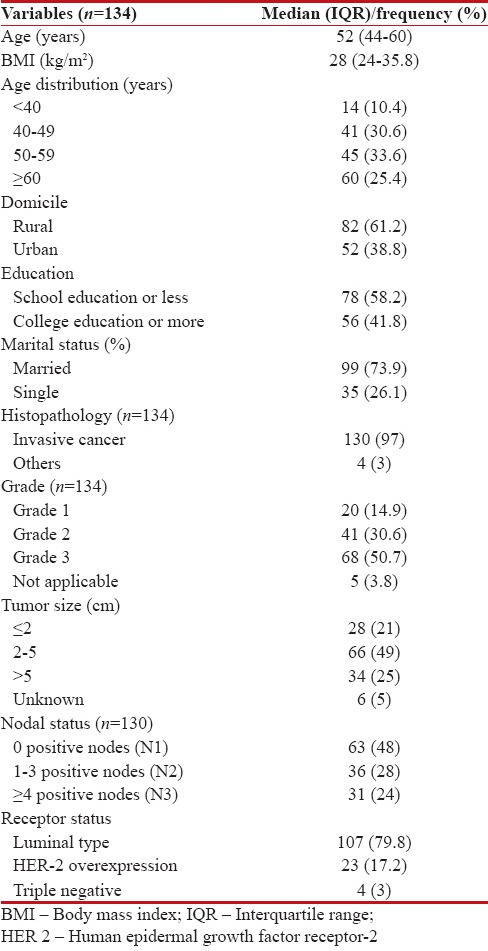
Women (n = 134) participating in the study had a median age of 52 years with an interquartile range (IQR) of 44–60 years. Of these 134 women, 72 (53.7%) had mastectomy and the rest had BCS. Although the option of breast reconstruction after mastectomy was available, none of the women in the study group had reconstruction. The patients recruited for the study had a median body mass index of 28 with an IQR of 24–35.8. The majority of participating women were married (73.9%) and had completed school education (78%). Forty-four (32.8%) women had neoadjuvant chemotherapy (NACT) before surgery and the rest of the women (n = 90), who constituted 67%, had upfront surgery. The majority of women (n = 117, 87%) had invasive ductal carcinoma. For women with invasive carcinoma, the histological Grade was I, II, and III in 14.9%, 30.6%, and 50.7%, respectively [Table 1].
Table 1.
Sample characteristics
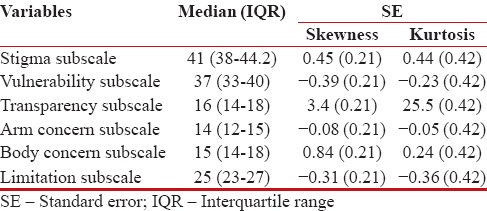
Shapiro–Wilk test (P > 0.05) and visual inspection of the histograms and Q–Q plots showed that stigma scores were not normally distributed. The median stigma score was 41, with an IQR of 38–44.2 [Table 2]. In the absence of any formal cutoff for stigma, the sample was divided into two groups based on the 25/75th percentile score. The top 25th percentile of stigma scores was considered to be representing women (n = 37) who felt high degrees of stigma. The women who perceived high stigma were compared with the rest of the sample of women recruited in the study.
Table 2.
Body image of women undergoing treatment for breast cancer
The exploratory variables chosen for analyses were based on the social construct of stigma and its cognitive-affective domains,[5] and information was collected on our data collection schedule. Sociodemographic information, disease status, degree of social support, and affective symptoms were used in exploratory analysis. Although age was not significantly associated with outcome in univariate analysis, this was considered in the multivariate model as it often works as a confounder in similar research. The histopathological characteristics and other pathological parameters were not included in further analysis as they would unlikely have any impact on perceived stigma.
In the univariate analysis, high levels of stigma were associated with lesser educational attainment (odds ratio [OR] =2.92, confidence interval [CI] 1.25–6.8, P = 0.01), BCS as opposed to mastectomy (OR = 4.78, CI 2.07–11.03, P < 0.001), higher anxiety score (OR = 2.4, CI 1.09–5.33, P = 0.03), and higher depression score (OR = 3.08, CI 1.37–6.89, P < 0.001) [Tables 3 and 4].
Table 3.
Univariate analysis for stigma
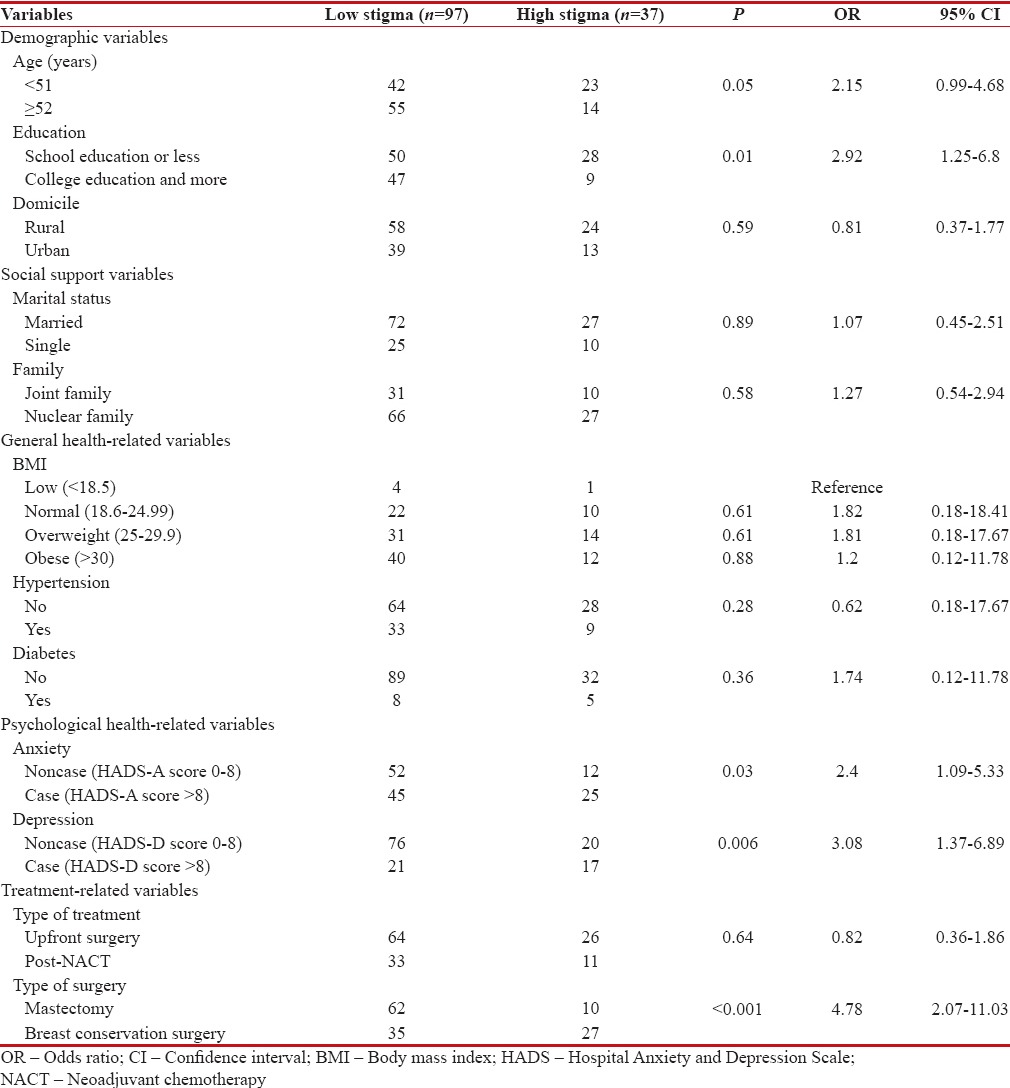
Table 4.
Multivariate analysis for stigma (logistic regression)
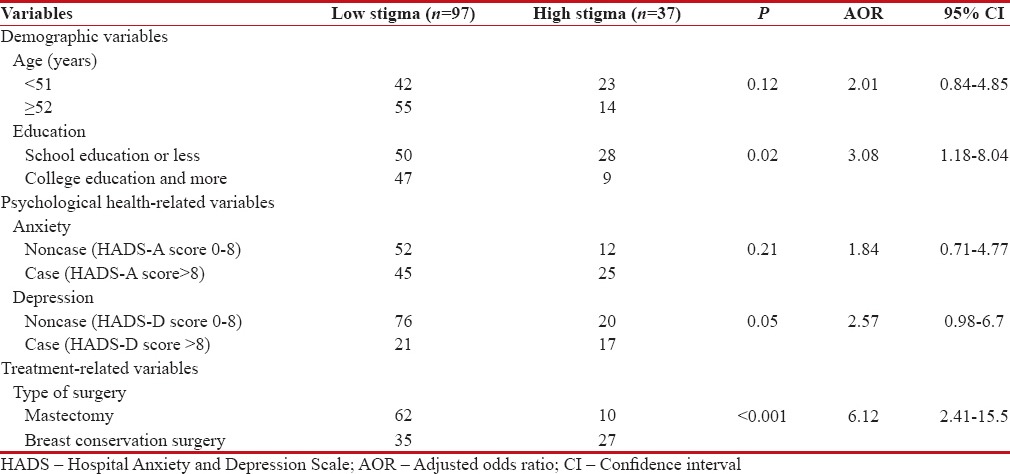
On multivariate logistic regression, with stigma as the dependent variable, being less educated (OR 3.08, CI 1.18–8.04, P = 0.02) was associated with higher self-perceived stigma. A perception of higher stigma was also significantly associated with opting for BCS (OR 6.12, CI 2.41–15.5, P < 0.01). In multivariate analysis, depression and anxiety in women undergoing surgical treatment for breast cancer were not significantly associated with stigma.
Discussion
In developing countries as opposed to the developed countries, breast cancer is often diagnosed at advanced stages. There are emerging reports that breast cancer survivors perceive stigma associated with the disease. A study from Thailand on stigma felt by women with breast cancer, reported that stigma was often associated with mis-attribution of cause and nature of the disease.[3] There are similar reports from South Africa.[15] These results are similar to those from the West[16] and were in the context of increased survivorship. The associations of stigma in breast cancer are understudied and more careful evaluation is required, both from a psycho-social perspective and at different points in the continuum of treatment. This study was planned to look at the associations of stigma around the time of decision-making about treatment options.
Women who had not received any formal education or were educated up to secondary school perceived high levels of stigma as compared to women who had been to college, even after controlling for other sociodemographic variables. There is literature on higher levels of education being related to better health awareness and less stigma in other countries.[17] However, the relationship of stigma with various social variables can be complex. In a recently published review on stigma against HIV, the reviewers noted that stigma is omnipresent against HIV-positive people even within health-care workers who are likely to be well educated and other sections of the society.[18]
Previous studies[19,20] have also reported increased stigma in younger patients. A possible explanation may be that a younger woman goes through constant social evaluations about her body and thus related issues are more distressing. In contrast, an older woman may have already experienced changes to her body and psychologically may be better equipped to deal with changes in appearance. Our results did not find a statistically significant association of stigma with age. However, this lack of association could be due to type 1 error or a small sample size.
In the current study, during univariate analysis, a high level of stigma was associated with depression and anxiety, based on the standard cutoff score on HADS. Previous research has shown that women with breast cancer are much more prone to develop depression, anxiety, and adjustment problems,[21] and these affective symptoms are more common in the 1st year after diagnosis.[22] In our study, the association of depression and stigma lost statistical significance in multivariate analysis once controlled for other factors. This is likely because stigma is a more social concept that starts much before anyone falls ill and is associated with the education of a woman.
The association of stigma with BCS was an unexpected finding, as published data suggest that mastectomy is commonly perceived as potentially more stigmatizing in women making breast cancer treatment decisions.[23] Most previous studies conclude that patients who underwent mastectomy experience more body image-related issues.[24,25] However, the data are not restricted to women having mastectomy, and in a study following BCS, 25% of women were found to have serious body image problems.[26] The current study was cross-sectional in design and did not include a presurgical assessment, so it was not possible to ascertain the direction of the association and it is not possible for us to comment if the perception of stigma following surgery was also present before choosing breast conservation. In the communities from which this study population is drawn, almost all women with operable breast cancer undergo mastectomy, and this was the expectation of most women and their families when they came for treatment. In this hospital, in contrast, breast conservation was discussed with all women with single, localized, well-defined tumors. If breast conservation was not possible at initial presentation, NACT was given with the intention of achieving it. Breast conservation either at presentation or following NACT was always a choice of the patient, and women who did not want to consider conservation, or were unwilling to have adjuvant radiotherapy, were offered mastectomy. Although postmastectomy reconstruction was available at the hospital, very few women and families were willing to even discuss this, as their primary focus was on treatment of the presenting cancer. It is possible that women who perceived high levels of stigma associated with the disease were more likely to choose to have BCS. A recent paper highlighted the preference of more normalizing treatment choices in patients with cancer in India and China even though they may not be the best options for the patient's long-term survival. The authors in this paper felt that this could be due to perceived stigma.[27] Our patients who undertook BCS may have decided on the treatment option as it was more normalizing and they were already feeling high levels of stigma. However, it is also possible that, due to the social construct of cancer in the developing countries, and also some increase in the cost of treatment associated with breast conservation, women who chose to have BCS were under social scrutiny and felt stigmatized.
The strengths of the present study include the recruitment of patients undergoing surgery in a single surgical unit, where the approach to information and treatment options was uniform. All interviews were conducted by a trained clinical psychologist. As the study was conducted in a newly built not-for-profit cancer hospital, women who participated in the study represented a wide socioeconomic group. Sample size, demographics, tumor stage, and age of the patients were representative of our current database of more than 1000 patients seen for curative breast surgery; however, the lack of follow-up interviews made it impossible for us to comment on the longitudinal nature of anxiety/depression and stigma over time.
BCS being related to stigma as found in the current study supports the idea that not only those who undergo mastectomy but also patients who opt for BCS have unmet social and emotional needs. We conclude that stigma is related to a complex social appraisal of cancer. It is associated with level of education and cannot be solely addressed by offering a choice of surgical technique. Along with discussions regarding preferred surgical treatment, women should also be assessed for perceived stigma, psychological morbidity, and have access to appropriate psycho-social interventions to clear any misconceptions. We propose that breast cancer clinics in developing countries should invest in training breast care nurses who would help women understand the nature of the disease and address any undue fears in the minds of the women who had completed treatment for breast cancer. In other words, the “tumor” should not be the only “target” in changing the predicament of the patient.
All patients undergoing treatment for breast cancer should undergo evaluation for unmet emotional needs. However, less educated women who choose to have BCS are at a particular risk of perceived stigma related to their body. If universal provision of psycho-social services is difficult due to resource constraints, the above factors should be kept in mind while screening for stigma and emotional distress in high-risk individuals. Identifying the most vulnerable group of patients in the population will help breast cancer survivors and inform health-care professionals to provide them support more effectively.
Future studies on the social aspects of cancer, especially stigma, are needed from developing countries who contribute maximally to the world's cancer burden. Stigma associated with breast cancer likely contributes to perception of wellness and impact on successful rehabilitation of this very vulnerable group of women. If cancer survivors have less stigma, they will be more open about their experiences of cancer treatment. The stories of hope may impact on other women accessing services earlier. As a research team, we are planning to explore how psycho-social variables impact on help seeking in women with cancer. If social and psychological barriers are tackled appropriately, it may have far-reaching consequences on cancer outcome in a country like India where many women present quite late even for potentially curable cancers such as breast cancer. Appropriate stigma reduction interventions should be tested using methodologically robust longitudinal research studies.
Financial support and sponsorship
This study was an investigator-initiated project and was supported by the Tata Medical Centre, Kolkata.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are indebted to Dr. Samiran Panda, Deputy Director of National Institute of Cholera and Enteric Diseases, Indian Council of Medical Research, for help with the statistical analysis and comments on an earlier draft of the paper.
References
- 1.Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, et al. The global burden of cancer 2013. JAMA Oncol. 2015;1:505–27. doi: 10.1001/jamaoncol.2015.0735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jassim GA, Whitford DL, Hickey A, Carter B. Psychological interventions for women with non-metastatic breast cancer. Cochrane Database Syst Rev. 2015;5:CD008729. doi: 10.1002/14651858.CD008729.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Suwankhong D, Liamputtong P. Breast cancer treatment: Experiences of changes and social stigma among Thai women in Southern Thailand. Cancer Nurs. 2016;39:213–20. doi: 10.1097/NCC.0000000000000255. [DOI] [PubMed] [Google Scholar]
- 4.Goffman E. Stigma: Notes on the Management of Spoiled Identity. Englewood Cliffs, NJ: Prentice Hall; 1963. [Google Scholar]
- 5.Link BG, Phelan JC. Conceptualising stigma. Annu Rev Sociol. 2001;27:363–85. [Google Scholar]
- 6.Resseguier N, Noguès C, Giorgi R, Julian-Reynier C. Psychometric properties of a French version of a Dutch scale for assessing breast and body image (BBIS) in healthy women. BMC Womens Health. 2013;13:24. doi: 10.1186/1472-6874-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fobair P, Stewart SL, Chang S, D’Onofrio C, Banks PJ, Bloom JR. Body image and sexual problems in young women with breast cancer. Psychooncology. 2006;15:579–94. doi: 10.1002/pon.991. [DOI] [PubMed] [Google Scholar]
- 8.Cash TF, Green GK. Body weight and body image among college women: Perception, cognition, and affect. J Pers Assess. 1986;50:290–301. doi: 10.1207/s15327752jpa5002_15. [DOI] [PubMed] [Google Scholar]
- 9.Teo I, Novy DM, Chang DW, Cox MG, Fingeret MC. Examining pain, body image, and depressive symptoms in patients with lymphedema secondary to breast cancer. Psychooncology. 2015;24:1377–83. doi: 10.1002/pon.3745. [DOI] [PubMed] [Google Scholar]
- 10.Moreira H, Canavarro MC. A longitudinal study about the body image and psychosocial adjustment of breast cancer patients during the course of the disease. Eur J Oncol Nurs. 2010;14:263–70. doi: 10.1016/j.ejon.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Shim HY, Shin JY, Kim JH, Kim SY, Yang HK, Park JH. Negative public attitudes towards cancer survivors returning to work: A nationwide survey in Korea. Cancer Res Treat. 2016;48:815–24. doi: 10.4143/crt.2015.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baxter NN, Goodwin PJ, McLeod RS, Dion R, Devins G, Bombardier C. Reliability and validity of the body image after breast cancer questionnaire. Breast J. 2006;12:221–32. doi: 10.1111/j.1075-122X.2006.00246.x. [DOI] [PubMed] [Google Scholar]
- 13.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 14.Sanyal J, Das S, Ghosh E, Banerjee TK, Bhaskar LV, Rao VR. Burden among Parkinson's disease care givers for a community based study from India. J Neurol Sci. 2015;358:276–81. doi: 10.1016/j.jns.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Mutebi M, Edge J. Stigma, survivorship and solutions: Addressing the challenges of living with breast cancer in low-resource areas. S Afr Med J. 2014;104:383. doi: 10.7196/samj.8253. [DOI] [PubMed] [Google Scholar]
- 16.Bell K. The breast-cancer-ization of cancer survivorship: Implications for experiences of the disease. Soc Sci Med. 2014;110:56–63. doi: 10.1016/j.socscimed.2014.03.031. [DOI] [PubMed] [Google Scholar]
- 17.Holman D. Exploring the relationship between social class, mental illness stigma and mental health literacy using British national survey data. Health (London) 2015;19:413–29. doi: 10.1177/1363459314554316. [DOI] [PubMed] [Google Scholar]
- 18.Chambers LA, Rueda S, Baker DN, Wilson MG, Deutsch R, Raeifar E, et al. Stigma, HIV and health: A qualitative synthesis. BMC Public Health. 2015;15:848. doi: 10.1186/s12889-015-2197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bloom JR, Stewart SL, Chang S, Banks PJ. Then and now: Quality of life of young breast cancer survivors. Psychooncology. 2004;13:147–60. doi: 10.1002/pon.794. [DOI] [PubMed] [Google Scholar]
- 20.Moyer A, Salovey P. Psychosocial sequelae of breast cancer and its treatment. Ann Behav Med. 1996;18:110–25. doi: 10.1007/BF02909583. [DOI] [PubMed] [Google Scholar]
- 21.Karakoyun-Celik O, Gorken I, Sahin S, Orcin E, Alanyali H, Kinay M. Depression and anxiety levels in woman under follow-up for breast cancer: Relationship to coping with cancer and quality of life. Med Oncol. 2010;27:108–13. doi: 10.1007/s12032-009-9181-4. [DOI] [PubMed] [Google Scholar]
- 22.Burgess C, Cornelius V, Love S, Graham J, Richards M, Ramirez A. Depression and anxiety in women with early breast cancer: Five year observational cohort study. BMJ. 2005;330:702. doi: 10.1136/bmj.38343.670868.D3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Waljee JF, Ubel PA, Atisha DM, Hu ES, Alderman AK. The choice for breast cancer surgery: Can women accurately predict postoperative quality of life and disease-related stigma? Ann Surg Oncol. 2011;18:2477–82. doi: 10.1245/s10434-011-1582-x. [DOI] [PubMed] [Google Scholar]
- 24.Lasry JC, Margolese RG, Poisson R, Shibata H, Fleischer D, Lafleur D, et al. Depression and body image following mastectomy and lumpectomy. J Chronic Dis. 1987;40:529–34. doi: 10.1016/0021-9681(87)90010-5. [DOI] [PubMed] [Google Scholar]
- 25.Montebarocci O, Lo Dato F, Baldaro B, Morselli P, Rossi NC. Anxiety and body satisfaction before and six months after mastectomy and breast reconstruction surgery. Psychol Rep. 2007;101:100–6. doi: 10.2466/pr0.101.1.100-106. [DOI] [PubMed] [Google Scholar]
- 26.Sneeuw KC, Aaronson NK, Yarnold JR, Broderick M, Regan J, Ross G, et al. Cosmetic and functional outcomes of breast conserving treatment for early stage breast cancer 2. Relationship with psychosocial functioning. Radiother Oncol. 1992;25:160–6. doi: 10.1016/0167-8140(92)90262-s. [DOI] [PubMed] [Google Scholar]
- 27.Goss PE, Strasser-Weippl K, Lee-Bychkovsky BL, Fan L, Li J, Chavarri-Guerra Y, et al. Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. 2014;15:489–538. doi: 10.1016/S1470-2045(14)70029-4. [DOI] [PubMed] [Google Scholar]


