Abstract
Background:
The Latarjet procedure is commonly performed in the setting of glenoid bone loss for treatment of recurrent anterior shoulder instability; however, little is known regarding the outcomes of this procedure in elite American football players.
Purpose:
(1) Determine the prevalence, clinical features, and imaging findings of elite college football athletes who present to the National Football League (NFL) Combine with a previous Latarjet procedure and (2) describe these athletes’ performance in the NFL in terms of draft status and initial playing time.
Study Design:
Case series; Level of evidence, 4.
Methods:
After review of all football players who participated in the NFL Combine from 2009 to 2016, any player with a previous Latarjet procedure was included in this study. Medical records, position on the field, and draft position were recorded for each player. In addition, imaging studies were reviewed to determine fixation type, hardware complications, and status of the bone block. For those players who were ultimately drafted, performance was assessed based on games played and started, total snaps, and percentage of eligible snaps in which the player participated during his rookie season.
Results:
Overall, 13 of 2617 (<1%) players at the combine were identified with a previous Latarjet procedure. Radiographically, 8 of 13 (61%) showed 2-screw fixation, while 5 of 13 (39%) had 1 screw. Of the 13 players, 6 (46%) players demonstrated hardware complications. All players had evidence of degenerative changes on plain radiographs, with 10 (77%) graded as mild, 1 (8%) as moderate, and 2 (15%) as severe according to the Samilson Prieto classification. Six of the 13 (46%) players went undrafted, while the remaining 7 (54%) were drafted; however, no player participated in more than half of the plays for which he was eligible during his rookie season.
Conclusion:
Only a small percentage of players at the NFL Combine (<1%) had undergone a Latarjet procedure. High rates of postoperative complications and radiographically confirmed degenerative change were observed. Athletes who had undergone a Latarjet procedure demonstrated a variable amount of playing time, but none participated in more than half of their eligible plays during their rookie season.
Keywords: football (American), National Football League, shoulder instability, Latarjet, injury rate
Anterior shoulder instability is common in contact athletes, particularly in American football players.11,12 Nearly 10% of players at the National Football League (NFL) Scouting Combine present with a history of shoulder dislocation or subluxation.3 Moreover, shoulder stabilization surgery is the fourth most common procedure documented at the combine, with 4.7% of incoming NFL players reporting a prior shoulder stabilization procedure.3 A history of shoulder instability or recurrent instability may have a negative impact on a prospective NFL football player’s career, as demonstrated by Brophy et al,4,6 who reported that offensive and defensive linemen with known instability have a decreased chance of playing in the NFL.
In the setting of anterior shoulder instability with significant bone loss, the Latarjet procedure is widely advocated as the treatment of choice. This procedure has demonstrated excellent long-term outcomes, particularly in contact sport athletes. One recent study reported that rugby players who underwent the Latarjet procedure had no recurrence of subluxation or dislocation at a mean follow-up of 12 years.14 In contrast, high rates of recurrent instability have been reported following arthroscopic and open Bankart reconstruction in this same population: 89% and 38%, respectively.7,15
Despite the documented success of the Latarjet procedure, little is known regarding its prevalence or its effect on performance in elite football players. The purposes of this study were (1) to determine the prevalence and imaging findings of elite college football athletes who presented to the NFL Scouting Combine with a previous Latarjet procedure and (2) to describe the impact of this procedure on these players’ early career performances in the NFL.
Methods
This study was approved by both the institutional review board (Partners Human Research Committee, protocol No. 2015P002224/MGH) and the NFL Physician Society Research Committee. A retrospective review of all participants at the NFL Scouting Combine from 2009 through 2016 was conducted. Inclusion criteria consisted of any prospective NFL player who underwent medical and performance testing at the NFL Scouting Combine who demonstrated evidence of a previous Latarjet procedure based on a history completed at the combine. In addition, all radiographic imaging dictations were reviewed and screened for mention of hardware in the proximity of the glenohumeral joint. Any mention of hardware led to a thorough screening of all radiographic imaging for the respective player to determine whether a Latarjet procedure had been performed. As part of the review, medical records, imaging, position played, and draft position were recorded for each player who underwent a Latarjet procedure. Furthermore, radiographic findings were collected from standard imaging studies performed at the combine, including the anteroposterior (AP) and axillary views, and were analyzed for the following characteristics: position of the bone block, type and number of screws used for fixation, presence of hardware complications, resorption of the bone block, and degenerative changes. Degenerative changes were graded as mild, moderate, or severe based on the criteria previously established by Samilson and Prieto.16
For those patients with computed tomography (CT) scans, location and amount of bone resorption as well as the degree of bone block union with the native glenoid bone were assessed. Location of resorption was documented using a modified version of the bone block partitioning first described by Giacomo et al,8 with division of the bone block into 6 sections instead of the original 8: medial or lateral, inferior or superior, and deep or superficial, excluding proximal or distal. In addition, relationship of hardware to the bone block was recorded using a classification put forth by Zhu et al17: Grade 0 indicates that the screw head is completely buried in the bone block, grade I indicates that only the screw head is exposed outside the bone graft, grade II indicates that a portion of the screw shaft in addition to the screw head is exposed, and grade III indicates that the screw in its entirety is exposed with nearly total bone graft resorption and minimal to no bony contact between the graft and native glenoid neck.
To assess the performance of those athletes who were ultimately drafted, the following measures were analyzed during each athlete’s rookie season: total number of games in which the athlete participated, number of games started, total number of snaps played, and snap percentage, which was defined as number of snaps played divided by total number of snaps for which that player was eligible—in other words, the team’s total number of offensive snaps for offensive players or total number of defensive snaps for defensive players.
Results
Demographics
Of the 2617 players who participated in the NFL Combine between 2009 and 2016, 13 (<1%) were identified who had a history of Latarjet surgery. Eight of these played defense, including 5 defensive backs, 2 linebackers, and 1 defensive lineman. Five played offense, including 2 wide receivers, 2 offensive linemen, and 1 running back. Six of the 13 (46%) players went undrafted, and the remaining 7 (54%) were drafted from the third to the seventh round. The positions of those players drafted included 3 defensive backs, 2 linebackers, 1 running back, and 1 wide receiver.
Fixation Method and Plain Radiographic Findings
All 13 players who had undergone a Latarjet procedure before presenting at the NFL Scouting Combine had plain shoulder radiographs available for review, including AP and axillary views. In 7 players, the Latarjet procedure served as the primary procedure for treatment of recurrent instability (Figure 1). Five players underwent the Latarjet procedure after 1 prior surgery, and 1 player had 2 prior surgeries before ultimately undergoing the Latarjet procedure. Seven players had 2-screw constructs, while the remaining 6 players had 1 screw for fixation of the coracoid bone block (Table 1). Hardware complications, including screw breakage, bending, and pullout, were observed in 6 of 13 players, of which 3 specifically suffered screw pullout (Figure 2 and Table 1). All 13 players showed evidence of degenerative change on the humeral head and/or the glenoid, although the majority of players had mild degenerative changes (77%). Table 1 summarizes all radiographic findings of these 13 players.
Figure 1.
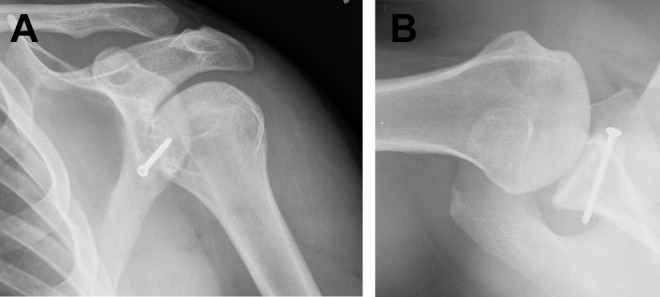
(A) Anteroposterior and (B) axillary views of the left shoulder showing coracoid bone block fixation with a single cortical screw. The hardware appears to be well engaged. Subtle evidence of bony resorption is seen on the axillary image as well as mild degenerative changes with sclerosis, flattening of the humeral head, and cystic change in the glenoid.
TABLE 1.
Radiographic Characteristics of All 13 NFL Prospective Players Who Previously Underwent the Latarjet Procedurea
| Player | No. of Surgeries | No. of Screws | Type of Screw | Bicortical Screws | Hardware Complication | Screws Pulled Out | Bone Resorption on Axial Radiograph | Degenerative Changes |
|---|---|---|---|---|---|---|---|---|
| 1 | 1 | 1 | Cannulated, partially threaded | Yes | No | Yes | Yes | Mild |
| 2 | 3 | 1 | Cortical, fully threaded | Yes | No | No | Yes | Mild |
| 3 | 1 | 1 | Cannulated, partially threaded | No | No | No | Yes | Mild |
| 4 | 2 | 2 | Cannulated, partially threaded | Yes | No | Yes | Yes | Severe |
| 5 | 2 | 2 | Cannulated, fully threaded | Yes | Yes—bent screw | No | Yes | Severe |
| 6 | 1 | 1 | Cannulated, partially threaded | Yes | Yes—broken screw | No | Yes | Moderate |
| 7 | 1 | 2 | Cannulated, fully threaded | No | Yes—broken screw | Yes | Yes | Mild |
| 8 | 2 | 2 | Cortical, fully threaded | Yes | No | No | Yes | Mild |
| 9 | 2 | 1 | Cannulated, partially threaded | No | Yes—bent screw | No | No | Mild |
| 10 | 1 | 1 | Cortical, fully threaded | Yes | No | No | No | Mild |
| 11 | 1 | 2 | Cannulated, fully threaded | Yes | No | No | Yes | Mild |
| 12 | 1 | 2 | Cannulated, fully threaded | Yes | No | No | Yes | Mild |
| 13 | 2 | 2 | Cannulated, partially threaded | Yes | No | No | No | Mild |
aBased on radiographic analysis as well as the total number of surgeries each player had undergone, including the Latarjet procedure.
Figure 2.
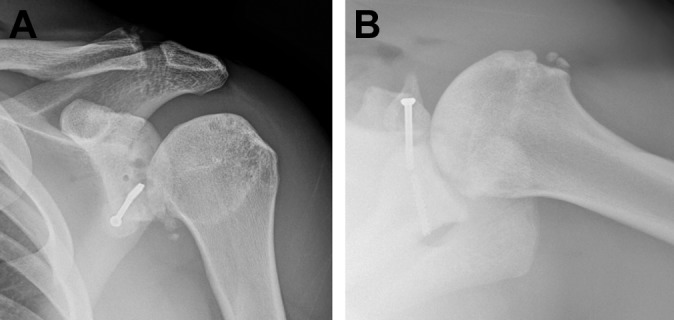
(A) Anteroposterior and (B) axillary views of the left shoulder demonstrate 1 cannulated partially threaded screw used for fixation of the coracoid bone block. The screw is broken, with notable evidence of degenerative changes and incomplete healing as well as bony resorption of the graft.
Bone Resorption and Healing on Computed Tomography Imaging
Eight of the 13 players had undergone CT scans, which were available for review from NFL Scouting Combine imaging archives. Table 2 demonstrates the radiographic characteristics of the 8 players with CT scans. With regard to position of the bone block, 6 players had the coracoid fixed to the anterior inferior glenoid or 3- to 5-o’clock position, while the other 2 players had slightly more anterior placement on the glenoid rim with 2- to 4-o’clock positioning (Table 2). In the axial plane, 6 players had their bone block positioned slightly lateral to the native glenoid, while the remaining 2 players had their bone block placed flush. Notably, all 8 of the athletes with CT scans had evidence of bony resorption of the bone block on CT imaging. Three of the 8 (38%) players showed evidence of minimal resorption (<25%), while the remainder (62%) demonstrated moderate to nearly complete resorption. Analysis of the interaction of the hardware and the bone block as described by Zhu et al17 showed that 5 players had grade I findings, 2 players had grade II, and 1 player had grade III. Quantifying the percentage of the bone block with confirmed bony bridging to the native glenoid demonstrated that 2 athletes had essentially 0% bridging and only 1 athlete featured complete 100% bony bridging (Table 2). Of the 2 athletes with 0% bony healing, 1 athlete had screw pullout and the other did not have any radiographic hardware complications. Figures 3 and 4 demonstrate examples of the CT imaging that was reviewed.
TABLE 2.
Radiographic Analysis of the 8 Players Who Underwent Latarjet Who Had a CT Scan From the NFL Combine Available for Review
| Player | Position of Bone Block (clock face) | Position of Bone Block (medial, optimal, lateral) | Amount of Resorption on CT, % | Location of Resorption on CT | Classificationb | % Bony Bridging/Healing |
|---|---|---|---|---|---|---|
| 1 | 3 to 5 | Lateral | 50 | Lateral; superior; superficial and deep | II | 50 |
| 3 | 3 to 5 | Lateral | 50 | Lateral; superior; deep | I | 0 |
| 4 | 3 to 5 | Lateral | 90 | Lateral; superior; deep | III | 0 |
| 5 | 2 to 4 | Lateral | 75 | Lateral; inferior; superficial | II | 50 |
| 9 | 3 to 5 | Optimal | 10 | Medial; inferior; superficial | I | 90 |
| 11 | 3 to 5 | Lateral | 40 | Lateral; inferior; deep | I | 70 |
| 12 | 2 to 4 | Lateral | 25 | Lateral; inferior; deep | I | 80 |
| 13 | 3 to 5 | Optimal | 25 | Medial; inferior; superficial and deep | I | 100 |
aCT, computed tomography; NFL, National Football League.
bClassification according to Zhu et al.17 Grade 0: screw head is completely buried in the bone block. Grade I: screw head is exposed outside the bone graft. Grade II: screw shaft in addition to the screw head is exposed. Grade III: screw is exposed, nearly all of the bone graft is resorbed, and no bone is left in contact with the glenoid neck.
Figure 3.
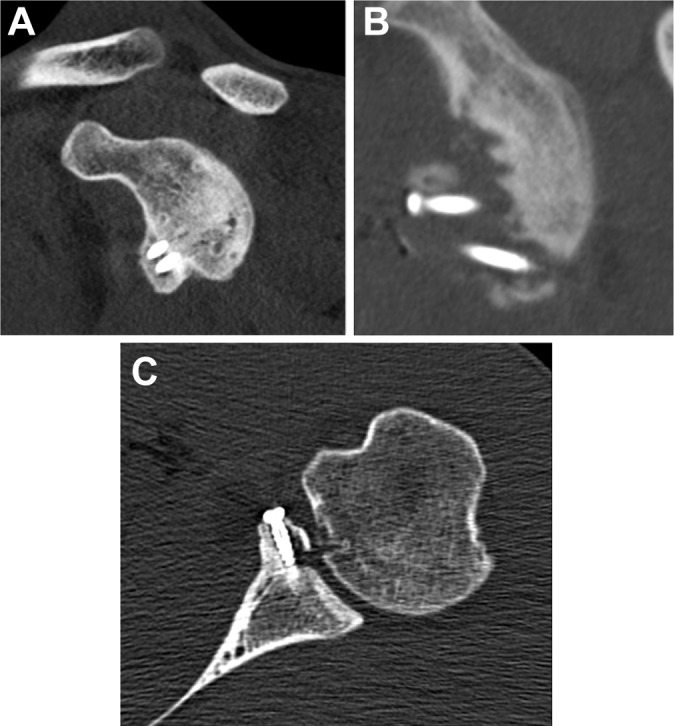
(A) Sagittal 2-dimensional reconstruction of the left shoulder demonstrates the coracoid bone block in an optimal position, with nearly 100% bony bridging to the glenoid. Hardware is in place with minimal bone resorption. (B) Sagittal 2-dimensional reconstruction of the left shoulder of a different athlete that demonstrates significant bony resorption of the bone block. (C) Axial 2-dimensional image of the left shoulder that shows the bone block to be flush with the native glenoid with hardware in place but shows evidence of bony resorption lateral to the screw located within the bone block.
Figure 4.
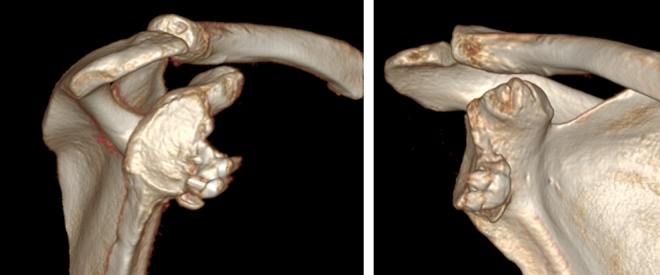
A 3-dimensional reconstruction with humeral subtraction of the right shoulder of an athlete with a previous Latarjet procedure. The bone block appears well positioned and the hardware is engaged. However, there is evidence of bony resorption lateral to the inferior screw in the bone block with additional evidence of degenerative change of the glenoid.
Performance Outcomes
Of the 13 players, 7 (54%) were subsequently selected in their respective NFL draft. Five of the 7 players participated in games during their rookie season, with only 1 player taking part in all 16 of his team’s games. Although 4 of the 7 players did participate in more than 75% of all games for an NFL season, none featured a snap percentage above 50% during their first season of eligible play in the NFL. In other words, no player was included in more than half of the plays for which he was eligible for his respective team. Of the remaining 3 athletes, 2 did not appear in a single game, and the third athlete played in 3 games during his rookie season. In terms of snap percentage, all 3 of these players had values below 1%, demonstrating minimal to no play during their rookie seasons. Table 3 shows the performance metrics analyzed for those players who had a history of Latarjet and who were drafted.
TABLE 3.
Volume of Play Measures During the Players’ Rookie Season
| Player | Drafted (Round) | Games Started, n | Games Played, n | Total Snaps, n | Snap Percentagea |
|---|---|---|---|---|---|
| 1 | Yes (7) | 3 | 16 | 383 | 37.9 |
| 2 | Yes (4) | 7 | 13 | 517 | 47.8 |
| 3 | Yes (7) | 2 | 15 | 228 | 20.2 |
| 4 | No | ||||
| 5 | No | ||||
| 6 | Yes (6) | ||||
| 7 | No | 0 | 0 | 0 | 0 |
| 8 | Yes (4) | ||||
| 9 | Yes (7) | 4 | 13 | 543 | 48.6 |
| 10 | No | 0 | 0 | 0 | 0 |
| 11 | Yes (3) | ||||
| 12 | No | 0 | 3 | 1 | 0.10 |
| 13 | No |
aPercentage of eligible snaps played (offense or defense).
Discussion
The most important finding of this study was that players with a history of the Latarjet procedure had a high rate of postoperative complications, including hardware failure (of note, 46% of the players had only had 1 screw used for fixation), radiographic degenerative joint changes, and bone block resorption. In addition, half of the players with a history of a Latarjet procedure were drafted. Those drafted had variable amounts of playing time based on games played and started and snap percentage. Overall, the Latarjet procedure was rarely performed (<1% of all athletes) in the players at the NFL Combine.
Despite such a low prevalence of the Latarjet procedure in this study population, the risk of shoulder dislocation and recurrent instability is known to be high for contact sport athletes.5,11,12 Brophy et al3,5 reported that 10% of players at the NFL Scouting Combine presented with a history of some form of shoulder instability and that shoulder stabilization surgery was documented in 4.7% of all players entering the NFL Combine. High instability recurrence rates have been reported in contact athletes with bony defects treated with Bankart repairs, and hence Bankart repair alone is not recommended.7 Burkhart and De Beer7 evaluated 194 consecutive arthroscopic Bankart repairs, including those in 101 contact athletes, and found a 6.5% recurrence rate for those athletes without a structural bone defect versus an 89% recurrence rate for those with bony defects at a mean follow-up of 27 months. In contrast, several authors have reported success following bone transfer procedures involving the glenohumeral joint in contact athletes.1,2,10,14 Beranger et al2 reported that all of the 47 athletes examined in their study returned to sports after Latarjet-Bristow, although those individuals who practiced overhead sports were less likely to return to preinjury levels. The Latarjet procedure is popularly performed in Europe for treatment of recurrent anterior shoulder instability in contact athletes, while the procedure is less frequently performed in the United States. As a result, comparisons between studies on this procedure from these 2 global regions are difficult because of the differences in the treatment approach.
In the present study, 6 of the 13 players with a history of a Latarjet procedure (46%) had hardware complications, which included 2 with broken hardware, 2 with bent screws, and 2 with screw pullout. All 13 players had evidence of degenerative changes on their plain radiographs, although the majority (10/13, 77%) had mild changes. These degenerative changes may be attributed to recurrent instability episodes before or after the procedure that occurred as a result of postoperative complications. Bone resorption was common; all 8 players who had undergone a CT examination demonstrated some degree of bone resorption, and 62% of these had moderate to complete resorption. In addition, nonunion was observed in 2 of these 8 athletes. Griesser et al9 reported a similarly high 30% complication rate after the Latarjet-Bristow procedure in a systematic review that included 45 studies (1904 shoulders) at a mean clinical follow-up of 6.8 years. The authors found a non-union rate of 9.1% and reported a 7% reoperation rate, 35% of which consisted of removal of symptomatic hardware. Mizuno et al13 found a 20% prevalence of arthritis in a retrospective review of 68 shoulders at a mean follow-up of 20 years after a Latarjet procedure. Allain et al1 reported a higher prevalence of glenohumeral arthritis, 71%, at a mean follow-up of 14 years. As demonstrated by Griesser et al,9 nonunion of the coracoid bone block to the native bone is a known complication of the Latarjet procedure; however, no correlation exists between healing rate and symptoms. Giacomo et al8 similarly noted a high prevalence of osteolysis of the coracoid graft in a CT evaluation of 26 patients. The authors found osteolysis most frequently at the proximal, superficial aspect of the coracoid bone block but did not find any correlation between degree of osteolysis and clinical findings. Given the demands placed on American football athletes, this may result in a higher complication rate, as we have reported, than other previous reports with lesser high-risk patients.
In this study, 7 of the 13 players with a history of a Latarjet procedure were ultimately drafted into the NFL. Given the small number of athletes in this study, resulting from the rarity of this procedure in incoming NFL prospects, conclusions cannot be drawn regarding the effect of Latarjet on these players’ performance. However, previous evidence of a history of shoulder instability has been associated with a negative effect on the career of a football player.5 In particular, of these athletes, none demonstrated a snap percentage greater than 50%, meaning that these players participated in less than half of eligible plays for their respective teams. Four of the 7 had snap percentages between 20% and 50%. As opposed to snap percentage, games started and games played have previously been used as measures of playing time and performance in prior studies.5 However, analysis of number of snaps played might provide a more sophisticated interpretation of playing time. In this case series, 4 players participated in 13 or more games during their rookie seasons, but none of these athletes had snap percentages greater than 50%, which suggests that analyzing only their number of appearances in games may overestimate their participation. Further studies with larger numbers of players are needed to verify the utility of recording number of snaps and snap percentage as opposed to number of games started and played.
We acknowledge some limitations to this study. It is retrospective in nature and therefore bound by the restraints associated with this study design. Furthermore, all data were collected at the NFL Combine, which is a process that has not been proven to be without error. No clinical examination findings, which may have affected subsequent in-league performance, including persistent laxity and loss of shoulder range of motion, were collected. This report also did not distinguish between preoperative function prior to Latarjet or varying surgeons and surgical techniques. In addition postoperative care for these athletes after their Latarjet procedures was not examined or compared. Given the rarity of this procedure and the small patient number included in this study, no definitive conclusions can be made regarding the effect of these radiographic findings on player performance or clinical outcomes. Furthermore, no control group was used for comparison to the Latarjet cohort and, as such, no definitive conclusions can be drawn regarding the effect of the Latarjet procedure on these players’ participation or performance. Despite these limitations, our findings in this report may be useful for both players and NFL team physicians and organizations in guiding and counseling incoming NFL athletes who have undergone the Latarjet procedure.
Conclusion
Only a small percentage (<1%) of players at the NFL Combine from 2009 to 2016 had undergone a Latarjet procedure. High rates of postoperative complications and a high prevalence of radiographic degenerative changes of the glenohumeral joint were observed after a Latarjet procedure. Athletes who had undergone a Latarjet procedure had a variable amount of playing time during their rookie seasons, but none participated in more than half of the plays for which he was eligible.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.T.P. receives royalties from Arthrex and SLACK Inc and is a paid consultant for Arthrex and the Joint Restoration Foundation (AlloSource). R.F.L. receives royalties from Arthrex, Ossur, and Smith & Nephew; is a paid consultant for Arthrex, Ossur, and Smith & Nephew; and receives research support from Arthrex, Linvatec, Ossur, and Smith & Nephew. M.D.P. is a paid consultant for Arthrex and DePuy-Mitek.
Ethical approval for this study was obtained from Partners Human Research Committee (protocol No. 2015P002224/MGH).
References
- 1. Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80(6):841–852. [DOI] [PubMed] [Google Scholar]
- 2. Beranger JS, Klouche S, Bauer T, Demoures T, Hardy P. Anterior shoulder stabilization by Bristow-Latarjet procedure in athletes: return-to-sport and functional outcomes at minimum 2-year follow-up. Eur J Orthop Surg Traumatol. 2016;26(3):277–282. [DOI] [PubMed] [Google Scholar]
- 3. Brophy RH, Barnes R, Rodeo SA, Warren RF. Prevalence of musculoskeletal disorders at the NFL Combine—trends from 1987 to 2000. Med Sci Sports Exerc. 2007;39(1):22–27. [DOI] [PubMed] [Google Scholar]
- 4. Brophy RH, Chehab EL, Barnes RP, Lyman S, Rodeo SA, Warren RF. Predictive value of orthopedic evaluation and injury history at the NFL Combine. Med Sci Sports Exerc. 2008;40(8):1368–1372. [DOI] [PubMed] [Google Scholar]
- 5. Brophy RH, Gill CS, Lyman S, Barnes RP, Rodeo SA, Warren RF. Effect of shoulder stabilization on career length in National Football League athletes. Am J Sports Med. 2011;39(4):704–709. [DOI] [PubMed] [Google Scholar]
- 6. Brophy RH, Lyman S, Chehab EL, Barnes RP, Rodeo SA, Warren RF. Predictive value of prior injury on career in professional American football is affected by player position. Am J Sports Med. 2009;37(4):768–775. [DOI] [PubMed] [Google Scholar]
- 7. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. [DOI] [PubMed] [Google Scholar]
- 8. Giacomo GD, Costantini A, de Gasperis N, et al. Coracoid bone graft osteolysis after Latarjet procedure: a comparison study between two screws standard technique vs mini-plate fixation. Int J Shoulder Surg. 2013;7(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Griesser MJ, Harris JD, McCoy BW, et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: a systematic review. J Shoulder Elbow Surg. 2013;22(2):286–292. [DOI] [PubMed] [Google Scholar]
- 10. Joshi MA, Young AA, Balestro J-C, Walch G. The Latarjet-Patte procedure for recurrent anterior shoulder instability in contact athletes. Orthop Clin North Am. 2015;46(1):105–111. [DOI] [PubMed] [Google Scholar]
- 11. Kaplan LD. Prevalence and variance of shoulder injuries in elite collegiate football players. Am J Sports Med. 2005;33(8):1142–1146. [DOI] [PubMed] [Google Scholar]
- 12. Leclere LE, Asnis PD, Griffith MH, Granito D, Berkson EM, Gill TJ. Shoulder instability in professional football players. Sports Health. 2013;5(5):455–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mizuno N, Denard PJ, Raiss P, Melis B, Walch G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J Shoulder Elbow Surg. 2014;23(11):1691–1699. [DOI] [PubMed] [Google Scholar]
- 14. Neyton L, Young A, Dawidziak B, et al. Surgical treatment of anterior instability in Rugby Union players: clinical and radiographic results of the Latarjet-Patte procedure with minimum 5-year follow-up. J Shoulder Elbow Surg. 2012;21(12):1721–1727. [DOI] [PubMed] [Google Scholar]
- 15. Roberts SN, Taylor DE, Brown JN, Hayes MG, Saies A. Open and arthroscopic techniques for the treatment of traumatic anterior shoulder instability in Australian rules football players. J Shoulder Elbow Surg. 1999;8(5):403–409. [DOI] [PubMed] [Google Scholar]
- 16. Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am. 1983;65(4):456–460. [PubMed] [Google Scholar]
- 17. Zhu Y-M, Jiang C-Y, Lu Y, Li F-L, Wu G. Coracoid bone graft resorption after Latarjet procedure is underestimated: a new classification system and a clinical review with computed tomography evaluation. J Shoulder Elbow Surg. 2015;24(11):1782–1788. [DOI] [PubMed] [Google Scholar]


