Abstract
Context:
Taping is commonly used in the management of several musculoskeletal conditions, including patellofemoral pain syndrome (PFPS). Specific guidelines for taping are unknown.
Objective:
To investigate the efficacy of knee taping in the management of PFPS. Our hypothesis was that tension taping and exercise would be superior to placebo taping and exercise as well as to exercise or taping alone.
Data Sources:
The PubMed/MEDLINE, Cochrane, Rehabilitation and Sports Medicine Source, and CINAHL databases were reviewed for English-language randomized controlled trials (RCTs) evaluating the efficacy of various taping techniques that were published between 1995 and April 2015. Keywords utilized included taping, McConnell, kinesio-taping, kinesiotaping, patellofemoral pain, and knee.
Study Selection:
Studies included consisted of RCTs (level 1 or 2) with participants of all ages who had anterior knee or patellofemoral pain symptoms and had received nonsurgical management using any taping technique.
Study Design:
Systematic review.
Level of Evidence:
Level 2.
Data Extraction:
A checklist method was used to determine selection, performance, detection, and attrition bias for each article. A quality of evidence grading was then referenced using the validated PEDro database for RCTs. Three difference comparison groups were compared: tension taping and exercise versus placebo taping and exercise (group 1), placebo taping and exercise versus exercise alone (group 2), and tension taping and exercise versus taping alone (group 3).
Results:
Five RCTs with 235 total patients with multiple intervention arms were included. Taping strategies included McConnell and Kinesiotaping. Visual analog scale (VAS) scores indicated improvement in all 3 comparison groups (group 1: 91 patients, 39% of total, mean VAS improvement 44.9 [tension taping + exercise] vs 66 [placebo taping + exercise]; group 2: 56 patients, 24% of total, mean VAS improvement 66 [placebo taping + exercise] vs 47.6 [exercise alone]; and group 3: 112 patients, 48% of total, mean VAS improvement 44.9 [tension taping + exercise] vs 14.1 [taping alone]).
Conclusion:
This systematic review supports knee taping only as an adjunct to traditional exercise therapy for PFPS; however, it does not support taping in isolation.
Keywords: patellofemoral pain syndrome, taping, McConnell, Kinesiotaping
Patellofemoral pain syndrome (PFPS) is a common musculoskeletal problem characterized by anterior knee pain, especially in adolescents and young adults.18 Patients often describe escalation of symptoms with ascending and descending stairs, squatting, running, or prolonged sitting, as these activities increase the compressive loading forces at the patellofemoral joint.14 Nonoperative measures including a comprehensive physical therapy program, are the first-line treatment. Physical therapy regimens include a mix of therapeutic modalities, manual techniques, exercise therapy, and knee-taping techniques with the goal of reducing pain, restoring muscular balance, and reestablishing functional activities and/or athletic endeavors.7,16,20 The purpose of this study was to analyze the literature to provide clinical recommendations regarding appropriate use of taping for pain modulation or performance enhancement.
Methods
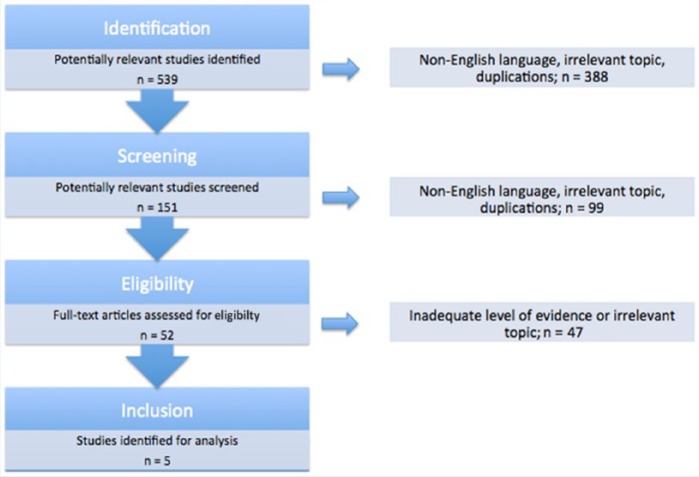
A systematic review method was used based on the framework outlined by Wright et al.19 A systematic literature search of PubMed/MEDLINE, CINAHL, Rehabilitation and Sports Medicine Source, and the Cochrane databases was performed for articles published from 1995 to April 2015. The risk of bias and quality of evidence grading was determined using the PEDro database. This combination search strategy employed the following keywords: (“kinesiotape” OR “kinesiotaping” OR “taping” OR “tape”) AND (“knee” OR “knees” OR “patellofemoral”). This search identified 539 articles, which were narrowed to 7 English-language, randomized controlled trials (RCTs) (Figure 1) after review of titles and abstracts using the following inclusion criteria by 2 independent reviewers:
Figure 1.
Article selection.
Design: Studies at the level of RCTs (level 1 or 2 evidence)
Participants: All ages with anterior knee or patellofemoral pain symptoms
Intervention: Nonsurgical management of knee injury using any taping technique
Comparison: No taping or placebo taping
Outcomes: Pain
Non–English language studies were excluded. Quality was independently assessed by 2 authors using the PEDro Scale (Appendix 1, available in the online version of this article).
Data Extraction and Summary
Selected articles were reviewed by 2 authors, and data were extracted and recorded using a customized Google form. The following categories of information were extracted for each article: objective, study design, study population, intervention group, control group, and outcome (including results, metrics, and statistics). Articles were grouped into 3 categories based on the control group used in the study design. A checklist method hierarchy to determine selection, performance, detection, and attrition bias was used for each article. A quality of evidence grading was then referenced using the validated PEDro database for RCTs. A systematic grading using the PEDro scale was performed for any RCTs that were not currently included in the database. A weighted mean (based on number of patients per paper) was used to report aggregate mean values for outcomes. It was not possible to report P values as some studies did not report a full set of data or the standard deviations of the mean for their study groups.
Three comparison groups were defined: tension taping and exercise versus placebo taping and exercise (group 1), placebo taping and exercise versus exercise alone (group 2), and tension taping and exercise versus taping alone (group 3).
Results
A total of 235 participants from 5 studies with mean age of 28.79 years (range, 14-50 years) were included in this systematic review. Of the 235 participants analyzed, 35% were men (Table 1). The time to follow-up ranged from 45 minutes after taping application to 1 year after intervention. Taping strategies included kinesiology taping (53 participants, 23% of total) (Figure 2) and McConnell (182 participants, 77% of total) techniques (Figure 3). Taping techniques were evaluated alone or in conjunction with physical therapy. All 7 articles evaluated pain using visual analog scales (VAS) (Table 2).
Table 1.
Patient demographics
| Studies, n | 5 |
| Patients, n | 235 |
| Male sex, n (%) | 82 (34.89) |
| Mean age, y | 28.79 |
| Age range, y | 14-50 |
| Follow-up, range | 45 min–1 y |
Figure 2.
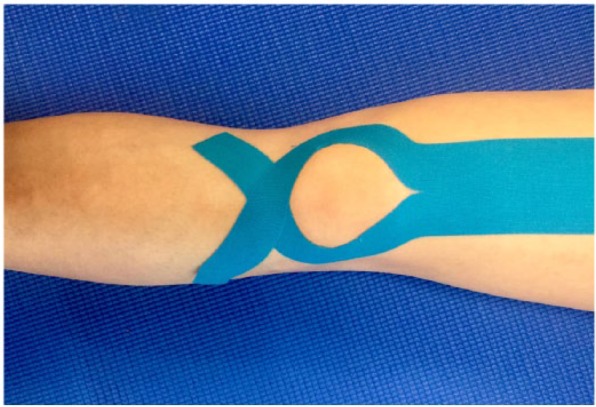
Kinesiology taping technique.
Figure 3.
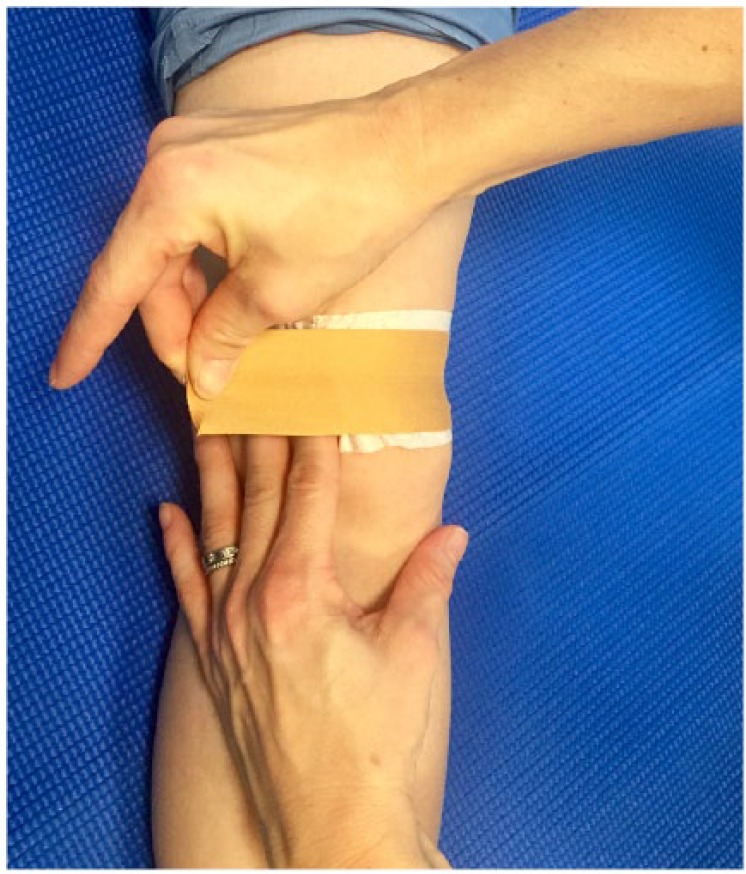
The McConnell taping technique involves pulling the patella medially with the tape.
Table 2.
Summary of individual studies
| Study | Study Type (Level of Evidence) | Study Population | Intervention | Outcome |
|---|---|---|---|---|
| Whittingham et al17 | RCT (level 1) | 30 Army recruits (17-25 years old) referred for physiotherapy by unit medical officers with a diagnosis of acute PFPS | Group 1: McConnell-type anterior taping applied to affected knee. Daily patellofemoral rehabilitation exercises performed under supervision. Group 2: Placebo McConnell-type patellar taping applied to the affected knee. Daily patellofemoral rehabilitation exercise performed under supervision. Group 3: Exercise program alone. |
There were statistically significant improvements in pain (VAS) for all groups at 2-, 3-, and 4-week assessments. The group receiving McConnell-type patellar taping and exercises had no pain at 4 weeks. No difference existed between placebo taping + exercise group and the exercise alone group at any time point. |
| Aytar et al2 | Randomized, double-blind study (level 1) | 22 patients (24.1 ± 3.2 years) with the diagnosis of PFPS | Group 1: Kinesiotaping. Group 2: Placebo Kinesiotaping (without tension). Both groups underwent outcome measurement assessment before and 45 minutes after tape application. |
There were no significant differences between groups regarding intensity of pain (VAS) after application of the Kinesiotape. |
| Clark et al4 | RCT (level 1) | 81 subjects (16-40 years old) with anterior knee pain | Group 1: Exercise, McConnell-type patellar taping, and education. Group 2: Exercise and education. Group 3: McConnell-type patellar taping and education. Group 4: Education alone. |
All groups showed significant improvements in pain (VAS) scores; however, these improvements did not vary significantly between the 4 groups at 3 months and 1 year. |
| Crossley et al5 | Randomized, double-blind study (level 1) | 71 subjects (14-40 years old) with diagnosis of PFPS | Group 1: Standardized physical therapy protocol including McConnell-type patellar taping. Group 2: Sham ultrasound and placebo McConnell-type patellar taping (without tension). |
The physical therapy group demonstrated significantly greater reduction in pain scores (VAS) for mean pain and worst pain than did the placebo group at 6 weeks. |
| Akbas et al1 | RCT (level 1) | 31 women (17-50 years old) with the diagnosis of PFPS | Group 1: Kinesiotaping plus muscle strengthening and soft tissue stretching. Group 2: No taping. Muscle strengthening and soft tissue stretching. |
At 6 weeks, significant improvements were found for pain (VAS) in both groups at rest and with activities. There were no significant differences between groups. |
PFPS, patellofemoral pain syndrome; RCT, randomized controlled trial; VAS, visual analog scale.
Pain was assessed using VAS in all 5 studies, which is a common method used to evaluate pain severity on a 0- to 100-mm scale (Table 3). Noninterventional or sham modalities were included in 1 study5; however, they were not assessed as a distinct treatment modality in our analysis.
Table 3.
Results by study design
| Demographics |
VAS Score Improvement |
|||||
|---|---|---|---|---|---|---|
| Group | Design | Patients (n) | % Total | Intervention | Control | |
| 1 | Tension taping + exercise | Placebo taping + exercise | 91 | 38.72 | 44.90 | 66.00 |
| 2 | Placebo taping + exercise | Exercise alone | 56 | 23.83 | 66.00 | 47.90 |
| 3 | Tension taping + exercise | Tension taping alone | 112 | 47.66 | 44.90 | 14.10 |
VAS, visual analog scale.
Tension Taping and Exercise vs Placebo Taping and Exercise (Group 1)
Four studies1,4,5,17 were included in the analysis (91 patients, 39% of total), with superior improvements found with the combination of placebo taping and exercise therapy (66 vs 44.90).
Placebo Taping and Exercise vs Exercise Alone (Group 2)
This analysis (56 patients, 24% of total) included 3 studies,1,4,17 and found larger reductions in pain scores with the combination of placebo taping and exercise (66.0 vs 47.6).
Tension Taping and Exercise vs Tension Taping Alone (Group 3)
All 5 studies1,2,4,5,17 (112 patients, 48% of total) found a mean VAS improvement, although it was greater when exercise was incorporated (44.9 vs 14.1).
Discussion
PFPS is highly prevalent in the athletic population. The etiology of pain may be multifactorial, resulting from anatomic, mechanical, and training factors. Patients may present with a diverse array of symptoms and clinical examination findings, including muscular weaknesses or imbalances, flexibility deficits, biomechanical flaws, and/or training errors. While knee taping is ubiquitous in the management of PFPS, providers often question its utility.
Various taping techniques exist, including McConnell taping, infrapatellar taping, Kinesiotaping, and custom taping methods.3,6,8,15 McConnell tape is a rigid adhesive that is structurally supportive. Kinesiology tape is a more compliant adhesive, which places the muscle under gentle stretch while still allowing full range of motion.9 While the physiologic mechanism of taping is not completely understood, McConnell taping is in part designed to reposition the patella within the femoral trochlea, theoretically reducing pain from PFPS and improving both quadriceps and patellofemoral kinematics.11
The foremost finding of this study is that taping alone does not significantly reduce pain. There is evidence, however, that knee taping, including placebo taping, combined with exercise provides superior reduction in pain compared with exercise alone. As a result, rehabilitation programs should be multifactorial, with an emphasis on exercise therapy and education, while utilizing adjuncts, such as knee taping, to complement the treatment regimen. In this analysis, when exercise was included in comparison groups, the exercise group was consistently superior, regardless of whether exercise was coupled with tension or placebo taping. As previous studies have demonstrated, knee taping alone does not control pain.10,12,13 Therapies such as proprioceptive training, shoe inserts, and taping may be best utilized as a complement to traditional exercise therapy; however, they have not been effective when implemented alone.
Limitations
A major limitation of this review is that only 5 level 1 RCTs examining the efficacy of knee-taping techniques have been conducted for this common knee problem. As a result, there is a potential for bias in the validity of this evidence. Further, given the ease of identifying the taping strategy by the treating therapist or patient, a common methodological problem among all articles was the lack of blinding of the treating therapist or patient. This could lead to heightened performance bias among patients or assessment bias if the treating therapist was also the assessor of outcome. Furthermore, there is a lack of literature differentiating between tension-taping methodologies. Response bias was also a concern among all studies evaluating pain, as the studies relied on self-reported data. However, all studies did use standardized VAS measures known to be reliable and valid, which may balance these types of bias. Another limitation exists due to the lack of intention-to-treat analyses in the included studies, which would have enabled a more reliable estimate of true treatment effectiveness by replicating real-world conditions that include noncompliance and protocol violations. Finally, the current literature of RCTs with clinically pertinent outcomes is limited and inadequate to determine the effects of taping conclusively. The strength of this study would be bolstered if more consistent functional outcome measures had been available for analysis.
Conclusion
Knee taping can be an adjunct to traditional exercise therapy in the setting of PFPS. The evidence does not support knee taping utilized in isolation for patellofemoral pain.
Supplementary Material
Footnotes
The following author declared potential conflicts of interest: Matthew T. Provencher, CAPT, MT, MD, MC, USNR, is a paid consultant for Arthrex, Inc, and Joint Restoration Foundation (Allosource); has provided expert testimony for the NFL; has grants/grants pending from the Department of Defense; and receives royalties from Arthrex, Inc and SLACK Incorporated.
References
- 1. Akbas E, Atay AO, Yüksel I. The effects of additional kinesio taping over exercise in the treatment of patellofemoral pain syndrome. Acta Orthop Traumatol Turc. 2011;45:335-341. [DOI] [PubMed] [Google Scholar]
- 2. Aytar A, Ozunlu N, Surenkok O, Baltacı G, Oztop P, Karatas M. Initial effects of Kinesio® taping in patients with patellofemoral pain syndrome: a randomized, double-blind study. Isokinet Exerc Sci. 2011;19:135-142. [Google Scholar]
- 3. Campolo M, Babu J, Dmochowska K, Scariah S, Varughese J. A comparison of two taping techniques (Kinesio and McConnell) and their effect on anterior knee pain during functional activities. Int J Sports Phys Ther. 2013;8:105-110. [PMC free article] [PubMed] [Google Scholar]
- 4. Clark DI, Downing N, Mitchell J, Coulson L, Syzpryt EP, Doherty M. Physiotherapy for anterior knee pain: a randomised controlled trial. Ann Rheum Dis. 2000;59:700-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Crossley K, Bennell K, Green S, Cowan S, McConnell J. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med. 2002;30:857-865. [DOI] [PubMed] [Google Scholar]
- 6. Crossley K, Bennell K, Green S, McConnell J. A systematic review of physical interventions for patellofemoral pain syndrome. Clin J Sport Med. 2001;11:103-110. [DOI] [PubMed] [Google Scholar]
- 7. Hiemstra LA, Kerslake S, Irving C. Anterior knee pain in the athlete. Clin Sports Med. 2014;33:437-459. [DOI] [PubMed] [Google Scholar]
- 8. Jessee AD, Gourley MM, Valovich McLeod TC. Bracing and taping techniques and patellofemoral pain syndrome. J Athl Train. 2012;47:358-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kalron A, Bar-Sela S. A systematic review of the effectiveness of Kinesio Taping—fact or fashion? Eur J Phys Rehabil Med. 2013;49:699-709. [PubMed] [Google Scholar]
- 10. Lowry CD, Cleland JA, Dyke K. Management of patients with patellofemoral pain syndrome using a multimodal approach: a case series. J Orthop Sports Phys Ther. 2008;38:691-702. [DOI] [PubMed] [Google Scholar]
- 11. McConnell J. The management of chondromalacia patellae: a long term solution. Aust J Physiother. 1986;32:215-223. [DOI] [PubMed] [Google Scholar]
- 12. McConnell J. The physical therapist’s approach to patellofemoral disorders. Clin Sports Med. 2002;21:363-387. [DOI] [PubMed] [Google Scholar]
- 13. Rixe JA, Glick JE, Brady J, Olympia RP. A review of the management of patellofemoral pain syndrome. Phys Sportsmed. 2013;41:19-28. [DOI] [PubMed] [Google Scholar]
- 14. Rothermich MA, Glaviano NR, Li J, Hart JM. Patellofemoral pain: epidemiology, pathophysiology, and treatment options. Clin Sports Med. 2015;34:313-327. [DOI] [PubMed] [Google Scholar]
- 15. Song C-Y, Huang H-Y, Chen S-C, Lin J-J, Chang AH. Effects of femoral rotational taping on pain, lower extremity kinematics, and muscle activation in female patients with patellofemoral pain. J Sci Med Sport. 2015;18:388-393. [DOI] [PubMed] [Google Scholar]
- 16. Werner S. Anterior knee pain: an update of physical therapy. Knee Surg Sports Traumatol Arthrosc. 2014;22:2286-2294. [DOI] [PubMed] [Google Scholar]
- 17. Whittingham M, Palmer S, Macmillan F. Effects of taping on pain and function in patellofemoral pain syndrome: a randomized controlled trial. J Orthop Sports Phys Ther. 2004;34:504-510. [DOI] [PubMed] [Google Scholar]
- 18. Wood L, Muller S, Peat G. The epidemiology of patellofemoral disorders in adulthood: a review of routine general practice morbidity recording. Prim Health Care Res Dev. 2011;12:157-164. [DOI] [PubMed] [Google Scholar]
- 19. Wright RW, Brand RA, Dunn W, Spindler KP. How to write a systematic review. Clin Orthop Relat Res. 2007;455:23-29. [DOI] [PubMed] [Google Scholar]
- 20. Yen Y-M. Assessment and treatment of knee pain in the child and adolescent athlete. Pediatr Clin North Am. 2014;61:1155-1173. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.