Abstract
Context:
Hip arthroscopy is gaining popularity within the field of orthopaedic surgery. The development and innovation of hip-specific arthroscopic instrumentation and improved techniques has resulted in improved access to the hip joint and ability to treat various hip pathologies.
Evidence Acquisition:
Electronic databases, including PubMed and MEDLINE, were queried for articles relating to hip arthroscopy indications (1930-2017).
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
Initially used as a technique for loose body removal, drainage/debridement of septic arthritis, and treatment of pediatric hip disorders, hip arthroscopy is currently used to treat various hip conditions. The recognition of femoroacetabular impingement (FAI) as a source of hip pain in young adults has rapidly expanded hip arthroscopy by applying the principles of osseous correction that were previously described and demonstrated via an open surgical dislocation approach. Hip pathologies can be divided into central compartment, peripheral compartment, peritrochanteric space, and subgluteal space disorders.
Conclusion:
Although hip arthroscopy is a minimally invasive procedure that may offer decreased morbidity, diminished risk of neurovascular injury, and shorter recovery periods compared with traditional open exposures to the hip, it is important to understand the appropriate patient selection and indications.
Keywords: hip arthroscopy, femoroacetabular impingement, labral tear, synovial disorders, indications
Although initially described in 1931, hip arthroscopy has been gaining popularity since the 1980s.10,11 Hip arthroscopy was initially limited by the unique anatomy of the hip joint, which presented challenges due to the constrained bony anatomy, thick soft tissue envelope, and proximity of the neurovascular structures. Arthroscopy instrumentation used in the knee and the shoulder was not routinely capable of handling the depth of the hip joint. However, the development of hip-specific arthroscopic instrumentation and improved techniques for exposure has resulted in greater accessibility to the joint. Multiple studies have demonstrated the successful treatment of labral tears, chondral defects, and loose bodies with an arthroscopic approach.13,56 The recognition of femoroacetabular impingement (FAI) as a source of hip pain in young adults has also expanded the indications of hip arthroscopy by applying the principles of osseous correction, which were previously described and demonstrated via an open surgical dislocation approach.39 The number of hip arthroscopies performed by American Board of Orthopedic Surgery candidates increased 18-fold between 2003 and 2009.22 Although hip arthroscopy is a minimally invasive procedure that may offer decreased morbidity, diminished risk of neurovascular injury, and shorter recovery periods compared with traditional open exposures to the hip, it is important to understand the appropriate patient selection and indications to optimize patient outcomes and minimize complications. Current indications for hip arthroscopy can be divided into 4 pathologies: the central, peripheral, peritrochanteric, and subgluteal compartments (Table 1).
Table 1.
Indications for hip arthroscopy
| Central compartment |
| Labral tears |
| Chondral pathology |
| Ligamentum teres pathology |
| Septic arthritis |
| Loose bodies |
| Peripheral compartment |
| Femoroacetabular impingement |
| Subspine impingement |
| Synovial disorders |
| Capsular disorders |
| Psoas tendon disorders |
| Peritrochanteric compartment |
| Greater trochanteric pain syndrome |
| External snapping hip/iliotibial band disorder |
| Deep gluteal space |
| Ischiofemoral impingement |
| Proximal hamstring disorders |
| Sciatic nerve disorders |
Central (Intra-articular) Compartment
Labral Pathology
The acetabular labrum is a ring of fibrocartilage that acts as a “suction-seal” to ensure continuous lubrication of the hip joint and improve joint stability and kinematics by distributing contact forces and deepening the hip joint.34,35 Labral injury may result in painful clicking and locking, reduced range of motion, and interference with daily activities.72 Labral pathology most commonly occurs in the form of a tear or degeneration and can be secondary to FAI, dysplasia, or trauma. Labral pathology most commonly occurs along the anterior and superior acetabular margins; however, the location typically reflects the areas of mechanical conflict between femoral and acetabular pathomorphology.52 Debridement has historically been the treatment for labral tears and has demonstrated good results.14 However, with the improvement of instrumentation and development of labral-specific implants, labral repair techniques have become more popular. Studies have demonstrated the superior results of repair when compared with debridement.55,57 The objectives of labral preservation are to treat the resultant symptoms and restore the suction-seal function, with the goal of preventing the premature development of arthritis (Figure 1).66 Labral reconstruction is a newer technique that has gained popularity and has had good short-term results; however, the indications for this procedure are continuing to be refined.9 This technique is best indicated in patients with a prior labral resection/deficiency and who continue to have pain despite appropriate treatment of the bony pathomorphology of FAI.
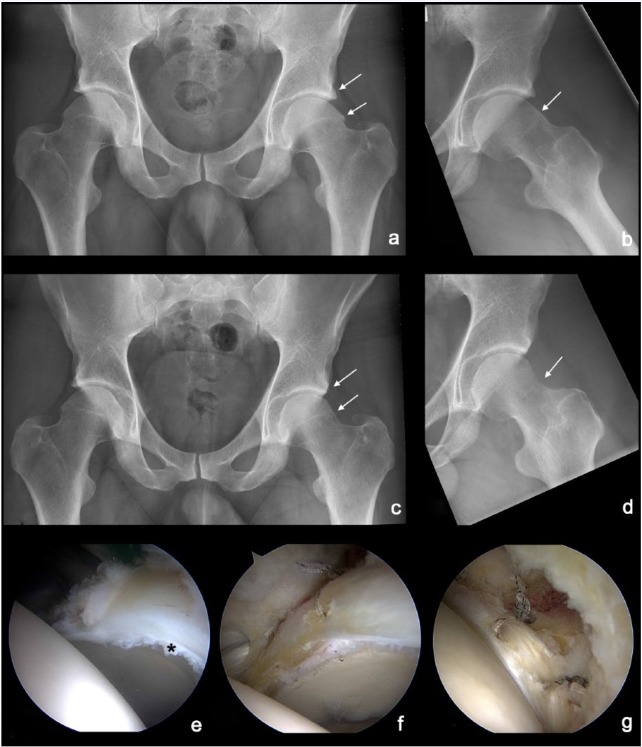
Figure 1.
Left hip combined femoroacetabular impingement with labral tear. (a and b) Preoperative anteroposterior and Dunn lateral radiograph demonstrating the combined cam- and pincer-type pathomorphology (arrows). (c and d) Postoperative radiographs demonstrate correction of the acetabular overcoverage and restoration of the femoral head-neck offset (arrows). (e) Intraoperative view of the acetabular labral tear (*). (f and g) Labral repair with base-type configuration and restoration of the labral suction-seal.
Chondral Lesions
Chondral surface pathology can occur traumatically, both acutely and chronically, from repetitive mechanical impingement (FAI) or as a result of acetabular rim overload that occurs as a result of acetabular dysplasia. Chondral injuries may occur on either the articular surface of the femoral head (more common with acute trauma) or the acetabulum (typical with FAI).11 These defects have limited healing capacity and have inferior outcomes in patients undergoing hip arthroscopy.16,84,88 Chondral lesions of the acetabulum are more commonly associated with “inclusion-type” hip disorders, such as cam-type FAI, and reflect a morphological incongruity between the femoral head-neck junction and the acetabulum. Loss of the normal sphericity and offset at the head-neck junction (FAI) typically causes delamination and/or debonding of the acetabular chondral surface.77 Many of the arthroscopic techniques that treat chondral defects in the hip were adapted from techniques used in the knee. These techniques include microfracture, fibrin adhesive, autologous osteochondral transplantation, osteochondral allograft transplantation, and autologous chondrocyte implantation with tissue-engineered scaffolds.3,5,21,81,82
Surface irregularity and fraying of the chondral surface may be treated successfully with limited debridement.77 Acetabular chondral delamination may occur in the presence or absence of an intact labrochondral junction. With an intact labrochondral junction, chondral delamination may be successfully treated by labral refixation, which indirectly stabilizes the chondral surface. Authors have described techniques for mobilization of the chondral delamination and performing microfracture beneath the chondral flap while utilizing fibrin glue or other techniques to “reattach” the delaminated chondral surface.77 Others have described suturing these chondral lesions; however, the long-term results of these treatment methods are unknown.78
Chondral flaps or full-thickness cartilage defects may be treated with marrow stimulation, such as microfracture. This process results in the release of mesenchymal stem cells in addition to clot formation, which eventually leads to the formation of a more stable fibrocartilaginous tissue. A recent systematic review of 267 patients among 12 studies demonstrated positive outcomes after hip arthroscopy with microfracture, with a low complication rate (0.7%).62 Additionally, a recent prospective, matched-control study of patients undergoing hip arthroscopy and microfracture for focal chondral damage demonstrated no significant differences in the patient-reported outcomes scores (modified Harris Hip Score, nonarthritic hip score, Hip Outcome Score) at a minimum of 2 years postoperatively.61
Recently, the development of injectable, minced extracellular matrix, which includes type 2 collagen, proteogylcans, and cartilaginous growth factors, has been used in addition to microfracture with the goal of promoting the production of hyaline-like tissue rather than the fibrocartilage-like tissue most commonly noted after microfracture (Figure 2).63 Other novel techniques such as autologous matrix-induced chondrogenesis (AMIC) and matrix-induced autologous chondrocyte implantation (MACI) have been utilized in the hip; however, no long-term follow-up data currently exist to support these techniques. AMIC is a single-stage approach in which a microfracture bed is enhanced with the application of a type I/III collagen matrix. On the other hand, MACI requires 2 stages in which a cartilage biopsy is taken during the first surgery and the chondrocytes are cultured into a 3-dimensional biocompatible scaffold. This scaffold is then inserted into the cartilage defect during second-stage surgery. Chondral lesions of the femoral head are less common. The cartilage of the femoral head is thinner and its angles are more challenging for arthroscopic instrumentation; thus, it is more difficult to prepare an adequate border for marrow stimulation. Mosaicplasty and osteochondral autograft and allograft transplantation has been demonstrated on the femoral head via an open approach; however, this treatment has yet to be described arthroscopically.43 Retrograde drilling of the femoral head from the lateral femur is another option to provide marrow stimulation to the chondral lesion on the femoral head.
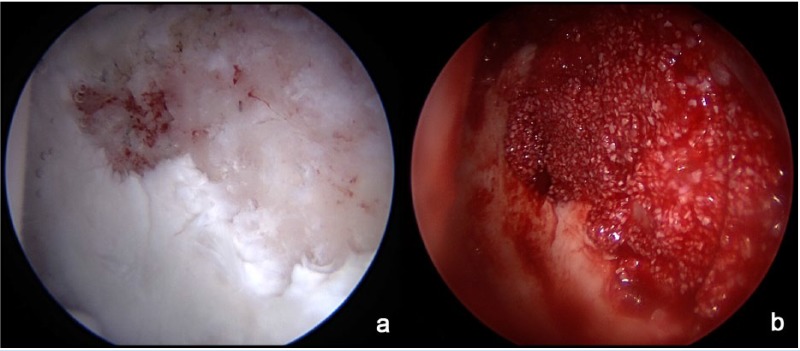
Figure 2.
(a) Full-thickness defect of the acetabular cartilage adjacent to a labral tear. (b) After microfracture of the underlying subchondral bone, an injectable, minced extracellular matrix has been placed. This is further sealed and covered with fibrin glue with the goal of promoting the production of hyaline-like tissue rather than the fibrocartilage-like tissue most commonly noted after microfracture.
Given the limited joint space for instrumentation during hip arthroscopy, the risk of iatrogenic chondral injury exists. Injuries to friable cartilage heal poorly, and no perfect arthroscopic treatment for smaller defects has been reported.50 Caution should therefore be exercised by hip arthroscopists during joint entry and surgical maneuvers to avoid iatrogenic chondral injury.
Ligamentum Teres Injuries
The ligamentum teres is a strong, intra-articular ligament that stabilizes the hip, particularly with respect to adduction, flexion, and external rotation.2 Hip arthroscopy has dramatically improved our understanding of the ligamentum teres and its contribution to the hip joint in addition to its pathologic states. Lesions of the ligamentum teres include partial or complete traumatic tears, degenerative tears, and avulsion fractures at the foveal insertion.20 Traumatic hip subluxations or dislocations have a high incidence of ligamentum teres tears.73 In the setting of ligamentum teres pathology, the synovium that normally surrounds the ligament is disrupted and the injured fibers are visualized.
Ligamentum teres injuries are difficult to diagnose, and patients may present with mechanical hip pain and describe painful locking, clicking, or giving way. Arthroscopic debridement relieves mechanical symptoms and pain.17,41,51 Reconstruction techniques have also been described despite limited evidence.2 A recent systematic review demonstrated similar clinical results when comparing patients who underwent selective debridement and reconstruction.24 However, the appropriate indications for reconstructive procedures are not currently well established, as patients with ligamentum teres pathology may also have underlying bony instability patterns that may better improve with corrective osteotomy. When significant tears in the ligamentum teres are encountered in the absence of degenerative change, traumatic (subluxation) and atraumatic (dysplasia/multidirectional instability) instability should be suspected. Both Gray and Villar40 and Botser et al8 proposed various classification systems based on arthroscopic findings for ligamentum teres injuries, with each class determined by the completeness and character of the tear.
Septic Arthritis
Septic arthritis is an infection of the hip joint that demands immediate and accurate diagnosis as well as effective treatment to maximize the likelihood of a favorable outcome and to prevent disabling sequelae. It can cause acute chondrolysis and irreversible damage to joint articular surfaces, and, if left untreated, may lead to osteomyelitis, sepsis, and eventually osteoarthritis of the joint.
Open arthrotomy with adequate irrigation and debridement was the standard form of treatment of patients with septic arthritis. Arthroscopic drainage of septic arthritis of the hip has been used as an alternative to open arthrotomy based on its success in the knee.49 In a comparative study, El-Sayed showed comparable eradication of infection at greater than 12-month follow-up, with no recurrence or development of complications, when comparing arthroscopic versus open treatment of septic arthritis.32 Arthroscopic drainage of septic arthritis of the hip appears to be a valid alternative to open arthrotomy, especially in acute, promptly diagnosed cases and in the hands of experienced arthroscopists. Patients who present with subacute symptoms may have extra-articular extension of the infection and may be better treated with an open approach.
Loose Bodies/Synovial Chondromatosis
Hip arthroscopy has become a valuable tool, allowing for direct visualization and minimally invasive treatment of loose bodies.53 Loose bodies are typically small fragments of bone, cartilage, or diseased synovium that are typically mobile within the hip joint, causing mechanical symptoms such as popping, catching, and locking. Because of the variable location and composition of loose bodies, physical examination and radiological imaging are unreliable. A large number of small loose bodies may be the product of primary or secondary synovial chondromatosis/osteochondromatosis. Primary synovial chondromatosis is a proliferative disease affecting the joint synovium. During this process, synovial membrane metaplasia occurs resulting in enlargement and later calcification. These areas may subsequently break away, thus becoming free in the joint to potentially cause pain and mechanical symptoms.23 Secondary synovial chondromatosis is more common and typically occurs secondary to trauma. Damage to articular cartilage as a result of trauma can result in loose chondral fragments. Hip arthroscopy allows for the identification and removal of these fragments and provides the opportunity for simultaneous treatment of the damaged chondral surface (Figure 3).23 Loose bodies can often be adherent to the synovium and must be separated for removal. Large graspers, shavers, and chest tubes can be used to assist with loose body removal. Additional portals may often be required to access the medial and posterior aspect of the hip.
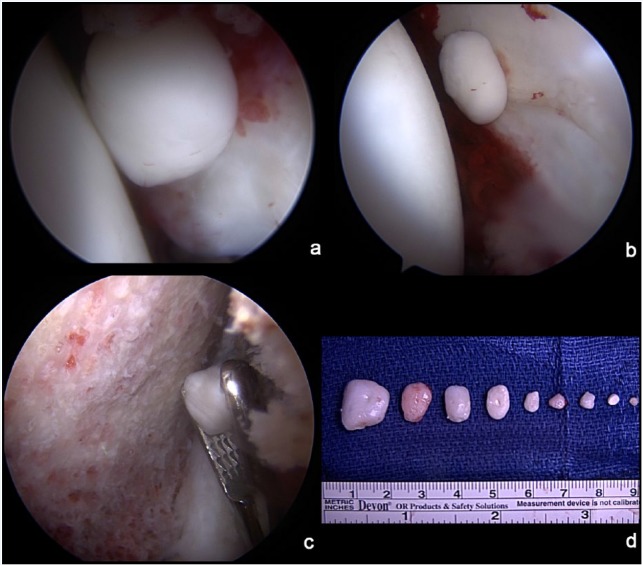
Figure 3.
Synovial chondromatosis. (a) A loose fragment is noted in the anterior aspect of the hip near the midanterior portal. (b) An additional fragment is noted laterally while viewing through the midanterior portal. (c) A large grasper is used to retrieve an additional loose body in the peripheral compartment along the femoral neck. (d) Gross view of the multiple loose fragments that were removed.
Peripheral Compartment
Femoroacetabular Impingement
FAI is a disorder that results from abnormal contact between the femoral head-neck junction and acetabulum that can lead to labral and/or chondral pathology.39 Cam-type FAI leads to a characteristic “inclusion-type” injury pattern with delamination of the articular cartilage and tearing of the acetabular labrum. Pincer-type FAI, on the other hand, leads to an “impaction-type” injury to the acetabular labrum with degenerative tear patterns. Repetitive impingement may result in pain and discomfort among patients and is one of the predominant causes of arthritis in the nondysplastic hip.
Ganz et al38 developed an open surgical dislocation approach via a trochanteric osteotomy to surgically address FAI in symptomatic patients. However, with the advent and advancement of hip arthroscopy, arthroscopic procedures may provide equal or greater improvement in outcomes when compared with open surgical dislocation for the treatment of FAI, with lower reoperation and complication rates.30,42 Arthroscopy also minimizes trauma to the periarticular soft tissues without the need for trochanteric osteotomy, potentially reducing recovery time and morbidity related to abductor dysfunction.
However, successful treatment of the bony pathomorphology requires adequate visualization and treatment to minimize the potential for inadequate resection with resultant symptomatic residual FAI deformity, as this remains the most common reason for subsequent revision hip preservation surgery.4,7,46,74 Intraoperative fluoroscopy can be helpful to systematically assess and treat cam and pincer morphology. Larson previously described a reproducible and systematic intraoperative fluoroscopic evaluation of the hip for the management of cam and pincer morphology during arthroscopic treatment of FAI.56,76 Rotation of the pelvis with table tilt and Trendelenburg/reverse Trendelenburg positioning can be performed to obtain an intraoperative fluoroscopic view that mirrors the preoperative, well-centered anteroposterior pelvic radiograph. Further confirmation of the precise location of the cam deformity with reproducible fluoroscopic views may also result in a more precise and comprehensive resection.76 A templated preoperative plan is important, and correlation with intraoperative radiographs and dynamic assessment is crucial to ensure adequate correction and avoid recurrent symptoms (see Figure 1).
Subspine Impingement
Extra-articular sources of FAI have been increasingly recognized and treated. One of the more common sources has been subspine impingement, which is the mechanical conflict between the anterior inferior iliac spine (AIIS) and the distal femoral neck. The various etiologies of AIIS pathomorphology include apophyseal avulsions, rectus femoris avulsions with ossification, overcorrection after periacetabular osteotomy, and developmental deformity. Arthroscopic decompression of the AIIS structures can improve outcomes.44,59 Hetsroni et al45 recently classified AIIS morphology; however, one must also be aware of the variations in the anatomy as a low-lying AIIS may be mistaken as a false positive crossover sign on an anteroposterior pelvic radiograph.90
Synovial Disorders
The synovial lining may degenerate over time secondary to trauma, repetitive stress, and/or a variety of inflammatory arthropathies, such as synovial chondromatosis, rheumatoid arthritis, and pigmented villonodular synovitis (PVNS). Arthroscopy for synovial disease allows not only minimally invasive treatment but also definitive diagnosis. Synovial biopsies can be performed and confirm the diagnosis of inflammatory arthropathy and thus guide subsequent medical treatment. Arthroscopic synovectomy may also slow articular cartilage deterioration, thus preserving hip function; however, more diffuse disease extending outside the joint space into the adjacent soft tissues may warrant open surgical excision.23
PVNS is a benign, locally aggressive proliferative disorder of the synovium that may involve the hip in up to 15% of cases.86 This process may occur in either a diffuse or localized form and has been traditionally treated with open synovectomy with modest results when compared with other joints.86 However, hip arthroscopy may allow equal outcomes with less morbidity and faster recovery. Case series have demonstrated favorable results with improvement in clinical scores.18 However, additional nontraditional portals or perhaps a T-capsulotomy may be needed to improve visualization and access to the entire pathology (Figure 4). Large graspers, shavers, and radiofrequency devices are also crucial for the complete removal and resection of the offending lesions. Focal foveal and inferomedial PVNS pathology is the most predictably managed, whereas diffuse PVNS extending along the posterior capsule might be more completely managed with an open approach.
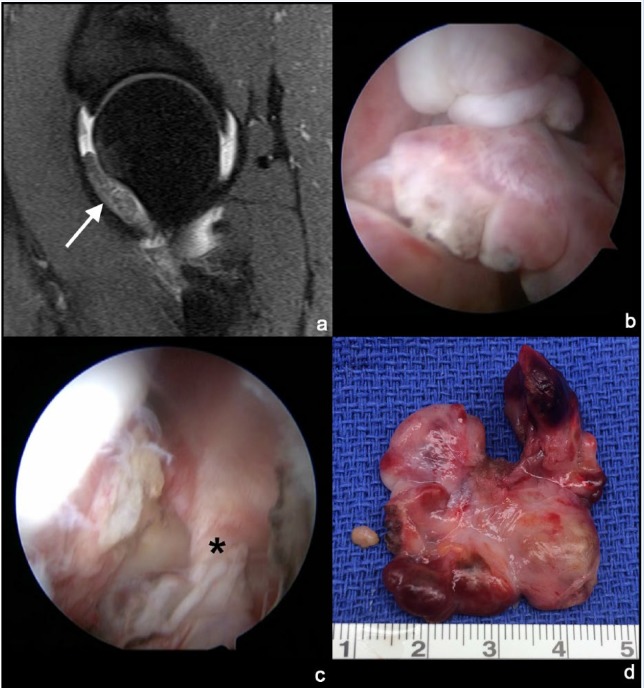
Figure 4.
Pigmented villonodular synovitis (PVNS). (a) Sagittal T2-weighted magnetic resonance image demonstrating the intra-articular soft tissue mass along the anterior femoral neck (arrow). (b) Visualization of the lobular, nodular PVNS mass. (c) A stalk is noted that connects the mass with the hip synovium of the anterior capsule (*). (d) Gross specimen demonstrating the multinodular and lobular nature of the PVNS mass.
Synovial chondromatosis is another rare benign, proliferative disorder in which multiple metaplastic cartilaginous masses form within the synovial membrane. These masses may calcify or ossify with time and may separate from the synovium, thus becoming intra-articular loose bodies. The loose bodies may result in mechanical injury to the chondral surfaces of the femoral head and/or acetabulum via third-body wear. Although good clinical outcomes and high patient satisfaction have been established with the arthroscopic treatment of synovial chondromatosis, recurrence rates vary between 0% and 31%.1,23,80
Capsular Disorders (Adhesive Capsulitis and Capsular Laxity)
Although the hip is a deep-seated joint, the capsule provides additional stability to both translational and rotational range of motion. The capsule consists of 4 ligamentous structures: the iliofemoral, ischiofemoral, and pubofemoral ligaments and the zona orbicularis. The iliofemoral ligament is the strongest ligament and is commonly cut transversely during an interportal capsulotomy between the anterolateral and midanterior portals. A T-capsulotomy extension may also be utilized to aide in exposure and is made parallel to the fibers of the iliofemoral ligament. Recent investigations have demonstrated the importance of iliofemoral ligament integrity for normal hip kinematics. Capsular repair has become more common in lieu of these investigations as well as reports of iatrogenic postoperative hip dislocation.65,67,75 A recent study also demonstrated improved clinical outcomes when complete capsular closure was performed when compared with partial capsular closure.37
Underlying capsular laxity may also be associated with hip pain and instability. Traumatic injuries can result in capsular incompetence with or without labral damage. Atraumatic hip instability may be the result of repetitive external rotation with axial loading, resulting in anterior subluxation and microinstability (native laxity). Others may be predisposed to hip instability due to acetabular dysplasia, general ligamentous laxity, or connective tissue disorders.79,85 Recent case series have also proposed that the structural abnormalities associated with FAI may predispose patients to posterior hip instability and subluxation events, with 1 series reporting favorable outcomes after arthroscopic osteoplasty and labral refixation.6,54 Finally, iatrogenic capsular laxity may also exist in patients who have undergone prior hip arthroscopy with an unrepaired capsulotomy.
Arthroscopic capsular or labral repair or reconstruction may be beneficial for patients with recurrent hip instability, particularly after trauma.85 Capsular plication of borderline acetabular dysplasia may provide good clinical outcomes.15,31,60,69 While functional scores may improve with borderline acetabular dysplasia, the clinical results are inferior, and failure rates are higher compared with a cohort undergoing arthroscopy for FAI.60 Critical assessment of preoperative radiographs is necessary, as capsular repair or plication is not sufficient to stabilize a hip with primarily dysplastic features, such as a lateral center-edge angle less than 20°, Tönnis angle greater than 15°, femoral head lateralization, and/or a break in the Shenton line.7
Clinical examination of hip adhesive capsulitis is similar to that of the shoulder. It can be nonspecific in other hip pathologies that cause pain and a decreased passive range of motion of the joint, such as FAI. However, it is much more difficult to diagnose given that decreased range of motion of the hip is not as noticeable as limited motion of the shoulder.12 Arthroscopy with capsulotomy or capsulectomy followed by manipulation can effectively treat patients with adhesive capsulitis of the hip in a minimally invasive fashion.12
Psoas Tendon Disorders
The iliopsoas myotendinous unit is a powerful hip flexor that may be a source of anterior hip pain (tendinitis, bursitis, impingement, and snapping). As the iliopsoas travels toward the lesser trochanter, the tendon rotates posteriorly within the muscle, lying immediately anterior to the hip joint. Iliopsoas snapping, commonly referred to as coxa saltans internus, is characterized by painful audible or palpable snapping of the iliopsoas during hip motion. This is usually reproduced as the hip is flexed, abducted, and externally rotated to extension and neutral rotation. The underlying mechanism of the snapping is somewhat controversial; however, a recent study suggests that snapping is due to a sudden flipping of the psoas tendon over the iliacus muscle rather than a snapping over the iliopectineal eminence.25,89 Surgical treatment may be warranted if a patient has undergone physical therapy, activity modification, and corticosteroid injection with no improvement. Hip arthroscopy may be utilized to lengthen the musculotendinous unit, with the goal of preventing the snapping and irritation of the underlying bursa. Arthroscopic release of the iliopsoas tendon has been described and performed at 3 different locations: in the central compartment (transcapsular), in the peripheral compartment, and at the lesser trochanter. Although outcomes are generally good and there is no difference between techniques,48 there does exist a period of transient weakness and atrophy of the iliopsoas musculature on magnetic resonance imaging (MRI). Psoas tendon lengthening should be performed with caution as there is a risk of recurrent snapping as well as poor outcomes. Worse outcomes have occurred in patients with high femoral anteversion (>25°), indicating that the iliopsoas may function as a dynamic stabilizer of the hip in this patient population or perhaps those with underlying acetabular dysplasia.33
Iliopsoas tendon impingement is another pathologic process that may result in a typical labral tear at the “psoas-U” along the acetabular rim, which is thought to be due to an excessively tight iliopsoas tendon. Surgical management of iliopsoas tendon impingement focuses on treatment of the labral pathology either by repair or selective debridement as well as lengthening of the iliopsoas tendon. Recent studies have demonstrated successful clinical improvement19,29,70; however, long-term follow-up studies are necessary to determine the optimal treatment.
Peritrochanteric Compartment
Greater Trochanteric Pain Syndrome
Greater trochanteric pain syndrome encompasses several pathologies. Greater trochanteric pain syndrome is relatively common, affecting 10% to 25% of the population.83 Trochanteric bursitis is the most common form and typically involves inflammation of the bursa between the trochanteric facets and the gluteus medius, gluteus minimus, and the iliotibial band. Tears in the abductor tendons and musculature can also occur and thus contribute to lateral hip pain. This pathology is often compared with rotator cuff tears in the shoulder. Recent advances in MRI as well as hip arthroscopy have led to an improved understanding of the anatomy and pathology of the lateral hip and trochanteric space disorders. With appropriately placed arthroscopic portals, a clear space lying between the iliotibial band and the greater trochanter can be identified.68 An arthroscopic bursectomy is usually required to obtain adequate visualization of the structures of interest. The gluteus maximus insertion and the vastus lateralis origin are usually the easiest structures to identify for proper orientation.
The gluteus medius, which inserts on the lateral and posterior facets of the greater trochanter, lies posterior to the gluteus minimus insertion and is usually torn along its articular side, and tears can be partial, intrasubstance, or complete.28 A thorough knowledge of the normal footprint anatomy is crucial to fully assess the abductor tendons.87 The greater trochanter attachment site is gently decorticated with an arthroscopic bur, followed by placement of suture anchors, which can be performed under fluoroscopic guidance to assist with the anchor trajectory. The sutures are subsequently passed and tied, approximating the tendon to the bone. Double-row constructs may improve tendon repair surface area. Ultimately, open repair with allograft augmentation or gluteus maximus transfer can be considered for more chronic retracted or irreparable tears. Open versus arthroscopic approaches are often based on surgeon experience with various approaches.
Snapping Hip Disorder
Coxa saltans externus may occur due to snapping of the posterior iliotibial band over the greater trochanter, which may cause abrasion of the greater trochanter. The clinical diagnosis is often made visually, as patients can often reproduce the visible snapping. Additionally, palpation of the greater trochanter with hip flexion and extension may allow the identification of abnormal motion and friction of the iliotibial band. If this snapping does not improve with nonoperative treatment, an arthroscopic release may be indicated. This release can be done from either the superficial or deep surface. Various releases have been described such as an H-type (Mosier), z-type, or diamond-shaped configuration,47 allowing the iliotibial band to expand around the greater trochanter. Immediate weightbearing and a stretching program are instituted postoperatively, with commonly reported return to full activity and predictable pain relief.
Deep Gluteal Compartment
Ischiofemoral Impingement
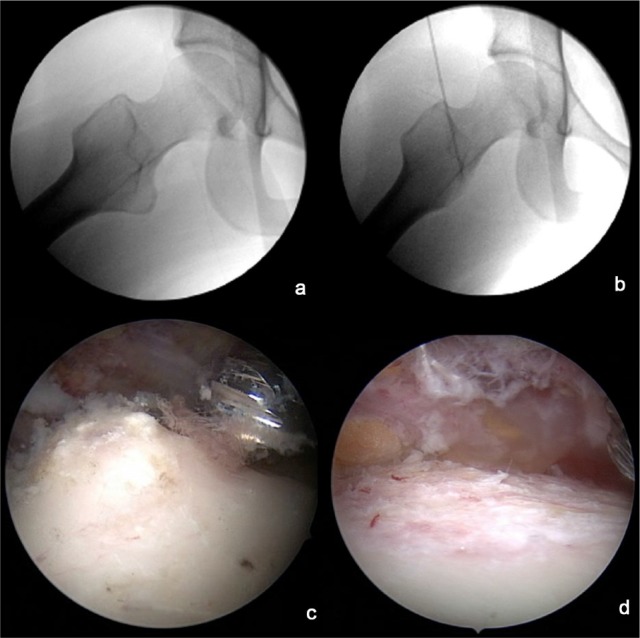
Ischiofemoral impingement is an often unrecognized source of hip pain that occurs due to abnormal contact between the lesser trochanter/posterior femur and the lateral border of the ischium. Characteristic MRI findings include edema within the quadratus femoris and a narrowed ischiofemoral space. Ultrasound- or computed tomography–guided injections of anesthetics and/or corticosteroid into the ischiofemoral space can be both diagnostic and therapeutic. If nonoperative treatment fails and the patient experienced temporary relief with a prior injection, surgical treatment may be warranted. Treatment is focused on restoring “normal anatomy” by increasing the size of the ischiofemoral space. This may involve a lesser trochanter resection (Figure 5) with or without osteoplasty of the lateral ischium. The lesser trochanter resection can be performed endoscopically, either anteriorly or posteriorly. If an osteoplasty of the ischium is required, an open posterior approach may be needed to partially detach the proximal hamstring origin, although endoscopic approaches have been described.26,27 The lateral ischium is then resected until appropriate clearance is obtained with dynamic hip extension and adduction testing. The hamstring origin is then reattached to the remaining ischium using suture anchors.
Figure 5.
(a) Intraoperative fluoroscopic radiograph profiling the lesser trochanter. (b) Lesser trochanter resection has been performed for ischiofemoral impingement. (c) Arthroscopic visualization of the lesser trochanter through the distal anterolateral portal. (d) Visualization after resection of the lesser trochanter.
Proximal Hamstrings Disorders
Recent advancement in the understanding of the posterior hip anatomy and biomechanics has led to an improvement in the diagnosis and treatment of deep gluteal space disorders. The proximal hamstrings origin lies close to the sciatic nerve and lesser trochanter, which can all be implicated in the cause of posterior hip pain. Pathology of the proximal hamstrings origin can occur due to chronic, repetitive injuries or a single acute event. Patients may experience pain with sitting, stretching, or exertion. Traditionally, proximal hamstring ruptures have been managed with open repair; however, advances in techniques and equipment have allowed treatment of the hamstrings origin in an endoscopic manner.26,27 Partial-thickness injuries to the proximal hamstrings tendons that do not respond to nonoperative treatment may also be treated with endoscopic debridement and/or repair. However, no long-term studies exist that determine its efficacy or whether there are increased risks given the challenges with the endoscopic approach.
Sciatic Nerve
Knowledge of the anatomical relationship of the sciatic nerve and its surrounding structures is important to further diagnose causes of deep gluteal space pain. The sciatic nerve passes through the sciatic notch intimately in association with the piriformis muscle, which can compress the nerve and lead to symptoms. The sciatic nerve normally accommodates hip movement with excursion; however, neighboring pathologic tissue may result in entrapment, thus reducing the space available for nerve excursion during hip flexion and rotation. This can result in pain in the buttocks and radiation into the posterior thigh.64 Endoscopic treatment may be used to decompress the offending structures; however, this treatment may be ineffective if tethering structures are too proximal in the pelvis or distal in the thigh.64 Sciatic nerve decompression is a relatively new indication for hip endoscopy and requires familiarity with the anatomy of the subgluteal space.
Contraindications
Hip arthroscopy is a relatively new technique, and appropriate indications continue to be refined. Although multiple studies have shown that younger patients may have superior outcomes, others have demonstrated clinical improvement in patients older than 60 years without signs of advanced arthritis. Additionally, the adolescent population may benefit for arthroscopic treatment alone or in conjunction with other adjunctive procedures. Successful outcomes from hip arthroscopy require careful patient selection as well as recognition of patient- or technique-specific factors that may compromise clinical outcomes or preclude the procedure.
Absolute Contraindications
Advanced osteoarthritis of the hip with fully denuded articular cartilage is one of the absolute contraindications to hip arthroscopy given the universal poor results that have been reported. A radiographic joint space less than 2 mm or more than 50% joint space narrowing on plain radiographs58 has been shown to be associated with inferior outcomes and a higher rate of conversion to total hip arthroplasty, and therefore, should be considered when evaluating patients.71 Additionally, ankylosis of the joint is a contraindication as arthroscopic instruments cannot be safely maneuvered without adequate joint distraction.11 Hip arthroscopy should also not be the sole treatment in the setting of acetabular and/or femoral dysplasia. Dysplastic features such as femoral head migration (>1 cm lateral or break in the Shenton line) indicate a more global structural instability that is not amendable to hip arthroscopy alone. Additional radiographic measurements that suggest acetabular dysplastic features include a lateral center-edge angle less than 20°, a Tönnis angle greater than 15°, and anterior center-edge angle less than 20°. Patients who demonstrate this instability should be considered for a periacetabular osteotomy (PAO). Finally, rim resection in severe acetabular retroversion should be avoided as this may exacerbate instability from a posteriorly deficient acetabulum. An anteverting PAO is indicated in this setting. However, hip arthroscopy in these settings may be used as an adjunct to pelvic or femoral osteotomy to treat intra-articular pathology. Hip arthroscopy should also not be the primary treatment for severe patterns of FAI, such as slipped capital femoral epiphysis or Perthes deformities, as these are better treated with open surgical hip dislocation.
Relative Contraindications
Obesity multiplies the technical challenges of hip arthroscopy and increases the risk of complications, as current arthroscopic instrumentation may not have sufficient length to access the joint.53 Obesity and deconditioning also make compliance with postoperative rehabilitation more difficult. Arthroscopic procedures may also be contraindicated for patients with known neurological injury/disorders, such as pudendal neuralgia or peroneal or sciatic nerve palsy, as hip traction may risk further neurologic impairment.36 Borderline acetabular dysplasia (BD) is another setting in which arthroscopy may or may not be indicated. Radiographic measurements that have defined BD include a lateral center-edge angle between 20° and 25° and a Tönnis angle between 10° and 15°. It is important to determine, via history and physical examination, whether the predominant symptoms result from underlying hip instability or hip impingement. Three-dimensional imaging such as a computed tomography scanning may also be helpful to determine the acetabular volume and version as well as the femoral version when deciding whether hip arthroscopy alone is feasible. Should hip arthroscopy be performed, care should be taken to avoid any acetabular rim resection and thus avoid iatrogenic instability. Capsular management and adequate repair and/or plication is also crucial in patients with BD, as this may impart stability to the hip and may improve clinical outcomes.31,60,69 However, long-term studies of hip arthroscopy in the setting of BD and comparison studies to patients undergoing PAO are necessary to determine the appropriate treatment for this challenging patient population. Finally, large femoral-sided deformities that extend laterally and posteriorly to the retinacular vessels, although difficult to treat comprehensively with arthroscopy, may be accessed in the hands of experienced hip arthroscopists. However, revision hip arthroscopy is becoming more common, and at times, these large deformities may be better addressed with an open procedure.
Summary
Until recently, hip arthroscopy was not widely performed due to the complexity and access to this deep joint in addition to the surrounding tissue envelope and constrained alignment of the bony structures. However, the number of hip arthroscopic procedures has increased over the past decade given the rapid evolution of instrumentation to allow safe access to the hip in combination with the expanded indications that allow treatment of a growing number of disorders of the hip. Although hip arthroscopy is a minimally invasive procedure that may offer decreased morbidity and shorter recovery periods compared with open procedures, appropriate patient selection and indications are needed to optimize patient outcomes and minimize complications. These indications and contraindications will continue to evolve as outcome studies are further reported.
Footnotes
The following authors declared potential conflicts of interest: James R. Ross, MD, is a paid consultant for Smith & Nephew; Christopher M. Larson, MD, is a paid consultant for Smith & Nephew and A3 Surgical and has stock options in A3 Surgical; Asheesh Bedi, MD, is a paid consultant for Arthrex, Inc and has stock/stock options in A3 Surgical.
References
- 1. Adelani MA, Wupperman RM, Holt GE. Benign synovial disorders. J Am Acad Orthop Surg. 2008;16:268-275. [DOI] [PubMed] [Google Scholar]
- 2. Bardakos NV, Villar RN. The ligamentum teres of the adult hip. J Bone Joint Surg Br. 2009;91:8-15. [DOI] [PubMed] [Google Scholar]
- 3. Bedi A, Feeley BT, Williams RJ., 3rd Management of articular cartilage defects of the knee. J Bone Joint Surg Am. 2010;92:994-1009. [DOI] [PubMed] [Google Scholar]
- 4. Bedi A, Ross JR, Kelly BT, Larson CM. Avoiding complications and treating failures of arthroscopic femoroacetabular impingement correction. Instr Course Lect. 2015;64:297-306. [PubMed] [Google Scholar]
- 5. Behery O, Siston RA, Harris JD, Flanigan DC. Treatment of cartilage defects of the knee: expanding on the existing algorithm. Clin J Sports Med. 2014;24:21-30. [DOI] [PubMed] [Google Scholar]
- 6. Berkes MB, Cross MB, Shindle MK, Bedi A, Kelly BT. Traumatic posterior hip instability and femoroacetabular impingement in athletes. Am J Orthop. 2012;41:166-171. [PubMed] [Google Scholar]
- 7. Bogunovic L, Gottlieb M, Pashos G, Baca G, Clohisy JC. Why do hip arthroscopy procedures fail? Clin Orthop Relat Res. 2013;471:2523-2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Botser IB, Martin DE, Stout CE, Domb BG. Tears of the ligamentum teres: prevalence in hip arthroscopy using 2 classification systems. Am J Sports Med. 2011;39(suppl):117S-125S. [DOI] [PubMed] [Google Scholar]
- 9. Boykin RE, Patterson D, Briggs KK, Dee A, Philippon MJ. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med. 2013;41:2296-2301. [DOI] [PubMed] [Google Scholar]
- 10. Burman MS. Arthroscopy or the direct visualization of joints. J Bone Joint Surg Am. 1931;4:669. [DOI] [PubMed] [Google Scholar]
- 11. Byrd JW. Hip arthroscopy. J Am Acad Orthop Surg. 2006;14:433-444. [DOI] [PubMed] [Google Scholar]
- 12. Byrd JW, Jones KS. Adhesive capsulitis of the hip. Arthroscopy. 2006;22:89-94. [DOI] [PubMed] [Google Scholar]
- 13. Byrd JW, Jones KS. Arthroscopic management of femoroacetabular impingement: minimum 2-year follow-up. Arthroscopy. 2011;27:1379-1388. [DOI] [PubMed] [Google Scholar]
- 14. Byrd JW, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25:365-368. [DOI] [PubMed] [Google Scholar]
- 15. Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055-1060. [DOI] [PubMed] [Google Scholar]
- 16. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578-587. [DOI] [PubMed] [Google Scholar]
- 17. Byrd JW, Jones KS. Traumatic rupture of the ligamentum teres as a source of pain. Arthroscopy. 2004;20:385-391. [DOI] [PubMed] [Google Scholar]
- 18. Byrd JW, Jones KS, Maiers GP., 2nd Two to 10 years’ follow-up of arthroscopic management of pigmented vollonodular synovitis in the hip: a case series. Arthroscopy. 2013;29:1783-1787. [DOI] [PubMed] [Google Scholar]
- 19. Cascio BM, King D, Yen YM. Psoas impingement causing labrum tear: a series from three tertiary hip arthroscopy centers. J La State Med Soc. 2013;165:88-93. [PubMed] [Google Scholar]
- 20. Cerezeal L, Kassarjian A, Canga A, et al. Anatomy, biomechanics, imaging, and management of ligamentum teres injuries. Radiographics 2010;30:1637-1651. [DOI] [PubMed] [Google Scholar]
- 21. Chahal J, Gross AE, Gross C, et al. Outcomes of osteochondral allograft transplantation in the knee. Arthroscopy. 2013;29:575-588. [DOI] [PubMed] [Google Scholar]
- 22. Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94:e23. [DOI] [PubMed] [Google Scholar]
- 23. de Sa D, Horner NS, MacDonald A, et al. Arthroscopic surgery for synovial chondromatosis of the hip: a systemic review of rates and predisposing factors for recurrence. Arthroscopy. 2014;30:1499-1504.e2. [DOI] [PubMed] [Google Scholar]
- 24. de SA D, Phillips M, Philippon MJ, Letkemann S, Simunovic N, Ayeni OR. Ligamentum teres injuries of the hip: a systematic review examining surgical indications, treatment, options and outcomes. Arthroscopy. 2014;30:1634-1641. [DOI] [PubMed] [Google Scholar]
- 25. Deslandes M, Guillin R, Cardinal E, Hobden R, Bureau NJ. The snapping iliopsoas tendon: new mechanism using dynamic sonography. AJR Am J Roentgenol. 2008;190:576-581. [DOI] [PubMed] [Google Scholar]
- 26. Dierckman BD, Guanche CA. Endoscopic proximal hamstring repair and ischial bursectomy. Arthrosc Tech. 2012;1:e201-e207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Domb BG, Linder D, Sharp KG, Sadik A, Gerhardt MB. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech. 2013;2:e35-e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Domb BG, Nasser RM, Botser IB. Partial-thickness tears of the gluteus medius: rationale and technique for trans-tendinous endoscopic repair. Arthroscopy. 2010;26:1697-1705. [DOI] [PubMed] [Google Scholar]
- 29. Domb BG, Sindle MK, McArthur B, Voos JE, Magennis EM, Kelly BT. Iliopsoas impingement: a newly identified cause of labral pathology in the hip. HSS J. 2011;7:145-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Domb BG, Stake CE, Botser IB, Jackson TJ. Surgical dislocation of the hip versus arthroscopic treatment of femoroacetabular impingement: a prospective matched-pair study with average 2 year follow up. Arthroscopy. 2013;29:1506-1513. [DOI] [PubMed] [Google Scholar]
- 31. Domb BG, Stake CE, Lindner D, El-Bitat Y, Jackson TJ. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013; 41:2591-2598. [DOI] [PubMed] [Google Scholar]
- 32. El-Sayed AM. Treatment of early septic arthritis of the hip in children: comparison of results of open arthrotomy versus arthroscopic drainage. J Child Orthop. 2008;2:229-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Fabricant PD, Bedi A, De La Torre K, Kelly BT. Clinical outcomes after arthroscopic psoas lengthening: the effect of femoral version. Arthroscopy. 2012;28:965-971. [DOI] [PubMed] [Google Scholar]
- 34. Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;32:171-178. [DOI] [PubMed] [Google Scholar]
- 35. Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech. 2000;33:953-960. [DOI] [PubMed] [Google Scholar]
- 36. Flierl MA, Stahel PF, Hak DJ, Morgan SJ, Smith WR. Traction table-related complications in orthopaedic surgery. J Am Acad Orthop Surg. 2010;18:668-675. [DOI] [PubMed] [Google Scholar]
- 37. Frank RM, Lee S, Bush-Joseph CA, Kelly BT, Salata MJ, Nho SJ. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42:2634-2642. [DOI] [PubMed] [Google Scholar]
- 38. Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119-1124. [DOI] [PubMed] [Google Scholar]
- 39. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112-120. [DOI] [PubMed] [Google Scholar]
- 40. Gray AJ, Villar RN, The ligamentum teres of the hip: an arthroscopic classification of its pathology. Arthroscopy. 1997;13:575-578. [DOI] [PubMed] [Google Scholar]
- 41. Guanche CA, Sikka RS. Acetabular labral tears with underlying chondromalacia: a possible association with high-level running. Arthroscopy. 2005;21:580-585. [DOI] [PubMed] [Google Scholar]
- 42. Harris JD, Erickson BJ, Bush-Joseph CA, Nho SJ. Treatment of femoroacetabular impingement: a systematic review. Curr Rev Musculoskelet Med. 2013;6:207-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hart R, Janecek M, Visca P, Bucek P, Kocis J. Mosaicplasty for the treatment of femoral head defect after incorrect resorbable screw insertion. Arthroscopy. 2003;19:E1-E5. [DOI] [PubMed] [Google Scholar]
- 44. Hetsroni I, Larson CM, Dela Torre K, Zbeda RM, Magennis E, Kelly BT. Anterior inferior iliac spine deformity as an extra-articular source for hip impingement: a series of 10 patients treated with arthroscopic decompression. Arthroscopy. 2012;28:1644-1653. [DOI] [PubMed] [Google Scholar]
- 45. Hetsroni I, Poultsides L, Bedi A, Larson CM, Kelly BT. Anterior inferior iliac spine morphology correlates with hip range of motion: a classification system and dynamic model. Clin Orthop Relat Res. 2013;471:2497-2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Heyworth BE, Shindle Mk, Voos JE, Rudzki JR, Kelly BT. Radiologic and intraoperative findings in revision hip arthroscopy. Arthroscopy. 2007;23:1295-1302. [DOI] [PubMed] [Google Scholar]
- 47. Ilizaliturri VM, Jr, Camacho-Galindo J. Endoscopic treatment of snapping hips, iliotibial band, and iliopsoas tendon. Sports Med Arthrosc. 2010;18:120-127. [DOI] [PubMed] [Google Scholar]
- 48. Ilizaliturri VM, Jr, Chaidez C, Villegas P, Briseño A, Camacho-Galindo J. Prospective randomized study of 2 different techniques for endoscopic iliopsoas tendon release in the treatment of internal snapping hip syndrome. Arthroscopy. 2009;25:159-163. [DOI] [PubMed] [Google Scholar]
- 49. Jackson RW. The septic knee-arthroscopic treatment. Arthroscopy. 1985;1:194-197. [DOI] [PubMed] [Google Scholar]
- 50. Jordan MA, Van Thiel GS, Chahal J, Nho SJ. Operative treatment of chondral defects in the hip joint: a systematic review. Curr Rev Musculoskelet Med. 2012;5:244-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kashiwagi N, Suzuki S, Seto Y. Arthroscopic treatment for traumatic hip dislocation with avulsion fracture of the ligamentum teres. Arthroscopy. 2001;17:67-69. [DOI] [PubMed] [Google Scholar]
- 52. Khanduja V, Villar RN. Arthroscopic surgery of the hip: current concepts and recent advances. J Bone Joint Surg Br. 2006;88:1557-1566. [DOI] [PubMed] [Google Scholar]
- 53. Krebs VE. The role of hip arthroscopy in the treatment of synovial disorders and loose bodies. Clin Orthop Relat Res. 2003;406:48-59. [DOI] [PubMed] [Google Scholar]
- 54. Krych AJ, Thompson M, Larson CM, Byrd JW, Kelly BT. Is posterior hip instability associated with cam and pincer deformity? Clin Orthop Relat Res. 2012;470:3390-3397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Larson CM, Giveans MR. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement. Arthroscopy. 2009;25:369-376. [DOI] [PubMed] [Google Scholar]
- 56. Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540-546. [DOI] [PubMed] [Google Scholar]
- 57. Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015-1021. [DOI] [PubMed] [Google Scholar]
- 58. Larson CM, Giveans MR, Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res. 2011;469:1667-1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Larson CM, Kelly BT, Stone RM. Making a case for anterior inferior iliac spine/subspine hip impingement: three representative case reports and proposed concept. Arthroscopy. 2011;27:1732-1737. [DOI] [PubMed] [Google Scholar]
- 60. Larson CM, Ross JR, Stone RM, et al. Arthroscopic management of dysplastic hip deformities: predictors of success and failure with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2016;44:447-453. [DOI] [PubMed] [Google Scholar]
- 61. Lodhia P, Gui C, Chandrasekaran S, Suarez-Ahedo C, Vermula SP, Domb BG. Microfracture in the hip: a matched-control study with average 3-year follow-up. J Hip Preserv Surg. 2015;2:417-427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. MacDonald AE, Bedi A, Horner A, et al. Indications and outcomes for microfracture as an adjunct to hip arthroscopy for treatment of chondral defects in patients with femoroacetabular impingement: a systematic review. Arthroscopy. 2016;32:190-200. [DOI] [PubMed] [Google Scholar]
- 63. Malinin T, Temple HT, Carpenter EM. Induction of regeneration of articular cartilage defects by freeze-dried particulate cartilage allografts. Poster presented at: The ICRS 2009 Meeting; July 7-11, 2009; Miami, FL. [Google Scholar]
- 64. Martin HD, Shears SA, Johnson JC, Smathers AM, Palmer IJ. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011;27:172-181. [DOI] [PubMed] [Google Scholar]
- 65. Matsuda DK. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400-404. [DOI] [PubMed] [Google Scholar]
- 66. McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The watershed labral lesion: its relationship on early arthritis of the hip. J Arthroplasty. 2001;16(8 suppl 1):81-87. [DOI] [PubMed] [Google Scholar]
- 67. Mei-Dan O, McConkey MO, Brick M. Catastrophic failure of hip arthroscopy due to iatrogenic instability: can partial division of the ligamentum teres and iliofemoral ligament cause subluxation? Arthroscopy. 2012;28:440-445. [DOI] [PubMed] [Google Scholar]
- 68. Mosier BA, Quinlan NJ, Martin SD. Peritrochanteric endoscopy. Clin Sports Med. 2016;35:449-467. [DOI] [PubMed] [Google Scholar]
- 69. Nawabi DH, Degen RM, Fields KG, et al. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med. 2016;44:1017-1023. [DOI] [PubMed] [Google Scholar]
- 70. Nelson IR, Keene JS. Results of labral-level arthroscopic iliopsoas tenotomies for the treatment of labral impingement. Arthroscopy. 2014;30:688-694. [DOI] [PubMed] [Google Scholar]
- 71. Philippon MJ, Briggs KK, Carlisle JC, Patterson DC. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res. 2013;471:2492-2496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Philippon MJ, Faucet SC, Briggs KK. Arthroscopic hip labral repair. Arthrosc Tech. 2013;2:e73-e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Philippon MJ, Kuppersmith DA, Wolff AB, Briggs KK. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy. 2009;25:167-174. [DOI] [PubMed] [Google Scholar]
- 74. Philippon MJ, Schenker ML, Briggs KK, Kuppersmith DA, Maxwell RB, Stubbs AJ. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918-1921. [DOI] [PubMed] [Google Scholar]
- 75. Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am. 2009;91:192-197. [DOI] [PubMed] [Google Scholar]
- 76. Ross JR, Bedi A, Stone RM, et al. Intraoperative fluoroscopic imaging to treat cam deformities: correlation with 3-dimensional computed tomography. Am J Sports Med. 2014;42:1370-1376. [DOI] [PubMed] [Google Scholar]
- 77. Sampson TG. Arthroscopic treatment of chondral lesions of the hip. Clin Sports Med. 2011;30:331-348. [DOI] [PubMed] [Google Scholar]
- 78. Sekiya JK, Martin RL, Lesniak BP. Arthroscopic repair of delaminated acetabular cartilage in femoroacetabular impingement. Orthopedics. 2009;32:692-696. [DOI] [PubMed] [Google Scholar]
- 79. Smith MV, Sekiya JK. Hip instability. Sports Med Arthrosc. 2010;18:108-112. [DOI] [PubMed] [Google Scholar]
- 80. Startzman A, Collins D, Carreira D. A systematic literature review of synovial chondromatosis and pigmented villonodular synovitis of the hip. Phys Sportsmed. 2016;44:425-431. [DOI] [PubMed] [Google Scholar]
- 81. Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG. Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy. 2003;19:477-484. [DOI] [PubMed] [Google Scholar]
- 82. Steadman JR, Miller BS, Karas SG, Schlegel TF, Briggs KK, Hawkins RJ. The microfracture technique in the treatment of full-thickness chondral lesions of the knee in National Football League players. J Knee Surg. 2003;16:83-86. [PubMed] [Google Scholar]
- 83. Strauss EJ, Nho SJ, Kelly BT. Greater trochanteric pain syndrome. Sports Med Arthrosc. 2010;18:113-119. [DOI] [PubMed] [Google Scholar]
- 84. Streich NA, Gotterbarm T, Barie A, Schmitt H. Prognostic value of chondral defects on the outcome after arthroscopic treatment of acetabular labral tears. Knee Surg Sports Traumatol Arthrosc. 2009;17:1257-1263. [DOI] [PubMed] [Google Scholar]
- 85. Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24:1407-1421. [DOI] [PubMed] [Google Scholar]
- 86. Vastel L, Lambert P, De Pinieux G, Charrois O, Kerboull M, Courpied JP. Surgical treatment of pigmented villonodular synovitis of the hip. J Bone Joint Surg Am. 2005;87:1019-1024. [DOI] [PubMed] [Google Scholar]
- 87. Voos JE, Rudzki JR, Shindle MK, Martin H, Kelly BT. Arthroscopic anatomy and surgical techniques for peritrochanteric space disorders in the hip. Arthroscopy. 2007;23:1246.e1-1246.e5. [DOI] [PubMed] [Google Scholar]
- 88. Ward JP, Rogers P, Youm T. Failed hip arthroscopy: causes and treatment options. Orthopedics. 2012;35:612-617. [DOI] [PubMed] [Google Scholar]
- 89. Winston P, Awan R, Cassidy JD, Bleakney RK. Clinical examination and ultrasound of self-reported snapping hip syndrome in elite ballet dancers. Am J Sports Med. 2007;35:118-126. [DOI] [PubMed] [Google Scholar]
- 90. Zaltz I, Kelly BT, Hetsroni I, Bedi A. The crossover sign overestimates acetabular retroversion. Clin Orthop Relat Res. 2013;471:2463-2470. [DOI] [PMC free article] [PubMed] [Google Scholar]