Abstract
Background:
Inguinal hernia is a commonly encountered cause of pain in athletes. Because of the anatomic complexity, lack of standard imaging, and the dynamic condition, there is no unified opinion explaining its underlying pathology.
Hypothesis:
Athletes with persistent groin pain would have a high prevalence of inguinal hernia with dynamic ultrasound, and herniorrhaphy would successfully return athletes to activity.
Study Design:
Case-control study.
Level of Evidence:
Level 3.
Methods:
Forty-seven amateur and professional athletes with sports-related groin pain who underwent ultrasound were selected based on history and examination. Patients with prior groin surgery or hip pathology were excluded. Clinical and surgical documentation were correlated with imaging. The study group was compared with 41 age-matched asymptomatic athletes.
Results:
Ultrasound was positive for hernia with movement of bowel, bladder, or omental tissue anterior to the inferior epigastric vessels during Valsalva maneuver. The 47-patient symptomatic study group included 41 patients with direct inguinal hernias, 1 with indirect inguinal hernia, and 5 with negative ultrasound. Of 42 patients with hernia, 39 significantly improved with herniorrhaphy, 2 failed to improve after surgery and were diagnosed with adductor longus tears, and 1 improved with physical therapy. Five patients with negative ultrasound underwent magnetic resonance imaging and were diagnosed with hip labral tear or osteitis pubis. The 41-patient asymptomatic control group included 3 patients with direct inguinal hernias, 2 with indirect inguinal hernias, and 3 with femoral hernias.
Conclusion:
Inguinal hernias are a major component of groin pain in athletes. Prevalence of direct inguinal hernia in symptomatic athletes was greater than that for controls (P < 0.001). Surgery was successful in returning these athletes to sport: 39 of 42 (93%) athletes with groin pain and inguinal hernia became asymptomatic.
Clinical Relevance:
Persistent groin pain in the athlete may relate to inguinal hernia, which can be diagnosed with dynamic ultrasound imaging. Herniorrhaphy is successful at returning athletes to sports activity.
Keywords: athletic pubalgia, sports hernia, ultrasound
Groin pain is a common complaint among athletes involved in various athletic activities that put marked and rapidly shifting stress on the lower abdomen and lower extremities. Imaging studies may not clarify the diagnosis or delineate the pathology.7 There are 4 broad categories of groin pain: dysfunction of adductor longus, osteitis pubis, hernia of various etiologies, and intrinsic hip abnormality.7
There are multiple causes of groin pain in athletes, including hernias, that may stem from multiple different pathologies. One of these is an external oblique muscle aponeurosis tear associated with separation of the conjoined tendon and inguinal ligament. This may be one of the underlying causes of inguinal hernia, and thus groin pain in soccer players,9 and is amenable to surgical treatment by using a 6-layer suture repair.9 Dynamic ultrasound can detect inguinal wall deficiency when clinical examinations are negative despite persistent groin pain.17 A tear of the external oblique muscle aponeurosis superior to the deep inguinal ring without obvious inguinal hernia is sufficient to cause groin pain and is amenable to repair at this level.20 Weakness of the lower abdominal wall is another potential source of groin pain in athletes.1,3,5,7,8,10,12,13,18 Surgical repair, either laparoscopic18 or open,12 is the standard treatment.
Dynamic ultrasound with Valsalva maneuver was explored to obtain a clinical imaging diagnosis of inguinal hernia. We hypothesized that inguinal canal weakness is the causative factor of groin pain in these athletes.
Methods
After institutional review board approval, a retrospective review of electronic patient records was performed identifying all patients examined for inguinal hernia using ultrasound from 2004 to 2008. Forty-seven patients selected on the basis of active participation in professional or amateur sports with pain in the groin directly attributed to athletic activity formed the study group.
All patients were examined using supine ultrasound. Two dedicated musculoskeletal sonographers performed all studies, which were immediately reviewed by the musculoskeletal radiologist and rescanned as necessary. The GE Logic 9 machine (GE Healthcare) and linear 9- to 12-MHz transducer was used in 40 (85%) patients, while a Philips HDI 5000 machine (Philips Healthcare) and linear 9- to 12-MHz transducer was used in the other 7 (15%) patients.
The transducer was placed transversely over the origin of the inferior epigastric artery. A Valsalva maneuver was taught with the patient pressing air against the back of his or her hand. The adequacy of the Valsalva maneuver was judged by the degree of visual distention of the femoral and iliac veins. With repetitive Valsalva, the movement of tissues medially or laterally relative to the inferior epigastric vessels was noted to diagnose direct or indirect inguinal hernia.
The transducer was then moved incrementally medial to the inferior epigastric artery following the pampiniform veins along the spermatic cord (Figure 1). Once the spermatic cord or the round ligament was visualized, movement of the tissues was observed relative to the cord or ligament while repeating the Valsalva maneuver. The cord or ligament was followed down to the level of the medial attachment of the inguinal ligament. It was often necessary to repeat the Valsalva effort 3 to 10 times to observe satisfactory tissue movement over the lower portion of Hesselbach triangle.
Figure 1.
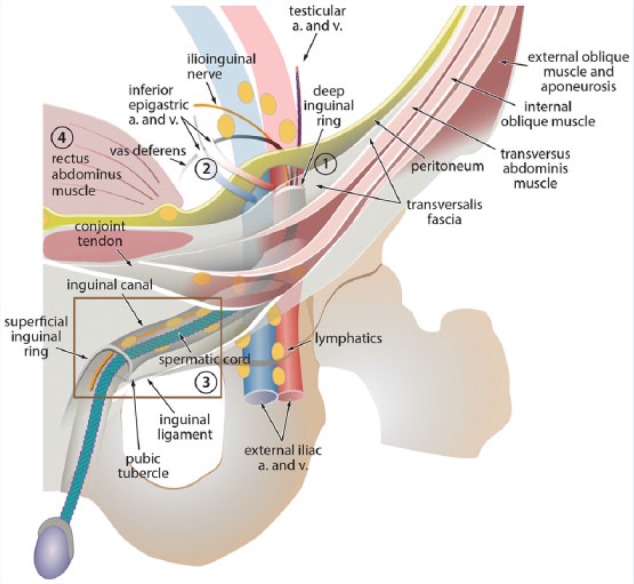
Diagram of the inguinal canal (IC) and its contents. The deep inguinal ring is formed by the transversalis fascia, and the IC is lined by the same layers that line the abdominal wall. The external superficial ring is a triangular opening in the oblique aponeurosis. The inferior epigastric artery (a.) and vein (v.) originate from the external iliac artery and vein and lie medial to the internal inguinal ring. Locations of the abdominal wall hernias in relation to the IC are as follows: Indirect inguinal hernias lie lateral to the inferior epigastric arteries (1); direct inguinal hernias lie medial and inferior to the inferior epigastric vessels (2); femoral hernias lie inferior and medial to the femoral vessels (3); and spigelian hernias lie lateral to the rectus abdominus muscle (4). Reproduced with permission from Revzin MV, Ersahin D, Israel GM, et al. US of the inguinal canal: comprehensive review of pathologic processes with CT and MR imaging correlation. Radiographics. 2016;36:2028-2048.
From the medial aspect of the inguinal ligament, the transducer was moved over the superior pubic ramus to where it showed the narrowest cross-section of the pectineus muscle (Figure 1). This muscle medial to the femoral vein bounds the femoral canal. Valsalva maneuver was repeated in search of movement ventral to the pectineus muscle, where femoral hernia can be identified. The last Valsalva maneuver was performed with the transducer placed transversely over the obturator canal and external obturator muscle to assess for obturator hernia.
To exclude possible hip and pubic symphysis abnormalities, each study also included assessment of the external hip capsule with longitudinal images through the iliofemoral ligament from its origin deep to the origin of the rectus femoris to its insertion on the femur. The pubic symphysis was assessed for symmetry of the pubic bones and cortical smoothness. The adductor longus origin was assessed, and the long axis of the muscle was compared with the opposite side for possible tear.
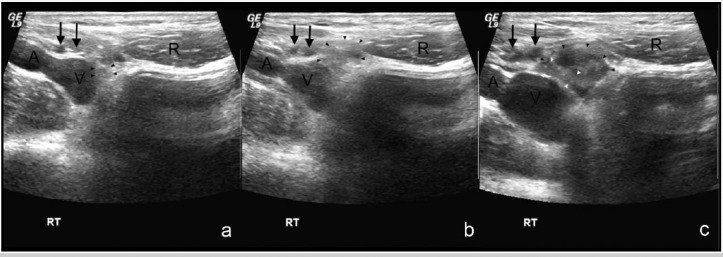
The criterion used to diagnose inguinal hernias by ultrasound was movement of bowel, bladder, or omental lipomatous tissue in any combination anterior to the inferior epigastric vessels with or without Valsalva maneuver. A direct inguinal hernia was defined as tissue movement medial to the inferior epigastric vessels. An indirect inguinal hernia was defined as tissue movement lateral to the inferior epigastric vessels extending medially over the vessels. A femoral hernia was defined as tissue movement medial to the femoral vessels and deep to the inguinal ligament. An obturator hernia was defined as tissue movement through the obturator foramen. The overall finding of transient direct inguinal hernia of the right groin (Figure 2), progressive left direct inguinal hernia (Figure 3), and detailed panoramic view of the left groin structures (Figure 4) are shown.
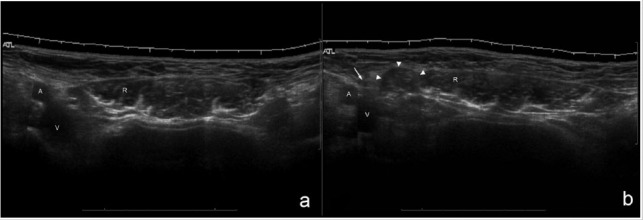
Figure 2.
Panoramic ultrasound views of the lower abdomen before and during Valsalva maneuver demonstrate a right direct inguinal hernia in a 34-year-old male hockey player who presented with right groin pain. (a) Panoramic view demonstrates right and left rectus abdominis muscles without soft tissue protrusion. The anatomic landmarks of the right rectus abdominis muscle (R), iliac artery (A), and iliac vein (V) are marked. (b) Panoramic view with Valsalva maneuver demonstrates protrusion of soft tissue (white arrowheads) medial to the inferior epigastric vessels (white arrow) and lateral to the right abdominal rectus muscle (R) compatible with right direct inguinal hernia.
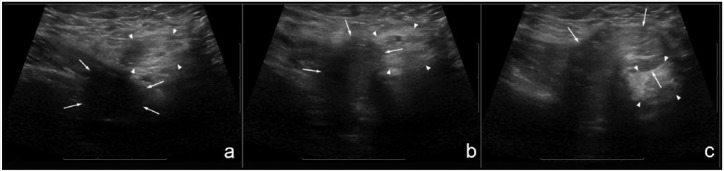
Figure 3.
A 38-year-old male hockey player who presented with pain in the left groin. Positive dynamic sonograms show start, halfway, and full Valsalva efforts. (a) At the beginning of the Valsalva maneuver, a focal defect of the aponeurosis (arrows) is seen without herniation of the soft tissue; the spermatic cord (arrowheads) is seen slightly lateral to it. (b) During halfway Valsalva effort, hypoechoic, likely omental, tissue (arrows) protrudes via the defect in the aponeurosis medial to the spermatic cord (arrowheads), displacing the cord laterally. (c) With full Valsalva effort, more echogenic tissue (arrows) protrudes medially and over the spermatic cord (arrowheads), displacing the cord posteriorly proving a direct inguinal hernia.
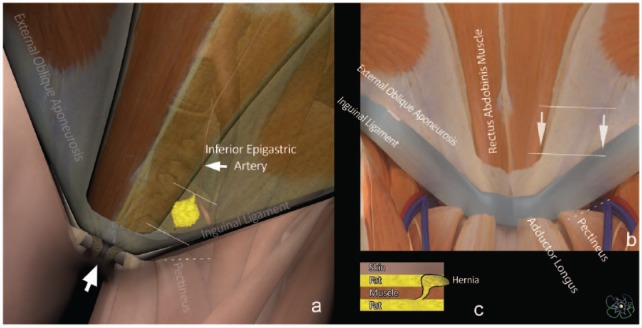
Figure 4.
Illustration of direct inguinal hernia of the lower abdomen in an athlete. (a) The fat-containing hernia (yellow) is shown as a protrusion of tissue through the Hesselbach triangle. With the rectus abdominis and the external oblique aponeurosis made transparent, the lateral border of that triangle is visible as the inferior epigastric artery in the abdomen; the inguinal ligament forms the inferior border and the lateral rectus abdominis the medial border of the triangle. Each of these landmarks is visible by ultrasound. The white lines on the drawing indicate the extent of the ultrasound scan from the origin of the inferior epigastric artery to the corner where the medial inguinal ligament and distal lateral rectus abdominis meet. The vertical arrow points at the symphysis pubis, an easily recognizable osseous landmark that helps distinguish right- and left-sided hernias. (b) In an athlete without hernia, this frontal view illustrates the same anatomy as in (a) but without the transparency of the rectus abdominis and of external oblique aponeurosis. The lines show the orientation of the linear transducer over the Hesselbach triangle. The arrows show the movement of the transducer from beginning to end of the scan. In both (a) and (b), the dashed line shows the position of the transducer for detection of femoral hernias, with pectineus and inguinal ligaments as landmarks. (c) This cross-section of the abdomen delineates why direct hernias are so challenging to detect. The abdominal fatty tissue that directly transgresses the abdominal wall in this type of hernia does not contrast much with identical fatty tissue in the hypodermis.
Medical records pertinent to the episodes of groin pain were reviewed and correlated with surgical findings and outcomes. Only patients with a history suggestive of activity-related hernia and with negative or equivocal clinical examination findings are routinely referred for ultrasound examination. All operations were performed by 1 of 4 general surgeons. Procedures were performed using local anesthesia and conscious sedation so that Valsalva maneuvers could be performed on request. Each surgical patient was scheduled to see the surgeon for a minimum of 2 postoperative visits, between 1- and 6-month total duration.
All ultrasound studies were read initially by 1 of 3 experienced musculoskeletal radiologists. All ultrasound examinations were blinded to the previous results, surgical findings, and clinical outcomes. One discrepancy was noted, where a direct inguinal hernia was initially diagnosed as negative but was reversed during review.
The results were compared with an asymptomatic control group of 41 healthy male patients prospectively recruited from the radiology and orthopaedic residency programs (mean age, 28.0 years; range, 22-35 years; median age, 27.9 years). These participants regularly engaged in athletic activities and were all scanned and reviewed by senior staff.
A standard chi-square test for proportions was used to test the difference in direct hernia prevalence between the symptomatic and asymptomatic groups. The Fisher exact test was used to compare indirect and femoral hernias in the presence of sparse data. SAS version 9.2 software was utilized to perform statistical analyses (SAS Institute).
Results
The length of clinical follow-up ranged from 0 days to more than 10 years, with a mean follow-up of 22 months (Table 1). Three patients returned to college shortly after surgery and were not examined physically in the office during follow-up; they were contacted via telephone 2 months after surgery and reported satisfactory results.
Table 1.
Study group demographics
| n | Mean Age (Range), y | Median Age, y | |
|---|---|---|---|
| Sex | |||
| Male | 39 | 32.3 (16-62) | 32.5 |
| Female | 8 | 22.3 (12-36) | 19.5 |
| Sport | |||
| Ice hockey | 16 | ||
| Soccer | 6 | ||
| Football | 5 | ||
| Track/running | 4 | ||
| Weight lifting | 4 | ||
| Baseball | 3 | ||
| Figure skating | 2 | ||
| Tennis | 2 | ||
| Wrestling | 2 | ||
| Basketball | 2 | ||
| Volleyball | 1 |
Forty-two of 47 patients with pain demonstrated inguinal hernia on ultrasound: 41 patients had direct inguinal hernias and 1 patient had an indirect inguinal hernia. Of 41 patients with direct hernias, 27 hernias were unilateral and 14 hernias were bilateral. Of 14 patients with bilateral inguinal hernias, 11 had symptoms bilaterally. Three patients were symptomatic unilaterally with asymptomatic smaller contralateral hernias on ultrasound. No femoral or obturator hernias were found. No pubic symphysis or hip joint abnormalities were noted on ultrasound imaging.
Thirty-nine patients with positive ultrasound findings demonstrated either complete pain resolution or significant improvement with surgery and were classified as true positives. One patient in this group had an indirect inguinal hernia found on ultrasound and confirmed at surgery. The true positive group also included 24 patients with unilateral direct inguinal hernias and 14 patients with bilateral direct inguinal hernias. All 11 patients with symptomatic bilateral inguinal hernias were operated on on both sides. The 3 patients with bilateral hernias but only unilateral symptoms were operated on only on the symptomatic side with the larger herniation.
Unilateral direct inguinal hernias were observed in 2 patients who failed to improve after surgical repair. These patients were later diagnosed with adductor longus tear and adductor longus tendinosis. A single patient with ultrasound findings of unilateral direct inguinal hernia had pain resolution with physical therapy alone. These 3 patients were classified as false positives.
Surgical exploration in the direct hernia group corroborated ultrasound findings in describing a hernial sac, weakness in the transversalis fascia wall, or defect in the external oblique aponeurosis during the intraoperative Valsalva maneuver. Although surgical findings may have overlapped in patients who underwent repair, the primary physical finding was recorded and utilized. Findings were not recorded in 1 patient (Table 2). None of these findings had been noted during clinical testing preoperatively.
Table 2.
Surgical findings
| Surgical Finding | Patients, n |
|---|---|
| Hernia sac identified | 10 |
| Weakening/laxity of the transversalis fascia | 12 |
| Frank defect of the external oblique aponeurosis | 16 |
| Not recorded | 1 |
Five patients had negative ultrasound examinations and had alternative diagnoses assigned. Of this group, 3 patients had labral tears shown by magnetic resonance imaging (MRI); all 3 had pain relief with image-guided injection of 1% lidocaine in the hip joint. One patient underwent open surgery for removal of a cam deformity of the femoral head, and 1 patient was given a diagnosis of osteitis pubis based on a nuclear scan; his symptoms improved with a corticosteroid injection in the symphysis pubis. One patient was taken to surgery for hernia repair despite a negative ultrasound. A spermatic cord lipoma was identified intraoperatively but no hernia. This patient was later found to have a labral tear by MRI. These 5 patients were classified as true negatives. No false negative patients were identified.
The prevalence of a direct inguinal hernia in this cohort of symptomatic athletic individuals was 87% (41/47), and the patients were successfully treated with surgical repair. The 41-patient, healthy control group revealed 3 direct inguinal, 2 indirect inguinal, and 3 femoral asymptomatic hernias, with 12% (5/41) prevalence of inguinal hernias and 20% (8/41) prevalence of all groin hernias (Table 3).
Table 3.
Distribution of hernias between symptomatic and asymptomatic control patients
| Hernia Type | Symptomatic Patients | Asymptomatic Patients | P |
|---|---|---|---|
| Direct inguinal | 87% (41/47) | 7% (3/41) | <0.001 |
| Indirect inguinal | 2% (1/47) | 5% (2/41) | 0.596 |
| Femoral | 0% (0/47) | 7% (3/41) | 0.097 |
The sensitivity of dynamic ultrasound in the symptomatic group, as judged by combined surgical and clinical follow-up, was 100% (positive predictive value, 93%; negative predictive value, 100%). Success was measured by 95% (39/41) of patients with sonographically proven inguinal hernia who became asymptomatic or who had significantly improved after hernia repair surgery.
Discussion
Groin pain can be a source of decreased performance and cessation of athletic activities for recreational and high-level athletes. Multiple pathologies may be root causes of athletic pubalgia, including adductor and rectus abdominis injuries. Intrinsic hip injury and osteitis pubis can also lead to groin pain in the athlete, further complicating the diagnosis. One component of groin pain in athletes is inguinal hernia.13,17 Disproportionate pull of the adductor and abdominal rectus muscles as the proposed mechanism for creation of inguinal hernias in athletes is accepted by some.11,19 In addition to a shear injury, the stress may also lead to stretching, thinning, and tearing of the pelvic floor.14 Injured transverse abdominal muscle and fascia of the pelvic floor, which normally work as a “shutter mechanism” during rectus contraction, are no longer able to provide reinforcement to the posterior wall of the inguinal canal.16
Complaints are typically nonspecific and isolated to periods of intense activity, and diagnosis can be difficult and take time. Direct inguinal hernias resulting in weakening of the posterior wall of the inguinal canal are difficult to diagnose by physical examination alone.15 Imaging studies are called upon to assist with diagnosis for these patients.
Intrinsic hip pathology, osteitis pubis, stress fractures, and avulsion injuries all commonly produce sports-related groin pain.14 Many of these may be visualized using MRI or computed tomography. Pubic symphysis instability and muscular insertional injury are well described and have been proposed as a primary cause of athletic groin pain.21 While definitely a valid explanation, this can be related to abdominal aponeurosis tear and resultant inguinal hernia. Dynamic ultrasound with provocative Valsalva maneuver may enable a quick and accurate diagnosis.4 Static imaging without Valsalva maneuver would miss the majority of hernias, tissue disruption, or laxity as presented on MRI (Figure 5) and ultrasound images (Figure 6). A larger study of athletes with groin pain and a clinical diagnosis of athletic pubalgia and “sports hernia” demonstrated only 2 of 102 patients with hernia on MRI.21 In that study, no Valsalva maneuver was utilized during MRI or surgery, precluding a direct comparison with our data. The patient population imaged was also different, as may be the definition of inguinal hernia, leading to further discrepancies in the results obtained.
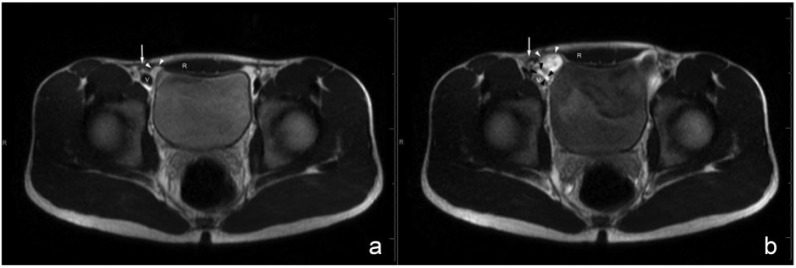
Figure 5.
Dynamic single-shot T2-weighted magnetic resonance imaging (MRI) of the lower abdomen before and during Valsalva maneuver demonstrate a right direct inguinal hernia in a 17-year-old male football player who presented with bilateral groin pain. (a) Without Valsalva maneuver, MRI demonstrates no herniation. (b) With full Valsalva effort, the bowel (black arrowheads) and omentum (white arrowheads) protrude medial to the right inferior epigastric vessels (white arrow), which is compatible with a direct inguinal hernia. Different soft tissues protrude in the left groin, findings that are also compatible with direct inguinal hernia. A supplemental video (available in the online version of this manuscript) shows the outward bulging of the anterior abdominal musculature and distention of the iliac veins (V), proving adequacy of Valsalva strain. During the Valsalva maneuver, tissues herniate medial to the epigastric arteries in both groins. R, rectus abdominus muscle.
Figure 6.
Sonographic correlation to the dynamic magnetic resonance imaging seen in Figure 5 confirming direct right inguinal hernia in the 17-year-old male football player who presented with bilateral groin pain. (a) At the beginning of Valsalva maneuver, mild right groin laxity with a wisp of soft tissue (black arrowheads) is seen lateral to the rectus abdominis muscle (R) and medial to the inferior epigastric vessels (arrows). (b) With halfway Valsalva effort, the echogenic soft tissues (black arrowheads) protrude medial to the inferior epigastric vessels (arrows). (c) With full Valsalva effort, the heterogeneous soft tissue (black arrowheads) and part of the bowel (white arrowheads) protrude medial to the inferior epigastric vessels (arrows). Note progressive distention of the iliac artery (A) and iliac vein (V) and inferior epigastric vessels (black arrows) with Valsalva maneuver.
Surgical findings in patients with sports-induced hernias may include thinning and weakening of the transversalis fascia with possible separation of the inguinal ligament from the conjoined tendon.10 The surgeons in this study did not report attenuated tissues with lost elasticity, commonly seen in older individuals who typically have direct inguinal hernias.6 No patients required reoperation or had any postsurgical complications.2 The ability to surgically mobilize and approximate the torn aponeurosis without tension further suggests the presence of healthy and robust elastic tissues.
A high prevalence of direct inguinal hernia in symptomatic athletes was demonstrated compared with a significantly lower prevalence of inguinal hernia in the asymptomatic control group. This supports direct inguinal hernia as an important component of hernia in athletes with groin pain. Consistent pain resolution, alleviation of sports-related symptoms, and return to play after hernia repair further supports the concept that weakening of the posterior wall of the inguinal canal contributes to groin pain and that surgical repair is effective in treating this pathology. Because none of the inguinal hernias were palpable by clinical examination and the defect/laxity of the aponeurosis could only be reliably seen with an intraoperative Valsalva maneuver, dynamic ultrasound imaging forms an important part of the diagnostic approach for athletes with groin pain and is accurate for inguinal hernia evaluation. These examinations are particularly helpful with the typically prolonged and delayed diagnostic process for these patients. Surgical repair provides consistent pain relief and successful return to play in athletes diagnosed with inguinal hernias.
The finding of direct inguinal hernias in 3 asymptomatic athletic individuals in the control group and 3 patients from the study group calls for clinical correlation before considering surgical intervention, as there may be other pathological entities with similar clinical presentation. It also may be that the incidental hernia in the groin may be an early stage of inguinal hernia in the athlete, possibly becoming symptomatic if and when the hernia reaches a size allowing protrusion of the omentum and/or nerve stretching. Prospective follow-up of those individuals may further our understanding of the natural history of the condition. Several patients evaluated for hernia because of athletic groin pain were later diagnosed with adductor longus injuries or hip labrum tears. This underscores the significant overlap in the clinical presentations of patients with pain from different causes.
The strength of our study lies in demonstrating the utility of dynamic ultrasound examination of the groin with Valsalva maneuver. Correlation with surgical observations was made possible because of the use of local anesthesia with conscious sedation. The limitations of our study relate to its retrospective design, the relatively small sample size, the inherent bias introduced by the sonographer who knew the patient’s symptoms and by the operating surgeon who was aware of the results of the ultrasound prior to the surgical procedure, as well as selective referral of patients for ultrasound examination based on their clinical presentation. Also, some patients had a relatively short formal documented clinical follow-up.
Conclusion
Athletic patients with complaints of persistent activity-related groin pain had a higher prevalence of inguinal hernia than an asymptomatic control population. Dynamic ultrasound evaluation can be a useful tool in the diagnosis of this complex clinical entity. Surgical repair of inguinal hernia was successful in returning athletes to their chosen activities.
Supplementary Material
Footnotes
The following author declared potential conflicts of interest: Marnix van Holsbeeck, MD, receives royalties from Elsevier and has stock/stock options in General Electric.
References
- 1. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396. [DOI] [PubMed] [Google Scholar]
- 2. Amid PK. Groin hernia repair: open techniques. World J Surg. 2005;29:1046-1051. [DOI] [PubMed] [Google Scholar]
- 3. Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533. [DOI] [PubMed] [Google Scholar]
- 4. Caudill P, Nyland J, Smith C, Yerasimides J, Lach J. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964. [DOI] [PubMed] [Google Scholar]
- 5. Edelman DS, Selesnick H. “Sports” hernia: treatment with biologic mesh (Surgisis): a preliminary study. Surg Endosc. 2006;20:971-973. [DOI] [PubMed] [Google Scholar]
- 6. Fallis LS. Direct inguinal hernia. Ann Surg. 1938;107:572-581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15:507-514. [DOI] [PubMed] [Google Scholar]
- 8. Genitsaris M, Goulimaris I, Sikas N. Laparoscopic repair of groin pain in athletes. Am J Sports Med. 2004;32:1238-1242. [DOI] [PubMed] [Google Scholar]
- 9. Gilmore J. Groin pain in the soccer athlete: fact, fiction, and treatment. Clin Sports Med. 1998;17:787-793. [DOI] [PubMed] [Google Scholar]
- 10. Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med. 1993;27:58-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Harmon KG. Evaluation of groin pain in athletes. Curr Sports Med Rep. 2007;6:354-361. [PubMed] [Google Scholar]
- 12. Joesting DR. Diagnosis and treatment of sportsman’s hernia. Curr Sports Med Rep. 2002;1:121-124. [DOI] [PubMed] [Google Scholar]
- 13. Kumar A, Doran J, Batt ME, Nguyen-Van-Tam JS, Beckingham IJ. Results of inguinal canal repair in athletes with sports hernia. J R Coll Surg Edinb. 2002;47:561-565. [PubMed] [Google Scholar]
- 14. LeBlanc KE, LeBlanc KA. Groin pain in athletes. Hernia. 2003;7:68-71. [DOI] [PubMed] [Google Scholar]
- 15. Moeller JL. Sportsman’s hernia. Curr Sports Med Rep. 2007;6:111-114. [DOI] [PubMed] [Google Scholar]
- 16. Nam A, Brody F. Management and therapy for sports hernia. J Am Coll Surg. 2008;206:154-164. [DOI] [PubMed] [Google Scholar]
- 17. Orchard JW, Read JW, Neophyton J, Garlick D. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian rules footballers. Br J Sports Med. 1998;32:134-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Paajanen H, Syvahuoko I, Airo I. Totally extraperitoneal endoscopic (TEP) treatment of sportsman’s hernia. Surg Laparosc Endosc Percutan Tech. 2004;14:215-218. [DOI] [PubMed] [Google Scholar]
- 19. Verrall GM, Slavotinek JP, Fon GT. Incidence of pubic bone marrow oedema in Australian rules football players: relation to groin pain. Br J Sports Med. 2001;35:28-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Williams P, Foster ME. ‘Gilmore’s groin’—or is it? Br J Sports Med. 1995;29:206-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zoga AC, Kavanagh EC, Omar IM, et al. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology. 2008;247:797-807. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.