Abstract
Study Design:
Retrospective cohort study.
Objective:
To determine if patients fused with multi-rod constructs to the pelvis have a lower incidence of lumbosacral rod failure and pseudarthrosis than those fused with dual-rod constructs.
Methods:
We performed a retrospective review of consecutive adult spinal deformity patients who underwent long fusion to the pelvis. Inclusion criteria were >5 levels, primary fusion or revision for L5-S1 pseudarthrosis, and minimum 1-year follow-up. Revision patients with indications other than L5-S1 pseudarthrosis were excluded. One-year follow-up plain radiographs were reviewed for rod integrity, and computed tomography scan (CT) was obtained whenever rod breakage was observed. Dual-rod and multi-rod (3 or 4 rods) cohorts were statistically compared.
Results:
There were 31 patients with 15 in the dual-rod group and 16 in the multi-rod group, with average ages of 68 ± 9 and 63 ± 12 years, respectively. No patients in the multi-rod group experienced rod fracture, whereas 6 in the dual-rod group fractured a rod (P = .007), with 4 occurring at the lumbosacral junction (P = .04). CT scan in the 4 lumbosacral rod fracture cases, and surgical exploration in 3, confirmed pseudarthrosis and hypertrophic nonunion at the L5-S1 junction.
Conclusion:
Patients with dual-rod constructs had a statistically greater incidence of lumbosacral pseudarthrosis with implant failure than those with multi-rod constructs. CT and surgical exploration showed hypertrophic nonunion as opposed to oligo- or atrophic nonunion. This suggests that mechanical instability, not biology, is the main reason for failure, and could be addressed with the use of multi-rods.
Keywords: multi-rod fusion, pelvic fixation, lumbosacral junction, pseudarthrosis, hypertrophic nonunion, rod fracture
Introduction
Long spinal fusion to the sacrum is indicated for a variety of degenerative, traumatic, and adult deformity conditions. This procedure can cause several complications including nerve root injury, loss of lumbar lordosis, and pseudarthrosis.1-3 Pseudarthrosis is a particularly prevalent complication and most commonly occurs at the 3-column osteotomy site or the lumbosacral junction.4,5
High biomechanical loads and shear forces make the lumbosacral junction especially difficult to stabilize during fusion.6-9 Long fusion constructs also increase the lever arm and moment on the lumbosacral junction, adding to the already rigorous mechanical environment.10 The longer the fusion construct, the higher the incidence of lumbosacral pseudarthrosis, suggesting that increased mechanical forces contribute to nonunion.11 This highlights the need for rigid surgical instrumentation in order to stabilize the L5-S1 junction.
Hypertrophic nonunion develops in long bones when instability causes fracture nonunion, despite adequate callus formation and bone production.12 In contrast, oligotrophic and atrophic nonunion occur when lack of vasculature and physiologic bone production prevent union.13 Although these principles were originally described for the appendicular skeleton, extrapolation to the spine may suggest that hypertrophic, as opposed to oligo- or atrophic, nonunion at the L5-S1 junction results from mechanical instability.
Several modifications to techniques and instrumentation for pelvic fixation have been developed to increase stability and enhance fusion rates.14,15 Despite these advances, pseudarthrosis and rod breakage remain common difficulties of long fusion to the sacrum.4,16,17
Multi-rod constructs have shown increased biomechanical stability when compared with canonical dual-rod constructs, but the paucity of comparative cohort studies leaves the efficacy of multi-rod constructs relatively unknown.18,19 Our objective with this retrospective cohort study was to compare the incidence of lumbosacral pseudarthrosis and rod failure between adult spinal deformity cohorts fused with either a dual-rod or multi-rod construct, and to investigate the kind of nonunion at the site of the pseudarthrosis.
Methods
Patient Sample
The institutional review board approved this study. We retrospectively reviewed consecutive adult spinal deformity patients with fusion to the sacrum by a single surgeon at a single center between 2011 and 2015. Inclusion criteria were >5 levels fused, primary fusion, extension to the sacrum and pelvis, and revision for L5-S1 pseudarthrosis. Patients younger than 18 years of age and adults who underwent a revision surgery for any indication other than L5-S1 pseudarthrosis were excluded. Patients fused with dual-rod constructs consisted of the first cohort, while those fused with multi-rod constructs consisted of the second cohort. All demographic and operative information were collected from the hospital medical records. Coronal and sagittal measurements were made on the most recent preoperative standing radiographs and the most immediate (within 6 weeks) postoperative standing radiographs.
Dual-Rod Constructs and Indications
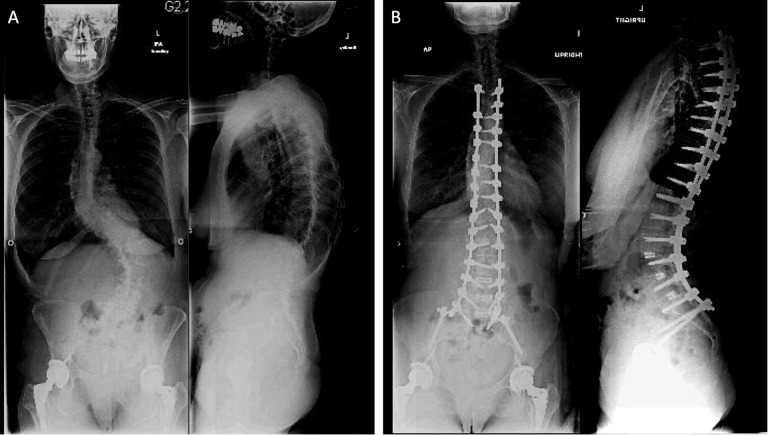
Patients fused with dual-rod constructs to the sacrum received a single rod on each side of the spinal column fixed to the pelvis with bilateral iliac screws and bilateral S1 screws (Figure 1). All rods used in this cohort were 5.5 mm in diameter. All patients received local autograft bone, allograft in the form of demineralized bone matrix, and recombinant human bone morphogenetic protein-2 (rh-BMP2) as a fusion adjunct.
Figure 1.
Representative AP and lateral radiographs of a dual-rod construct: (A) preoperative and (B) postoperative.
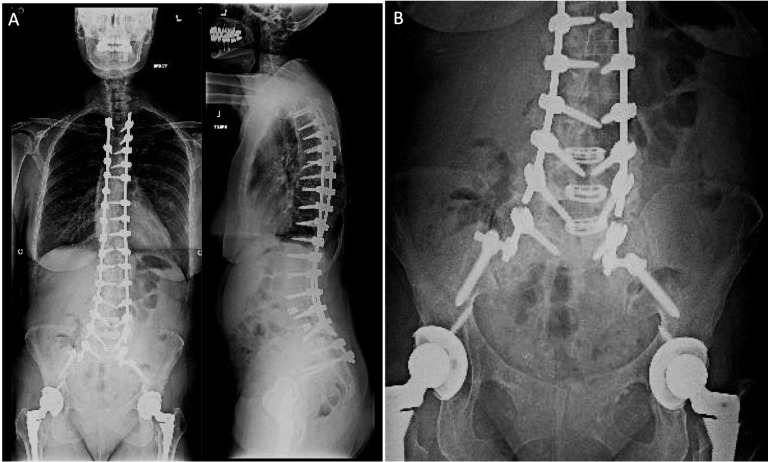
Multi-Rod Constructs and Indications
Patients fused with multi-rod constructs had bilateral iliac and bilateral sacral screws for pelvic fixation. Patients received either a single-rod on one side of the spinal column and an additional 1 or 2 rods using connectors. The additional rods did not extend the entire length of the construct, but extended to at least L1 in all cases (Figure 2). All rods used in this cohort were 5.5 mm in diameter. All patients received local autograft bone, allograft in the form of demineralized bone matrix, and rh-BMP2 as a fusion adjunct.
Figure 2.

AP and lateral radiographs of a representative multi-rod construct.
Cohort Allocation and Choice of Rod Material
The treating surgeon began treating spinal deformity patients in 2011 with dual-rod constructs and anecdotally noticed implant failure, and so he switched to multi-rod constructs.
Titanium rods were used in patients who had osteoporosis or had poorer bone quality judged by the surgeon intraoperatively. Given the less stiff properties of titanium, it was thought there would be less screw pullout if this material was used on those patients with poorer bone quality.
Rod Failure and Pseudarthrosis
Broken rods were determined on at least 1-year anterior-posterior and lateral radiographs. Whenever there were broken rods, 1-year postoperative computed tomography (CT) scans were reviewed to confirm the presence of lumbosacral pseudarthrosis based on criteria described by Shah et al.20 Any patient who underwent a revision surgery for L5-S1 pseudarthrosis also had motion confirmed during surgical exploration.
Hypertrophic Nonunion
To determine hypertrophic nonunion, all 1-year CT scans of patients who had a lumbosacral pseudarthrosis were analyzed. Hypertrophic nonunion was diagnosed based on abundant nonbridging callus formation at the index surgical level. Thin slice CT scans, which are accurate for identifying nonunion, were used.21,22
Statistical Analysis
All statistical analyses were performed with Prism GraphPad V6 (La Jolla, CA). Continuous variables were compared between cohorts with an unpaired t test, and categorical variables were compared with a Fisher’s exact test. Statistical significance was taken at P < .05.
Results
Patient Cohorts
We analyzed a total of 31 patients with 15 in the dual-rod group and 16 in the multi-rod group. There were no significant differences between the 2 groups with respect to several important demographic and operative characteristics, including age, gender, time since surgery, smoking status, hypertension, osteoporosis, oral steroid use, and Charlson Comorbidity Index (Table 1).23 Additionally, indication for surgery, number of levels fused, and preoperative coronal Cobb and preoperative sagittal vertical axis were not statistically different between the groups.
Table 1.
Preoperative Characteristics Between the Dual-Rod and Multi-Rod Cohorts.
| Dual-Rod (N = 15) | Multi-Rod (N = 16) | P | |
|---|---|---|---|
| Age (years) | 68 ± 9 | 63 ± 12 | .2152 |
| Male | 5 | 4 | .7403 |
| Female | 10 | 12 | |
| Time since surgery (months) | 36.34 ± 16.87 | 28.73 ± 7.98 | .1156 |
| Smoking | 0 | 1 | 1.0000 |
| HTN | 7 | 11 | .2852 |
| Osteoporosis | 3 | 2 | .6539 |
| Oral steroids | 0 | 0 | 1.0000 |
| CCI | 2.67 ± 1.40 | 2.38 ± 1.15 | .5292 |
| Primary fusion | 10 | 7 | .2852 |
| Extension to sacrum | 4 | 3 | .6851 |
| Revision for L5-S1 pseudo | 1 | 6 | .0829 |
| Levels fused | 11.33 ± 3.60 | 11.44 ± 3.74 | .9376 |
| Preoperative coronal Cobb (°) | 34.60 ± 22.25a | 32.61 ± 22.92 | .8120 |
| Preoperative SVA (mm) | 89.48 ± 68.42a | 117.30 ± 91.07 | .3698 |
Abbreviations: HTN, hypertension; CCI, Charlson Comorbidity Index; SVA, sagittal vertical axis.
aIn the dual-rod group, one patient did not have preoperative AP and lateral radiographs available for measurement, and a second patient did not have lateral radiograph with landmarks visible for measurement, so preoperative coronal cobb N = 14 and preoperative SVA N = 13 for the dual-rod group.
Operative Characteristics
Operatively, there were no statistically significant differences between the groups in terms of L5-S1 transforaminal lumbar interbody fusing, amount of rh-BMP2 used, operative time, estimated blood loss, or material of rod used (Table 2).
Table 2.
Operative Characteristics Between the Dual-Rod and Multi-Rod Cohorts.
| Dual-Rod (N = 15) | Multi-Rod (N = 16) | P | |
|---|---|---|---|
| Interbody | 13 | 13 | 1.0000 |
| Rh-BMP2 (mg) | 21.47 ± 11.58 | 26.25 ± 10.01 | .2275 |
| OR time (minutes) | 499.30 ± 139.70 | 512.00 ± 149.1 | .8083 |
| EBL (mL) | 2420 ± 2405 | 2291 ± 1993 | .8713 |
| Cobalt chrome | 11 | 10 | .4397 |
| Titanium | 4 | 6 |
Abbreviations: Rh-BMP2, recombinant human bone morphogenetic protein-2; OR, operating room; EBL, estimated blood loss.
Rod Breakage, Pseudarthrosis, and Hypertrophic Nonunion
A total of 6 patients experienced rod failure, all in the dual-rod group. The incidence of rod breakage between the 2 groups was statistically significant (P = .0068; Table 3). Of the 6 cases, 5 were instrumented with cobalt chrome alloy rods, and one was instrumented with a titanium alloy rod.
Table 3.
Lumbosacral Pseudarthrosis, Broken Rods, and Type of Rod Used Between the Dual-Rod and Multi-Rod Cohorts.a
| Dual-Rod (N = 15) | Multi Rod (N = 16) | P | |
|---|---|---|---|
| Rod fracture at any level | 6 | 0 | .0068 |
| L5-S1 rod fracture/pseudo | 4 | 0 | .0434 |
| Cobalt chrome | 5 | ||
| Titanium | 1 |
aBoldface indicates statistical significance.
Four of the rod fractures occurred at the lumbosacral junction (Figure 3). All 4 had pseudarthrosis confirmed on CT, and 3 of these patients had the pseudarthrosis confirmed intraoperatively during revision surgery. The fourth patient is currently not symptomatic and has yet to undergo revision. The rate of lumbosacral pseudarthrosis between the 2 groups was statistically significant (P = .0434; Table 3). The average time to rod fracture was 17.18 ± 8.92 months.
Figure 3.
(A) AP and lateral radiographs demonstrating bilateral broken rods at the lumbosacral junction. (B) Zoomed AP view of the lumbosacral junction.
All 4 lumbosacral pseudarthroses showed abundant, nonbridging callus formation at the lumbosacral junction on 1-year CT scan (Figure 4). Three of these patients were noted to have copious soft callus formation at the L5-S1 junction during revision surgery. These findings suggest a nonunion with abundant fibrous callus formation that clinically appears grossly similar to a hypertrophic nonunion.
Figure 4.

Sagittal CT scan of the lumbosacral junction showing pseudarthrosis as well as nonbridging callus formation, indicating hypertrophic nonunion.
Intact Rods Versus Broken Rods
There were no significant differences between dual-rod patients who did not experience rod fracture compared to the 6 dual-rod patients who did with respect to demographic characteristics, comorbidities, number of levels fused, and operative characteristics (Table 4). The patients who experienced rod fracture did, however, have a greater pre- and postoperative Cobb angle, and smaller postoperative thoracolumbar alignment and thoracic kyphosis Table 4). There were no differences in any other pre- or postoperative sagittal alignment measurements.
Table 4.
Characteristics of Dual-Rod Patients Who Experienced a Rod Fracture and Those Who Did Not.a
| Dual-Rod No Fracture (N = 9) | Dual-Rod Fracture (N = 6) | P | |
|---|---|---|---|
| Age (years) | 69 ± 9 | 66 ± 8 | .5068 |
| Male | 4 | 1 | .5804 |
| Female | 5 | 5 | |
| Smoking | 0 | 0 | 1.0000 |
| HTN | 4 | 3 | 1.0000 |
| Osteoporosis | 1 | 2 | .5253 |
| CCI | 2.67 ± 1.32 | 2.67 ± 1.63 | >.9999 |
| Levels fused | 11.22 ± 3.63 | 11.50 ± 3.89 | .8899 |
| Interbody | 7 | 5 | 1.0000 |
| Rh-BMP2 (mg) | 22.00 ± 12.00 | 20.67 ± 11.98 | .8362 |
| Preoperative coronal Cobb (°) | 17.94 ± 9.77b | 56.82 ± 10.83 | <.0001 |
| Preoperative TL (°) | 24.14 ± 21.04b | 11.83 ± 18.73 | .2927 |
| Preoperative TK (°) | 21.57 ± 11.91b | 27.50 ± 19.87 | .5198 |
| Preoperative SVA (mm) | 100.30 ± 86.68b | 76.89 ± 43.20 | .5622 |
| Postoperative coronal Cobb (°) | 9.89 ± 8.28c | 22.45 ± 9.14 | .0197 |
| Postoperative TL (°) | 19.00 ± 19.65c | −6.00 ± 20.48 | .0392 |
| Postoperative TK (°) | 38.63 ± 8.90c | 22.67 ± 18.06 | .0490 |
| Postoperative SVA (mm) | 65.62 ± 73.69c | 18.70 ± 33.97 | .1759 |
Abbreviations: HTN, hypertension; CCI, Charlson Comorbidity Index; rh-BMP2, recombinant human bone morphogenetic protein-2; TL, thoracolumbar alignment; TK, thoracic kyphosis; SVA, sagittal vertical axis.
aBoldface indicates statistical significance.
bIn the no fracture group, one patient did not have preoperative AP and lateral radiographs available for measurement, and a second patient did not have lateral radiograph with landmarks visible for measurement, so preoperative coronal Cobb N = 8 and preoperative sagittal measurements N = 7.
cOne patient in the no fracture group did not have postoperative radiographs available for measurement, so N = 8 for all postoperative measurements in the dual-rod group no fracture group.
Discussion
Our objective with this retrospective cohort study was to determine if multi-rod long fusion constructs provide increased stability and fusion rates at the lumbosacral junction. Of our 31 patients, 15 underwent dual-rod fusion and 16 underwent multi-rod fusion. Several important demographic characteristics, preoperative alignment measurements, intraoperative conditions, and follow-up time were not statistically different between the 2 groups, indicating our cohorts were well matched.
We found a significantly higher incidence of lumbosacral pseudarthrosis and rod breakage in the dual-rod group compared to the multi-rod group. There was no disadvantage in using the multi-rods with respect to estimated blood loss and operative time, suggesting they provide an efficacious alternative to dual-rod constructs for long fusion to the sacrum and pelvis. Our finding of a 26% lumbosacral pseudarthrosis rate in the dual-rod group is consistent with the range reported in the literature.3,4,16,17
We hypothesized that mechanical instability caused lumbosacral pseudarthrosis and that the increased stability of multiple rods would therefore improve fusion rates. Hypertrophic nonunion in long bones indicates mechanical instability as the cause of nonunion.12,13 Findings suggestive of hypertrophic, as opposed to oligo- or atrophic, nonunion at the lumbosacral junction in all 4 of our L5-S1 pseudarthrosis cases may support that mechanical instability led to pseudarthrosis. While this is an extrapolation of long bone pathophysiology to the spine that requires future research to elucidate, a number of biomechanical studies do demonstrate the mechanical superiority of multi-rod constructs. Shen et al proposed a 4-rod long fusion technique to overcome the mechanical challenge of the lumbosacral junction and demonstrated in human cadaveric spines that the 4-rod construct significantly reduced flexibility and motion of the L5-S1 segment with regard to flexion, extension, and axial rotation when compared to the 2-rod constructs.18,19 Wang and colleagues conducted a separate cadaveric biomechanical study of 4-rod fusion constructs compared to dual-rod constructs and found greater stability and decreased range of motion at the lumbosacral junction in the 4-rod constructs.24
Despite numerous biomechanical studies, the literature is sparse regarding the clinical outcome following multi-rod fusion. Hyun et al recently revealed that multi-rod constructs were associated with fewer broken rods and pseudarthrosis after 3-column osteotomy when compared to standard dual-rod constructs.25 A previous biomechanical study examining different revision strategies for lumbar pedicle subtraction osteotomy established that additional rods increased stiffness in flexion-extension and lateral bending, supporting improved mechanical stability as the reason for the decreased pseudarthrosis and broken rods observed by Hyun’s group.26
Kim et al showed that risk factors for pseudarthrosis include sagittal imbalance ≥5 cm, age >55 years, the presence of osteoarthritis of the hip, thoracolumbar alignment kyphosis ≥20°, and incomplete sacropelvic fixation (lack of either anterior column support at L5-S1 or a lack of bilateral iliac fixation).5 Of the 34 patients out of 144 who had pseudarthrosis, 15 had pseudarthrosis at L5-S1 while the remaining 17 patients had pseudarthrosis at T10-L2 (thoracolumbar junction). The 6 patients from our study in the dual-rod group who experienced a rod fracture had similar demographic and operative characteristics to the dual-rod patients who did not experience rod fracture, but had a statistically greater pre- and postoperative coronal Cobb angle, suggesting that the severity of coronal deformity may be a risk factor for developing rod failure.
Rod material confers different mechanical properties, as cobalt chrome rods have a superior stiffness and fatigue life than titanium alloy rods, and rod fracture is more frequent in adult spinal deformity cases corrected with titanium alloy rods.27,28 All of our patients were instrumented with 5.5-mm diameter rods, and there was no statistical difference in rod material used between the 2 cohorts, supporting that rod type did not influence incidence of pseudarthrosis. Though rod material is an important consideration for surgical planning, the utilization of additional rods to improve mechanical stability must be considered when planning deformity correction. The hypertrophic nonunion detected in each of the 4 dual-rod lumbosacral pseudarthrosis affirms that mechanical instability, and not lack of physiologic bone production, was the etiology of the nonunion.29-32 This finding further articulates the importance of increasing lumbosacral stability by deploying multiple rods.
Our results, along with the aforementioned biomechanical studies, exhibit that multiple rods increase mechanical stability and promote fusion at the lumbosacral junction. When treating adult spinal deformity patients with long fusion to the sacrum, multi-rod constructs provide a safe and effective alternative to traditional dual-rod constructs.
Limitations
This study was limited by a small sample size of patients, making the study relatively underpowered despite significant findings. Perhaps an important limitation was our lack of long-term follow-up. The lower quartile of follow-up time for all of our cases was 18.9 months, and the median follow-up time was 36.2 months, both longer than the median time to rod failure of 17.72 months. In spite of this, we still lack long-term follow-up and therefore cannot extend our conclusions to the long term. Additionally, we had a heterogonous population of patients that included revision surgeries for L5-S1 pseudarthrosis. The majority of revision surgeries were in the multi-rod cohort, which may have predisposed those patients to develop pseudarthrosis more so than the primary procedures of the dual-rod group.33 Our conclusion may be strengthened by the larger number of revisions included in the multi-rod group, but this is nonetheless a limitation because the cohorts were different. We demonstrated that several preoperative and operative characteristics were not statistically different between the groups, but we could not control for certain factors such as preoperative diagnoses and indications for surgery. Last, this study examined patients of a single surgeon, and therefore a single technique. The impact of the study would improve if expanded to multiple surgeons to demonstrate the results are consistently found regardless of which practitioner implants the multiple rod constructs.
Conclusion
We observed findings suggestive of hypertrophic nonunion in all cases of lumbosacral pseudarthrosis, indicating that mechanical instability, and not patient physiology, may have caused the pseudarthrosis. Using multi-rod constructs for long fusion to the sacrum reduced rates of lumbosacral pseudarthrosis and rod fracture, demonstrating they are more effective than dual-rod constructs for treating adult spinal deformity with long fusion to the sacrum.
Footnotes
Authors’ Note: The Icahn School of Medicine at Mount Sinai Institutional Review Board approved this research.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Balderston RA, Winter RB, Moe JH, Bradford DS, Lonstein JE. Fusion to the sacrum for nonparalytic scoliosis in the adult. Spine (Phila Pa 1976). 1986;11:824–829. [DOI] [PubMed] [Google Scholar]
- 2. Kostuik JP, Hall BB. Spinal fusions to the sacrum in adults with scoliosis. Spine (Phila Pa 1976). 1983;8:489–500. [DOI] [PubMed] [Google Scholar]
- 3. Eck KR, Bridwell KH, Ungacta FF, et al. Complications and results of long adult deformity fusions down to L4, L5, and the sacrum. Spine (Phila Pa 1976). 2001;26:E182–E192. [DOI] [PubMed] [Google Scholar]
- 4. Weistroffer JK, Perra JH, Lonstein JE, et al. Complications in long fusions to the sacrum for adult scoliosis: minimum five-year analysis of fifty patients. Spine (Phila Pa 1976). 2008;33:1478–1483. [DOI] [PubMed] [Google Scholar]
- 5. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006;31:2329–2336. [DOI] [PubMed] [Google Scholar]
- 6. Han JS, Goel VK, Ahn JY, et al. Loads in the spinal structures during lifting: development of a three-dimensional comprehensive biomechanical model. Eur Spine J. 1995;4:153–168. [DOI] [PubMed] [Google Scholar]
- 7. Gagnon D, Arjmand N, Plamondon A, Shirazi-Adl A, Lariviere C. An improved multi-joint EMG-assisted optimization approach to estimate joint and muscle forces in a musculoskeletal model of the lumbar spine. J Biomech. 2011;44:1521–1529. [DOI] [PubMed] [Google Scholar]
- 8. Panjabi MM, Oxland TR, Yamamoto I, Crisco JJ. Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg Am. 1994;76:413–424. [DOI] [PubMed] [Google Scholar]
- 9. Khurelbaatar T, Kim K, Hyuk Kim Y. A cervico-thoraco-lumbar multibody dynamic model for the estimation of joint loads and muscle forces. J Biomech Eng. 2015;137:111001. [DOI] [PubMed] [Google Scholar]
- 10. Chaudhari R, Zheng X, Wu C, Mehbod AA, Transfeldt EE, Winter RB. Effect of number of fusion levels on S1 screws in long fusion construct in a calf spine model. Spine (Phila Pa 1976). 2011;36:624–629. [DOI] [PubMed] [Google Scholar]
- 11. O’Shaughnessy BA, Bridwell KH, Lenke LG, et al. Does a long-fusion “T3-sacrum” portend a worse outcome than a short-fusion “T10-sacrum” in primary surgery for adult scoliosis? Spine (Phila Pa 1976). 2012;37:884–890. [DOI] [PubMed] [Google Scholar]
- 12. Bishop JA, Palanca AA, Bellino MJ, Lowenberg DW. Assessment of compromised fracture healing. J Am Acad Orthop Surg. 2012;20:273–282. [DOI] [PubMed] [Google Scholar]
- 13. Copuroglu C, Calori GM, Giannoudis PV. Fracture non-union: who is at risk? Injury. 2013;44:1379–1382. [DOI] [PubMed] [Google Scholar]
- 14. Shen FH, Mason JR, Shimer AL, Arlet VM. Pelvic fixation for adult scoliosis. Eur Spine J. 2013;22(suppl 2):S265–S275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jain A, Hassanzadeh H, Strike SA, Menga EN, Sponseller PD, Kebaish KM. Pelvic fixation in adult and pediatric spine surgery: historical perspective, indications, and techniques: AAOS exhibit selection. J Bone Joint Surg Am. 2015;97:1521–1528. [DOI] [PubMed] [Google Scholar]
- 16. Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque-Galveston, combined iliac and sacral screws, and sacral fixation. Spine (Phila Pa 1976). 2002;27:776–786. [DOI] [PubMed] [Google Scholar]
- 17. Edwards CC, Bridwell KH, Patel A, Rinella AS, Berra A, Lenke LG. Long adult deformity fusions to L5 and the sacrum. A matched cohort analysis. Spine (Phila Pa 1976). 2004;29:1996–2005. [DOI] [PubMed] [Google Scholar]
- 18. Shen FH, Harper M, Foster WC, Marks I, Arlet V. A novel “four-rod technique” for lumbo-pelvic reconstruction: theory and technical considerations. Spine (Phila Pa 1976). 2006;31:1395–1401. [DOI] [PubMed] [Google Scholar]
- 19. Kelly BP, Shen FH, Schwab JS, Arlet V, Diangelo DJ. Biomechanical testing of a novel four-rod technique for lumbo-pelvic reconstruction. Spine (Phila Pa 1976). 2008;33:E400–E406. [DOI] [PubMed] [Google Scholar]
- 20. Shah RR, Mohammed S, Saifuddin A, Taylor BA. Comparison of plain radiographs with CT scan to evaluate interbody fusion following the use of titanium interbody cages and transpedicular instrumentation. Eur Spine J. 2003;12:378–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Panagiotis M. Classification of non-union. Injury. 2005;36:S30–S37. [DOI] [PubMed] [Google Scholar]
- 22. Bhattacharyya T, Bouchard KA, Phadke A, Meigs JB, Kassarjian A, Salamipour H. The accuracy of computed tomography for the diagnosis of tibial nonunion. J Bone Joint Surg Am. 2006;88:692–697. [DOI] [PubMed] [Google Scholar]
- 23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 24. Wang T, Liu H, Zheng Z, et al. Biomechanical effect of 4-rod technique on lumbosacral fixation: an in vitro human cadaveric investigation. Spine (Phila Pa 1976). 2013;38:E925–E929. [DOI] [PubMed] [Google Scholar]
- 25. Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine (Phila Pa 1976). 2014;39:1899–1904. [DOI] [PubMed] [Google Scholar]
- 26. Scheer JK, Tang JA, Deviren V, et al. Biomechanical analysis of revision strategies for rod fracture in pedicle subtraction osteotomy. Neurosurgery. 2011;69:164–172. [DOI] [PubMed] [Google Scholar]
- 27. Nguyen TQ, Buckley JM, Ames C, Deviren V. The fatigue life of contoured cobalt chrome posterior spinal fusion rods. Proc Inst Mech Eng H. 2011;225:194–198. [DOI] [PubMed] [Google Scholar]
- 28. Smith JS, Shaffrey CI, Ames CP, et al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery. 2012;71:862–868. [DOI] [PubMed] [Google Scholar]
- 29. Claes LE, Heigele CA, Neidlinger-Wilke C, et al. Effects of mechanical factors on the fracture healing process. Clin Orthop. 1998;(355 suppl):S132–S147. [DOI] [PubMed] [Google Scholar]
- 30. Röntgen V, Blakytny R, Matthys R, et al. Fracture healing in mice under controlled rigid and flexible conditions using an adjustable external fixator. J Orthop Res. 2010;28:1456–1462. [DOI] [PubMed] [Google Scholar]
- 31. Klein P, Schell H, Streitparth F, et al. The initial phase of fracture healing is specifically sensitive to mechanical conditions. J Orthop Res. 2003;21:662–669. [DOI] [PubMed] [Google Scholar]
- 32. Niikura T, Lee SY, Sakai Y, Nishida K, Kuroda R, Kurosaka M. Causative factors of fracture nonunion: the proportions of mechanical, biological, patient-dependent, and patient-independent factors. J Orthop Sci. 2014;19:120–124. [DOI] [PubMed] [Google Scholar]
- 33. Kelly MP, Lenke LG, Bridwell KH, Agarwal R, Godzik J, Koester L. Fate of the adult revision spinal deformity patient: a single institution experience. Spine (Phila Pa 1976). 2013;38:E1196–E1200. [DOI] [PMC free article] [PubMed] [Google Scholar]