Abstract
Study Design:
Systematic literature review and meta-analysis of studies published in English language.
Objective:
Return to play after anterior cervical discectomy and fusion (ACDF) in contact athletes remains a controversial topic with no consensus opinion in the literature. Additional information is needed to properly advise and treat this population of patients. This study is a meta-analysis assessing return to competitive contact sports after undergoing an ACDF.
Methods:
A literature search of Medline, Embase, and Cochrane Reviews was performed to identify investigations reporting return to play following ACDF in professional contact athletes. The pooled results were performed by calculating the effect size based on the logic event rate. Studies were weighted by the inverse of the variance, which included both within and between-study error. Confidence intervals (CIs) were reported at 95%. Heterogeneity was assessed using the Q statistic and I 2. Sensitivity analysis and publication bias calculations were performed.
Results:
The initial literature search resulted in 166 articles, of which 5 were determined relevant. Overall, return to play data was provided for 48 patients. The pooled clinical success rate for return to play was 73.5% (CI = 56.7%, 85.8%). The logit event rate was calculated to be 1.036 (CI = 0.270, 1.802), which was statistically significant (P = .008). The studies included in this meta-analysis demonstrated minimal heterogeneity with Q value of 4.038 and I 2 value of 0.956.
Conclusions:
Elite contact athletes return to competition 73.5% of the time after undergoing ACDF. As this is the first study to pool results from existing studies, it provides strong evidence to guide decision making and expectations in this patient population.
Keywords: anterior cervical discectomy and fusion (ACDF), return to play, contact athletes, systematic review, meta-analysis, elite athletes, cervical spine injury
Introduction
Management of cervical spine injuries associated with neurapraxia or radiculopathy in contact sport athletes represents a unique challenge for the treating surgeon. Any intervention undertaken must provide symptomatic relief while allowing for safe and effective return to play. Anterior cervical discectomy and fusion (ACDF) is a proven and effective treatment with a high clinical success rate when treating for cervical radiculopathy in the general population.1-5 ACDF allows for removal of the offending lesion while providing indirect and direct decompression of the nerve root through foraminal distraction. Subsequent fusion helps stabilize the spine providing relief from symptoms related to associated cervical spondylosis.
While ACDF is regarded as the gold standard for the treatment of cervical spondylosis, less is known regarding the utility and role of ACDF in the treatment of conditions of the cervical spine in contact sport athletes. The biomechanical demands placed on the cervical spine are vastly greater in contact sport athletes when compared with the general population.6-9 Thus, special consideration must be taken into account in determining treatment options for cervical radiculopathy in contact sport athletes.
Recently, a number of studies have looked at the rate of return to play after ACDF in contact sport athletes in an attempt to determine the effectiveness of ACDF as a treatment of neck pain or cervical radiculopathy in contact sport athletes.10-15 While these studies have provided some guidance on the ability to return to play after ACDF, most of the data is from small retrospective case series.
To date, there remains no consensus in the literature to guide the treating physician in advising the elite contact athlete on return to play after ACDF. The purpose of this article is to perform a systematic review and meta-analysis to describe the likelihood of return to contact sports after ACDF.
Materials and Methods
Inclusion and Exclusion Criteria and Review Procedure
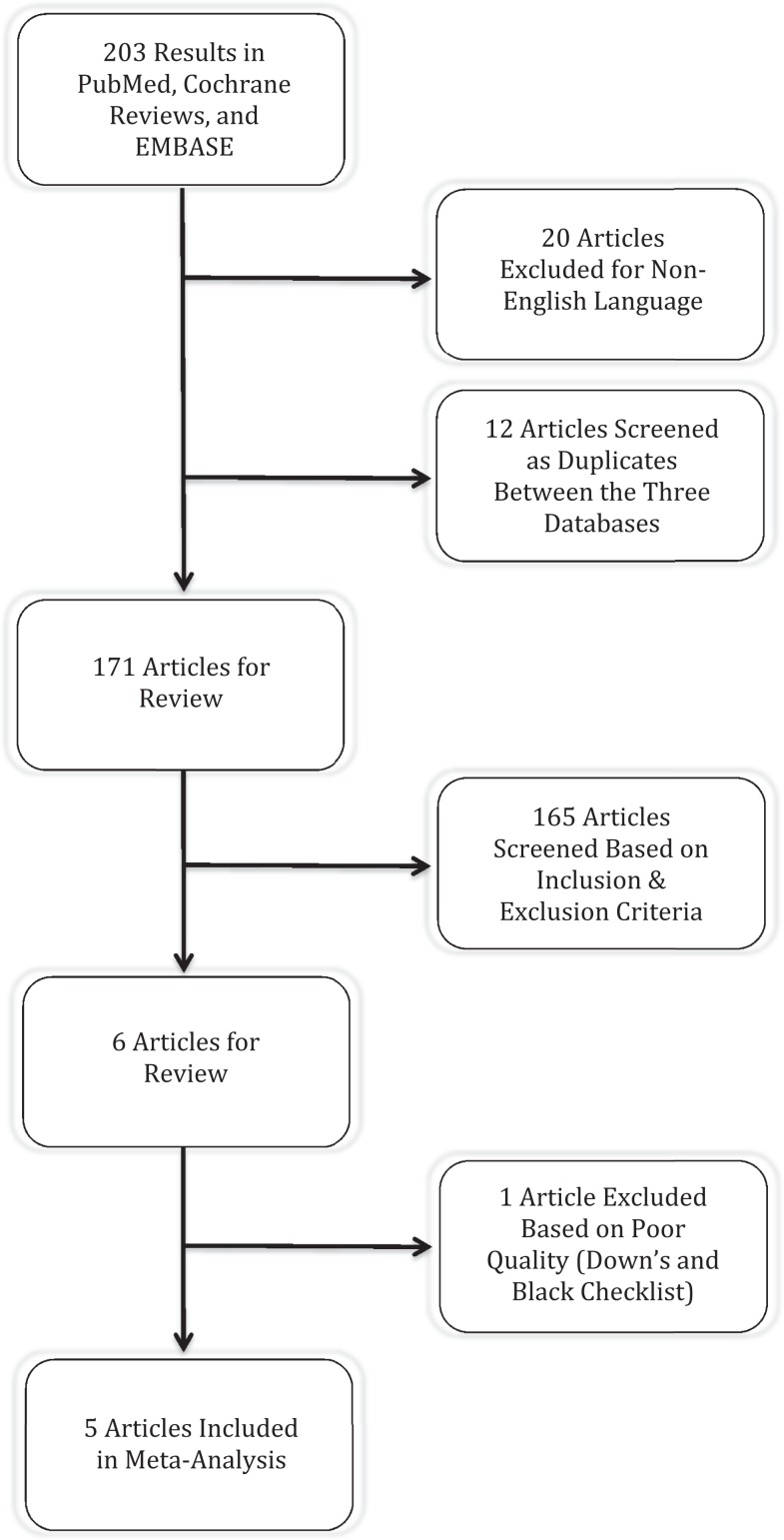
A systematic computerized literature search was performed using PubMed, Cochrane Database of Systematic Reviews, and EMBASE. The electronic databases were search from January 1990 to December 2014. Searches were performed from Medical Subject Headings (MeSH) used by the National Library of Medicine. Specifically, MeSH terms “anterior cervical discectomy and fusion,” “ACDF,” “athlete,” and “sport” were used. A full description of the search strings can be found in the appendix as well as a flow diagram of the systematic review. Inclusion criteria for the meta-analysis included adult, subaxial spine, operative treatment with ACDF, minimum of 6 months follow-up, and reported ability to return to play.
The abstracts for each article were reviewed by 2 independent authors to assess for inclusion in the meta-analysis. The authors jointly reviewed the full text of the articles meeting the inclusion criteria for the study. A third author was available in the event of a discrepancy between the 2 reviewers, and a consensus was reached after review. The methodological quality of each study was appraised in accordance with the Oxford Levels of Evidence 2.
Data Extraction
A database was created from the included studies with the following categories: (1) study ID to include author, journal, and year of publication; (2) reference; (3) study type and level of evidence; (4) number of patients; (5) sport played; (6) patient age; (7) length of follow-up; (8) operative levels; (9) surgical indication; (10) duration from surgery to return to play; And (11) clinical success. The primary outcomes variable was ability to return to play. This was calculated as a binary variable whereby return to play was success, and inability to return to play was failure.
Methodological Quality Assessment
Methodological quality assessment was accomplished using the Downs and Black checklist. It is a checklist that culminates in a total score that is directly proportional with the quality of the study. The total cumulative score is composed of a profile that measures quality of reporting, internal validity (bias and confounding), and external validity. According to Downs and Black,16 the performance results of the checklist showed a high internal consistency (KR-20 = 0.89), test-retest (r = 0.88), and interrater (r = 0.75) reliability.
The checklist consists of 27 items for which an answer “yes” correlates with a score of 1 and an answer “no” correlates with a score of 0. Notably, we used a modified Downs and Black checklist in which item 27 was shifted to a binary answer system. One point was award if a power or sample size calculation was present. This method produces a maximum score of 28.
Meta-Analysis
Pooling of the results was performed by calculating the effect size based on the logit event rate using Comprehensive Meta Analysis, version 2.2.050 (Biostat, Englewood, NJ).
We computed prevalence point estimates using the formula Logit Event Rate = Log[Event Rate/(1 − Event Rate)]. The event rate or prevalence is represented as the effect size of the meta-analysis. The studies were weighted in the meta-analysis by the inverse of the variance, which included both with and between study errors. The effect size and confidence intervals (CIs) were reported using a Forest plot. Confidence intervals were reported at a 95% level. A P value of .05 was set for significance. Heterogeneity was assessed using the Q statistic and I 2, where I 2 is the estimate of the percentage of error due to between-study variation. I 2 values below 25% generally indicate consistent results and homogeneous studies. A priori we selected a random effects model.
A sensitivity analysis was performed by varying the assumptions used in the meta-analysis, and also through single elimination of the studies to assess for significance. The Ebber test was used to assess for publication bias among the studies.
Results
Systematic Review
The initial PubMed, Cochrane Review, and EMBASE search resulted in 166 articles. After 2-reviewer assessment, 6 articles were identified that met all of the inclusion criteria.10-15 One study was excluded as the methodology of the article relied on an analysis of team injury reports and newspaper archives, and not on the direct treatment of players.12
The 5 studies that were selected for inclusion were all retrospective case series. Descriptive information for each study is provided in Table 1. Overall, return to play data was provided for 48 patients: 18 football players, 19 rugby players, 8 wrestlers, and 1 basketball player. The average age of the player at the time of surgery was 28.8 years. The most commonly operated levels were C3/4 and C5/6 with 10 operative levels each. There were 5 operative levels at C4/5, 9 operative levels at C6/7, and 2 operative levels at C7/T1. Four studies reported on the time required from surgery until return to play; the average was 7.29 months. There were no catastrophic events reported in any of the case series after return to play.
Table 1.
Summary Information of the Studies Included in the Meta-Analysis for Return to Play After Anterior Cervical Discectomy and Fusion.
| Study | Level of Evidence | Sport | No. of Patients | Age (Years) | Procedure | Graft/Hardware | Return to Play | Time to Return to Play | Confirmation of Fusion | Length of Return to Play |
|---|---|---|---|---|---|---|---|---|---|---|
| Meredith, 2013 | IV | Football | 3 | 27 | ACDF: C3/4 (1), 1 C4/5 (1), C5/6 (1) | Unspecified | 1/3 | Next season | Unspecified | Unspecified |
| Maroon, 2013 | IV | A: Football | A: 7 | A: 31.3 | ACDF: C3/4 (4), 1 C4/5 (1), C5/6 (8), C6/7 (2) | Unspecified | A: 5/7 | 5.46 months | Radiographic confirmation with flexion/extension X-rays | 1 to 3 years |
| B: Wrestling | B: 8 | B: 29.0 | B: 8/8 | |||||||
| Brigham, 2013 | IV | A: Football | A: 3 | A: 27 | ACDF: C3/4 (4), C5/6 (1) | Instrumented fusion, graft unspecified | A: 2/3 | 5 months; following season | CT at 1 year; unspecified; MRI; CT at 6 months | >3 years; 2 years; 1/2 season then reinjury; >2 years |
| B: Basketball | B: 1 | B: — | B: 0/1 | following season; 6 months | ||||||
| Maroon, 2007 | IV | Football | 5 | 27.2 | ACDF: C3/4 (1), 1 C4/5 (3), C6/7 (1) | Allograft bone and instrumented fusion | 5/5 | 1 (8 weeks), 4 (5-8 months) | Unspecified | 3 years; 3 years; 27 games; 7 games; 2 years |
| Andrews, 2008 | IV | Rugby | 19 | — | ACDF: Levels unspecified | Titanium or PEEK cages, instrumented fusion | 13/19 | 9/13 at 6 months; 1 at 12 months; 3 unspecified | Unspecified | Unspecified |
Abbreviations: ACDF, anterior cervical discectomy and fusion; CT, computed tomography; MRI, magnetic resonance imaging.
Summary of Investigations
Meredith et al15 reported a retrospective case series of a single NFL football team from 2000 to 2011. The authors included all athletes with magnetic resonance imaging (MRI) proven disc herniation with appropriately concordant symptoms. A total of 16 athletes met inclusion criteria. Linemen, linebackers, and defensive backs were the most represented positions (13/16 athletes; 81%). The most common presentation was radiculopathy after a single traumatic event (9/16 athletes; 56%). Three players had transient paresis. Three players underwent 1-level anterior cervical discectomy and fusion. These 3 players had failed nonoperative therapy and had evidence of spinal cord compression with signal change on MRI, but only one returned to sport.
Maroon et al14 published a retrospective case series of 15 professional athletes (7 football; 8 wrestlers) who had undergone a 1-level ACDF by a single neurosurgeon from 2003 to 2012. Seven of the 15 athletes presented with neurapraxia, 8 with cervical radiculopathy, and 2 with hyperintensity of the spinal cord. Cervical stenosis with effacement of the cerebrospinal fluid signal was noted in 14 subjects. The operative level included C3-4 (4 patients), C4-5 (1 patient), C5-6 (8 patients), and at C6-7 (2 patients). All athletes were cleared for return to play after a neurological examination with normal findings, and radiographic criteria for early fusion were confirmed. Thirteen of the 15 players returned to their sport between 2 and 12 months postoperatively (mean = 6 months), with 8 still participating. The return to play duration of the 5 who retired after full participation ranged from 1 to 3 years. All athletes remain asymptomatic for radicular or myelopathic symptoms or signs. Two football players were cleared from a neurologic standpoint but chose not to return to play.
Brigham et al13 presented a retrospective case series of 3 professional football players and 1 professional basketball player. All athletes had documented cervical cord contusions. None of the athletes had an acute disc herniation, fracture, instability, or focal cord compression. The first patient was a 27-year-old NFL safety who sustained a hyperextension injury to his neck. The player underwent a C3/4 ACDF and returned to play 5 months after surgery. The second patient was a professional basketball player with a history of multiple cervical contusions. In the first 6 months after being drafted into the National Basketball Association, he presented with his third episode of a cervical cord neuropraxia. He underwent an anterior fusion at the C3-C4 level and was kept out of competition for the remainder of the year. He returned and played for several more years. The third player was a 27-year-old NFL offensive lineman presenting with a brief episode of neck and shoulder pain. His cervical MR image demonstrated a contusion at the C5-C6 level. At the end of the season he underwent an anterior fusion at the C5-C6 level. The patient was able to return to play the following season, but ultimately developed a contusion at C3/4. The patient subsequently underwent an ACDF at C3/4 and has not returned to play. The fourth player is a 27-year-old defensive tackle who developed bilateral finger tingling after a face-to-face tackle. MRI reviled a cord contusion at C3/4. He subsequently underwent a C3/4 ACDF and was able to return to play at 6 months.
Andrews et al11 examined the outcome of 19 professional rugby union players who underwent anterior cervical discectomy and fusion between 1998 and 2003. Their mean age at operation was 28 years (range = 22-37). Radicular pain was eradicated in 15 patients, improved in 2 and patients, and 2 patients had no change. Neck pain was eradicated in 8 patients, improved in 9 patients, and 2 patients had no change. A total of 13 players returned to their previous level of rugby. One returned to professional rugby but played in a lower division. Nine of the 13 returned to rugby at 6 months after operation (range = 5-17). Only one player took more than 12 months to return to playing.
Maroon et al17 reported on 5 elite football players who were evaluated after experiencing episodes of neurapraxia. All patients experienced bilateral paresthesias—3 in all 4 extremities and 2 in the upper extremities—lasting a few minutes to more than 24 hours. Transient motor deficits occurred in 2 individuals but caused no permanent sequelae. After aggressive rehabilitation and confirmation of fusion ranging from 9 weeks to 8 months postoperatively, the players were allowed to return to active play. Two of the players developed recurrent career-ending disc herniations, one above and the other below the fusion level. One player required repeated spinal cord decompression.
Quality Assessment of Included Studies
The quality index score of our studies was a 9, as all of the included studies were retrospective case series. We defined a higher quality study as 16 to 18, a moderate quality study as 13 to 15, and a poorer quality study as 8 to 12.
Meta-Analysis Results
Clinical Results
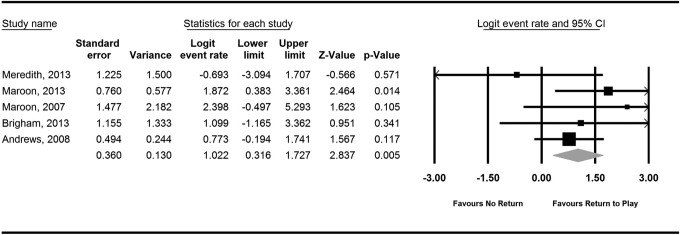
Clinical results were reported in 5 studies. The pooled success rate for returning to play after ACDF was 73.5% (CI = 56.7%, 85.8%) (Table 2). The logit event rate was calculated to be 1.022 (CI = 0.316, 1.827). A Forest plot of the logit event rates demonstrated favorable outcomes with respect to returning to play after ACDF (Figure 1). This pooled logit event rate was found to be statistically in favor of returning to professional contact sports after ACDF (P = .005).
Table 2.
Results of the Random Effects Model With the Return to Play Event Rate and Confidence Interval.
| Study | Event Rate | Lower Limit | Upper Limit | Z Value | P Value |
|---|---|---|---|---|---|
| Meredith, 2013 | 0.333 | 0.043 | 0.846 | −0.566 | .571 |
| Maroon, 2013 | 0.867 | 0.595 | 0.966 | 2.464 | .014 |
| Brigham, 2013 | 0.917 | 0.378 | 0.995 | 1.623 | .105 |
| Maroon, 2007 | 0.750 | 0.238 | 0.966 | 0.951 | .341 |
| Andrews, 2008 | 0.684 | 0.452 | 0.851 | 1.567 | .117 |
| 0.738 | 0.567 | 0.858 | 2.652 | .008 |
Figure 1.
Forest plot of the logit event rate for return to play after anterior cervical discectomy and fusion.
The studies included in this meta-analysis demonstrated minimal heterogeneity with Q value of 4.038 and I 2 value of 0.956 (Table 3).
Table 3.
Results of the Random Effects Model for Study Heterogeneity.
| Model | Number of Studies | Effect size and 95% Confidence Interval | Heterogeneity | ||||
|---|---|---|---|---|---|---|---|
| Point estimate | Variance | Lower limit | Upper limit | Q Value | I 2 | ||
| Random effects | 5 | 1.036 | 0.153 | 0.270 | 1.802 | 4.039 | 0.956 |
Sensitivity Analysis and Publication Bias
Single elimination of each study did not impact the overall results of the analysis. Single removal of each study resulted in P < .05, which validates the results of the model.
The Egger test for bias was performed to assess for publication bias within the studies. A value of 1.68 (95% CI = −1.32, 4.69) was found (P = .1721).
Discussion
ACDF is a frequently utilized procedure for the treatment of acute cervical disc herniation that is refractory to conservative management. Long accepted as the gold standard for the treatment of neurological deficits, neck pain, and radiculopathy associated with cervical disc herniations, ACDF is generally associated with a high clinical success rate in the general population. However, the demands of elite athletes in contact sports such as football or rugby represent a unique challenge for clinicians in the management of these patients. There is little evidence in the literature and no consensus opinion regarding the likelihood of returning to a professional contact sport after undergoing an ACDF.
Meta-analyses allow for the pooling of data from studies of similar design to determine if there is a significant effect. Furthermore, if there is a significant effect, pooling of the data allows for a determination of the magnitude of the intended effect. Our study utilized a random effects model. We selected a random effects model a priori, due to an expected level of heterogeneity among the studies included in the analysis. When dealing with heterogeneity among studies, we are left with several options: not to pool the data and perform a systematic review; ignore heterogeneity and use a fixed effects model; explore the heterogeneity; and allow for heterogeneity and use a random effects model. In a random effects model, we assume that the effect is not the same in all of the studies. The studies therefore represent a sample of possible studies where the effect varies. When allowing for heterogeneity in a random effects model, we get a less powerful analysis than a fixed effects mode because the P values are larger and the confidence intervals are wider.
Heterogeneity is prevalent, particularly in retrospective case series, as there is considerable variation in the methodology employed and surgical techniques used both within and between the studies in the analysis. In our study, the 5 studies included demonstrated minimal heterogeneity with an I 2 < 1. As defined by Higgins and Thompson,18 the calculation of study heterogeneity with the use of I 2 is a validated method that allows for a direct comparison between meta-analyses with different numbers of studies and different types of outcome data. Higgins and Thompson defined low, moderate, and high to I 2 values of 25%, 50%, and 75%, respectively. Higgins and Thompson, in an analysis of 509 meta-analyses found in the Cochrane Database of Systematic Reviews, found that over one quarter of all meta-analyses have I 2 values over 50%. The presence of heterogeneity, according to Higgins and Thompson, does not invalidate the results or the utilization of data pooling. In our study, with the I 2 < 1, the results reported likely represent the true effect.
The results of our meta-analysis indicate that in elite contact athletes who have undergone an ACDF for disc herniation or cord contusion, they are more likely to return to competition at the same level than retire. Meredith et al,15 in the smallest series of athletes in this analysis, found that only 1 patient out of 3 returned to competition. This rate of return is contradicted with the results found by Maroon and Brigham,13,14 who both showed greater than 70% return to play. In a recent study by Hsu,12 38 of 53 (72%) players successfully returned to play for 29 games over a 2.8-year period. which was significantly greater than that of the nonoperative group, in which only 21 of 46 (46%) players successfully returned to the field to play after treatment for 15 games over a 1.5-year period (P < .04). The rate of return reported by Hsu for professional football players is consistent with the rate of 73.5% found in the pooled results of this study.
Limitations are inherent with all meta-analyses, including the heterogeneity of the included studies, the possibility of missed studies within our search, and unknown biases within the primary studies. A random effects model was selected to control for some of the inherent heterogeneity among the studies; however, there was variability in the operative methods among the studies. Surgical technique, graft choices, postoperative protocol, and return to play criteria all varied both within and between the studies. For instance, Maroon et al14 reported using fibular allograft, whereas the other authors do not describe the graft type.
Another potential limitation of this meta-analysis is the use of studies of inferior quality (level IV case series) as part of our analysis. This particular area remains underrepresented in the literature. While we rely on small retrospective case series for the pooling of our data, this represents a significant increase in the reliability of information that has been predominantly anecdotal or based on single small series. Overall, there are 48 patients included in our study. This represents the largest aggregate of outcomes data in elite athletes undergoing ACDF. Hsu12 was able to report on 53 NFL players who underwent ACDF over 29 years; however, the data was collected from news articles and published injury reports. The author notes that this is a significant limitation as reporting errors, misdiagnosis, and selection bias are inherently prevalent. Furthermore, because of the source of the information, reporting errors are likely given the potential impact on game preparation and strategy.
Our study represents the first report of pooled outcomes following ACDF in elite contact athletes. The results indicate that in this patient population, there is a 73.5% likelihood of returning to the same level of competition following surgery. As this is the first study to pool results from existing studies, it provides strong evidence to guide decision making and the determination of appropriate expectations in this patient population. Given the relatively small number of patients in our study, an emphasis on the prospective collection of data in this population is needed moving forward.
Appendix
((("neck"[MeSH Terms] OR "neck"[All Fields] OR "cervical"[All Fields]) AND disc[All Fields] AND ("hernia"[MeSH Terms] OR "hernia"[All Fields] OR "herniation"[All Fields])) OR (("neck"[MeSH Terms] OR "neck"[All Fields] OR "cervical"[All Fields]) AND ("spine"[MeSH Terms] OR "spine"[All Fields]) AND ("surgery"[Subheading] OR "surgery"[All Fields] OR "surgical procedures, operative"[MeSH Terms] OR ("surgical"[All Fields] AND "procedures"[All Fields] AND "operative"[All Fields]) OR "operative surgical procedures"[All Fields] OR "surgery"[All Fields] OR "general surgery"[MeSH Terms] OR ("general"[All Fields] AND "surgery"[All Fields]) OR "general surgery"[All Fields])) OR (anterior[All Fields] AND ("neck"[MeSH Terms] OR "neck"[All Fields] OR "cervical"[All Fields]) AND spinal[All Fields] AND ("surgery"[Subheading] OR "surgery"[All Fields] OR "surgical procedures, operative"[MeSH Terms] OR ("surgical"[All Fields] AND "procedures"[All Fields] AND "operative"[All Fields]) OR "operative surgical procedures"[All Fields] OR "surgery"[All Fields] OR "general surgery"[MeSH Terms] OR ("general"[All Fields] AND "surgery"[All Fields]) OR "general surgery"[All Fields])) OR (anterior[All Fields] AND ("neck"[MeSH Terms] OR "neck"[All Fields] OR "cervical"[All Fields]) AND ("diskectomy"[MeSH Terms] OR "diskectomy"[All Fields] OR "discectomy"[All Fields]) AND ("Nucl Eng Des/Fusion"[Journal] OR "fusion"[All Fields] OR "FUSION"[Journal] OR "fusion"[All Fields]))) AND (("athletes"[MeSH Terms] OR "athletes"[All Fields] OR "athlete"[All Fields]) OR return-to-play[All Fields] OR ("football"[MeSH Terms] OR "football"[All Fields]) OR ("football"[MeSH Terms] OR "football"[All Fields] OR "rugby"[All Fields]) OR ("martial arts"[MeSH Terms] OR ("martial"[All Fields] AND "arts"[All Fields]) OR "martial arts"[All Fields]) OR ("boxing"[MeSH Terms] OR "boxing"[All Fields]) OR ("wrestling"[MeSH Terms] OR "wrestling"[All Fields]) OR ("racquet sports"[MeSH Terms] OR ("racquet"[All Fields] AND "sports"[All Fields]) OR "racquet sports"[All Fields] OR "lacrosse"[All Fields]) OR ("hockey"[MeSH Terms] OR "hockey"[All Fields]) OR polo[All Fields] OR (("Contact"[Journal] OR "contact"[All Fields] OR "Contact"[Journal] OR "contact"[All Fields]) AND ("sports"[MeSH Terms] OR "sports"[All Fields] OR "sport"[All Fields])))
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Cloward RB. The anterior approach for removal of ruptured cervical disks. J Neurosurg. 1958;15:602–617. [DOI] [PubMed] [Google Scholar]
- 2. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958;40-A:607–624. [PubMed] [Google Scholar]
- 3. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993;75:1298–1307. [DOI] [PubMed] [Google Scholar]
- 4. Emery SE, Bolesta MJ, Banks MA, Jones PK. Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine (Phila Pa 1976). 1994;19:660–663. [PubMed] [Google Scholar]
- 5. Carette S, Fehlings MG. Clinical practice. Cervical radiculopathy. N Engl J Med. 2005;353:392–399. [DOI] [PubMed] [Google Scholar]
- 6. Thomas BE, McCullen GM, Yuan HA. Cervical spine injuries in football players. J Am Acad Orthop Surg. 1999;7:338–347. [DOI] [PubMed] [Google Scholar]
- 7. Morganti C, Sweeney CA, Albanese SA, Burak C, Hosea T, Connolly PJ. Return to play after cervical spine injury. Spine (Phila Pa 1976). 2001;26:1131–1136. [DOI] [PubMed] [Google Scholar]
- 8. Torg JS, Guille JT, Jaffe S. Injuries to the cervical spine in American football players. J Bone Joint Surg Am. 2002;84-A(1):112–122. [DOI] [PubMed] [Google Scholar]
- 9. Rihn JA, Anderson DT, Lamb K, et al. Cervical spine injuries in American football. Sports Med. 2009;39:697–708. [DOI] [PubMed] [Google Scholar]
- 10. Maroon JC, El-Kadi H, Abla AA, et al. Cervical neurapraxia in elite athletes: evaluation and surgical treatment. Report of five cases. J Neurosurg Spine. 2007;6:356–363. [DOI] [PubMed] [Google Scholar]
- 11. Andrews J, Jones A, Davies PR, Howes J, Ahuja S. Is return to professional rugby union likely after anterior cervical spinal surgery? J Bone Joint Surg Br. 2008;90:619–621. [DOI] [PubMed] [Google Scholar]
- 12. Hsu WK. Outcomes following nonoperative and operative treatment for cervical disc herniations in National Football League athletes. Spine (Phila Pa 1976). 2011;36:800–805. [DOI] [PubMed] [Google Scholar]
- 13. Brigham CD, Capo J. Cervical spinal cord contusion in professional athletes: a case series with implications for return to play. Spine (Phila Pa 1976). 2013;38:315–323. [DOI] [PubMed] [Google Scholar]
- 14. Maroon JC, Bost JW, Petraglia AL, et al. Outcomes after anterior cervical discectomy and fusion in professional athletes. Neurosurgery. 2013;73:103–112. [DOI] [PubMed] [Google Scholar]
- 15. Meredith DS, Jones KJ, Barnes R, Rodeo SA, Cammisa FP, Warren RF. Operative and nonoperative treatment of cervical disc herniation in National Football League athletes. Am J Sports Med. 2013;41:2054–2058. [DOI] [PubMed] [Google Scholar]
- 16. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Maroon JC, Gardner P, Abla AA, El-Kadi H, Bost J. “Golfer’s stroke”: golf-induced stroke from vertebral artery dissection. Surg Neurol. 2007;67:163–168. [DOI] [PubMed] [Google Scholar]
- 18. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. [DOI] [PubMed] [Google Scholar]