Abstract
Objectives
This study was designed to quantify the relationship between the absence of heart failure risk factors in middle age and incident heart failure, heart failure-free survival, and overall survival.
Background
Quantification of years lived free from heart failure in the context of risk factor burden in mid-life may improve risk communication and prevention efforts.
Methods
We conducted a pooled, individual-level analysis sampling from communities across the United States as part of 4 cohort studies: the Framingham Heart, Framingham Offspring, Chicago Heart Association Detection Project in Industry, and ARIC (Atherosclerosis Risk In Communities) studies. Participants with and without hypertension (blood pressure ≥140/90 mm Hg or treatment), obesity (body mass index ≥30 kg/m2), or diabetes (fasting glucose ≥126 mg/dl or treatment), and combinations of these factors, at index ages of 45 years and 55 years through 95 years. Competing risk-adjusted Cox models, a modified Kaplan-Meier estimator, and Irwin’s restricted mean were used to estimate the association between the absence of risk factors at mid-life and incident heart failure, heart failure-free survival, and overall survival.
Results
For participants at age 45 years, over 516,537 person-years of follow-up, 1,677 incident heart failure events occurred. Men and women with no risk factors, compared to those with all 3, had 73% to 85% lower risks of incident heart failure. Men and women without hypertension, obesity, or diabetes at age 45 years lived on average 34.7 years and 38.0 years without incident heart failure, and they lived on average an additional 3 years to 15 years longer free of heart failure than those with 1, 2, or 3 risk factors. Similar trends were seen when stratified by race and at index age 55 years.
Conclusions
Prevention of hypertension, obesity, and diabetes by ages 45 years and 55 years may substantially prolong heart failure-free survival, decrease heart failure-related morbidity, and reduce the public health impact of heart failure.
Keywords: epidemiology, heart failure, prevention, risk factors
Graphical abstract
Introduction
Heart failure is a common, highly morbid, and costly condition with a growing impact on public health. The lifetime risk for heart failure ranges from 20% to 45% depending on sex and race (1). In America, the prevalence of heart failure among adults is approximately 5.7 million (2). Overall, heart failure patients have significantly lower quality of life than matched controls in a normal population and high mortality rates (2,3). The total estimated annual cost is $30.7 billion, and these costs are expected to increase nearly 127% over the next 20 years (2). Thus, efforts to prevent this highly prevalent, morbid, and costly disease are needed to reduce its substantial public health burden.
Recently, there has been a shift from focusing on disease risk to cardiovascular health promotion and preservation of ideal cardiovascular health (2,4). Instead of quantifying risk in terms of the relationship between a risk factor and increased chance of cardiovascular disease (CVD), estimating how the absence of risk factors translates into years lived free from CVD and prolonged longevity may be beneficial (5,6). Quantification of healthy survival free from specific CVD endpoints, such as heart failure, may enhance risk assessment and communication, promote public health policy to prevent heart failure, and provide insight into the mechanistic underpinnings of incident heart failure.
Risk factors for incident heart failure and lifetime heart failure risk have been described in numerous studies and include hypertension (HTN), obesity, diabetes mellitus (DM), male sex, metabolic syndrome, and atherosclerotic disease (1,2,7–10). Several studies have shown how lower risk factor burden during middle age is associated with better outcomes, including higher quality of life, less disability, lower CVD rates, higher cognitive abilities, and increased survival (4,6,11–13). HTN, obesity, and DM are highly prevalent and potentially preventable risk factors for heart failure. The absence of these 3 risk factors are key components of ideal cardiovascular health (4). However, to our knowledge, no study has quantified the relationship between the avoidance of HTN, obesity, and DM by mid-life and years lived free from heart failure across the remaining lifespan. Therefore, we sought to quantify the associations between prevalent HTN, obesity, and DM in mid-life and incident heart failure risk, years lived free from heart failure, overall survival, and percentage of life lived with heart failure in a large, contemporary epidemiological sample.
Methods
Sample
The methods for the selection and pooling of cohorts and the sample sizes in the Cardiovascular Disease Lifetime Risk Pooling Project (LRPP) have been previously described (14). Briefly, the LRPP is an individual-pooled dataset of 20 US-based community epidemiological cohorts with socio-demographics, CVD risk factors, and CVD outcomes. Individual participant data from the following 4 cohorts were sampled: Framingham Heart Study, Framingham Offspring Study, ARIC (Atherosclerosis Risk In Communities) study, and the Chicago Heart Association (CHA) Detection Project in Industry Study (15–18). Public-released datasets were used for all the cohorts except CHA, which was an internal set. This project was exempted from review by the institutional review board at Northwestern University.
The Framingham Heart Study enrolled white men and women, ages 30 years to 62 years, in 1948 from Framingham, Massachusetts. The Framingham Offspring Study enrolled white men and women, ages 5 to 70 years, in 1971 from Framingham, Massachusetts. Follow-up data through 2008 were included for both cohorts. The ARIC study enrolled white and black men and women, ages 45 to 64 years, from 1987 to 1989 from 4 sites (Forsyth County, North Carolina; Jackson, Mississippi; Minneapolis, Minnesota; and Washington County, Maryland). Follow-up data through 2007 were included. The CHA enrolled white and black men and women >18 years of age, in 1967 to 1973, from Chicago, Illinois. Follow-up data were included through 2008.
Ascertainment of baseline values, follow-up values, and outcomes
The methods for ascertaining baseline values, follow-up values, incident heart failure, and vital status have been described elsewhere (1,8,14,19). Participants self-report determined race. HTN was defined as blood pressure ≥140 mm Hg systolic or ≥90 mm Hg diastolic or treatment. Obesity was defined as a body mass index ≥30 kg/m2. Diabetes was defined as a fasting glucose ≥126 mg/dl or treatment. Additional details are included in the Online Appendix. Briefly, baseline and follow-up values were obtained during in-person examinations. In the Framingham, Framingham Offspring, and ARIC studies, potential heart failure events were identified via multiple mechanisms and then adjudicated by a central committee. Medicare primary discharge diagnosis coding was used to identify heart failure events in the CHA study. The incidence rates for heart failure for CHA participants after age 65 years were similar to those in the other cohorts. Methods for mortality ascertainment included contact with family and employers and matching to Social Security Administration files, the National Death Index, and National Death Index-Plus service. Mortality ascertainment for all 4 cohorts has been essentially complete.
Statistical analysis
Participants were grouped by sex and the 3 risk factors of interest—HTN, obesity, and DM—obtained at study examination within 5 years of index ages 45 years and 55 years. We categorized participants into those with and without HTN, obesity, or DM, and combinations of these factors, at index ages of 45 years and 55 years.
Cohort-specific analyses were performed as previously described by our group (11) to assess for differences in incident heart failure risk due to differences in sampling, geography, calendar year of inception, size, follow-up, and definition of outcome. Risk estimates for each risk factor group were overall similar across cohorts; therefore, data were pooled.
Competing risk of death Cox incidence models and hazard ratios for incident heart failure stratified by sex and race (black and non-Hispanic white) were created using the Lunn-McNeil method and Fine and Gray method (20,21). Competing risk of death models count deaths before incident heart failure as a separate event, not a withdrawal, which reduces overestimation of risk (22,23). These models were adjusted for age, education, and smoking status. Models stratified by sex were adjusted for race, and models stratified by race were adjusted for sex. Models stratified by participants with a single risk factor for heart failure were adjusted for the other 2 risk factors of interest. For example, the model for men at index age 45 years with HTN was adjusted for obesity and DM. We generated curves for cumulative hazard and hazard ratios. We performed interaction testing for sex and individual risk factors in pooled race-stratified models and race and individual risk factors in pooled sex-stratified models.
To calculate heart failure–free survival and overall survival for index ages 45 years and 55 years, we first used a modified Kaplan Meier analysis accounting for competing risks of death. Rates of incident heart failure and death were summed for participants up to age 95 years, or to the oldest age. We then used the Irwin’s restricted mean, which is similar to measuring the area under the survival curve, to calculate years lived free from heart failure and overall survival (6,24). Percentage of life lived with heart failure was calculated by dividing mean survival after incident heart failure by mean overall survival. Two-sided z-tests were used to assess for differences in heart failure–free survival and overall survival by risk factor status (HTN/no HTN, DM/no DM, obesity/no obesity, 3 risk factors/0 risk factors) for each stratum. To account for multiple comparisons, we used the Bonferroni correction. A p value of 0.00078 was considered to be statistically significant. All calculations were performed using SAS statistical software (version 9.1, SAS Institute, Cary, North Carolina).
Results
Participant risk factor burden is shown in Table 1. At index ages 45 years and 55 years, respectively, 53.2% and 43.7% of participants were free of HTN, obesity, and DM. Overall, 0.98% of participants had all 3 risk factors at age 45 years, and 2.6% had all 3 at age 55 years. Black participants at ages 45 years and 55 years had overall higher prevalence of individual and multiple risk factors. For example, at age 45 years, 36.1% of blacks did not have HTN, obesity, or DM; whereas 55.0% of whites were free of all 3 risks factors. Four percent of the black participants had all 3 risk factors at age 45 years, whereas 0.7% of white participants at age 45 years had all 3 risk factors.
Table 1.
Study Sample Characteristics and Distribution of Risk Factor Burden
| Men | Women | White | Black | |
|---|---|---|---|---|
| Age 45 yrs | ||||
| Number of participants | 9,719 | 9,530 | 17,392 | 1,857 |
| Person-yrs of follow-up | 256,193 | 260,344 | 474,765 | 41,772 |
| No risk factors | 4,545 (46.8) | 5,695 (59.8) | 9,570 (55.0) | 670 (36.1) |
| HTN | 4,367 (44.9) | 3,015 (31.6) | 6,466 (37.2) | 916 (49.3) |
| Obesity | 1,873 (19.3) | 1,579 (16.6) | 2,842 (16.3) | 610 (32.9) |
| DM | 357 (3.7) | 302 (3.2) | 472 (2.7) | 187 (10.1) |
| 1 risk factor | 3,835 (39.5) | 2,878 (30.2) | 5,978 (34.4) | 735 (40.0) |
| 2 risk factors | 1,255 (12.9) | 853 (9.0) | 1,730 (10.0) | 378 (20.4) |
| 3 risk factors | 84 (0.9) | 104 (1.1) | 114 (0.7) | 74 (4.0) |
| Total incident heart failure events | 894 (9.2) | 783 (8.2) | 1,485 (8.5) | 192 (10.3) |
| Total deaths | 3,930 (40.4) | 2,910 (30.5) | 6,326 (36.4) | 514 (27.7) |
| Age 55 yrs | ||||
| Number of participants | 11,124 | 12,791 | 21,042 | 2,873 |
| Person-yrs of follow-up | 223,727 | 278,525 | 452,791 | 49,461 |
| No risk factors | 4,630 (41.6) | 5,817 (45.5) | 9,748 (46.3) | 699 (24.3) |
| HTN | 5,244 (47.1) | 5,614 (43.9) | 9,151 (43.5) | 1,707 (59.4) |
| Obesity | 2,439 (21.9) | 3,042 (23.8) | 4,278 (20.3) | 1,203 (41.9) |
| DM | 859 (7.7) | 933 (7.3) | 1,230 (5.9) | 562 (19.6) |
| 1 risk factor | 4,668 (42.0) | 4,748 (37.1) | 8,278 (39.3) | 1,138 (39.6) |
| 2 risk factors | 1,604 (14.4) | 1,837 (14.4) | 2,667 (12.7) | 774 (26.9) |
| 3 risk factors | 222 (2.0) | 389 (3.0) | 349 (1.7) | 262 (9.1) |
| Total incident heart failure events | 1,416 (12.7) | 1,560 (12.2) | 2,512 (11.9) | 464 (16.2) |
| Total deaths | 5,895 (53.0) | 5,165 (40.4) | 10,047 (47.8) | 1,013 (35.3) |
Values are n or n (%).
DM = diabetes mellitus; HTN = hypertension.
From the 4 cohorts, 19,249 participants at age 45 years and 23,915 participants at age 55 years were included in this analysis (Table 1). Women comprised 49.5% and 53.5% of the sample at ages 45 years and 55 years, respectively. Black participants comprised 9.6% and 12.0% of the sample at ages 45 years and 55 years, respectively.
After the index age of 45 years, during 516,537 person-years of follow-up, 1,677 cases of incident heart failure were identified. At an index age of 55 years, during 502,252 person-years of follow-up, 2,976 cases of incident heart failure were identified. The median length of follow-up was 27.1 years and 20.3 years for participants at index ages 45 years and 55 years, respectively.
Risks for incident heart failure
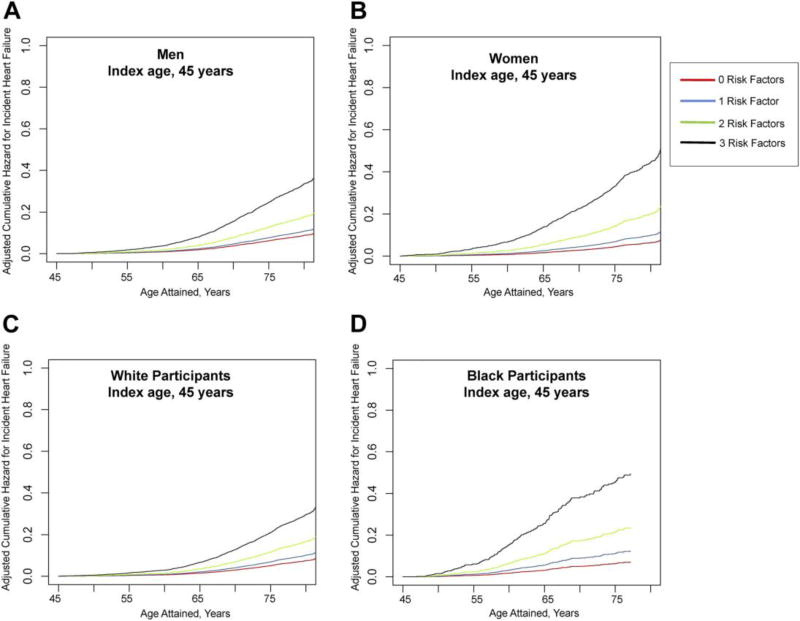
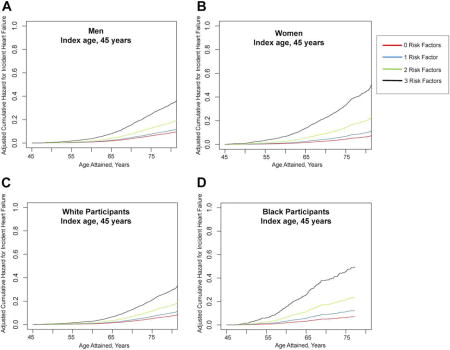
Figure 1 shows competing risk of death adjusted cumulative hazard curves for incident heart failure stratified by sex and race at age 45 years. There is a graded increase in risk for incident heart failure with increasing risk factor burden for both men and women with notable divergence with aging. The trends were similar when stratified by race.
Figure 1. Cumulative Hazard for Incident Heart Failure for Index Age 45 Years.
Display of the adjusted cumulative hazard for incident heart failure at index age 45 years by risk factor burden for men (A), women (B), white participants (C), and black participants (D).
The absence of HTN is associated with lower risk for incident heart failure in all strata except for men at index age 45 years (Online Table 1). Lower aggregate risk factor burden is consistently associated with lower risk for heart failure. At index age 45 years, for participants without HTN, obesity, and DM compared to those with all 3 risk factors, the risk of heart failure was substantially lower for men (hazard ratio [HR]: 0.27; 95% confidence interval [CI]: 0.16 to 0.44), for women (HR: 0.15; 95% CI: 0.10 to 0.22), for white participants (HR: 0.24; 95% CI: 0.16 to 0.38), and for black participants (HR = 0.12; 95% CI: 0.07 to 0.20). These trends for the cumulative hazard curves and HR are similar at index age of 55 years (Supplemental Figure 1, Supplemental Table 1). Significant interactions between race and DM, race and HTN, and sex and obesity were noted among some subgroups, but not consistently.
Years lived free from heart failure, overall survival, and percentage of life lived with heart failure
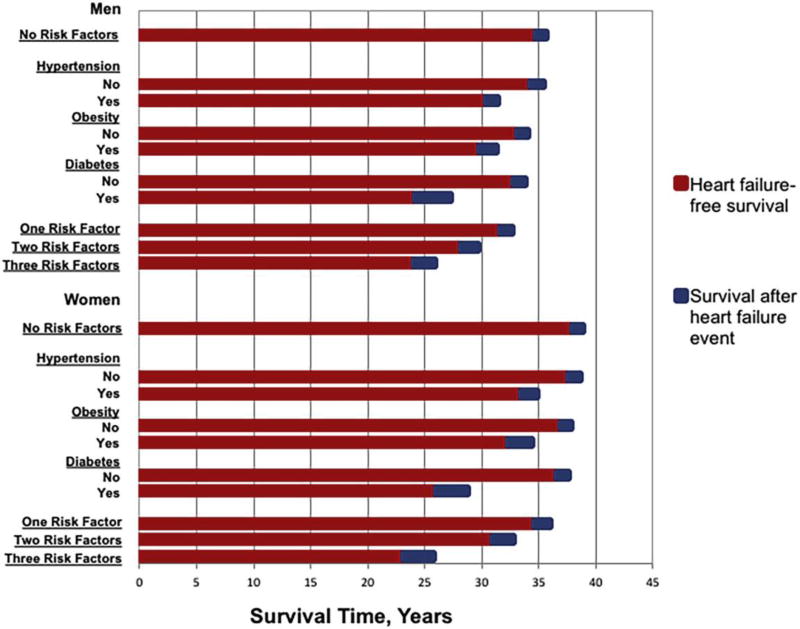
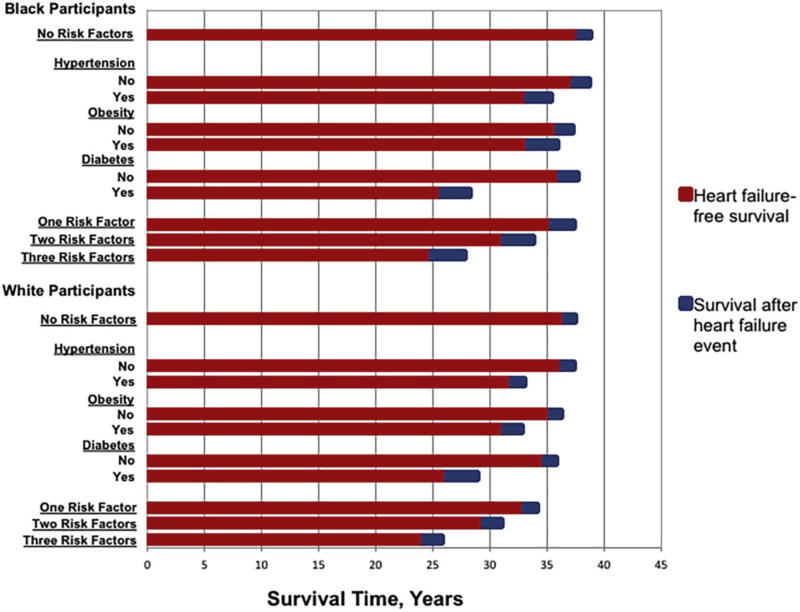
Across all strata for index age 45 years, the absence of HTN, obesity, or DM was associated with substantially longer heart failure–free survival (Figures 2 and 3). Diabetes appears to have the strongest association with shorter heart failure–free survival. At age 45 years, compared to those with DM, men and women without DM lived on average 8.6 years and 10.6 years longer without heart failure, respectively. At an index age of 45 years, black and white participants without DM lived an average 10.3 years and 8.6 years longer free from heart failure than those with DM, respectively. For each risk factor across the various sex, race, and age strata, differences in heart failure–free survival and overall survival were statistically significant (p < 0.00078) except for heart failure–free survival and overall survival for black participants with and without obesity at ages 45 years and 55 years and for black participants with and without HTN at age 45 years, for which estimates were in the same direction but not significant.
Figure 2. Heart Failure–Free Survival and Survival After Incident Heart Failure by Sex.
Display of heart failure–free survival, survival after heart failure event, and overall survival by risk factors (hypertension, obesity, and diabetes) for men and women at index age 45 years.
Figure 3. Heart Failure-Free Survival and Survival After Incident Heart Failure by Race.
Display of heart failure–free survival, survival after heart failure event, and overall survival by risk factors (hypertension, obesity, and diabetes) for black participants and white participants at index age 45 years.
Men at age 45 years without any of the 3 risk factors lived an average 10.6 years longer free of heart failure than those with all 3 risk factors. Women at age 45 years without any of the 3 risk factors lived an average 14.9 years longer free of heart failure than those with all 3 risk factors. White and black participants without HTN, obesity, or DM, compared to those with all 3 risk factors, had heart failure–free survival times that were 12.4 years and 12.9 years longer, respectively.
Similar trends were seen across the different strata for index age 55 years (Supplemental Figures 2 and 3). Differences in heart failure–free survival and overall survival were statistically significant between those without any of the 3 risk factors compared to those with all 3 risk factors (p < 0.00078). For the individual values of heart failure–free survival rates for each strata, see Supplemental Table 2.
Individuals without risk factors on average had longer overall survival and lower percentage of life lived with heart failure in most groups (Table 2, Supplemental Tables 3 to 5). The longer overall survival and lower percentage of life lived with heart failure were most pronounced when comparing participants with HTN, obesity, and DM to those without all 3 risk factors. For example, at index age 45 years, men with all 3 risk factors at age 45 years on average lived for 25.8 years and lived 6.9% of their life with heart failure. In contrast, men with no risk factors lived on average an additional 9.8 years and lived 2.7% of their lives with heart failure, suggesting a compression of heart failure–related morbidity.
Table 2.
Survival After Incident Heart Failure, Overall Survival, and Percentage of Life Lived With Heart Failure at Age 45 Stratified by Sex
| Men, Index Age 45 yrs | Women, Index Age 45 yrs | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Survival Time After Incident Heart Failure, yrs |
Overall Survival Time, yrs |
Percentage of Life Lived With Heart Failure |
Survival Time After Incident Heart Failure, yrs |
Overall Survival Time, yrs |
Percentage of Life Lived With Heart Failure |
|
| No HTN | 1.08 ± 0.08 | 35.4 ± 0.22 | 3.1 | 0.98 ± 0.07 | 38.5 ± 0.20 | 2.5 |
| HTN | 1.05 ± 0.10 | 31.4 ± 0.28 | 3.3 | 1.35 ± 0.14 | 34.8 ± 0.33 | 3.9 |
| No obesity | 0.98 ± 0.06 | 34.1 ± 0.19 | 2.9 | 0.90 ± 0.06 | 37.8 ± 0.18 | 2.4 |
| Obesity | 1.50 ± 0.15 | 31.3 ± 0.38 | 4.8 | 2.06 ± 0.24 | 34.4 ± 0.49 | 6.0 |
| No DM | 1.03 ± 0.06 | 33.8 ± 0.17 | 3.0 | 1.05 ± 0.06 | 37.6 ± 0.17 | 2.8 |
| DM | 3.12 ± 0.56 | 27.3 ± 0.79 | 11.4 | 2.79 ± 0.74 | 28.8 ± 1.00 | 9.7 |
| No risk factors | 0.96 ± 0.08 | 35.6 ± 0.24 | 2.7 | 0.82 ± 0.07 | 38.8 ± 0.20 | 2.1 |
| 1 risk factor | 1.06 ± 0.12 | 32.7 ± 0.30 | 3.2 | 1.37 ± 0.14 | 35.9 ± 0.33 | 3.8 |
| 2 risk factors | 1.49 ± 0.19 | 29.7 ± 0.45 | 5.0 | 1.82 ± 0.32 | 32.8 ± 0.64 | 5.5 |
| 3 risk factors | 1.77 ± 0.57 | 25.8 ± 2.01 | 6.9 | 2.64 ± 1.28 | 25.8 ± 1.87 | 10.2 |
Values are mean ± SE or %.
SE = standard error; other abbreviations as in Table 1.
Discussion
In this large, representative sample, we found that the absence of HTN, DM, and obesity at ages 45 years and 55 years is associated with 73% to 86% lower risks for incident heart failure over the remaining life course compared to those with all 3 risk factors. Furthermore, the absence of all 3 of these risk factors by age 45 years, compared to those with all 3 risk factors, is associated on average with >10 years of longer heart failure–free survival and up to 13 years longer overall survival. The observed trends were similar across race and sex groups. On average, the absence of all 3 individual risk factors at ages 45 years and 55 years appears to be associated with a smaller percentage of life lived with heart failure in the context of overall longer survival and suggestive of substantial compression of heart failure–related morbidity.
Pathophysiological mechanisms for the relationship of each of these risk factors and incident heart failure have been described (25–27). Numerous epidemiological investigations have illustrated the relationship between HTN, DM, and obesity and increased risk for incident heart failure, including in cohorts used in this analysis (1,8,10,13,26,28–36). Thus, although it is not surprising that the avoidance of these heart failure risk factors is associated with lower risk for incident heart failure, the magnitude of the associations observed are particularly impressive. This study adds to the understanding of how individual and aggregate risk factor levels specifically in middle age affect incident heart failure risk over the remaining lifespan. This is also the first study to quantify heart failure–free survival time associated with the avoidance of all these risk factors by mid-life. These findings are consistent with prior work illustrating the particularly high risk of heart failure associated with the presence of DM (36,37). In our study, men and women without DM at age 45 years compared to those with DM are, respectively, 62% and 60% less likely to develop heart failure in the adjusted model. It was surprising to see that avoidance of HTN by mid-life did not have a significant association with incident heart failure in men at age 45 years; however, we suspect the effect of HTN may be been attenuated by antihypertensive medication use. This effect would be consistent with SPRINT (Systolic Blood Pressure Intervention Trial), a randomized controlled trial that showed aggressive blood pressure treatment substantially reduced heart failure risks in patients with HTN (38).
Thinking about risk differently, we show how the absence of these factors at ages 45 years and 55 years, compared to those with HTN, obesity, and DM, significantly decreases risk for incident heart failure and substantially increases heart failure–free survival and overall survival. These data help reframe the heart failure prevention discussion by quantifying how primordial prevention—the prevention of the development of 3 heart failure risk factors—can lengthen healthy and overall survival and could vastly reduce the population burden of heart failure.
Lower risk factor burden in middle age has been shown to be associated with lower lifetime risks for atherosclerotic CVD, CVD death, and incident heart failure (11,13,33,39,40). Wilkins et al.(6) quantified the lifetime risk and years lived free from total CVD—defined as atherosclerotic CVD, hemorrhagic stroke, and heart failure—by the aggregate risk factor burden in middle age. Lower risk factor burden was consistently associated with longer total CVD-free survival. Our study adds to these findings by examining a heart failure–specific endpoint and examining the association between individual risk factors and incident heart failure. Our analysis also is more tailored to major risk factors for heart failure by including obesity and excluding total cholesterol and tobacco use (Table 3).
Table 3.
Summary of Study Design and Key Findings
| Prior key findings from relevant Cardiovascular Disease Lifetime Risk Pooling Project studies |
|
| Study objectives |
|
| Cohorts sampled from Cardiovascular Disease Lifetime Risk Pooling Project |
|
| Key findings |
|
The concept of compression of morbidity was first posited by Fries in 1980 (41). The theory states that ideal healthy behaviors lead to overall longer survival with shortened period of chronic illness at the end of life, and some epidemiological investigations have supported this theory (5). In our study, the absence of HTN, obesity, and DM, compared to those with all 3 risk factors, was associated with a shorter percentage of life lived with heart failure in the context of overall longer survival. These findings suggest that the primordial prevention of HTN, obesity, and DM are associated with the relative and absolute compression of heart failure–related morbidity across the remaining life course. Understanding how to maximize years of disease-free living and minimize the years of life burdened with chronic disease, lower quality of life, and higher costs may be important patient-centered outcomes relevant to policy makers, clinicians, and patients. Our study highlights the importance of preventing the development of HTN and other heart failure risk factors to prolong heart failure–free survival.
Compared to whites, blacks have higher heart failure prevalence rates, lower average age of incidence, and higher rates of morbidity and mortality (42). These disparities are thought to be multifactorial, including due to differences in risk factor prevalence, neurohormonal imbalance, endothelial dysfunction, genetic polymorphisms, and socioeconomic status (42). However, using a competing risk model, Huffman et al. (1)found the lifetime risk of heart failure was similar between black and white women and lower in black men than white men, likely due to other competing causes of death, such as chronic kidney disease, HIV, and traumatic deaths in blacks. In our analyses stratified by race, the prevalence of HTN, obesity, and DM was higher in blacks than in whites. The overall trends in risk of incident heart failure, years lived free from heart failure, and percentage of life lived with heart failure were similar. However, the differences in the average percentage of life lived with heart failure between black and white participants with all 3 risk factors at index age 45 years (10.5% vs. 6.3%) and age 55 years (22.1% vs. 12.8%) are particularly striking. The benefits of risk factor avoidance and primordial prevention were consistent and substantial in black and white participants. These data suggest that a public health strategy focused on primordial prevention of risk factors in blacks early on the life course may reduce disparities in heart failure incidence and prevalence.
Study limitations
First, some of the cohorts differed in their definitions of incident heart failure, which could affect the accuracy of the estimates reported. However, data from individual cohorts were examined before pooling, and the associations between HTN, obesity, and DM and incident heart failure risk were strikingly similar across cohorts. Moreover, using hospital discharge data for follow-up is clinically relevant and has been previously shown to be reliable and valid (43). Second, the different enrollment and follow-up periods of the cohorts could lead to birth cohort effects. However, although the prevalence of risk factors over time may vary, previous analyses from the LRPP have shown remarkably consistent associations between risk factors and CVD endpoints (11). Third, our data do not account for the change in risk factors before or after index ages 45 years or 55 years or the development or change in risk factors after mid-life. Certainly, some individuals prior to mid-life had risk factors but through lifestyle changes did not have them by the index ages, and many individuals without risk factors at 45 years developed HTN, obesity, or DM across their remaining life course. Inclusion of both these types of participants in the no risk factors groups would likely bias our findings toward the null, if anything.
Several strengths of this study include the large and well-phenotyped sample, broad geographical, community-based representation, in-person measurement of baseline characteristics, nearly complete vital status follow-up, and adjudicated outcome assessments.
Conclusions
These data suggest that the absence of HTN, obesity, and DM by ages 45 years and 55 years is associated with up to 86% lower risks for incident heart failure in men and women across the remaining life course. The avoidance of HTN, obesity, and DM by ages 45 years and 55 years may substantially prolong heart failure–free survival and reduce heart failure–related morbidity. These data underscore the importance of preventing the development of risk factors in mid-life for decreasing the public health impact of heart failure. Lastly, quantification of heart failure–free survival may be a novel, useful tool for risk communication to patients for the purposes of promoting cardiovascular health.
Supplementary Material
Perspectives.
COMPETENCY IN MEDICAL KNOWLEDGE
Patients without hypertension, obesity, and diabetes by mid-life have substantially lower risk for developing heart failure, more years lived free from heart failure, and reduced heart failure-related morbidity.
TRANSLATIONAL OUTLOOK 1
Preventing the development of risk factors for heart failure may be an effective strategy to reduce to the public health burden of heart failure.
TRANSLATIONAL OUTLOOK 2
Novel measures of risk, such as years lived free from heart failure, may be a useful tool for communicating risk or for informing public health strategies.
Acknowledgments
The authors thank the investigators of all the cohort studies included in this analysis for their hard work and dedication in collecting the underlying data, and especially the study participants, whose dedication and commitment have formed the basis of profound observations regarding health and disease that have contributed to improved health, longevity, and quality of life for millions of persons.
The Cardiovascular Disease Lifetime Risk Pooling has been supported by R21 HL085375 from the National Heart, Lung, and Blood Institute (NHLBI) and by institutional funds from Northwestern University Feinberg School of Medicine. This study was conducted with the use of limited-access datasets obtained by the NHLBI and does not necessarily reflect the opinions or views of the study investigators or the NHLBI. The ARIC study, Framingham Heart study, and the Framingham Offspring study are conducted and supported by the NHLBI in collaboration with the study investigators. Dr. Ahmad is supported by the NHLBI of the National Institutes of Health under Award number T32HL069771 and by a 2015 Research Fellowship Award from the Heart Failure Society of America. Dr. Rich has received honoraria from Otsuka from the speaker’s bureau. Dr. Wilkins is in part supported by NIH Loan Repayment Program.
Abbreviations and Acronyms
- BMI
body mass index
- CI
confidence interval
- CVD
cardiovascular disease
- DM
diabetes
- HR
hazard ratio
- HTN
hypertension
Footnotes
All other authors have reported that they have no relationships relevant to the contents of this paper to disclose
References
- 1.Huffman MD, Berry JD, Ning H, et al. Lifetime risk for heart failure among white and black Americans: cardiovascular lifetime risk pooling project. J Am Coll Cardiol. 2013;61:1510–1517. doi: 10.1016/j.jacc.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2016 Update: A report from the American Heart Association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- 3.Lesman-Leegte, Jaarsma T, Coyne JC, Hillege HL, Van Veldhuisen DJ, Sanderman R. Quality of life and depressive symptoms in the elderly: a comparison between patients with heart failure and age- and gender-matched community controls. J Cardiac Fail. 2009;15:17–23. doi: 10.1016/j.cardfail.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 4.Lloyd-Jones DM, Hong Y, Labarthe D, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 5.Fries JF, Bruce B, Chakravarty E. Compression of morbidity 1980–2011: a focused review of paradigms and progress. J Aging Res. 2011;2011:1–10. doi: 10.4061/2011/261702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilkins JT, Ning H, Berry J, Zhao L, Dyer AR, Lloyd-Jones DM. Lifetime risk and years lived free of total cardiovascular disease. JAMA. 2012;308:1795–1801. doi: 10.1001/jama.2012.14312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2010;8:30–41. doi: 10.1038/nrcardio.2010.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lloyd-Jones DM, Larson MG, Leip EP, et al. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002;106:3068–3072. doi: 10.1161/01.cir.0000039105.49749.6f. [DOI] [PubMed] [Google Scholar]
- 9.Bleumink GS, Knetsch AM, Sturkenboom MCJM, et al. Quantifying the heart failure epidemic: prevalence, incidence rate, lifetime risk and prognosis of heart failure The Rotterdam Study. Eur Heart J. 2004;25:1614–1619. doi: 10.1016/j.ehj.2004.06.038. [DOI] [PubMed] [Google Scholar]
- 10.Lee DS, Massaro JM, Wang TJ, et al. Antecedent blood pressure, body mass index, and the risk of incident heart failure in later life. Hypertension. 2007;50:869–876. doi: 10.1161/HYPERTENSIONAHA.107.095380. [DOI] [PubMed] [Google Scholar]
- 11.Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–329. doi: 10.1056/NEJMoa1012848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shah AM, Claggett B, Folsom AR, et al. Ideal cardiovascular health during adult life and cardiovascular structure and function among the elderly. Circulation. 2015;132:1979–1989. doi: 10.1161/CIRCULATIONAHA.115.017882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Folsom AR, Yamagishi K, Hozawa A, Chambless LE. Atherosclerosis risk in communities study investigators. Absolute and attributable risks of heart failure incidence in relation to optimal risk factors. Circ Heart Fail. 2009;2:11–17. doi: 10.1161/CIRCHEARTFAILURE.108.794933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilkins JT, Karmali KN, Huffman MD, et al. Data resource profile: the Cardiovascular Disease Lifetime Risk Pooling Project. Int J Epidemiol. 2015;44:1557–1564. doi: 10.1093/ije/dyv150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dawber TR, Kannel WB, Lyell LP. An approach to longitudinal studies in a community: the Framingham Study. Ann N Y Acad Sci. 1963;107:539–556. doi: 10.1111/j.1749-6632.1963.tb13299.x. [DOI] [PubMed] [Google Scholar]
- 16.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979;110:281–290. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 17.The ARIC Investigators. The Atherosclerosis Risk in Community (ARIC) study: design and objectives. Am J Epidemiol. 1989;129:687–702. [PubMed] [Google Scholar]
- 18.Stamler J, Dyer AR, Shekelle RB, Neaton J, Stamler R. Relationship of baseline major risk factors to coronary and all-cause mortality, and to longevity: findings from long-term follow-up of Chicago cohorts. Cardiology. 1993;82:191–222. doi: 10.1159/000175868. [DOI] [PubMed] [Google Scholar]
- 19.Kannel WB, D’Agostino RB, Silbershatz H, Belanger AJ, Wilson PWF, Levy D. Profile for estimating risk of heart failure. Arch Intern Med. 1999;159:1197–1204. doi: 10.1001/archinte.159.11.1197. [DOI] [PubMed] [Google Scholar]
- 20.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509. [Google Scholar]
- 21.Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;51:524–532. [PubMed] [Google Scholar]
- 22.Lloyd-Jones DM, Larson MG, Beiser A, Levy D. Lifetime risk of developing coronary heart disease. Lancet. 1999;353:89–92. doi: 10.1016/S0140-6736(98)10279-9. [DOI] [PubMed] [Google Scholar]
- 23.Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016;133:601–609. doi: 10.1161/CIRCULATIONAHA.115.017719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Irwin JO. The standard error of an estimate of expectation of life, with special reference to expectation of tumourless life in experiments with mice. J Hygiene. 1949;47:188. doi: 10.1017/s0022172400014443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Drazner MH. The progression of hypertensive heart disease. Circulation. 2011;123:327–334. doi: 10.1161/CIRCULATIONAHA.108.845792. [DOI] [PubMed] [Google Scholar]
- 26.Kenchaiah S, Gaziano JM, Vasan RS. Impact of obesity on the risk of heart failure and survival after the onset of heart failure. Med Clin North Am. 2004;88:1273–1294. doi: 10.1016/j.mcna.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 27.Taegtmeyer H. Adaptation and maladaptation of the heart in diabetes: part I: general concepts. Circulation. 2002;105:1727–1733. doi: 10.1161/01.cir.0000012466.50373.e8. [DOI] [PubMed] [Google Scholar]
- 28.Levy D, Larson MG, Vasan RS, Kannel WB, Ho KK. The progression from hypertension to congestive heart failure. JAMA. 1996;275:1557–1562. [PubMed] [Google Scholar]
- 29.Wilhelmsen L, Rosengren A, Eriksson H, Lappas G. Heart failure in the general population of men—morbidity, risk factors and prognosis. J Intern Med. 2001;249:253–261. doi: 10.1046/j.1365-2796.2001.00801.x. [DOI] [PubMed] [Google Scholar]
- 30.Lee DS, Gona P, Vasan RS, et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the Framingham Heart Study of the National Heart, Lung, and Blood Institute. Circulation. 2009;119:3070–3077. doi: 10.1161/CIRCULATIONAHA.108.815944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bibbins-Domingo K, Pletcher MJ, Lin F, et al. Racial differences in incident heart failure among young adults. N Engl J Med. 2009;360:1179–1190. doi: 10.1056/NEJMoa0807265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bahrami H, Bluemke DA, Kronmal R, et al. Novel metabolic risk factors for incident heart failure and their relationship with obesity: the MESA (Multi-Ethnic Study of Atherosclerosis) study. J Am Coll Cardiol. 2008;51:1775–1783. doi: 10.1016/j.jacc.2007.12.048. [DOI] [PubMed] [Google Scholar]
- 33.Djoussé L, Driver JA, Gaziano JM. Relation between modifiable lifestyle factors and lifetime risk of heart failure. JAMA. 2009;302:394–400. doi: 10.1001/jama.2009.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gottdiener JS, Arnold AM, Aurigemma GP, et al. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol. 2000;35:1628–1637. doi: 10.1016/s0735-1097(00)00582-9. [DOI] [PubMed] [Google Scholar]
- 35.Dunlay SM, Weston SA, Jacobsen SJ, Roger VL. Risk factors for heart failure: a population-based case-control study. Am J Med. 2009;122:1023–1028. doi: 10.1016/j.amjmed.2009.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Avery CL, Loehr LR, Baggett C, et al. The population burden of heart failure attributable to modifiable risk factors: the ARIC (Atherosclerosis Risk in Communities) study. J Am Coll Cardiol. 2012;60:1640–1646. doi: 10.1016/j.jacc.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bibbins-Domingo K. Predictors of heart failure among women with coronary disease. Circulation. 2004;110:1424–1430. doi: 10.1161/01.CIR.0000141726.01302.83. [DOI] [PubMed] [Google Scholar]
- 38.S.P.R.I.N.T. The Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lloyd-Jones DM, Leip EP, Larson MG, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 40.Nayor M, Enserro DM, Vasan RS, Xanthakis V. Cardiovascular health status and incidence of heart failure in the Framingham Offspring Study. Circ Heart Fail. 2016;9:e002416. doi: 10.1161/CIRCHEARTFAILURE.115.002416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 42.Sharma, Colvin-Adams M, Yancy CW. Heart failure in African Americans: disparities can be overcome. Cleve Clin J Med. 2014;81:301–311. doi: 10.3949/ccjm.81a.13045. [DOI] [PubMed] [Google Scholar]
- 43.Lee DS, Donovan L, Austin PC, et al. Comparison of coding of heart failure and comorbidities in administrative and clinical data for use in outcomes research. Med Care. 2005;43:182–188. doi: 10.1097/00005650-200502000-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.