Abstract
The variability of symptoms and the fact that they are not easily recognized in imaging studies make the diagnosis and treatment of posterior meniscal roots lesions a challenging task to the orthopedist. In recent years, a more precise understanding of the anatomy and biomechanical impair of the knee joint in these cases has enabled great advances in therapeutic approaches. Well-documented studies have shown that the repair of these lesions presents superior functional and clinical improvement when compared with meniscectomy. However, the progression of degenerative joint changes in the long-term still exhibits conflicting results.
Keywords: Knee injuries; Knee/anatomy & histology; Joint instability; Surgical procedures, operative; Menisci
Resumo
A variabilidade da sintomatologia e o fato de não serem facilmente reconhecidas nos exames de imagem tornam o diagnóstico e o tratamento das lesões das raízes posteriores dos meniscos tarefas desafiadoras para o ortopedista. Nos últimos anos, uma compreensão mais precisa da anatomia e do comprometimento biomecânico da articulação do joelho nessas lesões têm possibilitado grandes avanços nas abordagens terapêuticas. Estudos bem documentados demonstram que o reparo dessas lesões oferece uma melhoria clínica e funcional superior à meniscectomia. Entretanto, os resultados da progressão das alterações degenerativas articulares em longo prazo ainda são conflitantes.
Palavras-chave: Traumatismos do joelho, Joelho/anatomia & histologia, Instabilidade articular, Procedimentos cirúrgicos operatórios, Meniscos
Introduction
In the past, lesions of the meniscal roots were underdiagnosed and often unrecognized, but now they are better understood and have been biomechanically proven to be a source of overload in the knee joint.1, 2, 3, 4, 5, 6 They are possibly related to early-onset osteoarthritis.1, 7, 8, 9 The first description of a meniscal root lesion in the literature was made by Pagnani et al.,10 who in 1991 described the process of extrusion of the medial meniscus in a football player. Historically, this type of lesion was treated by partial or total meniscectomy, which, despite its good short-term subjective results, presented a higher risk of long-term joint degeneration.11
The menisci play important roles in the knee; their integrity is essential for the proper functioning of the joint.1, 12, 13 In addition to sharing the loads and reducing the joint contact pressure by increasing the contact surface between the femur and tibia,12 other functions assigned to the menisci are proprioception,14 stabilization,15 lubrication,16 and nutrition of the joint cartilage.17 The meniscal roots are essential for maintaining the meniscal ability to convert axial loads into circumferential tension.1, 5 Biomechanical studies show that lesions in these structures are comparable to a complete meniscectomy.1
As lesions of the posterior root of the meniscus are the most frequently reported in the literature,18, 19 this study aimed to provide the surgeon with a comprehensive review of this important condition in order to facilitate its understanding, diagnosis, and treatment.
Anatomy and composition
Knowledge of the anatomy of meniscal roots is important not only to allow a precise repair in cases of injury, but also to prevent iatrogenic damage during procedures close to their location, such as reconstruction of the anterior cruciate ligament (ACL) or intramedullary tibial nailing. Meniscal roots are defined as the insertion of the meniscal horns into the tibial plateau, and extend to a distance of 0.9 mm from the attachment site.20 Respecting some characteristics, the roots of the meniscus are basically formed by a dense fiber core, surrounded by additional fibers.1, 21, 22 Histologically, meniscal roots have a structure similar to a typical enthesis, comprised of four zones: meniscus fibers, non-calcified fibrocartilage, fibrocartilage, and calcified bone.23
In addition to the qualitative anatomy, it is important that the surgeon is familiar with the quantitative descriptions of relevant surgical landmarks when performing arthroscopic procedures.
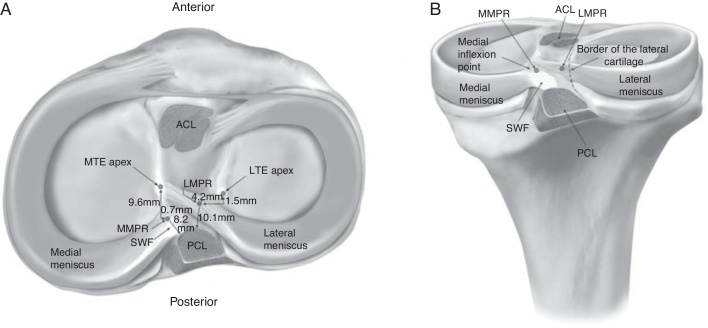
Medial meniscus posterior root (MMPR)
The additional fibers of the MMPR were first described by Anderson et al.24 as shiny white fibers (SWF). These fibers increase the attachment area of the medial meniscus to the posterior portion of the plateau. In a quantitative study, Johannsen et al.22 demonstrated that the area of the denser MMPR fiber insertion was on average 30.4 mm2, corresponding to a 6-mm diameter tunnel to reproduce its native attachment area. When SWFs were included in the measurement, the insertion area increased to 77.7 mm2. In the same study, the authors determined the distances from the center of the MMPR to the main arthroscopic frames. The MMPR was located 9.6 mm posterior and 0.7 mm lateral to the apex of the medial tibial eminence (the most reproducible landmark); 3.5 mm lateral to the inflection point of the medial tibial plateau articular cartilage; and 8.2 mm anterior to the most superior tibial attachment of the posterior cruciate ligament (PCL; Fig. 1).
Fig. 1.
Superior (A) and posterior (B) views of the posterior meniscal roots, evidencing their insertions and anatomical relationships.
LTE, lateral tibial eminence; MTE, medial tibial eminence; SWF, shiny white fibers located in the posterior horn of the medial meniscus; ACL, anterior cruciate ligament insertion; PCL, posterior cruciate ligament insertion; LMPR, lateral meniscus posterior root insertion; MMPR, medial meniscus posterior root insertion. Reprinted with the permission of Johannsen et al.22
Lateral meniscus posterior root (LMPR)
The attachment area of the main fibers of the LMPR measures 39.2 mm2, corresponding to a 7-mm diameter tunnel to reproduce its original attachment area.22 This area does not include the additional fibers, which extend to the lateral edge of the medial tibial eminence. Some authors have reported an LMPR area of 115 mm2.25 This discrepancy in measurement may be related to the inclusion of the additional fibers as part of the root. Johannsen et al.22 demonstrated that the center of LMPR is located 4.2 mm medial and 1.5 mm posterior to the lateral tibial eminence; 4.3 mm medial to articular cartilage margin of the lateral tibial plateau; 12.7 mm anterior to the superior aspect of the PCL tibial insertion; 10.1 mm posterior to the posteromedial corner of the anterior root attachment of the lateral meniscus; and 10.8 mm posterior to the posteromedial ACL band.22
An important consideration regarding the LMPR anatomy is the presence of the meniscofemoral ligaments (MFLs), which attach the LMPR to the medial femoral condyle.26 These ligaments play an important role in stabilizing the lateral meniscus and preventing or reducing extrusion in cases of injury to this root.26
Biomechanics
Approximately 50–70% of the load transmitted through the knee is supported by the medial and lateral menisci, respectively.12 The menisci are able to convert axial load into circumferential (hoop) stress; they aid in a uniform weight distribution to the joint, increasing the contact surface and reducing the peak pressure in the compartment.1 This is possible because the meniscus roots act as anchors for the meniscal horns, allowing them to resist the tendency toward extrusion generated by the axial force.1, 5
Damage to this complex may compromise its function.1, 2, 3, 4, 5, 6 Biomechanically, it has been shown that MMPR lesions reduce the contact surface and increases the peak pressure of the ipsilateral knee compartment, due to loss of circumferential (hoop) stress caused by the tear of the fibers. The biomechanical effect of this injury is similar to that of a knee undergoing total meniscectomy.1 Therefore, the integrity of the meniscal roots is of paramount importance to preserve the knee kinematics of the joint and prevent degenerative changes.1, 7, 8, 9
The menisci also play a role in knee stability, especially in the context of a ligament tear, where they have increased importance as a secondary restraint.27 Allaire et al.1 demonstrated that MMPR injury resulted in increased external rotation and lateral translation of the tibia. LMPR injuries have less repercussion on joint stability, possibly because the lateral meniscus has twice the mobility of the medial meniscus.2, 5, 25
The posterior horns of both menisci are more susceptible to injury than the anterior horns. This can be explained by the fact that they bear more load and are less mobile than their anterior counterparts.4, 28 The same reasons explain why the MMPR is more susceptible to damage when compared with the LMPR.2, 5, 25, 28
Lesions of the meniscal roots correlate with meniscal extrusion, defined as a displacement of the meniscus beyond the margin of the tibial plateau.29 Hein et al.13 demonstrated that MMPR lesions lead to medial meniscal displacement and the formation of a gap at the insertion site, which becomes significantly higher when compressive loads are applied to the knee. This impairs the transmission of circumferential (hoop) stress, leading to functional shock absorption failure and, consequently, to accelerated joint wear.13, 25, 29
In a biomechanical study, Ellman et al.21 defined the structural properties of meniscal roots, comparing intact roots with roots dissected from their additional fibers. They concluded that, except for the lateral meniscus anterior root, the supplementary fibers of the anterior medial meniscus root, the MMPR, and the LMPR are responsible for a significant increase in the mean maximum tensile strength resisted by its roots. These authors suggested that current fixation techniques are not capable of biomechanically reproduce the additional fibers of native meniscal roots. In their study, the maximum force resisted by the posterior meniscal roots was 513.8 N (MMPR) and 509 N (LMPR).25
Most studies that analyzed the biomechanical consequences of meniscal root lesions on the area and the tibiofemoral contact pressure were focused on the posterior roots.1, 2, 4, 5, 6, 8, 13, 30, 31, 32, 33, 34 Allaire et al.1 demonstrated that contact pressure increases with a reduction in the contact area in the medial compartment after MMPR injury. They reported an increase in peak contact pressure of 25.4%, which is comparable to a total meniscectomy. Recently, LaPrade et al.34 examined the effects of an MMPR injury in the area, assessing the mean contact pressure at 0°, 30°, 60°, and 90° of knee flexion. They observed a mean decrease in contact area of 57%, considering the flexion angles tested; the largest reduction was observed at 90° of flexion (64%), and the smallest, in total extension (45%). Regarding mean contact pressures, those authors reported a mean increase of 106%, with the highest increase at 90° of flexion (126%) and the lowest increase at total extension (79%).34
On the lateral side, Schillhammer et al.6 assessed the contact areas and peak contact pressure in the tibiofemoral compartment during simulated gait cycles after the posterior horn of the lateral meniscus was sectioned. They observed that this damage generates a significant increase in peak pressure in the lateral compartment, from 2.8 MPa to 4.2 MPa (50%), as well as a significant decrease (32.6%) of the maximum contact area (from 451 mm2 in the intact state to 304 mm2 after the posterior horn of the lateral meniscus was sectioned).6 LaPrade et al.5 reported their findings for five tested flexion angles (0°, 30°, 45°, 60°, and 90°) and found that an LMPR avulsion decreased contact area by 34% on average; the largest reported decrease was at 90° (40%) and the lowest reduction reported was in total extension (23%). Root avulsion was associated with a mean increase in contact pressure of 56%, with the highest increase at 90° (83%) and the lowest increase at total extension (29%).5
The LMPR has a biomechanical particularity: the consequences of the lesion of this root can vary according to the state of the MFLs, since they play an important role in the transmission of load in the lateral tibiofemoral compartment and in meniscal extrusion prevention.32 Forkel et al.,33 in a porcine model study, concluded that a significant increase in the lateral tibiofemoral contact pressure is only expected in combined LMPR and MFLs lesions. Brody et al.,26 in a study using magnetic resonance imaging (MRI), reported a prevalence of 14% lateral meniscus extrusion in cases of LMPR injury with intact MFLs, and of 60% in the case of combined injuries.
Classification
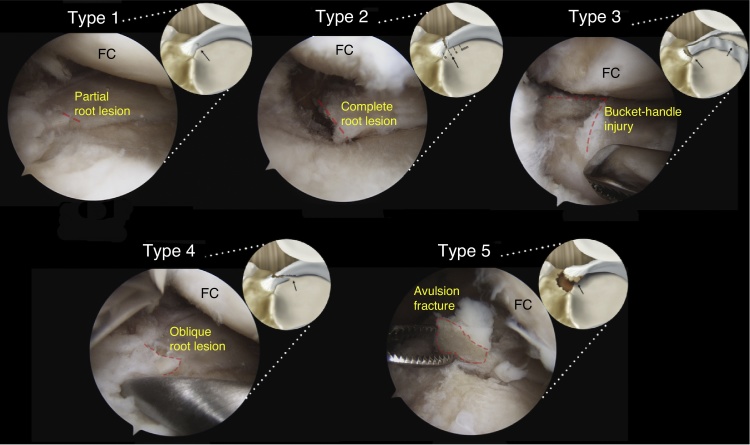
LaPrade et al. developed a classification system20 that can be used for both lesions of the posterior roots (Table 1), which facilitates the documentation of results and patient outcomes. This system can also be used to establish a more appropriate prognosis and therapeutic approach. Fig. 2 shows the classification system for lesions of posterior meniscal roots. It is interesting to note that, in that study, the authors reported a variant in which the MFLs remained intact despite root injury, possibly adding a certain degree of stability and preventing excessive extrusion of the lateral meniscus. All cases in which this variant was observed were reported in type 2 (complete) lesions.20
Table 1.
Classification of the meniscal root injuries.
| Classification | Characteristics | Frequency |
|---|---|---|
| Type 1 | Stable partial lesion within 9 mm of the center of the root fixation | 7 |
| Type 2 | Complete radial lesion within 9 mm of the center of the root fixation | 67.6 |
| 2A | 0–3 mm from the center of the root fixation | 38 |
| 2B | 3–6 mm from the center of the root fixation | 16.9 |
| 2C | 6–9 mm from the center of the root fixation | 12.7 |
| Type 3 | Bucket handle injury with complete displacement within 9 mm of the root fixation | 5.6 |
| Type 4 | Complex oblique pattern within 9 mm of the center of the root fixation | 9.9 |
| Type 5 | Avulsion fracture of the meniscal root of the tibial plateau | 9.9 |
Fig. 2.
Arthroscopic simulation and illustration of the different types of meniscal root lesions classified based on morphology: stable partial root lesion (type 1); complete radial lesion within 9 mm from the posterior fixation in the plateau (type 2); bucket-handle injury with complete root detachment (type 3); longitudinal or complex oblique lesion with total root detachment (type 4); and avulsion fracture of the meniscal root (type 5).
FC, femoral condyle.
Original photograph and partial reproduction of image, with the permission of LaPrade et al.20
Epidemiology and risk factors
Knowledge of the epidemiological characteristics, such as the chronology of lesions or associated pathologies, may help in the diagnosis of a meniscal root lesion. All four meniscal roots are subject to lesions, but the posterior roots are most commonly affected.4, 18, 28
MMPR lesions are the most frequent, with a prevalence of 10–21% among all meniscal surgeries.28 The percentage of all medial meniscus lesions that are located in the posterior root can reach 21.5%.19 They are more commonly observed in a chronic setting, usually in middle-aged women, with more subtle symptoms, degenerative pattern, and often without a definite history of trauma.19, 35 As observed in the acute setting, MMPR tears are usually related to multi-ligament lesions and cartilage damage classified as Outerbridge 2 or higher.18 Other factors related to MMPR injuries include body mass index (BMI), mechanical axis in varus, and low levels of physical activity.19 An increased risk of spontaneous knee osteonecrosis was also described in combination with MMPR lesions.36
LMPR lesions are more commonly observed in acute conditions, in association with ACL lesions, especially in young male patients.32, 37 Up to 8% of ACL injuries have an associated LMPR tear, while injury occurs only in 0.8% of patients with intact ACL.38
In a retrospective study, Mello et al.39 analyzed the epidemiology of meniscal lesions associated with ACL tear. The authors concluded that lateral meniscal injury was more frequent in the first four months after ACL tear, and that the later the reconstruction surgery, the greater the incidence of meniscal injury, especially those in the medial meniscus.
Anterior root lesions may also occur in a traumatic situation, but most studies describe them as a result of an iatrogenic injury, during the perforation of a tunnel for ACL reconstruction or for the introduction of an intramedullary tibial nail.28, 40
Matheny et al.18 described an association between the type of damage and chronicity of the problem. In their study, all lesions classified as types 3 and 5 were observed in acute settings, while lesions types 1, 2, and 4 were observed with similar frequencies in acute and chronic presentations.18
Behavioral characteristics related to Eastern cultures, such as kneeling and squatting, may also be associated with posterior root lesions41 but this aspect is not well defined in the literature.28
Diagnosis
As the symptomatology of meniscal root lesions is highly variable, diagnosis can be challenging, requiring a high degree of suspicion as well as knowledge of the associated risk factors and commonly related lesions.
Clinical evaluation
MMPR injuries are not necessarily associated with a traumatic event. Approximately 70% of patients report a routine event (such as squatting), while others do not report any specific event.25, 42 The most common symptoms of posterior meniscal root tears are posterior knee pain and pain in the articular line, which are nonspecific.32 Mechanical symptoms, such as blocking, are less common. Joint effusion is observed in only 14.3% of the cases, and McMurray test is positive in only 57.1% of patients.43 Seil et al.44 described a test to detect MMPR lesions based on meniscal extrusion. The maneuver consists in applying a stress in varus, with the knee in full extension, while palpating the anteromedial joint line. It is considered positive when the meniscus extrusion can be palpated and disappears when the knee is brought back into normal alignment.
Imaging
Magnetic resonance imaging is the most indicated noninvasive examination.4, 25, 38 Nonetheless, some authors postulate that the only way to confirm a posterior meniscal root injury is through arthroscopy.32 Up to one-third of adjacent radial MMPR lesions cannot be observed on MRI.9, 25 The ability of MRI to detect a posterior meniscal root tear depends on the image quality and the ability of the radiologist.25 Generally, T2-weighted sequences are more suitable to assess meniscal root injury.25 However, a recently-released protocol using fat suppression (FS 3 D VISTA) has shown better performance in the diagnosis of these lesions.28
Normally, posterior meniscal roots can be visualized in two consecutive coronal images as a fibrocartilage band that anchors the posterior horn of the meniscus to the tibial plateau.25 Ideally, coronal, sagittal, and axial images should be assessed.38
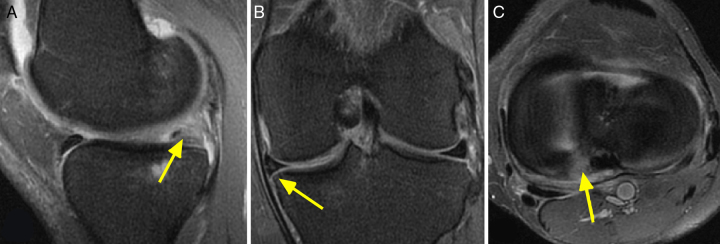
In cases of posterior meniscal root injury, the two most commonly observed radiological signs in MRI studies are meniscal extrusion and the ghost sign,4, 25, 29 which can be seen in Fig. 3.
Fig. 3.
T2-weighted magnetic resonance imaging of a left knee with lesion of the medial meniscus posterior root. Evidencing: (A) sagittal cut, showing the ghost sign (yellow arrow); (B) coronal cut, in which it is possible to observe the medial meniscus extrusion (yellow arrow), and (C) axial cut showing an increase in the sign in the posterior insertion area of the medial meniscus, indicating a radial lesion of this root.
Meniscal extrusion, defined as a meniscal dislocation in relation to the margin of the tibial plateau,29 has been highly correlated with the presence of a meniscal root lesion. Extrusions larger than 3 mm have been associated with meniscal and articular cartilage degeneration.29, 45
The ghost sign is defined as the absence of an identifiable meniscus in the sagittal plane or as a high signal replacing the low signal of the normal meniscus, followed by meniscal images with a normal signal in the immediately adjacent sequences.4, 29
Treatment indications and options
Treatment of posterior meniscal root tears requires a careful evaluation of each patient. Factors that should be considered when choosing a treatment option include – but are not limited to – the condition of articular cartilage and meniscal tissue, mechanical alignment, BMI, patient expectations, and willingness to adhere to the rehabilitation protocol.
Non-surgical treatment may be a reasonable option for older patients,46 those with clinical contraindication to surgery, and those with advanced joint damage in the ipsilateral compartment (Outerbridge 3 or 4). These should be managed with symptomatic relief through the use of analgesics and/or braces.
Surgical options include partial meniscectomy and meniscal root repair. Osteotomies may be indicated alone or in combination with another procedure in selected cases, to treat misalignment of the mechanical axis.31
Prior to the knowledge of the biomechanical and degenerative consequences for the joint and the advent of meniscal preservation techniques, meniscectomy was widely performed as a treatment option for these lesions.1, 7 Currently, selected patients may benefit from this procedure, such as those with osteoarthritis refractory to conservative treatment and who persist with complaints of pain and mechanical symptoms. Patients with partial lesions (type 1) may achieve good results with partial meniscectomy.47
Indications for meniscal repair include patients with an acute history whose cartilage has a normal or near normal appearance, as well as patients with chronic symptoms without preexisting significant osteoarthrosis.25, 35, 42 Contraindications include diffuse chondral injuries grades 3 and 4, uncorrected misalignment, root lesions with definitive meniscal degeneration, and obesity (BMI > 30).25, 35, 48
The techniques for meniscal roots repair can vary in relationship to the surgical approach, type of suture, device used, and fixation technique.
Some surgeons prefer to approach these lesions through a posteromedial portal and occasionally associate a posterolateral portal to facilitate sutures.42, 48, 49 Different ligatures have been reported in the literature, including polydioxanone (PDS) No. 1 (Ethicon, Somerville, NJ); Ethibond No. 2 (Ethicon, Somerville, NJ); and FiberWire No. 0 and No. 2 (Arthrex, Naples, FL).48 Most studies describe the use of two specific types of devices: a curved suture hook35, 42, 43, 49 and an arthroscopic suturing forceps loaded with a needle to pierce the meniscal tissue and deploy the suture.50, 51
Suture techniques reported in the literature include single suture, double suture, simple running suture, locked running suture, modified Kessler, and modified Mason-Allen.52, 53, 54
The most commonly reported fixation techniques are transtibial pull-out and anchors.2, 5, 34, 54 The transtibial pull-out can be attached to the anterior surface of the proximal tibia using a post-tie (screw and washer), cortical device, or bone bridge (when using a two-tunnel technique).43, 49
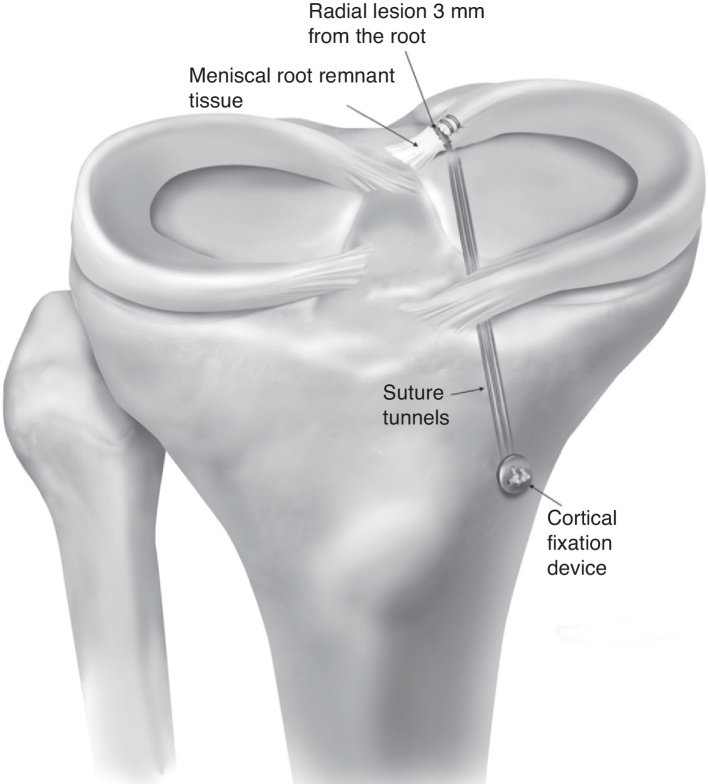
The preferred technique used by the senior author (RFL) involves the use of an arthroscopic forceps loaded with a needle to pierce the meniscal tissue. Two simple sutures are applied to the meniscal root and passed through two tunnels in the proximal tibia. Attachment to the anterior tibial surface is made with a cortical device (Fig. 4).
Fig. 4.
Technique for fixation of lesion of the posterior meniscal root through a transtibial suture fixated to a button on the anteromedial aspect of the tibia. An anatomical positioning of the fixation is necessary to restore the circumferential hoop stress of the meniscus.
Reprinted with the permission of Padalecki et al.2
Postoperative rehabilitation
The rehabilitation protocol used by the senior author (RFL) takes into account the anatomy, biomechanics, outcomes, and clinical judgment; it is divided into different phases and its progression is assessed according to the following criteria.
Phase 1
Based on surgical repair and range of motion (ROM). Weight bearing is not allowed during the first six weeks, in order to avoid stress in the meniscus. Passive movement is immediately performed, limited to 90° flexion for two weeks, followed by complete recovery of passive ROM. The patellofemoral joint, the quadriceps, and the patellar tendon are also immediately mobilized, to prevent scar tissue adhesions. To progress to phase 2, a full ROM (when compared with the contralateral limb) should be achieved, as well as minimal joint effusion, and normal knee temperature.
Level 2
From the seventh week onwards, pre-gait activities are initiated. Weight bearing of 25% of total body weight is allowed, and larger loads are initiated according to patient tolerance. The patient should feel comfortable walking for at least 25 min to progress to phase 3.
Phase 3
Exercises based on a greater number of repetitions and short rest periods are conducted to promote muscular endurance. Exercises with both legs progress to single leg exercises. Squats are progressed up to 70°, according to tolerance. At week 12, stationary bike, freestyle swimming, and treadmill walking are allowed.
Phase 4
The quadriceps is strengthened to achieve at least 80% of the force of the unaffected limb. Multiplanar exercises are initiated to allow neuromuscular control.
Phase 5
This phase varies according to patient demand. At week 22, patients are encouraged to return to running, agility, and change of direction activities. Total return to sports is authorized on a case-by-case status, based on the patient's ability.55
Assessment of outcomes
The comparison of clinical outcomes between the different techniques used to treat meniscal root lesions has conflicting results, as most publications present small samples, different inclusion criteria, lack of control group, and a low level of evidence.
Partial meniscectomy
Widely used in the past as the primary form of treatment of these lesions, the results of meniscectomy in the literature are conflicting. Ozkoc et al.9 analyzed 70 partial meniscectomies in a sample in which approximately 80% of patients were aged over 50 years and were obese. The Lysholm score56 improved from 53 to 67 points. However, despite patient satisfaction, the control radiographs evidenced arthrosis progression.9
In the evaluation of 46 cases of partial meniscectomy with a minimum follow-up of five years, Han et al.8 found radiographic signs of degenerative alterations in 16 patients, and only 56% reported improvement in pain, despite the fact that the Lysholm score had improved significantly.
Repair
Lee et al.43 analyzed the short-term clinical and radiographic results of 21 MMPR lesions treated using transtibial pull-out technique, and observed a significant improvement in both the Lysholm score and the HSS scale. Progression of the degenerative alterations was observed in only one of the knees; in all ten knees in which an arthroscopic revision was made, complete healing of the lesion was observed.43
Regarding the cure rates of the pull-out technique, Cho et al.49 found four completely healed lesions and eight partially healed injuries in 13 knees submitted to arthroscopic revision. The Lysholm score increased from 34.7 to 75.6, and the HSS score improved from 33.5 to 82.2.49
Chung et al.30 conducted a meta-analysis to assess the clinical outcomes of MMPR injury repair and observed a significant improvement on the Lysholm scale; however, meniscal extrusion did not improve, and osteoarthrosis progression was inevitable.
In a recent systematic review, all seven studies – including 172 patients treated with transtibial pull-out – demonstrated functional improvement after the procedure. Among those who underwent an arthroscopic review, 48% presented complete healing, 42% partial healing, and 10% treatment failure. Radiological aggravation of at least one stage in the Kellgren–Lawrence classification was observed in 16% of the 76 patients evaluated for osteoarthrosis progression.48
When comparing the fixation of meniscal root through anchors vs. the pull-out technique, Kim et al.42 found no significant differences in the IKDC,57, 58 Lysholm, and HSS scores, as well as in the degree of articular degeneration between the two groups.
Comparison between partial meniscectomy and repair techniques
The highest Lysholm and IKDC scores and lower rates of progression of degenerative changes were observed in patients with MMPR lesions treated with transtibial pull-out type when compared with those who underwent partial meniscectomy.35 Similar results were demonstrated by Chung et al.31: of 20 patients who underwent meniscectomy, seven required total knee arthroplasty, which was not required in the 37 patients treated with root fixation.
Final considerations
Studies suggest that patients undergoing posterior meniscal root repair, whether using anchors or the transtibial pull-out technique, present functional and clinical benefits when compared with those who underwent meniscectomy. However, more studies with a high level of evidence are needed to establish the relationship between the use of these techniques and the rate of progression to osteoarthritis in the long term.
Conflicts of interest
Dr. Robert F. LaPrade is a technical consultant for Arthrex, Össur, and Smith & Nephew. The other authors declare no conflicts of interest.
Footnotes
Study conducted in a partnership of the Instituto Brasil de Tecnologias da Saúde, Rio de Janeiro, RJ, Brazil, with the Steadman-Philippon Research Institute, Vail, United States.
References
- 1.Allaire R., Muriuki M., Gilbertson L., Harner C.D. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Jt Surg Am. 2008;90(9):1922–1931. doi: 10.2106/JBJS.G.00748. [DOI] [PubMed] [Google Scholar]
- 2.Padalecki J.R., Jansson K.S., Smith S.D., Dornan G.J., Pierce C.M., Wijdicks C.A. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699–707. doi: 10.1177/0363546513499314. [DOI] [PubMed] [Google Scholar]
- 3.Marzo J.M., Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124–129. doi: 10.1177/0363546508323254. [DOI] [PubMed] [Google Scholar]
- 4.Papalia R., Vasta S., Franceschi F., D’Adamio S., Maffulli N., Denaro V. Meniscal root tears: from basic science to ultimate surgery. Br Med Bull. 2013;106:91–115. doi: 10.1093/bmb/ldt002. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade C.M., Jansson K.S., Dornan G., Smith S.D., Wijdicks C.A., LaPrade R.F. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Jt Surg Am. 2014;96(6):471–479. doi: 10.2106/JBJS.L.01252. [DOI] [PubMed] [Google Scholar]
- 6.Schillhammer C.K., Werner F.W., Scuderi M.G., Cannizzaro J.P. Repair of lateral meniscus posterior horn detachment lesions: a biomechanical evaluation. Am J Sports Med. 2012;40(11):2604–2609. doi: 10.1177/0363546512458574. [DOI] [PubMed] [Google Scholar]
- 7.McDermott I.D., Amis A.A. The consequences of meniscectomy. J Bone Jt Surg Br. 2006;88(12):1549–1556. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 8.Han S.B., Shetty G.M., Lee D.H., Chae D.J., Seo S.S., Wang K.H. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26(10):1326–1332. doi: 10.1016/j.arthro.2010.01.032. [DOI] [PubMed] [Google Scholar]
- 9.Ozkoc G., Circi E., Gonc U., Irgit K., Pourbagher A., Tandogan R.N. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–854. doi: 10.1007/s00167-008-0569-z. [DOI] [PubMed] [Google Scholar]
- 10.Pagnani M.J., Cooper D.E., Warren R.F. Extrusion of the medial meniscus. Arthroscopy. 1991;7(3):297–300. doi: 10.1016/0749-8063(91)90131-g. [DOI] [PubMed] [Google Scholar]
- 11.Hede A., Larsen E., Sandberg H. The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop. 1992;16(2):122–125. doi: 10.1007/BF00180200. [DOI] [PubMed] [Google Scholar]
- 12.Seedhom B.B., Dowson D., Proceedings Wright V. Functions of the menisci. A preliminary study. Ann Rheum Dis. 1974;33(1):111. doi: 10.1136/ard.33.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hein C.N., Deperio J.G., Ehrensberger M.T., Marzo J.M. Effects of medial meniscal posterior horn avulsion and repair on meniscal displacement. Knee. 2011;18(3):189–192. doi: 10.1016/j.knee.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Zimny M.L., Albright D.J., Dabezies E. Mechanoreceptors in the human medial meniscus. Acta Anat. 1988;133(1):35–40. doi: 10.1159/000146611. [DOI] [PubMed] [Google Scholar]
- 15.Markolf K.L., Mensch J.S., Amstutz H.C. Stiffness and laxity of the knee – the contributions of the supporting structures. A quantitative in vitro study. J Bone Jt Surg Am. 1976;58(5):583–594. [PubMed] [Google Scholar]
- 16.Mac C.M. The movements of bones and joints; the synovial fluid and its assistants. J Bone Jt Surg Br. 1950;32-b(2):244–252. doi: 10.1302/0301-620X.32B2.244. [DOI] [PubMed] [Google Scholar]
- 17.Renstrom P., Johnson R.J. Anatomy and biomechanics of the menisci. Clin Sports Med. 1990;9(3):523–538. [PubMed] [Google Scholar]
- 18.Matheny L.M., Ockuly A.C., Steadman J.R., LaPrade R.F. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):3127–3131. doi: 10.1007/s00167-014-3073-7. [DOI] [PubMed] [Google Scholar]
- 19.Hwang B.Y., Kim S.J., Lee S.W., Lee H.E., Lee C.K., Hunter D.J. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606–1610. doi: 10.1177/0363546512447792. [DOI] [PubMed] [Google Scholar]
- 20.LaPrade C.M., James E.W., Cram T.R., Feagin J.A., Engebretsen L., LaPrade R.F. Meniscal root tears: a classification system based on tear morphology. Am J Sports Med. 2015;43(2):363–369. doi: 10.1177/0363546514559684. [DOI] [PubMed] [Google Scholar]
- 21.Ellman M.B., LaPrade C.M., Smith S.D., Rasmussen M.T., Engebretsen L., Wijdicks C.A. Structural properties of the meniscal roots. Am J Sports Med. 2014;42(8):1881–1887. doi: 10.1177/0363546514531730. [DOI] [PubMed] [Google Scholar]
- 22.Johannsen A.M., Civitarese D.M., Padalecki J.R., Goldsmith M.T., Wijdicks C.A., LaPrade R.F. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40(10):2342–2347. doi: 10.1177/0363546512457642. [DOI] [PubMed] [Google Scholar]
- 23.Messner K., Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998;193(Pt 2):161–178. doi: 10.1046/j.1469-7580.1998.19320161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson C.J., Ziegler C.G., Wijdicks C.A., Engebretsen L., LaPrade R.F. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Jt Surg Am. 2012;94(21):1936–1945. doi: 10.2106/JBJS.K.01710. [DOI] [PubMed] [Google Scholar]
- 25.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 26.Brody J.M., Lin H.M., Hulstyn M.J., Tung G.A. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239(3):805–810. doi: 10.1148/radiol.2393050559. [DOI] [PubMed] [Google Scholar]
- 27.Shybut T.B., Vega C.E., Haddad J., Alexander J.W., Gold J.E., Noble P.C. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43(4):905–911. doi: 10.1177/0363546514563910. [DOI] [PubMed] [Google Scholar]
- 28.Bonasia D.E., Pellegrino P., D’Amelio A., Cottino U., Rossi R. Meniscal root tear repair: why, when and how? Orthop Rev. 2015;7(2):5792. doi: 10.4081/or.2015.5792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lerer D.B., Umans H.R., Hu M.X., Jones M.H. The role of meniscal root pathology and radial meniscal tear in medial meniscal extrusion. Skelet Radiol. 2004;33(10):569–574. doi: 10.1007/s00256-004-0761-2. [DOI] [PubMed] [Google Scholar]
- 30.Chung K.S., Ha J.K., Ra H.J., Kim J.G. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1455–1468. doi: 10.1007/s00167-015-3832-0. [DOI] [PubMed] [Google Scholar]
- 31.Chung K.S., Ha J.K., Yeom C.H., Ra H.J., Jang H.S., Choi S.H. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy. 2015;31(10):1941–1950. doi: 10.1016/j.arthro.2015.03.035. [DOI] [PubMed] [Google Scholar]
- 32.Feucht M.J., Salzmann G.M., Bode G., Pestka J.M., Kuhle J., Sudkamp N.P. Posterior root tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):119–125. doi: 10.1007/s00167-014-2904-x. [DOI] [PubMed] [Google Scholar]
- 33.Forkel P., Herbort M., Schulze M., Rosenbaum D., Kirstein L., Raschke M. Biomechanical consequences of a posterior root tear of the lateral meniscus: stabilizing effect of the meniscofemoral ligament. Arch Orthop Trauma Surg. 2013;133(5):621–626. doi: 10.1007/s00402-013-1716-7. [DOI] [PubMed] [Google Scholar]
- 34.LaPrade C.M., Foad A., Smith S.D., Turnbull T.L., Dornan G.J., Engebretsen L. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43(4):912–920. doi: 10.1177/0363546514566191. [DOI] [PubMed] [Google Scholar]
- 35.Kim S.B., Ha J.K., Lee S.W., Kim D.W., Shim J.C., Kim J.G. Medial meniscus root tear refixation: comparison of clinical, radiologic, and arthroscopic findings with medial meniscectomy. Arthroscopy. 2011;27(3):346–354. doi: 10.1016/j.arthro.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 36.Robertson D.D., Armfield D.R., Towers J.D., Irrgang J.J., Maloney W.J., Harner C.D. Meniscal root injury and spontaneous osteonecrosis of the knee: an observation. J Bone Jt Surg Br. 2009;91(2):190–195. doi: 10.1302/0301-620X.91B2.21097. [DOI] [PubMed] [Google Scholar]
- 37.Anderson L., Watts M., Shapter O., Logan M., Risebury M., Duffy D. Repair of radial tears and posterior horn detachments of the lateral meniscus: minimum 2-year follow-up. Arthroscopy. 2010;26(12):1625–1632. doi: 10.1016/j.arthro.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 38.De Smet A.A., Blankenbaker D.G., Kijowski R., Graf B.K., Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. Am J Roentgenol. 2009;192(2):480–486. doi: 10.2214/AJR.08.1300. [DOI] [PubMed] [Google Scholar]
- 39.Mello W.A.J., Penteado P.C.F., Marchetto A., Fatarelli I.F.C., Rodrigues R.L., Cerqueira P.H. História das lesões meniscais na reconstrução do ligamento cruzado anterior. Rev Bras Ortop. 1999;34(11):569–574. [Google Scholar]
- 40.Ellman M.B., James E.W., LaPrade C.M., LaPrade R.F. Anterior meniscus root avulsion following intramedullary nailing for a tibial shaft fracture. Knee Surg Sports Traumatol Arthrosc. 2015;23(4):1188–1191. doi: 10.1007/s00167-014-2941-5. [DOI] [PubMed] [Google Scholar]
- 41.Bin S.I., Kim J.M., Shin S.J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20(4):373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 42.Kim J.H., Chung J.H., Lee D.H., Lee Y.S., Kim J.R., Ryu K.J. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. doi: 10.1016/j.arthro.2011.06.033. [DOI] [PubMed] [Google Scholar]
- 43.Lee J.H., Lim Y.J., Kim K.B., Kim K.H., Song J.H. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. doi: 10.1016/j.arthro.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 44.Seil R., Duck K., Pape D. A clinical sign to detect root avulsions of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2011;19(12):2072–2075. doi: 10.1007/s00167-011-1550-9. [DOI] [PubMed] [Google Scholar]
- 45.Costa C.R., Morrison W.B., Carrino J.A. Medial meniscus extrusion on knee MRI: is extent associated with severity of degeneration or type of tear? Am J Roentgenol. 2004;183(1):17–23. doi: 10.2214/ajr.183.1.1830017. [DOI] [PubMed] [Google Scholar]
- 46.Camanho G.L. Dor aguda no joelho do paciente idoso. Rev Bras Ortop. 2008;43(9):361–366. [Google Scholar]
- 47.Mordecai S.C., Al-Hadithy N., Ware H.E., Gupte C.M. Treatment of meniscal tears: an evidence based approach. World J Orthop. 2014;5(3):233–241. doi: 10.5312/wjo.v5.i3.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Feucht M.J., Kuhle J., Bode G., Mehl J., Schmal H., Sudkamp N.P. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: a systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31(9):1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 49.Cho J.H., Song J.G. Second-look arthroscopic assessment and clinical results of modified pull-out suture for posterior root tear of the medial meniscus. Knee Surg Relat Res. 2014;26(2):106–113. doi: 10.5792/ksrr.2014.26.2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Anz A.W., Branch E.A., Saliman J.D. Biomechanical comparison of arthroscopic repair constructs for meniscal root tears. Am J Sports Med. 2014;42(11):2699–2706. doi: 10.1177/0363546514549445. [DOI] [PubMed] [Google Scholar]
- 51.Blackman A.J., Stuart M.J., Levy B.A., McCarthy M.A., Krych A.J. Arthroscopic meniscal root repair using a ceterix novostitch suture passer. Arthrosc Tech. 2014;3(5):e643–e646. doi: 10.1016/j.eats.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mitchell R., Pitts R., Kim Y.M., Matava M.J. Medial meniscal root avulsion: a biomechanical comparison of 4 different repair constructs. Arthroscopy. 2016;32(1):111–119. doi: 10.1016/j.arthro.2015.07.013. [DOI] [PubMed] [Google Scholar]
- 53.Kopf S., Colvin A.C., Muriuki M., Zhang X., Harner C.D. Meniscal root suturing techniques: implications for root fixation. Am J Sports Med. 2011;39(10):2141–2146. doi: 10.1177/0363546511413250. [DOI] [PubMed] [Google Scholar]
- 54.Feucht M.J., Grande E., Brunhuber J., Burgkart R., Imhoff A.B., Braun S. Biomechanical evaluation of different suture techniques for arthroscopic transtibial pull-out repair of posterior medial meniscus root tears. Am J Sports Med. 2013;41(12):2784–2790. doi: 10.1177/0363546513502464. [DOI] [PubMed] [Google Scholar]
- 55.Mueller B.T., Moulton S.G., O’Brien L., LaPrade R.F. Rehabilitation following meniscal root repair: a clinical commentary. J Orthop Sports Phys Ther. 2016;46(2):104–113. doi: 10.2519/jospt.2016.6219. [DOI] [PubMed] [Google Scholar]
- 56.Peccin M.S., Ciconelli R., Cohen M. Questionário específico para sintomas do joelho Lysholm Knee Scoring Scale – Tradução e validação para a língua portuguesa. Acta Ortop Bras. 2006;14(5):268–272. [Google Scholar]
- 57.Metsavaht L., Leporace G., Riberto M., Sposito M.M., Del Castillo L.N., Oliveira L.P. Translation and cross-cultural adaptation of the lower extremity functional scale into a Brazilian Portuguese version and validation on patients with knee injuries. J Orthop Sports Phys Ther. 2012;42(11):932–939. doi: 10.2519/jospt.2012.4101. [DOI] [PubMed] [Google Scholar]
- 58.Metsavaht L., Leporace G., Sposito M.M., Riberto M., Batista L.A. Qual o melhor questionário para avaliar os aspectos físicos de pacientes com osteoartrite do joelho na população brasileira? Rev Bras Ortop. 2011;43(3):256–261. [Google Scholar]