Breast cancer is rare in young women, with an increase in incidence in the fourth and fifth decades. A trend is to defer childbearing to later in life. The issues of pregnancy and breast cancer are of importance as some women discover their breast cancer while pregnant and some may not have completed their family at the time of treatment. We discuss the case of a woman whose breast cancer was diagnosed during pregnancy. We review the choices she was faced with at the time of diagnosis and after treatment.
Sources and selection criteria
To review the effects of pregnancy on outcome in patients with breast cancer we included all studies after 1990 by searching Medline, CINAHL, and Embase combining the headings “pregnancy” and “breast neoplasm”. To investigate the outcome of breast cancer in pregnant women who underwent a termination after being diagnosed during pregnancy, we included all studies published after 1980 personally known to us. For the effects of chemotherapy and radiotherapy given during pregnancy, we searched Medline combining the headings “breast neoplasm”, “radiotherapy”, and the relevant chemotherapy agents. To assess whether delayed administration of chemotherapy impairs outcome, we searched Medline with the term “delay adj chemotherapy” combined with the heading “breast neoplasm”.
Case report
A 33 year old woman with a four year old child presented to her doctor with a painless lump in her right breast. On examination a discrete lump was felt in the upper half of the breast. The doctor referred the woman to a rapid access breast clinic, where a 1.5 cm lump and an area of increased nodularity was confirmed. The features on palpation were indeterminate for type of lesion. Ultrasound guided core biopsies were carried out as ultrasonography and mammography suggested a carcinoma (figs 1 and 2). While awaiting an appointment for the result of the biopsies, the patient discovered she was pregnant. The result of the biopsies confirmed a high grade invasive ductal carcinoma (fig 3).
Fig 1.
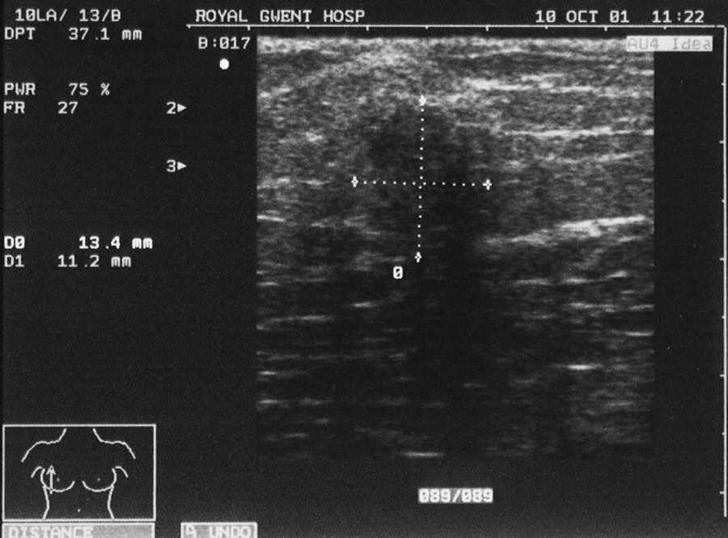
Ultrasonogram showing hypoechoic lesion with irregular margins and acoustic shadowing disrupting normal contours of breast tissue
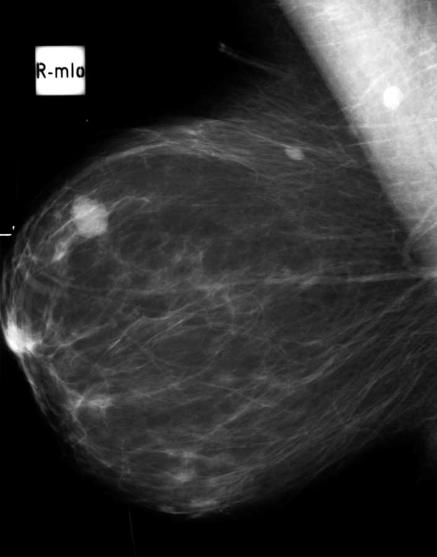
Fig 2.
Mammogram showing dense, oval, lobulated mass lesion with indistinct margins
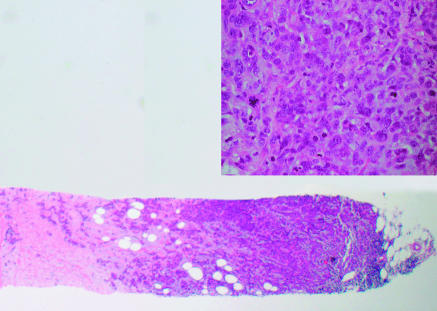
Fig 3.
Invasive ductal carcinoma in core breast biopsy sample (40×). Cells are disorganised, hyperchromatic, and pleomorphic, and several mitoses indicate aggressive, high grade breast cancer (inset, 400×)
The patient decided to terminate her pregnancy after a detailed discussion. Two weeks after the termination she underwent a wide local excision of the breast cancer with axillary node clearance. Histology confirmed a 15 mm, grade 2, invasive ductal carcinoma with possible vascular invasion. Excision was complete. Oestrogen receptor status was weakly positive. None of the 10 axillary lymph nodes examined contained metastatic disease. One month after surgery the patient started chemotherapy. She received six cycles of 5-fluorouracil, epirubicin, and cyclophosphamide. She tolerated chemotherapy well and started tamoxifen. Adjuvant therapy was completed with a course of radiotherapy to the breast. She was followed up every six months with yearly mammography. One year after finishing chemotherapy the patient's periods returned. When she was seen at follow-up she inquired about the implications of pregnancy and whether it would increase the likelihood of recurrence of the breast cancer.
Summary points
Pregnant women with breast cancer have a similar prognosis to that of non-pregnant women with the disease
Evidence is lacking that termination of pregnancy changes the outcome of breast cancer
Pregnancy after breast cancer does not alter the outcome of treatment
The ideal interval between treatment for breast cancer and subsequent pregnancy is unknown
Pregnancy and the prognosis of breast cancer
Pregnancy related increases in hormone levels may stimulate the growth of breast cancer and impair the outcome in patients whose disease is detected during pregnancy. Between 1990 and 2005, 23 studies reported on breast cancer and pregnancy. These studies can be classified into three groups: pregnancy before breast cancer, pregnancy related breast cancer, and subsequent pregnancy.
Pregnancy before breast cancer
Population studies have looked at the interval between last birth and diagnosis of breast cancer, on the assumption that the cancer is present at a subclinical level for some time and that pregnancy related hormonal changes promote its growth. These studies noted that the shorter the interval between birth and diagnosis, the poorer the outcomes.1 w1-w4 Although this evidence indirectly suggests that pregnancy may promote the growth of breast cancer, it does not apply to our patient as her disease was detected at the start of pregnancy. Her previous pregnancy is unlikely to have had an effect on the current disease as it preceded diagnosis by more than four years.
Pregnancy associated breast cancer
Pregnancy associated breast cancer is defined as breast cancer diagnosed during pregnancy or lactation or one year post partum (see table A on bmj.com). Most of the studies on this topic show that such women present with more advanced and aggressive disease.w5-8 w10 w11 Only two studies showed a worse survival when the women were matched stage by stage with non-pregnant women with breast cancer.1 w11
Undoubtedly pregnancy related hormonal changes could play a part in the promotion of breast cancer in all the circumstances in women with pregnancy associated breast cancer. Breast cancers detected during lactation show a different pattern of exposure to hormones than that of breast cancers detected during early pregnancy. In our patient, the presence of the breast cancer at a subclinical level when not pregnant was longer than the three weeks when the breast cancer was exposed to the pregnancy related increase of oestrogen.
Other methodological shortcomings of the studies on pregnancy associated breast cancer were their retrospective design, small sample sizes, and that they often covered long periods during which time breast cancer treatment had changed. In some studies, control groups were not matched for tumour size and stage (see table A on bmj.com).
Knowledge about the influence of pregnancy on breast cancer prognosis is therefore limited. No studies have looked specifically at women presenting with breast cancer during early pregnancy, which could help with the dilemma over management of our patient.
Termination of pregnancy
Our patient's options were to terminate the pregnancy and undergo conventional treatment or to continue with the pregnancy and adjust treatment.
Indications for termination of pregnancy are medical and social. In the case of our patient we had to consider both the mother, assuming a deleterious effect on the disease of continuing pregnancy, and the fetus, considering injury from treatment (surgery, radiotherapy, chemotherapy, or hormonal management).
The social indication in this case was the possibility of the child surviving the mother if the breast cancer recurred.
Medical indications
The mother
Compared with studies of breast cancer diagnosed during pregnancy, there is even less evidence on women who opt for termination after a diagnosis early in pregnancy. The few studies that have looked at this have been hampered by small numbers of patients analysed over decades who were not matched by age and tumour size and stage (see table B on bmj.com). These studies showed no difference in survival between women who did or did not terminate their pregnancy, apart from two where the women who underwent termination fared worse possibly because they were a selected group with advanced disease.w14 w17
The fetus
If pregnancy is to continue after a diagnosis of breast cancer, the effects of treatment (particularly radiotherapy and chemotherapy) on the developing fetus have to be considered.
Radiotherapy—The teratogenic potential of radioactivity on developing fetuses poses a particular dilemma in the management of pregnant women with breast cancer. During the first trimester, the fetus is outside the radiation field of the chest wall but still exposed to scattered radiation. At later stages of pregnancy, although the fetus has grown out of the pelvis and is closer to the radiation field, organogenesis is complete and the effects of radiation are thought to have diminished.2 Anecdotal reports mention fetal malformations (growth retardation with chemotherapy in the first trimester,w18 anal atresia, retrovaginal fistula) as well as normal pregnancy outcomes in pregnant women receiving radiotherapy for breast cancer.w19 w20 The teratogenic potential of radiotherapy has to be weighed up against improvements in recurrence-free survivalw21 and overall mortality from breast cancer.w22 w23 Whether evidence of reduced mortality from radiotherapy is strong enough to change the indications of its use during pregnancy is an issue of ongoing debate.3 If our patient had wanted to continue her pregnancy, we would not have recommended breast conserving surgery because of the need for adjuvant radiotherapy. A proportion of patients who have a mastectomy are advised to undergo radiotherapy to reduce the risk of local recurrence. The information required to make this decision is only available after surgery. Our patient would not have fallen into this category.
Chemotherapy—Our patient's core biopsy sample showed a high grade ductal carcinoma, and we expected her to require postoperative adjuvant chemotherapy. Chemotherapy has shown benefits in premenopausal women with high grade breast cancer, including those without lymph node metastasis.w24 Chemotherapy can cross the placenta and, if given up to week 15 of gestation, interferes with cell differentiation leading to permanent organ malformations or malformations of the central nervous system, eyes, bones, and teeth, which still undergo differentiation thereafter. Theoretically, miscarriage, stillbirth, and low for gestational age birth may occur. Most experience is with cyclophosphamide. Although normal outcomes have been reported in women who, unknowingly pregnant, received cyclophosphamide at conception and during the first trimester,w19 w25 several studies have reported congenital abnormalities.w26-w33 To our knowledge reports are lacking on adverse pregnancy outcomes after exposure to cyclophosphamide, epirubicin, and 5-fluorouracil during the second and third trimester. No long term follow-up studies have been carried out on neurodevelopment or late occurrence of malignancies in children exposed to these agents.
Delaying chemotherapy owing to pregnancy
The question arises as to whether delaying chemotherapy until the second trimester impairs a woman's prognosis. Assuming the diagnosis is made early in pregnancy, as in our patient, is it disadvantageous to delay chemotherapy?
One study detected no difference in disease-free survival in women receiving fluorouracil, doxorubicin, and cyclophosphamide within 10 weeks or after 10 weeks of surgery for breast cancer.4 The daily increased risk of developing axillary metastasis (as the most important prognostic indicator) for an untreated breast carcinoma in a pregnant woman is estimated to be 0.057%.5 After surgery, our patient should, if anything, have a lower risk. Therefore the concern of delaying chemotherapy is not reflected in the literature or by estimates about the risk of metastatic spread to the axilla.
Ultimately it is the patient who decides on the management of her breast cancer and pregnancy. Evidence is lacking of a poorer outcome if management is modified to allow continuation of pregnancy. If a pregnancy was planned then the patient not only has to come to terms with the diagnosis of breast cancer but also with the termination of her pregnancy.
Implications of breast cancer treatment on pregnancy
Subsequent pregnancy
Advice on the implications of subsequent pregnancies after breast cancer is limited. All studies on the effect of subsequent pregnancy on recurrence of breast cancer and survival found a better outcome in women who became pregnant after treatment (see table C on bmj.com). Women who decide to become pregnant after such treatment may, however, form a self selected group with better prognosis (“healthy mother effect”6). Matching pregnant and non-pregnant cohorts is another problem in the design of studies on subsequent pregnancies. Women who subsequently become pregnant are less likely to have had a recurrence before they became pregnant. This was adjusted for in only three studies.6 w37 w38
Studies on the effect of breast cancer treatment on subsequent pregnancies included patients with full term pregnancies or those who had a miscarriage or terminated their pregnancy. They form a heterogeneous group, as the hormonal changes of these events are different. Miscarriage and termination of pregnancies may be under-reported or included in the comparison group of non-pregnant women. Despite these limitations in design, the studies did not detect a worse outcome in women who subsequently became pregnant after treatment for breast cancer (see table C on bmj.com).
Timing of pregnancy
Opinion on the best timing of pregnancy after breast cancer treatment is divided. Only one study analysed the effect of timing and found no difference in outcome.7 About half of the patients became pregnant within two years of treatment.w37 w38
Reasons to defer pregnancy are based on the argument that most recurrences occur early after breast cancer treatment, particularly in women with lymphnode metastasis.8 Others point out that in the breast cancer overview studies recurrences occur at a constant rate,w40 and therefore women should not defer pregnancy.9 Our patient was not in a high risk group for early recurrence because of the absence of lymph node metastasis.
Additional educational resources
Petrek JA, Theriault RL. Pregnancy-associated breast cancer and subsequent pregnancy in breast cancer survivors. In: Harris JR, Lippman ME, Morrow M, Osborne CK, eds. Diseases of the breast, 3rd ed. Philadelphia: Lippincott Williams and Wilkins, 2004: 1036-46.
US National Cancer Institute (www.nci.nih.gov/cancertopics/pdq/treatment/breast-cancer-and-pregnancy/)—covers breast cancer and pregnancy. Versions available for doctors and patients.
Royal College of Obstetrics and Gynaecology (www.rcog.org.uk/resources/Public/Pregnancy_breast_cancer_No12.pdf)—evidence based guidelines on the management of breast cancer and pregnancy.
Information for patients
US based charity breastcancer.org (www.breastcancer.org/pregnancy_during.html)—lively animated website that covers breast cancer and pregnancy. It is possible to listen to the pronounciation of technical terms and their explanation by clicking on one of a selection of celebrities (for example, Martina Navratilova, Whoopi Goldberg). Links are also available to fertility related issues of breast cancer treatment.
UK breast cancer charity, Breast Cancer Care (www.breastcancercare.org.uk/Breastcancer/Youngerwomen andbreastcancer/Breastcancerduringpregnancy)—provides information on breast cancer and pregnancy for patients. Links are available to other relevant topics, such as how to talk to children about breast cancer, or to organisations that can help with child care during treatment.
Fertility declines in the fourth decade and may be further impaired by chemotherapy. By delaying pregnancy, a narrow window of opportunity of a possibly important aspect of quality of life and rehabilitation may be missed. We therefore attempted to draw a cautiously optimistic picture for our patient, but also outlined the dilemma of her not seeing her child grow up if the breast cancer recurred.
Tamoxifen and pregnancy
Tamoxifen has been investigated in uses as contradictory as emergency contraceptionw41 and ovulation induction.w42 It is licensed for ovulation induction and therefore women who do not want to become pregnant while taking it are advised to use a non-hormonal form of contraception. The British National Formulary recommends stopping tamoxifen for two months before attempting pregnancy.10 This is what we advised our patient. Congenital abnormalities have been reported after exposure to tamoxifen in utero in animal studiesw43 and case reports.w44 w45 Normal pregnancy outcomes have also been reported.w46-w49 Women who discontinue tamoxifen will miss out on its benefits but may not become pregnant. After an informed discussion, women may be offered the choice of stopping tamoxifen or continuing treatment for its well established beneficial effects on disease-free survival, accepting the unknown risk of fetal abnormalities.11
In the end our patient decided to avoid pregnancy. She continues to take tamoxifen.
Supplementary Material
 Details of studies and references w1-w49 are on bmj.com
Details of studies and references w1-w49 are on bmj.com
We thank the patient for contributing her case, A M Wake for the ultrasonogram and mammogram images, and I W Thompson and A M Rashid for the pathology slide.
Contributors: LB conceived the article. LAD liaised with the patient. All authors contributed ideas to the manuscript. CAG is guarantor for the paper.
Funding: None.
Competing interests: LB is opposed to abortion. His over-riding interest is to support women in making an informed decision. CAG and CC have been supported by AstraZeneca, the manufacturer of tamoxifen, to attend courses and conferences.
References
- 1.Guinee VF, Olsson H, Moller T, Hess KR, Taylor SH, Fahey T, et al. Effect of pregnancy on prognosis for young women with breast cancer. Lancet 1994;343: 1587-9. [DOI] [PubMed] [Google Scholar]
- 2.Saunders CM. Breast cancer and pregnancy. In: Tobias JS, Houghton J, Henderson IC, eds. Breast cancer—new horizons in research and treatment. London: Arnold, 2001(Sept 28); 316-31.
- 3.Murray EU, Werner ID. Frequency and abortion in breast cancer patients. [Letter.] S Afr Med J 1997;88: 155. [Google Scholar]
- 4.Buzdar AU, Smith TL, Powell KC, Blumenschein GR, Gehan EA. Effect of timing of initiation of adjuvant chemotherapy on disease-free survival in breast cancer. Breast Cancer Res Treat 1982;2: 163-9. [DOI] [PubMed] [Google Scholar]
- 5.Nettleton J, Long J, Kuban D, Wu R, Shaeffer J, El-Mahdi A. Breast cancer during pregnancy: quantifying the risk of treatment delay. Obstet Gynecol 1996;87: 414-8. [DOI] [PubMed] [Google Scholar]
- 6.Sankila R, Heinavaara S, HakulinenT. Survival of breast cancer patients after subsequent term pregnancy: `healthy mother effect.' Am J Obstet Gynecol 1994;170: 818-23. [DOI] [PubMed] [Google Scholar]
- 7.Kroman N. Should women be advised against breast cancer after breast-cancer treatment? Lancet 1997;350: 319-22. [DOI] [PubMed] [Google Scholar]
- 8.Donegan WL. Breast carcinoma and pregnancy. In: Donegan WL, Spratt JS, eds. Cancer of the breast, 4th ed. Philadelphia: WB Saunders, 1995; 732-41.
- 9.Merkel DE. Pregnancy and breast cancer. Sem Surg Oncol 1996;12: 370-5. [DOI] [PubMed] [Google Scholar]
- 10.British National Formulary. bnf.org/bnf/bnf/current/noframes/127053.htm?q=%22tamoxifen%22 (accessed 27 Apr 2005).
- 11.Barthelmes L, Gateley CA. Tamoxifen and pregnancy. Breast 2004;13: 446-51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.