Abstract
Objective
Most inpatient care for the uninsured and other vulnerable subpopulations occurs in safety‐net hospitals. As insurance expansion increases the choice of hospitals for the previously uninsured, we examined if Massachusetts health reform was associated with shifts in the volume of inpatient care from safety‐net to non‐safety‐net hospitals overall, or among other vulnerable sociodemographic (racial/ethnic minority, low socioeconomic status, high uninsured rate area) and clinical subpopulations (emergent status, diagnosis).
Data Sources/Study Setting
Discharge records for adults discharged from all nonfederal acute care hospitals in Massachusetts, New Jersey, New York, and Pennsylvania 2004–2010.
Study Design
Using a difference‐in‐differences design, we compared pre‐/post‐reform changes in safety‐net and non‐safety‐net hospital discharge outcomes in Massachusetts among adults 18–64 with corresponding changes in comparisons states with no reform, overall, and by subpopulations.
Principal Findings
Reform was not associated with changes in inpatient care use at safety‐net and non‐safety‐net hospitals across all discharges or in most subpopulations examined.
Conclusions
Demand for inpatient care at safety‐net hospitals may not decrease following insurance expansion. Whether this is due to other access barriers or patient preference needs to be explored.
Keywords: Health reform, insurance expansion, safety net, inpatient care, disparities
With sharp reductions in public payments to safety‐net hospitals (e.g., disproportionate share payments) under the Affordable Care Act (ACA), safety‐net hospitals will have to adapt to a new payment environment where financial viability is more closely tied to patient demand for inpatient care and insurance reimbursement rates for that care in a potentially more competitive marketplace that includes the newly insured (Andrulis and Siddiqui 2011). Declining safety‐net hospital inpatient volumes could signal the declining of the importance of safety‐net hospitals in the care of vulnerable populations and lead to a worsening of their financial position or even closure. Insurance expansion may (Newhouse 1996; Finkelstein et al. 2012) or may not (Kolstad and Kowalski 2012) lead to increased demand for health care, including inpatient care. As care for the uninsured is largely delivered through safety‐net providers, following insurance expansion, the newly insured gain a wider choice of providers, and some patients may switch hospitals based on preference, convenience, care coordination, or perceived provider quality (Hadley and Cunningham 2004; Chatterjee et al. 2012; Lasser et al. 2016). The extent of switching, though, may be curbed by the influence of other potential barriers, including physician availability and narrow provider networks (Gruber 2011; McCormick et al. 2012; Chandra, Gruber, and McKnight 2014; Cusano and Thomas 2014). Therefore, the actual impact of reform on use of inpatient care from safety‐net hospitals, which may occur over an extended period of time, is difficult to predict and is important to examine empirically. Understanding post‐reform changes in utilization of safety‐net hospitals is critical for future public policy aimed at ensuring health equity, a primary goal of the ACA (Andrulis and Siddiqui 2011).
A precursor to the ACA, the MA reform shared all the major elements of the ACA: individual and employer insurance mandate, subsidized insurance coverage, and establishment of an exchange for individual and group insurance plans (Miller 2012). Prior research on the impact of the MA reform about use of care from the safety net is limited (Ku et al. 2011; Mohan et al. 2013; Bazzoli and Clement 2014). Two studies found that overall inpatient discharges, covering all patient age groups, increased at a similar pace between 2006 and 2009 in safety‐net (1.8 percent) and non‐safety‐net hospitals (2.1 percent) (Ku et al. 2011; Mohan et al. 2013). Another study examined discharge volumes by payers (Bazzoli and Clement 2014). However, as prior studies were based on aggregate hospital‐level data, examination of patients aged 18–64, the target population for reform, or vulnerable sociodemographic subpopulations (race‐ethnic minorities or low income patients) was not possible.
Thus, given the paucity of data regarding patterns of inpatient care use specific to patients targeted by insurance reform, we used discharge‐level data for 2004–2010, to estimate the change in inpatient care utilization associated with MA reform among safety‐net and non‐safety‐net hospitals. To isolate the change associated with reform, we used a difference‐in‐differences design, contrasting the pre‐reform to post‐reform change in MA with the corresponding change in comparison states without an expansion. The primary outcome measure was hospital discharge volume covering patients aged 18–64. We tested the null hypothesis that MA health reform was associated with a reduction in discharge volume in safety‐net hospitals for overall care, and for care provided to subpopulations based on sociodemographics (racial/ethnic minority, low socioeconomic status, high uninsured rate area) and admission characteristics (emergent status and diagnostic condition).
Methods
Data and Study Population
Our primary data sources were the annual inpatient discharge databases for 2004–2010 from MA and three comparison states: New Jersey (NJ), New York (NY), and Pennsylvania (PA). We selected the comparison states for their geographic proximity to MA and sizable minority populations. We excluded discharge data for patients who were not residents of the state where the hospital was located, since our interest is in comparing the utilization patterns of MA residents with their counterparts in the comparison states. Due to state‐level differences in the types of hospitals covered in the discharge databases, we selected “community” hospitals, as defined by the American Hospital Association Annual Survey; specifically, these excluded nonacute long‐term care, psychiatric and rehabilitative care hospitals (American Hospital Association 2014). We also excluded hospitals that were not in operation during all years of the study period so that post‐reform changes could be compared with pre‐reform experience.
Cases and Controls
We identified all inpatient discharges for adults aged 18–64 in MA, the primary target beneficiaries of the reform (“cases”). Controls consisted of all inpatient discharges for the same age group in NJ, NY, and PA.
Pre‐reform and Post‐reform Periods
The main elements of MA health care reform — Medicaid expansion, subsidies for private insurance, and establishment of the insurance exchange — were introduced in phases beginning on 7/1/2006 and ending with the establishment of a penalty‐enforced individual mandate effective January 1, 2008. Treating this time interval as the “transition” period, we defined “pre‐reform” (1/1/2004–6/30/2006) and “post‐reform” (1/1/2008–6/30/2010) periods as 30 months preceding and following the transition period, respectively.
Primary Outcome Measure
Our primary outcome measure was the volume of hospital admissions. Treating a hospital as the unit of observation, volume was measured as the total count of hospital patient discharges stratified by quarter. With 498 hospitals and 26 quarter, there were a total of 12,948 observations.
Safety‐Net and Non‐Safety‐Net Hospitals
Safety‐net hospitals are generally characterized as the main providers of inpatient care for underserved and vulnerable populations (Institute of Medicine 2000). In the absence of a formal definition to identify safety‐net hospitals, we followed previous work and defined them as the top quartile of hospitals by the share of all discharges in each hospital covered by self‐pay, Medicaid, or other subsidized public care (e.g., Uncompensated Care Pool coverage in MA) (Werner, Goldman, and Dudley 2008; Ku et al. 2011). Hospitals in each state were grouped separately into safety‐net and non‐safety‐net hospitals. Only pre‐reform discharges were used in obtaining this grouping, to prevent potential confounding arising from the reform affecting receipt of care at safety‐net hospitals.
Patient and Admission Subgroups
Our main focus is on changes in outcome measures, following reform, in safety‐net versus non‐safety‐net hospitals in MA as compared to NJ, NY, and PA. We also examined these changes for several vulnerable subpopulations, to elicit greater granularity within the groups affected, including Hispanics, non‐Hispanic blacks, and low‐income‐area residents. Race and ethnicity data, obtained from the discharge data, were nearly complete. For instance, 3.6 percent and 1.9 percent of discharges in MA and control states, respectively, had missing race and/or ethnicity; these were grouped with non‐Hispanic whites based on evidence from our prior work (Hanchate et al. 2015; McCormick et al. 2015). Using median income of patient residence zip code, we identified residents in the lowest income quartile of zip codes (Jha et al. 2005).
To examine if outcome changes differed by baseline uninsured rate, we used county‐level data on pre‐reform uninsured rate and divided each state into two parts: the top and bottom half of counties by pre‐reform uninsured rate (Health Resources and Services Administration 2014).
Severity and acuity of medical condition may also affect the likelihood of switch from safety‐net to non‐safety‐net hospitals; for instance, demand for nonacute elective procedures is more likely to be susceptible to switch in provider. To examine such patterns, we estimated reform‐associated change in hospital volumes in safety‐net and non‐safety‐net hospitals for admissions differing in patient acuity and severity. Patient acuity was determined by whether the patient admission was through an emergency department (high acuity) or not (low acuity). Patient severity was quantified by risk of inpatient death; grouping the principal diagnosis code for all admissions into 283 categories using Agency for Healthcare Research and Quality (2010) Clinical Classification System, we identified the top half of diagnostic categories by average inpatient mortality as high risk and the remaining categories as low risk (Agency for Healthcare Research and Quality 2010).
Estimation
As an indicator of summary longitudinal trends, we compared quarterly rates of average admission volume for safety‐net and non‐safety‐net hospitals, adjusted for seasonality by using a four‐quarter moving average. We estimated log‐linear time series models to measure overall rates of change in the two hospital settings, in MA and comparison states. To isolate the change in volume associated with health reform, in each hospital setting (safety‐net and non‐safety‐net), we performed difference‐in‐differences analysis using linear regression models, including dichotomous indicators for post‐reform period (1/0) and MA hospitals (1/0) as covariates. The estimate of the post‐reform change in volume in MA associated with health reform — henceforth termed “net change” — was obtained from the coefficient of the interaction of the indicators for post‐reform period and MA hospitals (Wooldridge 2002; Kolstad and Kowalski 2012; Nasseh and Vujicic 2013; Dimick and Ryan 2014; Hanchate et al. 2015). We adjusted for state‐level annual changes in population aged 18–64 using an index of annual change with baseline (2004) value set at 1.0 in each state. Using a difference‐in‐differences specification, we also estimated the relative change between the two settings, that is, the difference in the change between safety‐net and non‐safety‐net hospitals associated with health reform. In both model specifications we also adjusted for unobserved hospital‐level differences with hospital fixed effects, and for secular temporal fluctuations (e.g., the economic downturn in 2008) with quarterly fixed effects (Cameron and Trivedi 2005; Hanchate et al. 2008; Kolstad and Kowalski 2012). We obtained robust standard error estimates adjusted for clustering at the hospital level (Bertrand, Duflo, and Mullainathan 2004; Cameron and Trivedi 2005). For ease of interpretation, we have also reported the net change in terms of percentage change in hospital volume using the pre‐reform mean value in MA as the baseline level.
We also assessed the suitability of the difference‐in‐differences design based on the criteria proposed by Ryan, Burgess, and Dimick (2015); results of this assessment are reported in Tables SA1–SA6. Statistical significance was assessed at the level of p < .05. All estimation was performed using Stata Version 13.1 (StataCorp 2014).
Sensitivity Analysis
We assessed the robustness of the main findings to choice of alternative thresholds in the hospital‐level proportion of patients covered by self‐pay, Medicaid, or other subsidized public program in the definition of safety‐net hospitals. Change in hospital capacity can confound volume changes; to assess this possibility we examined if annual hospital bed capacity varied systematically pre‐/post‐reform period across MA and control states, separately in safety‐net and non‐safety‐net hospitals.
The Boston University Medical Campus Institutional Review Board approved this study.
Results
We examined 64 hospitals in MA and 434 hospitals in the three control states which accounted for 99.8 percent and 96.7 percent of all discharges, respectively. We categorized 16 hospitals in MA and 107 hospitals in the control states as safety‐net hospitals (Table 1). Safety‐net hospitals had more young, non‐white, and low‐income patients compared to non‐safety‐net hospitals during the study period (2004–2010). Hospital volume, on average, was higher in safety‐net (2,308/quarter) than non‐safety‐net hospitals (1,261) in MA.
Table 1.
Study Population of Inpatient Discharges Age 18–64 in Massachusetts, New Jersey, New York, and Pennsylvania, 1/1/2004–6/30/2010
| Massachusetts | Control States | |||
|---|---|---|---|---|
| Safety‐Net Hospitals | Non‐Safety‐Net Hospitals | Safety‐Net Hospitals | Non‐Safety‐Net Hospitals | |
| No. of hospitals | 16 | 48 | 107 | 327 |
| No. of discharges | 960,269 | 1,573,550 | 5,247,415 | 11,178,273 |
| Patient age, % | ||||
| 18–44 | 52.4 | 50.1 | 53.2 | 48.4 |
| 45–54 | 23.5 | 23.4 | 24.0 | 24.0 |
| 55–64 | 24.1 | 26.5 | 22.7 | 27.6 |
| Race/ethnicity, % | ||||
| Whites, non‐Hispanic & Others | 73.8 | 87.7 | 51.7 | 78.2 |
| Blacks, non‐Hispanic | 12.7 | 6.1 | 32.4 | 13.7 |
| Hispanic | 13.5 | 6.2 | 15.9 | 8.1 |
| Income, Zip code median, % | ||||
| Low | 50.5 | 19.9 | 50.6 | 22.6 |
| Medium | 22.6 | 25.6 | 22.8 | 25.9 |
| High | 26.9 | 54.5 | 26.6 | 51.5 |
| Outcomes | ||||
| Mean discharge volume, quarterly | 2,308 | 1,261 | 1,886 | 1,307 |
During 2004–2010, quarterly hospital volumes showed similar longitudinal trends across safety‐net and non‐safety‐net hospitals in MA and comparison states. Overall, the volume of hospital admissions increased both in safety‐net (0.8 percent per year) and non‐safety‐net hospitals (1.0 percent) in MA (Figure 1); these rates were similar in control states (0.8 percent and 0.64 percent, respectively). Based on difference‐in‐differences analysis, health reform was associated with a 0.6 percent and 1.6 percent net increase in hospital admission volume in safety‐net and non‐safety‐net hospitals in MA, respectively; however, these changes were not statistically significant (Table 2 A and B). The relative change between safety‐net and non‐safety‐net hospitals associated with reform was −0.5 percent and not statistically significant. These quantities indicate cumulative changes over a 4‐year time interval (between the mid‐points of the pre‐ and post‐reform periods).
Figure 1.
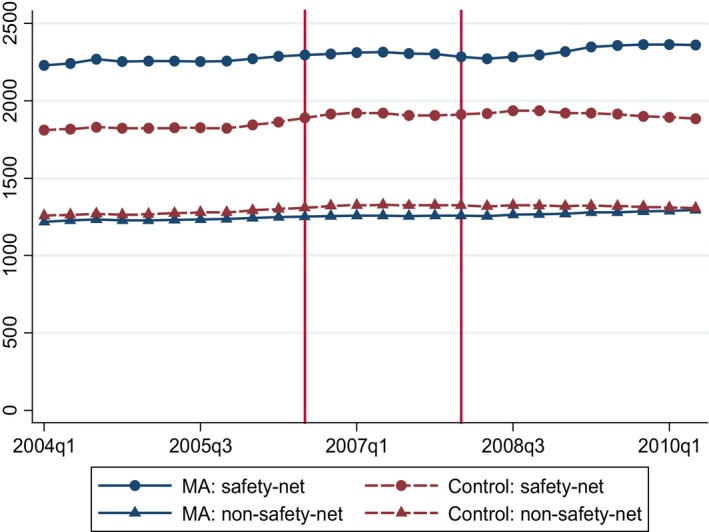
- Notes. To adjust for seasonality, we calculated a four‐quarter moving average. The vertical lines indicate the beginning and end of reform implementation (transition period).
Table 2.
Change in Hospital Admission Volume with Health Reform: (A) Regression Estimates and (B) % Change between Pre‐ and Post‐reform Periods
| Outcome | Safety‐Net Hospitals (a) | Non‐Safety‐Net Hospitals (b) | Relative Change between Safety‐Net and Non‐Safety‐Net Hospitals (c) |
|---|---|---|---|
| (A) | |||
| Post‐reform period × Massachusetts × safety‐net | −11.52 [−122.58, 99.54] | ||
| Post‐reform period × Massachusetts | 13.03 [−88.37, 114.42] | 20.32 [−30.00, 70.63] | 21.36 [−29.20, 71.92] |
| Post‐reform period × safety‐net | 36.64 [−13.70, 86.98] | ||
| Post‐reform period | 274.53* [29.61, 519.45] | 198.07* [75.54, 320.59] | 207.89* [95.52, 320.26] |
| Safety‐net | |||
| Transition period × Massachusetts × safety‐net | −14.97 [−78.91, 48.98] | ||
| Transition period × Massachusetts | −46.67 [−104.97, 12.04] | −29.11 [−58.38, 0.16] | −29.70* [−58.61, −0.80] |
| Transition period × safety‐net | 33.40 [−0.40, 67.20] | ||
| Transition period | 163.62* [47.63, 279.61] | 103.93* [41.45, 166.41] | 110.42* [53.98, 166.86] |
| State population index, age 18–64 (2004 = 1.0) | −5,817.89 [−13,428.19, 1,792.40] | −4,095.19* [−7,481.27, −709.11] | −4,520.30* [−7,670.04, −1,370.57] |
| Indicators of quarters (N = 26) | Yes | Yes | Yes |
| (B) | |||
| Change in admission volume associated with health reform | 0.6% [−3.9%, 5.0%] | 1.6% [−2.4%, 5.7%] | −0.5% [−5.4%, 4.4%] |
Statistical significance: * denotes p < .05.
These are estimates from the linear regression models used to estimate net change in MA associated with reform using residents of NJ, NY, and PA as controls and defining safety‐net hospitals as hospitals in the top 25% of state hospitals by share of all discharges covered by patients on self‐pay, Medicaid, and other subsidized public care. The outcome measure is the number of admissions in each hospital each quarter. We used data from 1/1/2004 to 6/30/2010, divided into 26 quarters, with the first 10 and last 10 representing the pre‐ and post‐reform periods, and the intermediate six quarters representing the transition period during which elements of the reform were phased in. All regressions allowed for hospital fixed effects to adjust for time invariant factors associated with volume. For safety‐net hospitals (column (a)), the difference‐in‐differences specification contrasted change between safety‐net hospitals in Massachusetts versus safety‐net hospitals in comparison states as follows (Ryan, Burgess, and Dimick 2015): y it = β 0 + β 1(Post‐reform * MA) + β 3 Post‐reform + β 4(Transition * MA) + β 5 Transition + β 6 Population\index + I t + I i where y it denotes admission volume in hospital i in quarter t, Post‐reform (1/0) is an indicator of the post‐reform period, MA (1/0) is an indicator of a hospital in Massachusetts, Transition (1/0) is an indicator of the transition period, and I t and I i denotes the set of dichotomous (dummy) indicators for 24 quarters (with indicators of 2 of the 26 quarters not included so as to identify the coefficients of Transition and Post‐reform terms; indicators of the last quarter of transition and post‐reform periods were not included) and hospital (N = 123 safety‐net hospitals). Population_index is an indicator of growth in annual state population treating the base year (2004) as 1.0; a population_index of 1.11 in 2008 indicates 11% increase in state population (relative to 2004); all quarters of each year are assigned the same index value. For non‐safety‐net hospitals, we estimated an analogous model (column (b)), now with N = 375 non‐safety‐net hospitals. To estimate relative change in safety‐net vs. non‐safety‐net hospitals in Massachusetts, contrasted with that in the comparison states (column (c)), we estimated the following model: where Safety‐net (1/0) is an indicator of a safety‐net hospital.
As a test of the suitability of NJ, NY, and PA as comparison states to MA, we obtained difference‐in‐differences estimates based on comparisons in hospital volume at distinct periods prior to reform (parallel trends test); estimates of no net change, indicating similar trends, support the choice of the comparison states (Table A2–A4).
In sensitivity analyses, alternate cut‐offs — top 10 percent and top 5 percent of hospitals by share of patients covered by self‐pay, Medicaid, and other subsidized public programs — in identifying safety‐net and non‐safety‐net hospitals also indicated no change in hospital volumes following reform (Table A5). We found no difference between MA and control states in the pre‐/post‐reform changes in hospital bed capacity in either the safety‐net or the non‐safety‐net hospitals (Table A6).
We also found no significant change in hospital discharge volume associated with health reform among the sociodemographic vulnerable subgroups: Hispanics, blacks, low‐income‐area residents, and high baseline uninsured rate areas (Table 3). Similarly, we found no significant change in hospital volumes for admissions grouped by patient risk and acuity (Table 4).
Table 3.
Change (%) in Hospital Admission Volume in Massachusetts Associated with Health Reform among Vulnerable Subpopulations by Safety‐Net Hospital Status
| Subpopulation | Safety‐Net Hospitals (a) | Non‐Safety‐Net Hospitals (b) | Relative Change between Safety‐Net and Non‐Safety‐Net Hospitals (c) |
|---|---|---|---|
| Race/ethnicity | |||
| Hispanics | 5.2% [−5.2%, 15.7%] | 4.3% [−15.2%, 23.7%] | 4.1% [−7.4%, 15.5%] |
| Blacks, non‐Hispanic | −6.4% [−27.3%, 14.4%] | 11.1% [−5.9%, 28.1%] | −1.3% [−13.0%, 10.5%] |
| Socioeconomic status | |||
| Low‐area‐ income residents | 1.9% [−2.2%, 6.0%] | −1.8% [−8.8%, 5.2%] | 2.4% [−2.0%, 6.7%] |
| Baseline uninsured rate | |||
| High uninsured rate counties | 0.2% [−8.3%, 8.7%] | 3.4% [−1.2%, 8.0%] | −4.1% [−14.1%, 5.8%] |
| Low uninsured rate counties | 0.8% [−3.1%, 4.7%] | −0.9% [−7.2%, 5.4%] | 1.4% [−2.7%, 5.4%] |
The regression models are identical to those used for Table 2 estimated separately for volumes for different subgroups of patients.
Table 4.
Change (%) in Hospital Admission Volume by Admission Severity, Acuity, and Safety‐Net Hospital Status
| Admission Type | Safety‐Net Hospitals (a) | Non‐Safety‐Net Hospitals (b) | Relative Change between Safety‐Net and Non‐Safety‐Net Hospitals (c) |
|---|---|---|---|
| Admission severity | |||
| High‐risk conditions | 5.4% [−1.3%, 12.1%] | 1.8% [−4.9%, 8.4%] | 4.9% [−2.7%, 12.4%] |
| Low‐risk conditions | −2.0% [−6.6%, 2.5%] | 1.6% [−2.7%, 5.8%] | −3.4% [−8.4%, 1.6%] |
| Admission acuity | |||
| High acuity | −2.2% [−16.6%, 12.3%] | 4.2% [−2.9%, 11.2%] | −5.0% [−19.7%, 9.7%] |
| Low acuity | 4.0% [−13.3%, 21.3%] | −0.6% [−6.7%, 5.6%] | 5.1% [−12.3%, 22.6%] |
The regression models are identical to those used for Table 2, estimated separately for hospital volumes of different types of admissions.
Discussion
The 2006/07 health reform in MA was not associated with any significant shifts in the volume of admissions at safety‐net hospitals after two and a half years. This finding was consistent across different sociodemographic and clinical subgroups.
Our findings are consistent with, but extend, those from earlier studies on the impact of MA health reform on inpatient care by safety‐net status. Two previous studies that examined overall discharge volume between 2006 and 2009 found similar growth in safety‐net (1.8 percent) and nonsafety‐net hospitals’ volume (2.1 percent); however, the experience of the top two safety‐net hospitals differed considerably with one increasing by 6.7 percent and the other decreasing by 17.5 percent (Ku et al. 2011; Mohan et al. 2013). Compared to these studies, our study contrasted the temporal change in MA with that in states where reform did not occur. In addition, while the previous studies combined discharges for all age groups, we examined discharges for patients aged 18–64, the beneficiary group targeted by reform. Our finding of no volume changes across the entirety of all MA hospitals is consistent with the finding of another previous study based on comparison of a random sample of MA hospitals with a sample from a large number of other states using Agency for Healthcare Research & Quality National Inpatient Sample data; that study focused on changes in the first year after reform (2008), in contrast with a longer horizon in this study (2008–2010) (Kolstad and Kowalski 2012).
Extending prior research, our findings indicated no shifts in discharge volumes, neither for overall admissions, nor for almost all subgroups by patient sociodemographics and admission characteristics. We concede that the precision of estimates for many of the subgroups is poor (i.e., wide confidence intervals), thereby not ruling out substantial changes (Tables 3 and 4). This is likely the result of multiple factors: the relatively small subgroup share out of overall discharges, high variation in post‐reform volume changes across MA safety‐net hospitals, and our use of a relatively conservative model (fixed hospital effects) that only utilizes within‐hospital longitudinal changes to evaluate outcome changes associated with reform; this specification was chosen to adjust for systematic unobserved differences across hospitals that may influence hospital‐level differences in volumes (Cameron and Trivedi 2005; Frakt 2015). In related studies using the same data sources, we found that, following reform, use of selected high‐volume inpatient elective procedures increased among Hispanics and lower‐income‐area residents in MA (Hanchate et al. 2012), and the share of two of these procedures (knee and hip replacement) performed in safety‐net hospitals decreased by 1 percent (Hanchate et al. 2015). While indicative of the potential for shifts away from safety‐net hospitals, such shifts in selective cohorts have not been sizable enough to affect the overall discharge volumes.
There are several possible interpretations for the lack of a shift away from safety‐net hospitals. One prior study found that between 2005 and 2009, safety‐net community health clinics, those receiving federal grants, experienced a 31 percent jump in the number of patients that received primary care, even as the proportion of those uninsured dropped sizably following insurance expansion (Katz 2011; Ku et al. 2011). Reporting findings of a population level survey, that study noted that the majority of patients who received care at safety nets did so for convenience (79 percent) and affordability (74 percent), with only a minority (25 percent) reporting difficulty with access to care elsewhere. The authors also noted that preference for safety‐net clinics and hospitals may be for additional services provided, including transportation, insurance enrollment assistance, language assistance, and community outreach activities. This view is consistent with national evidence from other studies, based on Medicare utilization data, which point to disproportionately higher concentration of racial/ethnic minority and low‐income patients in a small number of hospitals, often bypassing more proximate higher volume alternatives (Jha et al. 2007, 2008; Losina et al. 2007).
A contrary interpretation is that despite gaining insurance coverage after reform, many beneficiaries continued to face other barriers in accessing nonsafety‐net care. One post‐reform statewide survey indicated that 20 percent of respondents reported difficulty in finding outpatient care providers who accepted their insurance (Long and Masi 2008). One explanation is that for the initial 3 years following reform, the four managed care organizations that were contracted by the state to provide Medicaid plans prior to reform were the only insurers to offer plans under Commonwealth Care, the MA exchange insurance; as such, even the newly insured were likely to be restricted largely to the network of providers who were contracted with these managed care organizations (Massachusetts Medical Society 2007; Lischko, Bachman, and Vangeli 2009). By 2008, 277,000 previously uninsured gained subsidized coverage, of which 178,000 were covered by Commonwealth Care, the state‐subsidized exchange insurance, and the remaining 99,000 obtained Medicaid coverage (Doonan and Tull 2010). As two‐thirds of this latter population, with income below 150 percent FPL, was previously enrolled in the state's Uncompensated Care Pool program, which provided care primarily through safety‐net providers, it is likely that many in this population continued to receive care within the same cohort of safety‐net affiliated providers, even under Commonwealth Care (Blue Cross Blue Shield Foundation of Massachusetts 2011b).
Due to preference or lack of access to alternative providers, demand for inpatient services from safety‐net hospitals was not adversely affected by reform. The impact on overall revenues of the safety‐net hospitals is unclear. Financial performance of many MA safety‐net hospitals deteriorated immediately following reform (Kowalczyk 2009; Syre 2009). An important component of the reform package was the transition from lump sum uncompensated care payments by the state to hospitals to providing subsidized individual coverage for low‐income enrollees; between 2007 and 2008, the state reduced uncompensated care funds from $620 million to $373 million. Evidence on whether reductions in uncompensated care payments were offset by increased payments via insurance claims is limited. A recent analysis of the financial performance of MA hospitals indicated that the net margins for most safety‐net and non‐safety‐net hospitals did not vary much following reform; however, for the two largest safety‐net hospitals (Boston Medical Center and Cambridge Health Alliance), net margins suffered significantly (Bazzoli and Clement 2014). In retrospect, a more potent threat for the safety‐net hospitals following reform was not the loss of newly insured patients to non‐safety‐net hospitals, but instead the potential of revenue loss arising from the sudden reductions in uncompensated care payments not matched by increased revenues through insurance claims (Blue Cross Blue Shield Foundation of Massachusetts 2011a). Looking forward, as safety‐net hospitals have adjusted to the realignment of revenue sources following reform, with a greater share coming from insurance claims, a policy concern is that their financial performance will remain vulnerable to changes in reimbursement rates for those covered by Medicaid and Commonwealth Choice, particularly in times of state fiscal austerity (Blue Cross Blue Shield Foundation of Massachusetts 2011b).
Limitations
We recognize several limitations of our study. First, the ability to isolate the impact of reform on utilization changes depends on the choice of comparison states; while we confirmed that patterns of utilization changes in all states were similar prior to reform, there may be other unobserved factors post‐reform that differentially affected MA and the comparison states. Second, as noted earlier, our estimates cannot rule out sizable changes in utilization for some of the subgroups by race‐ethnicity and admission acuity/severity; however, specification of hospital fixed effects, a likely source of this lack of precision, is important for controlling confounding arising from unobserved systematic hospital differences (Cameron and Trivedi 2005; Kolstad and Kowalski 2012; Frakt 2015). Third, a limitation of the administrative data sources is the inability to identify individuals who changed insurance status after reform and identify their other health care utilization.
Conclusions
Our study found no significant changes in the volume of admissions following MA reform at safety‐net hospitals among the overall population as well as among sociodemographic vulnerable subgroups, including Hispanics, blacks, and low‐income area residents. An implication of our findings of patients’ continued reliance on safety‐net hospital inpatient care is that with a disproportionately higher load of those insured with state subsidies, and of those who continue to remain uninsured, the financial viability of safety‐net hospitals will continue to be sensitive to the levels of reimbursement rates of the state‐subsidized coverage plans and supplemental funding.
Due to the similarity in the central features of the two reforms, the experience in MA is indicative of the likely impact of ACA on safety‐net hospitals nationwide (Ayanian 2012). The scale of impact on safety‐net hospitals may vary by state, depending on baseline differences in the size of the uninsured, size of the safety‐net infrastructure, state support, and provider availability. The stability of hospital volumes at safety‐net hospitals in MA may partly be due to the integration of inpatient and outpatient care services provided to the previously uninsured through the uncompensated care pool program. Also, while overall demand for inpatient care did not increase in MA, other states may experience sizable increases, due either to pent‐up demand, larger proportional increases in numbers of newly insured or identification of new need following increased access to outpatient care. Patient preference for safety‐net hospitals and narrow provider networks may limit diversion of inpatient care to non‐safety‐net hospitals, particularly for those on subsidized coverage (Andrulis and Siddiqui 2011); however, in meeting this continued demand, safety‐net providers may be financially vulnerable as they adjust to the realignment of reimbursement of care for those newly insured and the ways in which states compensate for care for those who remain uninsured.
Supporting information
Appendix SA1: Author Matrix.
Table A1: Average (quarterly) Growth Rate by Hospital and State Setting.
Table A2: Difference‐in‐Differences Checklist Performance.
Table A3: Test of Validity of Comparison Cohort: Difference‐in‐Difference Estimate of Net Change in MA versus Comparison States during Pre‐Reform Period.
Table A4: Correlation between Longitudinal Volume Change and Baseline Hospital Volume.
Table A5: Change (%) in Hospital Discharge Volume Associated with Health Reform by Alternative Choice of Safety‐Net Hospital Grouping.
Table A6: Pre/Post‐reform Comparison of Change in Bed Capacity between Massachusetts and Control States.
Acknowledgments
Joint Acknowledgement/Disclosure Statement: This research has been supported by NIH grants (1U01HL105342‐01, N. Kressin, PI; Rx Foundation, A. Hanchate and K. Lasser, PI and 1R01MD007705‐01, A. Hanchate, PI). Dr. Kressin is supported in part by a Senior Research Career Scientist award from the Department of Veterans Affairs, Health Services Research & Development Service (RCS 02‐066‐1). Dr. Amresh Hanchate had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The views expressed in this article are those of the authors and do not necessarily represent the views of the National Institutes of Health, Boston University, or Department of Veterans Affairs. The authors acknowledge receipt of state discharge data from the Center for Health Information and Analysis (Massachusetts), Pennsylvania Health Care Cost Containment Council, New York State Department of Health, and State of New Jersey Department of Health; these agencies, their agents and staff, bear no responsibility or liability for the results of the analysis, which are solely the opinion of the authors.
Disclosures: None of the authors have a conflict of interest.
Disclaimers: None.
This work has been presented previously at the Society of General Internal Medicine Annual Meetings, April 2013, at the American Health Association Quality of Care and Outcomes Research Annual Meetings, May 2013, at the Academy Health Annual Meetings, June 2013 and at the American Heart Association Scientific Sessions, Nov 2013. These presentations were given under the title: Impact of Massachusetts Health Reform on Hospitalizations, Length of Stay and costs of Inpatient Care: Does Safety‐Net Matter?
References
- Agency for Healthcare Research and Quality . 2010. Clinical Classifications Software (CCS) 2010. Rockville, MD: Department of Health and Human Services, Agency for Healthcare Research and Quality. [Google Scholar]
- American Hospital Association . 2014. AHA Annual Survey Database. Chicago, IL: AHA. [Google Scholar]
- Andrulis, D. P. , and Siddiqui N. J.. 2011. “Health Reform Holds Both Risks and Rewards for Safety‐Net Providers and Racially and Ethnically Diverse Patients.” Health Affairs 30 (10): 1830–6. [DOI] [PubMed] [Google Scholar]
- Ayanian, J. Z. 2012. “The Massachusetts Journey to Expand Health Insurance Coverage.” Journal of General Internal Medicine 27 (2): 139–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzoli, G. J. , and Clement J. P.. 2014. “The Experiences of Massachusetts Hospitals as Statewide Health Insurance Reform Was Implemented.” Journal of Health Care for the Poor and Underserved 25 (1 Suppl): 63–78. [DOI] [PubMed] [Google Scholar]
- Bertrand, M. , Duflo E., and Mullainathan S.. 2004. “How Much Should We Trust Differences‐in‐Differences Estimates?” Quarterly Journal of Economics 119(1): 249–275. [Google Scholar]
- Blue Cross Blue Shield Foundation of Massachusetts . 2011a. Lessons from the Implementation of Massachusetts Health Reform. Boston, MA. [Google Scholar]
- Blue Cross Blue Shield Foundation of Massachusetts . 2011b. Massachusetts Health Reform: A Five‐Year Progress Report. Boston, MA. [Google Scholar]
- Cameron, A. C. , and Trivedi P. K.. 2005. Microeconometrics: Methods and Applications. New York: Cambridge University Press. [Google Scholar]
- Chandra, A. , Gruber J., and McKnight R.. 2014. “The Impact of Patient Cost‐Sharing On Low‐Income Populations: Evidence from Massachusetts.” Journal of Health Economics 33: 57–66. [DOI] [PubMed] [Google Scholar]
- Chatterjee, P. , Joynt K. E., Orav E. J., and Jha A. K.. 2012. “Patient Experience in Safety‐Net Hospitals: Implications for Improving Care and Value‐Based Purchasing.” Archives of Internal Medicine 172 (16): 1204–10. [DOI] [PubMed] [Google Scholar]
- Cusano, D. , and Thomas A.. 2014. “Narrow Networks under the ACA: Financial Drivers and Implementation Strategies.” Health Affairs Blog. Available at http://healthaffairs.org/blog/2014/02/17/narrow-networks-under-the-aca-financial-drivers-and-implementation-strategies/. [Google Scholar]
- Dimick, J. B. , and Ryan A. M.. 2014. “Methods for Evaluating Changes in Health Care Policy: The Difference‐in‐Differences Approach.” Journal of the American Medical Association 312 (22): 2401–2. [DOI] [PubMed] [Google Scholar]
- Doonan, M. T. , and Tull K. R.. 2010. “Health Care Reform in Massachusetts: Implementation of Coverage Expansions and a Health Insurance Mandate.” The Milbank Quarterly 88 (1): 54–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein, A. , Taubman S., Wright B., Bernstein M., Gruber J., Newhouse J. P., Allen H., Baicker K., and Group O. H. S.. 2012. “The Oregon Health Insurance Experiment: Evidence from the First Year.” The Quarterly Journal of Economics 127 (3): 1057–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frakt, A. 2015. “Fixed vs. Random Effects (Or, How to Have Fun at a Party).” The Incidental Economist. Available at http://theincidentaleconomist.com/wordpress/fixed-vs-random-effects-or-how-to-have-fun-at-a-party/ [Google Scholar]
- Gruber, J. 2011. “Massachusetts Points the Way to Successful Health Care Reform.” Journal of Policy Analysis and Management 30 (1): 184–92. [Google Scholar]
- Hadley, J. , and Cunningham P.. 2004. “Availability of Safety Net Providers and Access to Care of Uninsured Persons.” Health Services Research 39 (5): 1527–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanchate, A. D. , Zhang Y., Felson D. T., and Ash A. S.. 2008. “Exploring the Determinants of Racial and Ethnic Disparities in Total Knee Arthroplasty: Health Insurance, Income, and Assets.” Medical Care 46 (5): 481–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanchate, A. D. , Lasser K. E., Kapoor A., Rosen J., McCormick D., D'Amore M. M., and Kressin N. R.. 2012. “Massachusetts Reform and Disparities in Inpatient Care Utilization.” Medical Care 50: 569–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanchate, A. D. , Kapoor A., Katz J. N., McCormick D., Lasser K. E., Feng C., Manze M. G., and Kressin N. R.. 2015. “Massachusetts Health Reform and Disparities in Joint Replacement Use: Difference in Differences Study.” British Medical Journal 350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources and Services Administration . 2014. User Documentation for the Area Resource File. Washington, DC: U.S. Department of Health and Human Services. [Google Scholar]
- Institute of Medicine . 2000. America's Health Care Safety Net: Intact but Endangered. Washington, DC: National Academy Press. [PubMed] [Google Scholar]
- Jha, A. K. , Fisher E. S., Li Z., Orav E. J., and Epstein A. M.. 2005. “Racial Trends in the Use of Major Procedures among the Elderly.” The New England Journal of Medicine 353 (7): 683–91. [DOI] [PubMed] [Google Scholar]
- Jha, A. K. , Orav E. J., Li Z., and Epstein A. M.. 2007. “Concentration and Quality of Hospitals That Care for Elderly Black Patients.” Archives of Internal Medicine 167 (11): 1177–929. [DOI] [PubMed] [Google Scholar]
- Jha, A. K. , Orav E. J., Zheng J., and Epstein A. M.. 2008. “The Characteristics and Performance of Hospitals That Care for Elderly Hispanic Americans.” Health Affairs 27 (2): 528–37. [DOI] [PubMed] [Google Scholar]
- Newhouse J. P., and Insurance Experiment Group . 1996. Free for All? Lessons from The RAND Health Insurance Experiment. Cambridge, MA: Harvard University Press. [Google Scholar]
- Katz, M. H. 2011. “Safety‐Net Providers and Preparation for Health Reform: Staff Down, Staff Up, Staff Differently.” Archives of Internal Medicine 171 (15): 1319–20. [DOI] [PubMed] [Google Scholar]
- Kolstad, J. T. , and Kowalski A. E.. 2012. “The Impact of Health Care Reform on Hospital and Preventive Care: Evidence from Massachusetts.” Journal of Public Economics 96 (11): 909–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kowalczyk, L. 2009. “BMC's Finances Taken Turn for Worse.” The Boston Globe. [Google Scholar]
- Ku, L. , Jones E., Shin P., Byrne F. R., and Long S. K.. 2011. “Safety‐Net Providers after Health Care Reform: Lessons from Massachusetts.” Archives of Internal Medicine 171 (15): 1379–84. [DOI] [PubMed] [Google Scholar]
- Lasser, K. E. , Hanchate A., McCormick D., Chu C., Xuan Z., and Kressin N. R.. In press. “Massachusetts Health Reform's Effect on Hospitals’ Racial Mix of Patients and on Patients’ Use of Safety‐Net Hospitals.” Medical Care. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lischko, A. M. , Bachman S. B., Vangeli A., and Commonwealth Fund . 2009. The Massachusetts Commonwealth Health Insurance Connector: Structure and Functions. Washington, DC: Commonwealth Fund. [PubMed] [Google Scholar]
- Long, S. K. , and Masi P. B.. 2008. Access to and Affordability of Care in Massachusetts as of Fall 2008: Geographic and Racial/Ethnic Differences. Massachusetts Health Reform Survey Policy Brief. Washington DC: Urban Institute. [Google Scholar]
- Losina, E. , Wright E. A., Kessler C. L., Barrett J. A., Fossel A. H., Creel A. H., Mahomed N. N., Baron J. A., and Katz J. N.. 2007. “Neighborhoods Matter: Use of Hospitals with Worse Outcomes Following Total Knee Replacement by Patients from Vulnerable Populations.” Archives of Internal Medicine 167 (2): 182–7. [DOI] [PubMed] [Google Scholar]
- Massachusetts Medical Society . 2007. “Physician Guide to Commonwealth Care/Choice.” Available at http://www.massmed.org/advocacy/key-issues/health-care-reform/mms-physician-guide-to-commonwealth-care/choice-%28pdf%29/
- McCormick, D. , Sayah A., Lokko H., Woolhandler S., and Nardin R.. 2012. “Access to Care after Massachusetts’ Health Care Reform: A Safety Net Hospital Patient Survey.” Journal of General Internal Medicine 27 (11): 1548–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormick, D. , Hanchate A. D., Lasser K. E., Manze M. G., Lin M., Chu C., and Kressin N. R.. 2015. “Effect of Massachusetts Healthcare Reform On Racial and Ethnic Disparities in Admissions to Hospital for Ambulatory Care Sensitive Conditions: Retrospective Analysis of Hospital Episode Statistics.” British Medical Journal 350: h1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, S. 2012. “The Effect of the Massachusetts Reform on Health Care Utilization.” Inquiry 49 (4): 317–26. [DOI] [PubMed] [Google Scholar]
- Mohan, A. , Grant J., Batalden M., and McCormick D.. 2013. “The Health of Safety Net Hospitals Following Massachusetts Health Care Reform: Changes in Volume, Revenue, Costs, and Operating Margins from 2006 to 2009.” The International Journal of Health Services 43 (2): 321–35. [DOI] [PubMed] [Google Scholar]
- Nasseh, K. , and Vujicic M.. 2013. “Health Reform in Massachusetts Increased Adult Dental Care Use, Particularly among the Poor.” Health Affairs 32 (9): 1639–45. [DOI] [PubMed] [Google Scholar]
- Ryan, A. M. , Burgess J. F. Jr, and Dimick J. B.. 2015. “Why We Should Not Be Indifferent to Specification Choices for Difference‐in‐Differences.” Health Services Research 50 (4): 1211–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . 2014. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP. [Google Scholar]
- Syre, S. 2009. “Looking for a Level Field.” The Boston Globe. [Google Scholar]
- Werner, R. M. , Goldman L. E., and Dudley R. A.. 2008. “Comparison of Change in Quality of Care between Safety‐Net and Non‐Safety‐Net Hospitals.” Journal of the American Medical Association 299 (18): 2180–7. [DOI] [PubMed] [Google Scholar]
- Wooldridge, J. M. 2002. Econometric Analysis of Cross‐Section and Panel Data. Cambridge, MA: The MIT Press. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table A1: Average (quarterly) Growth Rate by Hospital and State Setting.
Table A2: Difference‐in‐Differences Checklist Performance.
Table A3: Test of Validity of Comparison Cohort: Difference‐in‐Difference Estimate of Net Change in MA versus Comparison States during Pre‐Reform Period.
Table A4: Correlation between Longitudinal Volume Change and Baseline Hospital Volume.
Table A5: Change (%) in Hospital Discharge Volume Associated with Health Reform by Alternative Choice of Safety‐Net Hospital Grouping.
Table A6: Pre/Post‐reform Comparison of Change in Bed Capacity between Massachusetts and Control States.


