Abstract
Objective
To examine the effects of distance to dentists and dentist supply on dental services use among children with Medicaid coverage in Iowa.
Data Source
Iowa Medicaid claims for enrolled children between 2000 and 2009.
Study Design
The study sample included 41,554 children (providing 158,942 child‐year observations) who were born in Iowa between 2000 and 2006 and enrolled from birth in the Iowa Medicaid program. Children were followed through 2009. We used logistic regression to simultaneously examine the effects of distance (miles to nearest dentist) and county‐level dentist supply on a broad range of dental services controlling for key confounders. Additional models only used within‐child variation over time to remove unobservable time‐invariant confounders.
Principal Findings
Distance was related to lower utilization of comprehensive dental exams (2 percent lower odds per 1 mile increase in distance), an effect that also held in models using within‐child variation only. Dentist supply was positively related to comprehensive exams and other preventive services and negatively related to major dental treatments; however, these associations became smaller and insignificant when examining within‐child changes except for other preventive services.
Conclusions
Longer distance to dentists is a barrier for use of comprehensive dental exams, conditional on dentist supply.
Keywords: Dental care, oral health, Medicaid, prevention, dentist supply, dental workforce
Oral health is tightly linked with physical health and overall quality of life, especially for children (U.S. Department of Health and Human Services [DHHS] 2000). Despite widespread improvements in public health, including fluoridated water systems, dental caries remains the most common chronic disease among children. In fact, there are nearly five times as many children with caries as asthma, the second most common chronic disease among children (U.S. Department of Health and Human Services [DHHS] 2000). Nearly 37 percent of children ages 2–8 experienced dental caries in primary teeth in 2011–2012, including 56 percent for 6‐ to 8‐year olds (Dye et al. 2015).
Contributing factors to disparities in children's oral health are often separated into demand‐side and supply‐side or provider factors. Socioeconomic status, demographics, and dental insurance factor prominently in access to and utilization of dental care (Yu et al. 2002; Edelstein and Chinn 2009). Supply‐side factors receive relatively less attention but are no less important in terms of access to care. Availability of dental care professionals is a growing concern, particularly in areas with low populations. Over 5,000 geographic areas are designated as dental care health professional shortage areas (U.S. Department of Health and Human Services [DHHS] 2015a). Despite use of dental services increasing among children over the past decade (Vujicic and Nasseh 2014), the majority of children do not have a dental visit in a given year as recommended (American Academy of Pediatric Dentistry [AAPD] 2013). The concern is that longer distances to treatment and limited supply of dentists lead to significant disparities in access to dental care compared to more populated areas that feature both shorter distances to treatment and more dental professionals.
Recently, Guarnizo‐Herreno and Wehby (2014) investigated the relationship between supply of dentists and children's oral health at the national level and found that living in an area with more dentists improved oral health outcomes among children. Chi and Leroux (2012) reviewed county‐level determinants of dental utilization for children with chronic conditions in Iowa and found that professional shortage areas predict a lower likelihood of child dental care. Allison and Manski (2007) also showed that lower dentist supply is associated with fewer dental visits among adults. McKernan et al. (2015) studied associations between service area characteristics and receipt of preventive dental visits among Medicaid‐enrolled children and found few differences overall but significant differences in access for Hispanic children. Another descriptive study focusing on orthodontic services found that mean travel distance was higher in dental service areas with greater utilization rates (opposite to what is expected), but there was no child‐level analysis (McKernan et al. 2013).
Access to dental care overall, and preventive dental services in particular, is critical for children. Left untreated, tooth decay can lead to school absences and ultimately poor school performance (Guarnizo‐Herreno and Wehby 2012a) as well as significant psychosocial problems (Blumenshine et al. 2008; Jackson et al. 2011; Guarnizo‐Herreno and Wehby 2012a; Seirawan, Faust, and Mulligan 2012). Moreover, downstream health care costs may be significantly higher for untreated cases if decay leads to acute symptoms requiring treatment in a hospital or ambulatory setting (Kanellis, Damiano, and Momany 2000). By contrast, early treatment of dental caries has been shown to be beneficial. Beil et al. (2012) find that very young children with existing caries are less likely to need subsequent treatment when they have a preventive dental visit.
In this study we evaluate the effects of both proximity to dentists measured by driving distance in miles to the nearest dentist and dentist supply using county‐level measures of dental professionals per capita on the dental care utilization of Iowa children enrolled in Medicaid. Using a large sample and longitudinal data, we capture a wide set of dental care measures, including comprehensive exams, preventive care, and both minor and major dental treatments (e.g., fillings, crowns, etc.). To our knowledge, this is the first study to evaluate how differences in both individual proximity to dentists and supply of dentists affect children's access to several types of dental services. This study features a number of innovations compared to previous studies: In addition to the longitudinal setup of our analysis, we simultaneously examine driving distance and supply of dentists as well as multiple dental services and treatments. Our multivariate model approach controls for several potential confounders and evaluates changes for the same child over time to further account for unobservable confounding, such as child health problems and their severity which may impact use of dental services (Chi et al. 2011). Our work is very timely given the ongoing debate about future shortages of the dentist workforce and implications for access to care especially for states with large populations in rural areas (U.S. Department of Health and Human Services [DHHS] 2015a). As we show below, there is significant geographic variation in dentist availability and driving distance across counties in Iowa as well as changes in these indicators over the past decade. Understanding the implications of these changes for access to care addresses an important knowledge gap in the literature.
Methods
Study Population and Sample
Our study population included children born between 2000 and 2006 in Iowa who were enrolled in the Iowa Medicaid program since the month of their birth. All children were followed for at least the first 2 years of life and throughout their enrollment in Medicaid until the end of 2009. We included children who were continuously enrolled in Medicaid throughout their follow‐up time in the study to accurately capture use of dental services. In the first 2 years of life, children were excluded from the sample if they had more than a 1 month gap in Medicaid enrollment during the year. After the first 2 years, children who were not enrolled in Medicaid for over 60 consecutive days in a given year were excluded for those years. The shorter gaps were allowed because it is unlikely that children obtained dental services during those short periods and to retain a large and representative sample.
The total sample included 45,794 eligible children providing a total of 189,283 child‐year observations. Of those children, 34,512 (75.4 percent) were geocoded to street addresses in all of their follow‐up years. Two children were excluded because they had the same address as the nearest dentist. After all exclusions, the primary analytical sample included 34,510 children providing 137,014 child‐year observations with geocoded addresses for all their follow‐up years up to the 9th year of life (133 child‐year observations at 10th year of life were excluded to improve model fit). To examine the sensitivity of our results to restricting the sample to children with geocoded street addresses in all years, we also evaluate a less restrictive sample that includes children who have geocoded data for 1 or more years of follow‐up (41,554 children providing 158,942 child‐year observations).
Distance and Dentist Supply
We calculated driving distance in miles between the child's address in a given year of life (1st, 2nd, etc.) and nearest dentist of all dentists who have treated Medicaid patients in that year. Ten child address data files were available between October 2002 and July 2009. To generate a longitudinal dataset where the child is observed for each of their followed life years, we assigned for each child the most recent address prior to, or in the first month of, each of the child's years of life when possible.
We measured dentist supply at the county level for each year by the number of total general and pediatric dentists per 1,000 children (aged 15 years or younger). Data on dentists were obtained from the Iowa Health Professions Tracking Systems, a regularly updated database of all licensed and practicing dentists in Iowa (Kuthy et al. 2009). We obtained the annual child population count from the Area‐Resource‐File (U.S. Department of Health and Human Services [DHHS] 2014).
Dental Services
We examined a wide range of dental services based on CDT codes from the Medicaid claims involving dental visits following similar approaches to previous studies using Medicaid data (Chi et al. 2013; Beil et al. 2014). The outcomes were binary indicators for specific services. First, we evaluated all comprehensive dental exams (CDT codes D0150 and D0120), and then split the exams into separate indicators based on whether the exam was followed by a dental treatment within 91 days from the date of the exam. This distinction allows us to differentiate between primary and secondary/tertiary care. We also evaluated an indicator for other preventive care defined as receiving a prophylaxis, fluoride application, or dental sealants regardless of whether a comprehensive exam was provided or not. We examined three categories of dental treatments: major treatments (e.g., root canal treatment, crowns); tooth extractions; and minor treatments (e.g., surface fillings).
Statistical Analysis
We examined the effects of distance to the nearest dentist and dentist supply by including them simultaneously in the models for use of dental services. For each of the dental services, we estimated two types of logistic regression. The first model was a standard logistic regression that utilizes both between‐child variation as well as within‐child variation over time. In that model, we controlled for several potential confounders, including dummy variables for the child's year of life, median household income (county‐level), number of siblings covered under Medicaid, gender, and race/ethnicity. Because of repeated observations for each child, we estimated the standard errors clustering at the child level using a Huber‐type estimator (Wooldridge 2002).
One weakness of the above model is that it is potentially prone to bias from unobservable child‐level confounders such as household socioeconomic characteristics and parental preferences for dental care and child health. To account for such unobservable confounders, we estimated a second model that only compares each child to him or herself over time using conditional fixed‐effect logistic regression with fixed effects for each child (Wooldridge 2002). This model removes the influence of unobservable time‐invariant confounders at the child level and allows for causal inference in the absence of time‐varying unobservable confounders. Because it only uses within‐child variation over time, the model can only be estimated for children with changes in their outcome variables (i.e., use of dental services) over time. As such, children who never use a certain dental service in all their study years or who use that service every year are excluded from the model (because their outcomes do not vary over time). Therefore, the estimation sample size is smaller for this model than the total sample. Observable, time‐invariant child characteristics (e.g., gender or race/ethnicity) are also not included as covariates as their effects are accounted for by the child's fixed effects.
Because use of dental services varies by age and is much less frequent in the first 2 years of life (Figure S1), we examined additional models stratified by age. Because the conditional fixed‐effects logistic regression requires a fairly long panel of yearly child observations over time, we only estimated these stratified models using standard logistic regression using both between‐ and within‐child variation.
Results
Descriptive Analyses
Table 1 reports summary statistics for the dental service measures and the explanatory variables for the primary analytical sample of 34,510 unique children (137,014 child‐year observations). On average, about 22 percent of children had a comprehensive exam in a given year; most of the exams were not followed by treatment within 91 days. About 30 percent of children received other preventive services in the form of prophylaxis, fluoride application, or dental sealants. Among treatments, minor treatments were most common (about 6 percent of children per year) followed by major treatments (2.5 percent) and extractions (1.5 percent). On average, the nearest dentist was about 2 miles from a child and there were about two dentists treating children in Medicaid per 1,000 children. However, there was substantial variation in these measures both across counties and over time. Figure 1 shows average distance to the nearest dentist and dentists per capita across counties in 2009 in the study population and changes across counties from 2000 until 2009. Several counties had declines or little change in average distance, whereas others had an increase. Geographic differences and time changes are also observed for the number of dentists (bottom panel, Figure 1). These figures indicate substantial variation in the sample to examine the effects of distance and dentist supply on use of dental services in this population.
Table 1.
Sample Summary Statistics
| Variable | % or Mean (SD) |
|---|---|
| Outcomes (use of dental services) | |
| Any comprehensive evaluation* | 22.41 |
| Comprehensive evaluation without treatment* | 19.17 |
| Comprehensive evaluation with treatment* | 4.75 |
| Preventive care | 29.71 |
| Major treatment | 2.49 |
| Extraction | 1.51 |
| Minor treatment | 6.18 |
| Main independent variables | |
| Distance to nearest dentist (miles) | 1.92 (3.23) |
| County‐level dentists per 1,000 children | 2.11 (0.56) |
| Covariates | |
| County‐level median household income | 44,859.93 (5,995.71) |
| Number of siblings in Medicaid | 0.35 (0.61) |
| Female | 48.88 |
| Black | 7.60 |
| Hispanic | 10.41 |
| White | 51.05 |
| Other race | 3.74 |
| Unknown race | 27.20 |
Summary statistics for primary analytical sample of 137,014 child‐year observations based on 34,510 unique children (136,937 child‐year observations with gender data and 137,012 child‐year observations with county‐level data including dentist supply and median household income).
*The sum of the rate of any comprehensive exam without treatment within 91 days from the date of the exam and rate of any comprehensive exam with treatment within 91 days exceeds the rate of any comprehensive exam because two comprehensive exams in the same year, one without treatment within 91 days and the other with treatment, are counted only once in the indicator for any comprehensive exam. The summary statistics are rounded to two decimals.
Figure 1.
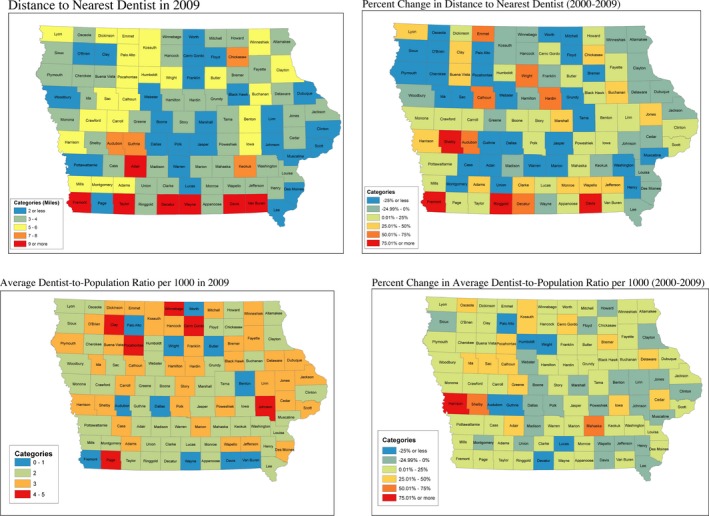
Average Distance to Nearest Dentist and Dentists (Treating Medicaid Children) per 1,000 Children across Iowa Counties in 2009 and Changes from 2000
Regression Results
Table 2 reports the estimates of the association of distance and dentist supply with use of dental services estimated from the two logistic regression models described above (detailed regression results are in Tables S1 and S2) for the primary analytical sample with address data for children. Starting with the standard logistic model that uses both between‐ and within‐child variation, we observe that an increase in distance to the nearest dentist is associated with a decline in the use of comprehensive exams (OR = 0.98; 95 percent CI: 0.98–0.99), specifically those not followed by treatment within 91 days. An increase in distance by 1 mile is associated with 2 percent lower odds of any comprehensive exam. However, there is no evidence that distance affected any of the other dental services in that model. Dentist supply is positively related to use of comprehensive exams not followed by treatment (OR = 1.17; 95 percent CI: 1.13–1.21), other preventive care (a prophylaxis, fluoride application, or dental sealants; OR = 1.1; 95 percent CI: 1.07–1.14), and to a decline in use of major treatments (OR = 0.89; 95 percent CI: 0.83–0.96). An increase by 1 dentist per 1,000 children is associated with a 17 percent increase in odds of comprehensive exams without treatment, 10 percent increase in odds of other preventive care, and 11 percent decline in odds of major treatments.
Table 2.
Logistic Regression Estimates (Odds Ratios and 95% CIs) for Use of Dental Services in Primary Analytical Sample
| Comprehensive Exam | Comprehensive Exam without Treatment within 91 days | Comprehensive Exam with Treatment within 91 days | Other Preventive Services | Major Treatment | Extraction | Minor Treatment | |
|---|---|---|---|---|---|---|---|
| Standard Logistic Regression | |||||||
| Distance | 0.98*** | 0.98*** | 1.00 | 1.00 | 1.00 | 0.99 | 1.01 |
| [0.98,0.99] | [0.98,0.99] | [0.99,1.01] | [0.99,1.01] | [0.99,1.01] | [0.98,1.01] | [1.00,1.01] | |
| Dentist supply | 1.16*** | 1.17*** | 1.01 | 1.10*** | 0.89*** | 0.97 | 0.99 |
| [1.12,1.20] | [1.13,1.21] | [0.96,1.07] | [1.07,1.14] | [0.83,0.96] | [0.89,1.07] | [0.94,1.04] | |
| N | 136,935 | 136,935 | 136,935 | 136,935 | 136,935 | 136,935 | 136,935 |
| Conditional Logistic Regression with Child Fixed Effects | |||||||
| Distance | 0.98** | 0.99 | 0.99 | 0.99* | 1.00 | 0.97 | 1.00 |
| [0.97,1.00] | [0.98,1.00] | [0.96,1.01] | [0.97,1.00] | [0.97,1.04] | [0.93,1.01] | [0.97,1.02] | |
| Dentist supply | 1.06 | 1.06 | 1.06 | 1.09* | 0.97 | 1.10 | 1.13 |
| [0.97,1.16] | [0.96,1.16] | [0.91,1.24] | [1.00,1.20] | [0.79,1.20] | [0.85,1.42] | [0.98,1.30] | |
| N | 76,069 | 70,409 | 28,322 | 88,798 | 16,917 | 11,753 | 34,767 |
95% CIs are in brackets. N indicates the number of child‐year observations included in the regressions. As noted above, N varies between outcomes in the conditional logit model because only children with variation in the outcome over time are included. The ORs and CIs are rounded to two decimals.
*p < .1; **p < .05; ***p < .01.
Turning next to the conditional fixed‐effect logit model which only uses within‐child variation over time, we observe that distance is still negatively related to receiving a comprehensive exam (OR = 0.98; 95 percent CI: 0.97–1.00), although we find no statistically significant effects when separating by whether a treatment was received within 91 days from the exam or not. The effect on any comprehensive exam is similar to that from the standard model, suggesting no major bias from unobservable time‐invariant child‐level factors for this outcome. Furthermore, we observe a marginally significant decline in receiving other preventive services in this model (OR = 0.99; 95 percent CI: 0.97–1.00), but do not find significant effects on treatments. In contrast to the standard model, the effects of dentist supply on comprehensive exams and major treatments are remarkably smaller in the conditional logit model and insignificant, suggesting that dentist supply associations in the standard model are confounded by other county‐level factors. The only exception is the effect on use of other preventive care which is marginally significant and of similar magnitude, indicating an improvement in this outcome with an increase in dentist supply.
Sensitivity Checks
As noted above, we also examined the models in a less restrictive and larger sample including children for any year with address data without requiring that they have data on all their follow‐up years (Table S3). We observe overall similar results as in the primary sample. The only notable exceptions in the conditional logit model are that the distance effect on comprehensive exams is significant for those not followed by treatment (within 91 days) with null effect for those followed by treatment (similar to the standard model) and that dentist supply is positively related to minor treatments (relatively similar effect to primary sample but now statistically significant). Also, the decline in the likelihood of extractions with greater distance became marginally significant (previously insignificant in the main sample). Overall, however, the main inference is unchanged in this sample.
Estimates by Age
The first age‐specific model we estimated was for receiving any comprehensive exam during the first 2 years of life. Comprehensive examination is recommended beginning in the first year of life (American Academy of Pediatric Dentistry [AAPD] 2013). However, <1 percent of our sample had this evaluation in first year of life (~11 percent in 2nd year). We found a similar association for distance as in the full sample (OR = 0.98; 95 percent CI: 0.97–0.99), but a stronger positive association for dentist supply (OR = 1.29; 95 percent CI: 1.22–1.36).
Next, we estimated models for all dental services for children aged 3–5 years and children aged 6–9 years (Table 3). Interestingly, we observed overall similar associations among children aged 3–5 years as in the full sample, with the exception of a significant decline in extractions as distance increased. In contrast, we found that distance and dental supply had an insignificant effect on use of dental services for children 6–9 years with the exception of an increase in other preventive services with more dentists.
Table 3.
Standard Logistic Regression Estimates (Odds Ratios and 95% CIs) for Use of Dental Services by Age
| Comprehensive Exam | Comprehensive Exam without Treatment within 91 days | Comprehensive Exam with Treatment within 91 days | Other Preventive Services | Major Treatment | Extraction | Minor Treatment | |
|---|---|---|---|---|---|---|---|
| Age 3–5 | |||||||
| Distance | 0.98*** | 0.98*** | 0.99 | 1.00 | 1.00 | 0.98** | 1.01 |
| [0.98,0.99] | [0.98,0.99] | [0.98,1.00] | [0.99,1.00] | [0.98,1.01] | [0.95,1.00] | [1.00,1.01] | |
| Dentist supply | 1.10*** | 1.11*** | 1.00 | 1.06*** | 0.91** | 1.00 | 0.97 |
| [1.06,1.14] | [1.07,1.15] | [0.94,1.06] | [1.02,1.10] | [0.85,0.99] | [0.89,1.12] | [0.92,1.03] | |
| N | 63,356 | 63,356 | 63,356 | 63,356 | 63,356 | 63,356 | 63,356 |
| Age 6–9 | |||||||
| Distance | 0.99 | 0.99 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| [0.98,1.00] | [0.98,1.00] | [0.98,1.01] | [0.99,1.01] | [0.98,1.02] | [0.98,1.02] | [0.99,1.02] | |
| Dentist supply | 1.01 | 1.00 | 1.02 | 1.12*** | 0.97 | 1.02 | 1.04 |
| [0.94,1.07] | [0.94,1.07] | [0.95,1.10] | [1.04,1.20] | [0.87,1.08] | [0.92,1.14] | [0.96,1.11] | |
| N | 18,473 | 18,473 | 18,473 | 18,473 | 18,473 | 18,473 | 18,473 |
95% CIs are in brackets. The ORs and CIs are rounded to two decimals.
**p < .05; ***p < .01.
Discussion
We evaluated the effects of both child‐level distance to the nearest dentist and dentist supply on use of dental services for children enrolled in Medicaid in Iowa. We found evidence that increased distance to the nearest dentist is associated with a decrease in likelihood of a comprehensive exam. A 1 SD increase in distance (about 3.3 miles) equates to a decrease of about 6 percent in the odds of a comprehensive exam. Our results do not show distance to be a significant factor for other dental services, however. We also found weaker evidence for a positive relationship between supply of dentists and comprehensive exams. The odds of a comprehensive exam increase by 17 percent with an additional dentist per 1,000 children. However, when evaluating the effect of dentist supply using variation for the same child over time, the effect diminishes, suggesting that dentist supply is possibly confounded with other county‐level factors related to dental services use, which may include social and economic conditions (Quinn, Catalano, and Felber 2009; Guarnizo‐Herreno and Wehby 2012b). The exception is for other preventive services, in which case dentist supply continues to show an effect. These results are consistent with previous studies reporting a positive association between dentist supply and use of preventive dental care using state‐level data (e.g., Lin et al. 2012 ), and that such association becomes less prominent after adjusting for additional state‐level characteristics (Guarnizo‐Herreno and Wehby 2014).
To further characterize the impact of distance and dentist supply on use of dental services, we stratified our analyses by age group. We found the strongest associations with both distance and dentist supply for younger children ages 3–5. Dental problems are overall less severe among younger children, and some parents may downplay the importance of primary (i.e., “temporary”) teeth, which may lead some parents to consider the use of dental care as discretionary, making it more sensitive to supply‐side factors. Guarnizo‐Herreno and Wehby (2014), in assessing the effects of dentist supply nationally, also find that the oral health of younger children (grouped as those aged 1–10 years in their study) is much more sensitive to dental supply than older children. Our results are generally consistent with theirs, but suggest further heterogeneity among young children in that use of dental services is most sensitive to geographic barriers prior to school entry. Whether requiring dental screening prior to school entry reduces the importance of supply‐side factors for subsequent use of dental services among younger children is an important question for future research. In 2008, the state of Iowa began requiring screenings prior to the school year for children ages 3–6 (Iowa Department of Public Health [IDPH] 2015). Individual school districts may have had similar requirements in place prior to the state requirement. It is possible that the effects we observe among younger children would have been even more pronounced without such requirements.
These findings carry important policy implications. Across a relatively rural state like Iowa, child‐level geographic proximity, in this case distance to the nearest dentist, plays a role in use of comprehensive dental screenings, particularly for younger children, conditional on the number of dentists in the county. In the models that remove as many of the confounders as possible (conditional logit), we find that individual distance matters more for comprehensive examinations than dentist supply. This finding offers insights for designing policies and interventions to address geographic barriers to dental care and shortfalls in preventive dental care. Identifying and lowering time and travel costs to dentists for families is a more relevant target than the goal of simply increasing the number of dentists in a given area (e.g., county) as not all dentists will be equally accessible distance‐wise to the majority of children in that area. In the same vein, policies that address geographic disparities through incentives that encourage dental professionals to practice in underserved locales would be well served to focus on average distance to dentists for residents rather than per capita dentists, although both factors ultimately play a role.
Our study has several strengths, including the large sample, longitudinal data, objective measures of dental use, and utilizing within‐child variation over time to remove time‐invariant confounders. It also has some caveats that can be considered in future research. Despite the richness of the data, an inherent challenge in using administrative datasets like Medicaid claims is not being able to fully disentangle dental health from use of dental services. Future studies that examine the effects of geographic proximity on dental health outcomes would be particularly useful to further understand the implications of geographic barriers for children's oral health. We also focus on children in Medicaid in Iowa. Examining the generalizability to non‐Medicaid children including those with and without private dental insurance and to nationally representative samples is also important due to the existence of racial/ethnic, socioeconomic, and geographic disparities in dental health and use of dental services (Lewis et al. 2007; Liu et al. 2007; Guarnizo‐Herreno and Wehby 2012b).
Supporting information
Appendix SA1: Author Matrix.
Table S1: Odds Ratios (and 95% CIs)—Standard Logit in Main Sample.
Table S2: Odds Ratios (and 95% CIs)—Conditional Logit in Main Sample.
Table S3: Logistic Regression Estimates (Odds Ratios and 95% CIs) for Use of Dental Services from Sensitivity Check Models Using Less Restrictive Sample.
Figure S1: Use of Dental Services by Age in Study Population.
Acknowledgments
Joint Acknowledgement/Disclosure Statement: This work was supported by Grant 5RC 1 DE020303 from the National Institute of Dental and Craniofacial Research.
Disclosures: None.
Disclaimers: None.
References
- Allison, R. A. , and Manski R. J.. 2007. “The Supply of Dentists and Access to Care in Rural Kansas.” Journal of Rural Health 23 (3): 198–206. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatric Dentistry (AAPD) . 2013. “Guideline on Periodicity of Examination, Preventive Dental Services, Anticipatory Guidance/Counseling, and Oral Treatment for Infants, Children, and Adolescents.” Pediatric Dentistry 35 (5): E148–56. [PubMed] [Google Scholar]
- Beil, H. , Rozier R. G., Preisser J. S., Stearns S. C., and Lee J. Y.. 2012. “Effect of Early Preventive Dental Visits on Subsequent Dental Treatment and Expenditures.” Medical Care 50 (9): 749–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beil, H. , Rozier R. G., Preisser J. S., Stearns S. C., and Lee J. Y.. 2014. “Effects of Early Dental Office Visits on Dental Caries Experience.” American Journal of Public Health 104 (10): 1979–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenshine, S. L. , Vann W. F. Jr, Gizlice Z., and Lee J. Y.. 2008. “Children's School Performance: Impact of General and Oral Health.” Journal of Public Health Dentistry 68 (2): 82–7. [DOI] [PubMed] [Google Scholar]
- Chi, D. L. , and Leroux B.. 2012. “County‐Level Determinants of Dental Utilization for Medicaid‐Enrolled Children with Chronic Conditions: How Does Place Affect use?” Health Place 18 (6): 1422–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi, D. L. , Momany E. T., Neff J., Jones M. P., Warren J. J., Slayton R. L., Weber‐Gasparoni K., and Damiano P. C.. 2011. “Impact of Chronic Condition Status and Severity on the Time to First Dental Visit for Newly Medicaid‐Enrolled Children in Iowa.” Health Services Research 46 (2): 572–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi, D. L. , Momany E. T., Jones M. P., Kuthy R. A., Askelson N. M., Wehby G. L., and Damiano P. C.. 2013. “Relationship between Medical Well Baby Visits and First Dental Examinations for Young Children in Medicaid.” American Journal of Public Health 103 (2): 347–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye, B. A. , Thornton‐Evans G., Li X., and Iafolla T. J.. 2015. “Dental Caries and Sealant Prevalence in Children and Adolescents in the United States, 2011‐2012.” NCHS Data Brief, no. 191, pp. 1–8. [PubMed] [Google Scholar]
- Edelstein, B. L. , and Chinn C. H.. 2009. “Update on Disparities in Oral Health and Access to Dental Care for America's Children.” Academic Pediatric 9 (6): 415–9. [DOI] [PubMed] [Google Scholar]
- Guarnizo‐Herreno, C. C. , and Wehby G. L.. 2012a. “Children's Dental Health, School Performance, and Psychosocial Well‐Being.” Journal of Pediatrics 161 (6): 1153–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarnizo‐Herreno, C. C. , and Wehby G. L.. 2012b. “Explaining Racial/Ethnic Disparities in Children's Dental Health: A Decomposition Analysis.” American Journal of Public Health 102 (5): 859–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guarnizo‐Herreno, C. C. , and Wehby G. L.. 2014. “Dentist Supply and Children's Oral Health in the United States.” American Journal of Public Health 104 (10): e51–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iowa Department of Public Health (IDPH) . 2015. “School Dental Screenings” [accessed on December 01, 2015]. Available at http://www.idph.iowa.gov/ohds/oral-health-center/school-screenings
- Jackson, S. L. , Vann W. F. Jr, Kotch J. B., Pahel B. T., and Lee J. Y.. 2011. “Impact of Poor Oral Health on Children's School Attendance and Performance.” American Journal of Public Health 101 (10): 1900–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanellis, M. J. , Damiano P. C., and Momany E. T.. 2000. “Medicaid Costs Associated with the Hospitalization of Young Children for Restorative Dental Treatment under General Anesthesia.” Journal of Public Health Dentistry 60 (1): 28–32. [PubMed] [Google Scholar]
- Kuthy, R. A. , McKernan S. C., Hand J. S., and Johnsen D. C.. 2009. “Dentist Workforce Trends in a Primarily Rural State: Iowa: 1997‐2007.” Journal of the American Dental Association 140 (12): 1527–34. [DOI] [PubMed] [Google Scholar]
- Lewis, C. W. , Johnston B. D., Linsenmeyar K. A., Williams A., and Mouradian W.. 2007. “Preventive Dental Care for Children in the United States: A National Perspective.” Pediatrics 119 (3): e544–53. [DOI] [PubMed] [Google Scholar]
- Lin, M. , Sappenfield W., Hernandez L., Clark C., Liu J., Collins J., and Carle A. C.. 2012. “Child‐ and State‐Level Characteristics Associated with Preventive Dental Care Access among U.S. Children 5‐17 Years of Age.” Maternal and Child Health Journal Supplement 2: 320–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, J. , Probst J. C., Martin A. B., Wang J. Y., and Salinas C. F.. 2007. “Disparities in Dental Insurance Coverage and Dental Care among US Children: The National Survey of Children's Health.” Pediatrics 119 (S1): S12–21. [DOI] [PubMed] [Google Scholar]
- McKernan, S. C. , Kuthy R. A., Momany E. T., McQuistan M. R., Hanley P. F., Jones M. P., and Damiano P. C.. 2013. “Geographic Accessibility and Utilization of Orthodontic Services among Medicaid Children and Adolescents.” Journal of Public Health Dentistry 73 (1): 56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKernan, S. C. , Kuthy R. A., Hanley P. F., Jones M. P., Momany E. T., McQuistan M. R., and Damiano P. C.. 2015. “Geographic Variation of Dental Utilization among Low Income Children.” Health Place 34: 150–6. [DOI] [PubMed] [Google Scholar]
- Quinn, B. C. , Catalano R. A., and Felber E.. 2009. “The Effect of Community‐Level Unemployment on Preventive Oral Health Care Utilization.” Health Services Research 44 (1): 162–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seirawan, H. , Faust S., and Mulligan R.. 2012. “The Impact of Oral Health on the Academic Performance of Disadvantaged Children.” American Journal of Public Health 102 (9): 1729–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (DHHS) . 2000. “Oral Health in America: A Report of the Surgeon General” [accessed on October 22, 2015]. Available at http://silk.nih.gov/public/hck1ocv.@www.surgeon.fullrpt.pdf
- U.S. Department of Health and Human Services (DHHS) . 2014. “Health Resources and Services Administrations. Area Health Resources Files” [accessed on December 4, 2014]. Available at http://ahrf.hrsa.gov/
- U.S. Department of Health and Human Services (DHHS) . 2015a. “Shortage Designation: Health Professional Shortage Areas & Medically Underserved Areas/Populations” [accessed on October 22, 2015]. Available at http://www.hrsa.gov/shortage/
- U.S. Department of Health and Human Services (DHHS), Health Resources and Services Administration, National Center for Health Workforce Analysis . 2015b. “National and State‐Level Projections of Dentists and Dental Hygienists in the U.S., 2012‐2025” [accessed on December 01, 2015]. Available at http://bhpr.hrsa.gov/healthworkforce/supplydemand/dentistry/nationalstatelevelprojectionsdentists.pdf
- Vujicic, M. , and Nasseh K.. 2014. “A Decade in Dental Care Utilization among Adults and Children (2001‐2010).” Health Services Research 49 (2): 460–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge, J. M. 2002. Econometric Analysis of Cross Section and Panel Data, 2d Edition Cambridge, MA: MIT Press. [Google Scholar]
- Yu, S. M. , Bellamy H. A., Kogan M. D., Dunbar J. L., Schwalberg R. H., and Schuster M. A.. 2002. “Factors That Influence Receipt of Recommended Preventive Pediatric Health and Dental Care.” Pediatrics 110 (6): e73. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1: Odds Ratios (and 95% CIs)—Standard Logit in Main Sample.
Table S2: Odds Ratios (and 95% CIs)—Conditional Logit in Main Sample.
Table S3: Logistic Regression Estimates (Odds Ratios and 95% CIs) for Use of Dental Services from Sensitivity Check Models Using Less Restrictive Sample.
Figure S1: Use of Dental Services by Age in Study Population.


