Abstract
Objectives
To examine the acceptability of yoga research tailored to recruit and retain a minority population (both English and Spanish speaking) with arthritis. Yoga research for arthritis often underrepresents minorities and acceptability for this population has not previously been investigated.
Design
Acceptability was evaluated using retention, adherence, journals, and semi-structured exit interviews from twelve participants with osteoarthritis or rheumatoid arthritis undergoing an 8-week yoga intervention. Journal quotes were analyzed using content analysis techniques. NVivo software was used to organize transcripts and assemble themes. Two methods of triangulation (data and investigator) were used to overcome potential bias from a single-perspective interpretation. Exit interview comments were content analyzed using a card sort method. The study was designed with a cultural infrastructure including a multicultural research team, translators, and bilingual materials and classes, to facilitate trust and acceptability for primarily Hispanic and Black/African-American adults.
Setting
Washington, D.C. metropolitan area, USA.
Results
On average participants attended 10 of 16 classes, with home practice 2–3 days a week. All who completed were still practicing yoga three-months later. Qualitative narrative analysis identified major themes related to facilitating factors and barriers for yoga practice, self-efficacy, and support. Participant comments indicated that offering an arthritis-based yoga intervention and using a culturally congruent research design was found to be acceptable.
Conclusions
As yoga research grows, there is a need to understand and promote acceptability for typically under-represented populations. This study attempts to inform the expansion of multicultural research designed to recruit and retain those from diverse backgrounds.
Keywords: Osteoarthritis, Rheumatoid arthritis, Yoga, Minority, Bilingual, Qualitative, Journals, Narratives
1. Introduction
There is promising evidence that yoga may be a safe and beneficial intervention for both osteoarthritis (OA) and rheumatoid arthritis (RA).1–3 A limitation of the existing yoga research is the under-representation of diverse and minority populations. Lifetime yoga practitioners are more likely female, younger, non-Hispanic white, college educated, higher earners, and have better health status than non-practitioners.4 The perspective of this group tends to be more heavily represented in yoga research. Hispanic and non-Hispanic Blacks are increasingly using yoga in the US.5 While a few articles in the literature6–9 found that when exposed to yoga practices, diverse populations benefit from these practices, anticipate using them in everyday life, report greater self-efficacy in pain management, increased body awareness, and a stronger mind-body connection; none of the articles were specifically related to minority populations with arthritis.
In order for an intervention to be used by participants, they must find it to be acceptable. Acceptability can be influenced by values and perceptions related to ethnicity, culture, education, and personal experience.10 This study was created to evaluate the feasibility and acceptability for a yoga intervention in a convenience sample of minority patients (either English or Spanish speaking) receiving rheumatology care at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) Community Health Clinic (CHC) in a racially diverse area of the Washington, DC metro region.10 Patients are referred to the rheumatology clinic from other neighborhood health centers, clinics, or practices in the area and care is provided without regard to medical insurance status.11 Acceptability was evaluated by using retention and adherence indicators as well as participant narratives collected from three sources: 1) weekly journals, 2) semi-structured exit interviews, and 3) field notes.
1.1. Sociocultural considerations within clinical research
Traditional “gold standards” research processes may not be effective for ethnic minority populations.12 Documented barriers to research include fear of unintended outcomes, language barriers, childcare, lack of transportation, legal status, and competing demands.12 Specifically, within African American communities, mistrust has been historically documented as a significant factor affecting recruitment and retention.13 For this study, cultural values such as allocentrism or collectivism (emphasizing the group rather than oneself) and familialism or familismo (strong identification with, feelings of loyalty, and attachment to family) were thought to potentially impact the recruitment of Hispanic participants. Under the concept of simpatía,14 small talk was used when appropriate to build rapport, facilitate cooperation, and build trusting relationships between the researchers and participants.
The most commonly articulated facilitators for minority participation in health research has been to include culturally congruent study designs, altruism, and emphasis on the convenience of participation.12 For some within the African American community additional facilitating factors include safety assurances; trust in the researcher and reputation of the research institution, and the inclusion of diverse racial and ethnic groups.12 These were incorporated when designing the research study. It was hypothesized that by including bilingual, culturally relevant recruitment materials, researchers, and yoga instructors; participants would be more willing to enroll. Also that retention would be enhanced by offering a bilingual, community-based, arthritis-based yoga intervention, and classes with others living with arthritis.10 The underlying premise being that if attention was paid to incorporate cultural aspects into the study design, yoga would be acceptable to minority persons with arthritis. This paper describes a study design developed to overcome potential barriers, positively influence recruitment and retention, and to facilitate trust. Additionally, it contributes to the body of literature advocating for research designed from a multi-cultural framework.15
2. Methods
2.1. Designing the study
Rheumatology and rehabilitation medicine clinicians with prior clinical experience with this population served as key informants when designing the study. The yoga study is a follow-up intervention to a descriptive study by Wallen et al. examining the diverse health beliefs and behaviors among primarily African-American and Hispanic patients receiving rheumatology care from the same NIAMS CHC.16,17 The Wallen study highlighted the importance of cultural compatibility in research through the comment from one participant, “Where are the people who look like me?” This comment served as a reminder of the importance of the creation of a research team which reflected the diverse cultural background of the study population. A multicultural research team was assembled which included Black (American, West African and West Indian), bilingual (from Central and South America, Mexico, and Puerto Rico), and non-minority researchers and clinicians.
Two bicultural interpreters18 were hired as research assistants to assist with language and cultural barriers. Their cultural understanding helped to maintain research integrity and negotiate concepts not easily translated between languages; which most likely enhanced the willingness of participants to respond and enroll onto the study.18,19 Both participated in recruitment and enrollment, translated in all yoga classes, and provided follow-up calls as needed, to provide a sense of continuity.
The study used Hatha yoga and follows the format of a previous randomized research study Yoga for Arthritis, conducted through Johns Hopkins University.1 Bilingual yoga classes were held for 60 min biweekly, over an eight week period, at a yoga studio in Washington, DC. Classes included deep breathing, relaxation, meditation, poses for strength, flexibility, and balance. Additional details can be found in the protocol article.10 Participants were encouraged to develop a home practice based on poses taught during each yoga class. All participants received yoga equipment and bilingual manuals with pictures of the poses to facilitate home practice.
2.2. Recruitment and data collection
Patients were referred by rheumatology and physical rehabilitation medicine clinicians, who were already familiar with their care. All patients enrolled onto the study were medically cleared to participate in light to moderate exercise, were 18 years of age or older, and had a diagnosis of either osteoarthritis or rheumatoid arthritis. Detailed eligibility criteria can be found in the protocol article.10 Approval to conduct the study was obtained through the National Institute of Diabetes and Digestive and Kidney Disease (NIDDK)/National Institute of Arthritis and Musculoskeletal and Skin Disease’s (NIAMS) intramural institutional review board (IRB).
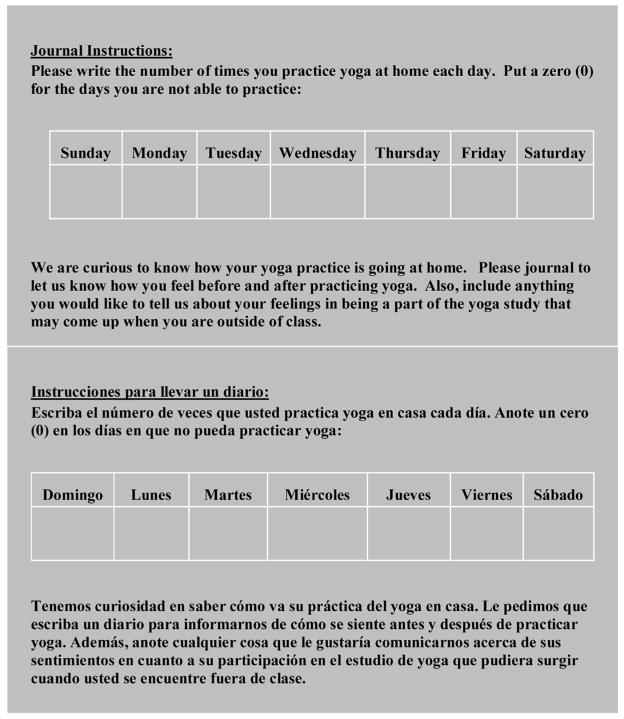
Personal journals and semi-structured open-ended exit interviews were selected to ensure the participant’s perspectives were effectively captured. This methodology encouraged a dialog which allowed for the discovery of new themes, as opposed to closed survey questions that might limit participant responses. A qualitative approach was viewed as a less intimidating approach to give a voice to those typically under-represented in research.20 Bilingual journals (Fig. 1) were used to record the frequency and duration of home practice sessions, and observations while on the study. Narratives21 were used to capture participant perspectives, beliefs, and motivations underlying their participation in the study. Spanish narratives were translated and transcribed into English by the research assistants, then verified using team translation. Team translation provided the opportunity to clarify meaning over verbatim translation, to minimize bias;14 and to provide more succinct translations. For example the journal entry, “Me gustaria tener mas energia y animo” was originally translated as “I would like to have more energy and motivation”. A second native speaker suggested “motivation” was adequate for animo but it could be more precise to use “drive,” “spirit,” or “liveliness.”
Fig. 1.
Sample Journal Instructions.
Semi-structured exit interviews were conducted, in English and Spanish, regarding: i) opinions of yoga classes and location; and ii) perceptions of class design (bilingual, multi-ethnic teachers, classes with others with arthritis); iii) willingness to recommend yoga classes; iv) viewing yoga as self-care for arthritis; v) likelihood of continuing yoga practice. Field notes and observational data were collected during the interview process, while attending yoga classes, and after any contact with participants outside of the yoga classes.
2.3. Data analysis
Journals were analyzed using content analysis techniques. An audit trail22 was maintained through written documentation of the group process. NVivo (version 10) electronic database was used to organize transcripts and assemble themes.23 Two methods of triangulation24 were used to overcome the potential bias from using a single-perspective interpretation: 1) data triangulation was used when more than one source of data (journals and interviews, or quantitative) was available to evaluate the same phenomenon; and 2) investigator triangulation used several evaluators to review themes.24
Analyses and validation were conducted in three stages. In stage 1, two researchers (SHM and GTA) each independently coded using inductive analysis. Using an iterative coding process, stage 1 results were discussed with additional members of the research team (KRM, MML, and GW) until consensus was achieved and saturation of themes was reached. In stage 2, an independent coder evaluated quotes. Her feedback led to a reevaluation of some themes by the team. Finally for stage 3, credibility22 was established through the rheumatologist’s (MW) evaluation of themes and perspective of the portrayal of participant quotes based upon clinical experience with the patient population. Suggestions from each stage were incorporated into the selection of the final themes.
Since exit interview responses were from open-ended questions, as opposed to the journal entries, these were content analyzed using a cutting and sorting (card sort) method.25 Responses were categorized as elaborating on survey questions, mapping to existing journal themes, or identifying unique themes. Field notes were added, when needed, to clarify participant comments.
3. Results
Baseline assessments (n = 30) of enrollees indicated an average age of 50 years (range 32–69), mostly Hispanic (70%) or Black/African American (17%), female (93%), and Spanish speaking (69%). The larger percentage of those enrolled were diagnosed with RA (90%). Spanish speaking participants were mostly from El Salvador; other countries in Central America, South America, and Mexico. Acculturation was measured using length of time in US (average 17 years) and a self-reported measure of English language proficiency.14 Self-report indicated only 13% did not speak any English. The baseline pain intensity scores, shown in selected quotes, were assessed using a 10 point scoring system (0-no pain to 10-worst pain imaginable).26
3.1. Acceptability
The following information was collected to better understand recruitment, retention, and adherence. Of the 59 patients referred, 30 (51%) were enrolled. Reasons for refusals included: too busy (34%), not interested (21%), classes too far away (21%), transportation issues (14%), childcare issues (10%). Yoga classes were offered as a group intervention, therefore scheduling was driven by the ability to create a cohort who could attend classes during the same times. Participants remained on a waiting list until a suitable cohort was formed. The start of the intervention was determined by attending the first yoga class; 60% of those enrolled met criteria. Of the 18 participants who started the intervention, 12 completed. Comparable to the previous Yoga for Arthritis study9 attrition was highest prior to the first class (while waiting for a cohort to form). Those who completed on average attended 10 out of 16 classes. Home practice averaged 2–3 days a week for approximately 20 min each day. Three-months after completing the intervention all who completed the protocol were still practicing yoga.
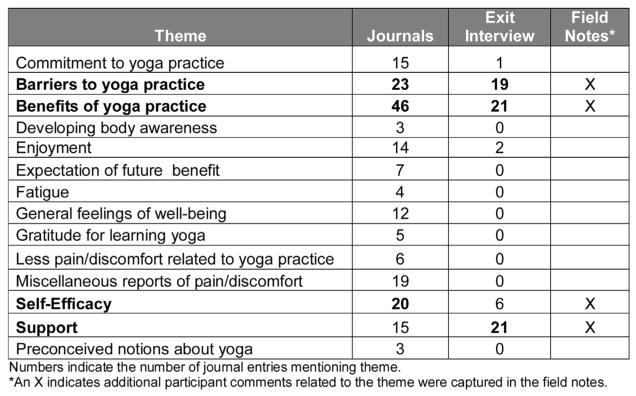
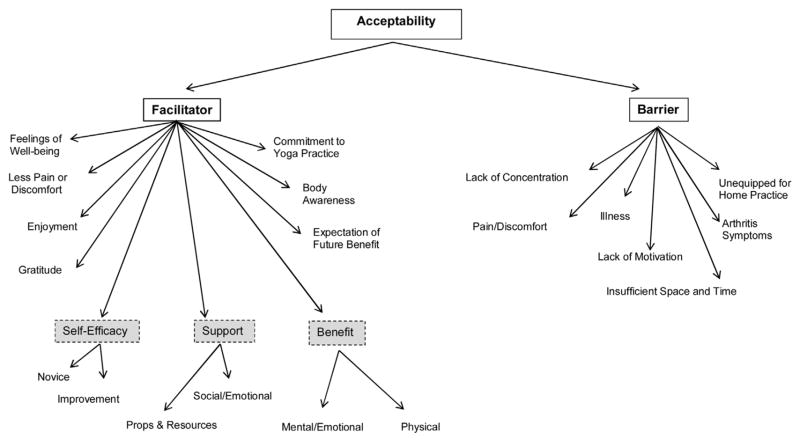
Participant narratives (n = 12) were used to assess the acceptability of participating in the yoga research study from the participant’s perspective. Information from three sources (journals, exit interviews, and field notes) were condensed down to a matrix format27 (Fig. 2) to help visualize which themes were prominent based on the method of data collection. The majority of themes were related to benefits and barriers of yoga practice, support, and self-efficacy and are discussed in more detail below. Fig. 3 offers a schema highlighting the organization of themes and sub-themes.
Fig. 2.
Matrix of Themes by Source of Data Collection.
Fig. 3.
Journal Themes and Subthemes Related to Acceptability.
3.2. Perceived benefit from taking yoga classes
Journal quotes related to benefits included those that were both mental/emotional (relaxation, tranquility, less stress, calm mind); and physical (energy, flexibility, stretching, improved sleep). Examples of participant’s journal quotes are shown in Table 1. Quotes categorized as perceived benefits, were viewed by the researchers as factors which motivated continued yoga class attendance. Exit interview responses (Table 2) showed 94% viewed yoga as a way to care for their arthritis symptoms. Most agreed that the yoga poses work well for people with arthritis; nearly 2 out of 3 prefer taking classes with others who have arthritis. When asked, “Now that you have completed the study, do you see yoga as a way to care for your arthritis?” comments included balance, stretching, calms mind, relaxation and breathing.
It is an illness where the bones get stiff and hard and with the exercise for me they (the joints) are more “docile” and stretch more. —49 year old Hispanic female, RA, pain score 8
Helps me position my body when I drive, everything. Brings a calmness. Stretch I need. Meditation calms my mind.—45 year old African American female, RA, pain score 7
Table 1.
Participant Quotes
| Themes | Sub-themes | Participant Quotes |
|---|---|---|
| Perceived benefit | Mental/Emotional |
I am very grateful for doing yoga. I am more tranquil and I can sleep more because I practice breathing and letting go of everything in my mind. −60 year old Hispanic female, OA, pain score 5 When I do the exercises I feel good, I am thinking about what I am doing, I feel very centered in thought and spirit. −62 year old Hispanic female, RA, pain score 8 |
| Physical |
Class was good today. I was on the mat for the first time. I feel I got a better workout on the mat. After we worked on our feet mine actually felt better. I seem to have more energy when I left class. −65 year old African American female, RA, pain score 3 I am very happy because I have learned yoga, it is something new for me, it is helping me feel better, sleep better, to stretch and that helps me in my arthritis and I forget that I have it/suffer from it. −60 year old Hispanic female, OA, pain score 5 |
|
| Self –Efficacy | Improvement |
Practiced for 30 minutes. No Pain. I’m getting into a better flow with my home practice, but still need to use the manual. −45 year old African American female, RA, pain score 7 It was a very good experience because I didn’t need help. Although I am not sure it was perfect but just the experience, I hope to perfect it. −60 year old Hispanic female, OA, pain score 5 |
| Novice |
I try to do it when I exercise I can and I want to learn them and that way I won’t depend on the instructors, soon she will leave us alone and we will have to do it ourselves. −60 year old Hispanic female, OA, pain score 5 I tried to do the exercise on Wednesday but I don’t think I did very well. I need to keep my mind only on what I am doing….I tried to do a ten minute meditation. I was concentrating on just one sentence. It was hard to stay focus. I tried just seeing it in my head like a tie on tape but was hard. I don’t know if I am doing this correctly. −65 year old African American female, RA, pain score 3 |
|
| Support | Social/Emotional |
Today I did standing poses, my son did them too, and he was also helping me by telling me how. Then I felt that gradually, the stretches are rather easy to do. −46 year old Hispanic female, RA, pain score 5 I had a lot of fun practicing with my eight year old daughter. −45 year old African American female, RA, pain score 7 |
| Props and Resources |
I stretch my legs, my arms, whole body, I cannot balance but I grab a chair −60 year old Hispanic female, OA, pain score 5 Standing on the toes holding the wall, it is pretty good. I did the warm up looking at the book. −62 year old African American female, RA, pain score 8 |
|
| Barriers | Lack of concentration | (I) am also confused because when I relax in the moment that I am doing the exercise my mind starts to think about what I will be doing later. −33 year old Hispanic female, RA, pain score 4 |
| Pain/Discomfort | Today I practiced in the morning, I didn’t feel as motivated to do it. Because I had some pain. But afterwards I felt somewhat better. −46 year old Hispanic female, RA, pain score 5 |
Table 2.
Exit Interview Responses (n = 16).
| Question Text | Response categories | Freq (%) |
|---|---|---|
| Overall how satisfied were you with the yoga classes? | Completely satisfied | 12 (75%) |
| Mostly satisfied | 3 (19%) | |
| Equally satisfied/dissatisfied | 1 (6%) | |
| Yoga classes should be offered in both English/Spanish. | Strongly agree | 5 (31%) |
| Agree | 10 (63%) | |
| Neither agree/disagree | 1 (6%) | |
| I feel more comfortable taking yoga classes from teachers with diverse racial/ethnic backgrounds. | Strongly agree | 4 (29%) |
| Agree | 4 (29%) | |
| Neither agree/disagree | 6 (43%) | |
| I prefer taking yoga classes with others who have arthritis. | Strongly agree | 5 (31%) |
| Agree | 5 (31%) | |
| Neither agree/disagree | 6 (38%) | |
| The yoga poses offered work well for people with arthritis. | Strongly agree | 7 (44%) |
| Agree | 7 (44%) | |
| Neither agree/disagree | 2 (13%) | |
| Would recommend yoga classes to friend with arthritis? | Yes | 15 (94%) |
| No | 1 (6%) | |
| Now that you have completed the study do you see yoga as a way to care for your arthritis? | Yes | 15 (94%) |
| No | 1 (6%) | |
| How likely is it that you would take another yoga class? | Extremely likely | 10 (63%) |
| Fairly likely | 3 (19%) | |
| Somewhat likely | 2 (13%) | |
| Slightly likely | 1 (6%) | |
| How likely is it that you would practice yoga on your own now? | Extremely likely | 6 (38%) |
| Somewhat likely | 6 (38%) | |
| Fairly likely | 3 (19%) | |
| Slightly likely | 1 (6%) |
3.3. Barriers for practicing yoga
Fig. 3 highlights themes that emerged related to barriers to yoga practice which included lack of concentration, lack of motivation, insufficient time and space to practice, illness and arthritis symptoms. Quotes offered in Table 1 highlight sub-themes in this category. During the exit interviews, in response to the question, “What did you like least about the yoga classes?” responses included, the location of the yoga studio was ‘too far away’, and difficulty fitting classes into work schedules. The cost of public transportation was also stated as a barrier. An unanticipated barrier for some was lack of internet access or GPS for directions which resulted in needing increased assistance to locate the yoga studio on the first day. During the course of the study, one student withdrew for religious reasons.28
3.4. Self-efficacy (confidence in ability to practice yoga)
Self-efficacy can be influenced by learning a new behavior, seeing people similar to oneself succeed, and by correcting misinterpretations of physical ability.29 Participants’ comments such as those highlighted in Table 1, indicated an increased self-confidence and a focus on mastering the yoga poses. Initially most lacked body awareness and were focused on getting the poses “right”. Because of small class sizes, detailed modification and use of props was tailored to the specific need of each participant. As the classes progressed, it could be observed that some were able to incorporate modifications, self-adjust or require less cueing. Some participants came to class early or stayed afterwards to obtain additional personal instruction/clarification related to their home practice.
3.5. Support
Unlike in some cultures where only the individual receives an intervention, within the concept of familialism or familismo family members were encouraged to participate in yoga classes. Approximately half of participants brought their school-aged children to the studio; some joined the class, which served as additional support for home practice (Table 1). Other sources of support, elucidated through the journal quotes, were the resources offered through the protocol. In response to the exit interview question, ‘What did you like most about the yoga classes?’ responses included stretching, the instructor, support, relaxation, and using the manual:
The people that gave it, the teachers, have patience and are “amiable” treated me with a lot of respect. I am happy/content (with) them (teachers). —49 year old Hispanic female, RA, pain score 8
For me everything. But I can’t remember all the sequences. I am remembering [as I go]. I look at it in the manual. —62 year old Hispanic female, RA, pain score 8
3.6. Exit interviews
Specific questions were included in the exit interview to better understand how participants viewed some of the study design features (bilingual classes, multi-ethnic teachers, taking classes with others with arthritis) (Table 2). For those completing the intervention, exit interviews (n = 16) were completed in the yoga studio following the last class. An attempt was also made to complete the interview, by phone, for those who withdrew from the study after attending the first class. On average, the interview lasted 30 min. Most were satisfied with the yoga classes, agree yoga classes should be bilingual, and would recommend yoga classes to a friend with arthritis. Half were more comfortable taking yoga classes from teachers with diverse racial/ethnic backgrounds, and others who have arthritis. During the one-on-one exit interviews participants were encouraged to elaborate on structured questions through open-ended options, listed in the appendix of the original protocol.10 The majority of these comments were related to benefits and barriers to yoga practice, and support (Fig. 2).
4. Discussion
Before undertaking this research, it was not clear if the bilingual minority population served by a community rheumatology clinic would view yoga as an acceptable modality in managing their arthritis symptoms. When designing the study, the team spent considerable time discussing ways to build a ‘cultural infrastructure’ to overcome potential barriers seen in the clinical setting and known from previous research.
Beyond the barrier of low minority representation in research, there was an additional unfamiliarity with yoga. Discussions regarding potential barriers with introducing yoga to this population included the lack of full-figured, culturally relevant images of minorities doing yoga; the lack of yoga studios in this community; and the cost of yoga classes, for those with little to no discretionary income. Preconceived ideas about yoga included: concern that the entire class would be chanting, that the movements would increase arthritis pain, or yoga would conflict with religious beliefs.
These may have partially been overcome through referrals from clinicians for whom there was already a trusted relationship. Some of the referring clinicians attended the yoga classes, which most likely served to validate the intervention outside of the clinical research setting. When designing recruitment materials, a day-long photoshoot was held in order to obtain pictures of minorities doing yoga. While creating the protocol, the decision was made to decrease what might be deemed as ‘spiritual’ aspects of yoga. As discussed in-depth in a previous article, the decision was made that no music would be played, there would be no chanting “OM” or bowing to say “Namaste,” and the Sanskrit names for yoga poses would not be used.28 However, in an attempt to maintain the core essence of Hatha yoga, postures (asanas), breathing techniques (pranayama), and meditation were maintained. The yoga offered was primarily influenced by Integral, Iyengar and Kripalu yoga, each of which focuses on proper, gentle physical alignment, while also including a strong component of mindfulness during and between postures.10
4.1. Cultural infrastructure
This study validates the positive impact of creating a multi-cultural, interdisciplinary team of researchers and clinicians when designing research studies focused on enhancing acceptability for diverse populations. Several participants reported appreciating the decisions made related to study design (multicultural staff, arthritis-specific yoga, bilingual materials and classes) in an effort to make the study more inclusive.
In comparison, the previous Yoga for Arthritis study, was not specifically designed to address minority participation. While the study had a diverse participant pool, and was conducted in an area with a similar diverse culture and social determinants (Baltimore, MD), there were few Spanish-speakers, and the strongest predictor of attrition was minority race.1
4.2. Facilitators and barriers
Collecting and analyzing narratives show that overall, participants on this study reported positive experiences. Facilitating factors included feelings of well-being, less pain or discomfort, gratitude, body awareness, expectation of future benefit and commitment to yoga practice. Positive feedback, along with follow-up reports verifying that those who completed the study continue to practice yoga three months after completing the intervention, support the inference of acceptability for this study population.
Reports of physical and emotional benefits along with self-efficacy were also viewed as indicators of facilitating continued yoga practice. The study was designed to promote not only a culturally supportive atmosphere, but to offer support within a cohort of others with arthritis. In the previous health behaviors study30 it was asserted that ‘social support’ should be considered an important aspect in health outcomes for Hispanics with chronic rheumatic diseases. Involving family members in the plan of care for this population could facilitate health promotion and chronic disease management.30 Over the course of the study, as each cohort became more familiar with each other, there was a tendency to offer rides to those taking public transportation, to offer more precise Spanish translations of yoga modifications, and to make ‘friendly’ gestures to get the attention of classmates not following the group. Several groups brought food to the last class as a way to mark the end of their time together.
Reported barriers to yoga practice included lack of concentration, miscellaneous reports of pain/discomfort, illness, lack of motivation, unequipped for home practice, arthritis symptoms. Participants were recruited from an extensive area surrounding the Washington, DC area. While distance and conflicting schedules were mentioned as a barriers, some attended classes even though they travelled as much as 1–2 h to get to the studio. Some were willing to rearrange their schedules to come on their days off from work or lunch hour. Overall, the results obtained by using qualitative methodology indicate that offering an arthritis-based yoga intervention was found to be acceptable to participants who completed the study.
4.3. Limitations
Generalizability of this study is limited due to the convenience sample of minority patients receiving rheumatology care at a clinic in the Washington DC area. Additionally since participants were predominantly female, results cannot be used to infer whether males would have had a similar experience. While an attempt was made to obtain exit interviews from those who attended at least one yoga class, another limitation is that there was less feedback from those who withdrew from the study. As journal completion was optional, all participants did not complete journals; therefore conclusions reached may not represent the views of the entire study population.
5. Conclusion
History has shown that research studies conducted on one gender or group may not translate to all members of a society. As yoga research continues to demonstrate positive benefits, there is an increasing need to explore the acceptability for populations not typically known to practice yoga. This paper highlights the perception that cultural infrastructure, established from previous experience with the population, was sufficient to encourage participation in the yoga intervention. After recruitment and retention were addressed, participants were able to focus on their arthritis symptoms (the main purpose for offering the yoga intervention), and continued practicing yoga after completing the study.
Acknowledgments
Funding source
All funding for this study is provided by the National Institutes of Health Clinical Center Intramural Research Program.
The study was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS). The authors wish to thank all study participants, Charlene Muhammad MS RYT500, Alice Fike MSN, Lorena Wilson MSN, and Regina Andrade MA.
Footnotes
Declaration of conflicting interests
Steffany Haaz Moonaz reports consulting fees from NIH during the conduct of the study and provides arthritis-related continuing education for yoga professionals. All remaining authors declare that there is no conflict of interest.
Trial registration
ClinicalTrials.gov: NCT01617421.
References
- 1.Moonaz SH, Bingham CO, Wissow L, Bartlett SJ. Yoga in sedentary adults with arthritis: effects of a randomized controlled pragmatic trial. J Rheumatol. 2015;42(July (1)):1194–1202. doi: 10.3899/jrheum.141129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ward L, Stebbings S, Cherkin D, Baxter GD. Yoga for functional ability, pain and psychosocial outcomes in musculoskeletal conditions: a systematic review and meta-analysis. Musculoskelet Care. 2013;11(December (4)):203–217. doi: 10.1002/msc.1042. [DOI] [PubMed] [Google Scholar]
- 3.Evans S, Moieni M, Lung K, et al. Impact of iyengar yoga on quality of life in young women with rheumatoid arthritis. Clin J Pain. 2013;29(November (11)):988–997. doi: 10.1097/AJP.0b013e31827da381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cramer H, Ward L, Steel A, Lauche R, Dobos G. Prevalence Zhang Y. Patterns, and predictors of yoga use: results of a U.S. nationally representative survey. Am J Prev Med. 2016;50(February (2)):230–235. doi: 10.1016/j.amepre.2015.07.037. [DOI] [PubMed] [Google Scholar]
- 5.Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL. Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Report. 2015;10(February (79)):1–16. [PMC free article] [PubMed] [Google Scholar]
- 6.Haber D. Yoga as a preventive health care program for white and black elders: an exploratory study. Int J Aging Hum Dev. 1983;17(3):169–176. doi: 10.2190/HU5C-32FH-APVU-N6FY. [DOI] [PubMed] [Google Scholar]
- 7.Wilson A, Marchesiello K, Khalsa SB. Perceived benefits of Kripalu yoga classes in diverse and underserved populations. Int J Yoga Ther. 2008;18(1):65–71. [Google Scholar]
- 8.Saper RB, Boah AR, Keosaian J, Cerrada C, Weinberg J, Sherman KJ. Comparing once- versus twice-weekly yoga classes for chronic low back pain in predominantly low income minorities: a randomized dosing trial. Evid Based Complement Alternat Med. 2013;2013:658030. doi: 10.1155/2013/658030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keosaian JE, Lemaster CM, Dresner D, et al. We’re all in this together: a qualitative study of predominantly low income minority participants in a yoga trial for chronic low back pain. Complement Ther Med. 2016;24(February):34–39. doi: 10.1016/j.ctim.2015.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Middleton KR, Ward MM, Haaz S, et al. A pilot study of yoga as self-care for arthritis in minority communities. Health Qual Life Outcomes. 2013;11(55):55. doi: 10.1186/1477-7525-11-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Potter J, Odutola J, Gonzales CA, Ward MM. Validation of English and Spanish-language versions of a screening questionnaire for rheumatoid arthritis in an underserved community. J Rheumatol. 2008;35(8):1545–1549. [PMC free article] [PubMed] [Google Scholar]
- 12.George S, Duran N, Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. Am J Public Health. 2014;104(February (2)):e16–31. doi: 10.2105/AJPH.2013.301706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brooks K, Fessler BJ, Bastian H, Alarcón GS. Sociocultural issues in clinical research. Arthritis Care Res. 2001;45(2):203–207. doi: 10.1002/1529-0131(200104)45:2<203::AID-ANR174>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 14.Marín G, Marín BVO. Research with Hispanic Populations. Sage Publications; 1991. [Google Scholar]
- 15.Kagawa-Singer M. Improving the validity and generalizability of studies with underserved U.S. populations expanding the research paradigm. Ann Epidemiol. 2000;10(8 Suppl 1):S92–103. doi: 10.1016/s1047-2797(00)00192-7. [DOI] [PubMed] [Google Scholar]
- 16.Wallen GR, Middleton KR, Rivera-Goba MV, Mittleman BB. Validating English-and Spanish-language patient-reported outcome measures in underserved patients with rheumatic disease. Arthritis Res Ther. 2011;13(January (1)):R1. doi: 10.1186/ar3219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wallen GR, Middleton KR, Miller-Davis C, et al. Rheumatic disease patients, community leaders, and health behavior researchers: partners in research. Prog Community Health Partnersh: Res Educ Action. 2012;6(4):403–404. doi: 10.1353/cpr.2012.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berman RC, Tyyska V. A critical reflection on the use of translators/interpreters in a qualitative cross-language research project. Int J Qual Methods. 2011;10(2):178–190. [Google Scholar]
- 19.Liamputtong P. Doing Cross-Cultural Research: Ethical and Methodological Perspectives. 1. Netherlands: Springer; 2008. [Google Scholar]
- 20.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009;119(March (10)):1442–1452. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 21.Riessman CK. Narrative Methods for the Human Sciences. SAGE Publications; 2008. [Google Scholar]
- 22.Lapan SD, Quartaroli MLT, Riemer FJ. Qualitative Research: An Introduction to Methods and Designs. Wiley; 2011. [Google Scholar]
- 23.Qualitative data analysis software computer program. Version 10. QSR International Pty Ltd; 2012. [Google Scholar]
- 24.Patton MQ. Qualitative Research & Evaluation Methods. SAGE Publications; 2002. [Google Scholar]
- 25.Ryan GW, Bernard HR. Techniques to identify themes. Field Methods. 2003;15(February(1)):85–109. [Google Scholar]
- 26. [Accessed 3 November 2016];PROMIS Adult Profile Instruments. 2016 Available at: https://www.assessmentcenter.net/documents/PROMIS%20Profile%20Scoring%20<otherrefdata>Manual.pdf.
- 27.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. SAGE Publications; 1994. [Google Scholar]
- 28.Middleton KR, Andrade R, Moonaz SH, Muhammad C, Wallen GR. Yoga research and spirituality: a case study discussion. Int J Yoga Ther. 2015;25(1):33–35. doi: 10.17761/1531-2054-25.1.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(April (2)):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 30.Brooks AT, Andrade RE, Middleton KR, Wallen GR. Social support: a key variable for health promotion and chronic disease management in Hispanic patients with rheumatic diseases. Clin Med Insights Arthritis Musculoskelet Disord. 2014;7:21–26. doi: 10.4137/CMAMD.S13849. [DOI] [PMC free article] [PubMed] [Google Scholar]