Abstract
Background:
Postpartum home care plays an important role in prevention of postpartum complications. Regular visits of mothers during this period are imperative. This study aimed to provide postpartum home care for mothers to assess its effects on mothers’ health in Iran.
Materials and Methods:
This study was carried out in two phases. First, a comprehensive postpartum home care program was compiled by performing a comparative study, using the available guidelines in this regard in different countries and based on the opinions of the experts. Next, a clinical trial was carried out on 276 women who gave birth in the university hospitals affiliated to Shahid Beheshti University of Medical Sciences. There were 92 mothers in the intervention and 184 in the control group. The intervention group mothers were provided with postpartum home care service while the control group did not receive such a service.
Results:
Outcome assessment at 60 days’ postpartum revealed a significant difference between the two groups in terms of the use of supplements, birth control methods, postpartum depression, breastfeeding problems, constipation, and fatigue (P < 0.05). No significant differences were noted between the two groups with regard to hospitalization, hemorrhoids, backache and lumbar pain (P > 0.05).
Conclusion:
The postpartum home care program had a positive effect on some aspects of the mothers’ health status and their satisfaction in our society.
Keywords: Home visit, mother's health, postpartum care, postpartum depression, women's health
INTRODUCTION
The postpartum period starts from 1 h after delivery to 42 days and is a critical period for the mothers’ health.[1] Women experience various physical, mental, and emotional changes during this period, which may interfere with their daily routine.[2] A wide range of complications have been reported during this period such as physical, mental, and emotional problems including fatigue, concerns with regard to sexual intercourse, hemorrhoids, constipation, breastfeeding problem, anxiety, stress, depression, sleep disorders, bleeding, urinary incontinence, and posttraumatic stress disorder. Women's health after delivery is the most important factor affecting the health of their children.[3] Significant changes that occur postpartum result in a drop in the quality of life of mothers during this critical period.[4] Most mothers have inadequate knowledge about the postpartum care and complications.[5] For this reason, first-time mothers are often not well prepared for this task and require the support of the family, friends, and health personnel.[6] Provision of postpartum care is the most important measure to prevent unwanted consequences. Thus, performance of health personnel and providing social support for the mothers play important roles in preparing them to cope with the new situation.[7] Postpartum home visit is a suitable method to obviate the educational and supportive needs of mothers because it is often difficult for them to go somewhere during the 1st day after delivery and it would be best if they could be provided with care services at the convenience of their home.[8] Postpartum home care refers to the measures taken to prevent complications and promote the health of mothers during this period and improve the quality of their relationship with their newborns. This service helps mothers to better cope with their new, stressful life and empowers them to better manage taking care of themselves and their infants.[9] Moreover, postpartum home care may have unique advantages for prevention of mental and psychological complications in mothers.[10] Women who received midwifery care services at home reported the best quality of services compared to those receiving these services at the hospital. Furthermore, women who received postpartum home visits had higher level of satisfaction with the services.[11] Considering the limited number of studies on the postpartum home care services in Iran, this study aimed to design and provide postpartum home care service for mothers to assess its efficacy. The results of this study can help promote mothers’ health and their satisfaction since it is believed that postpartum home services can significantly decrease the common complications in this period and increase mothers’ satisfaction.
MATERIALS AND METHODS
This study was conducted in two phases. In the first phase, a comparative study was conducted to review the postpartum care guidelines in different countries. After brainstorming with the experts in the field, a consensus with regard to the necessary guidelines was achieved. A search was carried out in Google Scholar, Google, National Guideline Clearinghouse, World Health Organization (WHO), PubMed, NICE, and Cochrane databases to find postpartum home care guides in different countries. More comprehensive guidelines were selected. Next, based on the opinions of gynecologists and obstetricians and community medicine specialists, some modifications were made in the guidelines (according the conditions and needs of mothers in Iran); these changes were applied to the national care protocol for the mothers’ health, which is routinely provided for mothers in the health centers as postpartum care service.
In the second phase, a clinical trial was carried out to assess the effect of home visits on mothers’ health and was registered in IRCT (code 2013060313565N1). The compiled instruction was used for home visit of mothers. The study population included women who gave birth in Taleghani, Shohada, Mahdiyeh, and Imam Hossein Hospitals. A total of 276 mothers who met the following inclusion criteria and signed written informed consent forms were consecutively selected and entered in the study [Figure 1]. The inclusion criteria were: Iranian nationality, no underlying disease, no pregnancy hypertension, no preeclampsia, no pregnancy diabetes, single birth with normal birth weight, no congenital anomaly, Edinburgh Postnatal Depression Scale of <10, no history of depression, and not taking antidepressants. Sixty-eight participants were chosen from each hospital. The selected mothers filled out the Edinburgh Postnatal Depression questionnaire. Those scoring over 10 in this questionnaire and whose had suicide thoughts were excluded and referred to a psychiatrist. The exclusion criteria were unwillingness for participation or wishing to quit for any reason. A total of 92 mothers were evaluated in the intervention and 184 in the control group (two controls per each mother in the intervention group). The intervention group mothers received postpartum home care service while the control group did not receive such a service. The data were collected by a trained midwife through observation, interview, history taking, and clinical examination of mothers. The collected data were recorded in the respective questionnaire. These data included demographics and pregnancy information. The questionnaire was filled out for all mothers. For those receiving postpartum home care, postpartum care checklist was filled out on day's 3–5 and 13–15 after childbirth. The content of care was the items mentioned in the Ministry of Health instruction[12] and included examinations, observations, questions and necessary instructions and training with regard to personal hygiene, mental, psychological, and sexual health, oral and dental health, risk factors, common complaints in the postpartum period, nutrition in this period and use of supplements, breastfeeding and its related problems and duration, care for the infant, and contraception. Anti-D globulin if is indicated injection was emphasized in the first and dental examination; the Papanicolaou test and birth control were emphasized in the second phase of care. Instructions on how to manage postpartum complications and exercise activities in this period were also added to the respective national protocol. Outcome assessment was done on day 60, and health parameters of the mothers in the two groups of intervention and control were assessed and compared. These parameters included the use of supplements by mothers, postpartum depression, hospitalization due to postpartum complications, common physical complaints and their significance and satisfaction of mothers with the emotional, communication, and educational services received in the two groups. To diagnose postpartum depression, Edinburgh Postnatal Depression questionnaire was used. This questionnaire, designed by Cox et al. in 1978,[13] has 10 questions and is widely used as a Postnatal Depression Scale. Its sensitivity, specificity, and predictive value have been previously confirmed for use in the Iranian populations.[14,15] In this questionnaire, scores of <10 indicate no depression, 10–12 indicate mild depression, and scores of over 13 and presence of suicidal thoughts indicate severe depression.[16] To determine the level of satisfaction of mothers with the service received, the questionnaire designed by Mirmolaei et al.[1] was used. To assess the validity of the questionnaire, content validity was evaluated. For this purpose, 10 experts, who were the scientific faculty members of School of Nursing and Midwifery of Tehran University of Medical Sciences, confirmed the questionnaire for its content. Reliability was assessed by retest, and the correlation coefficient was calculated to be 0.8.[1] The data were analyzed using Chi-square test, Fisher's exact test, and t-test. Descriptive statistics were also applied. All statistical analyses were carried out using SPSS version 18 (IBM Company). P = 0.05 or less was considered statistically significant.
Figure 1.
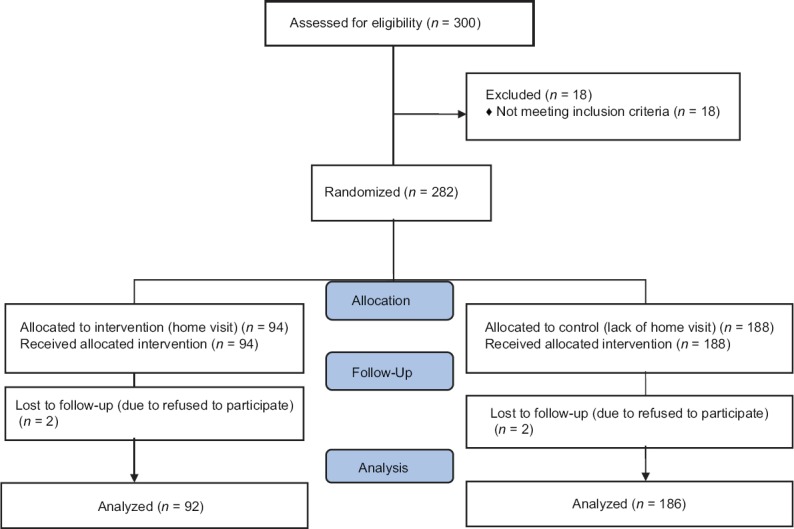
Study flowchart
RESULTS
The guidelines by the WHO, Australia, United Kingdom, United States, Canada, and Latin America were selected since they were more comprehensive than the others. Parts of these guidelines were added to the national protocol for mothers’ health based on the opinions of the experts and stakeholders; the added sections discussed the management of common postpartum complications and conduction of sport activities and physical exercise. For diagnosis of postpartum depression during the visits on days 13 and 15, Edinburgh Postnatal Depression questionnaire was used.
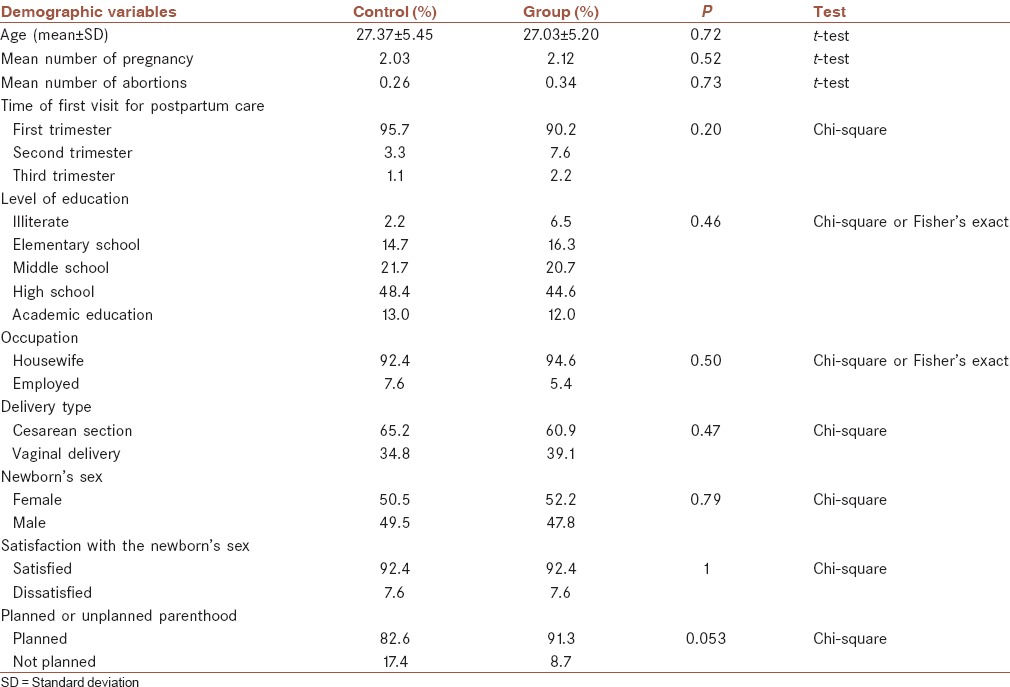
In the second phase of the study, the following results were obtained in the two groups. No significant differences existed between the two groups of intervention and control for the demographic factors and some factors related to depression, and the two groups were similar in this respect [Table 1]. Assessment of health parameters of the mothers and newborns at 60 days after delivery revealed the following results:
Table 1.
The descriptive statistics of the group which had postpartum health care services at home and the control group
With regard to the use of supplements by the mothers in the intervention group, 88% and 12% reported regular and irregular use of supplements, hematinic and multivitamin tablets during the first 60 days postpartum, respectively. All mothers in this group used supplements. In the control group, 73.4% and 6.19% reported regular and irregular use of supplements during the first 60 days, respectively; 13% used no supplement. The difference in this regard between the intervention and control groups was significant (P < 0.05). In terms of maternal hospitalization due to postpartum complications, although the hospitalization rate was lower in the group visited, the difference was not statistically significant (P > 0.05).
With regard to birth control to keep a minimum of 2-year interval between pregnancies, at 60 days postpartum, birth control was reported by 89.1% in the intervention group and 60.8% in the control group; the difference in this regard between the two groups was statistically significant (P < 0.05).
In terms of postpartum depression, 92.4% gained a score of <10 (no depression), 6.5% gained a score of over 13 (severe depression), and 1.1% gained a score of 10–13 (mild depression) in Edinburgh Postnatal Depression questionnaire. In the control group, 81.4% gained a score of <10 (no depression), 11.4% gained a score of 10–13 (mild depression), and 7.6% gained a score of over 13 (severe depression). The difference in this regard between the two groups was statistically significant (P < 0.05).
The two groups of intervention and control were not significantly different in terms of frequency of hemorrhoids (P > 0.05).
The frequency of backache and lumbar pain was lower in the intervention group, but the difference in this regard between the two groups was not statistically significant (P > 0.05).
Of the intervention group mothers, 10.9% complained of fatigue; this rate was 28.8% in the control group. The difference in this regard between the two groups was statistically significant (P < 0.05).
With regard to breastfeeding problems following lactation, 12% in the intervention group and 27.7% in the control group complained of congestion, mastitis, and cracked nipples; the difference in this regard was significant between the two groups (P < 0.05).
With regard to postpartum constipation, 13% in the intervention and 26.1% in the control group complained of constipation; the difference in this regard was significant between the two groups (P < 0.05).
Control mothers were evaluated in terms of seeking postpartum care. Based on the results, of 184 mothers who did not receive postpartum home care, 130 (70.7%) presented to health centers at least once during the first 60 days after delivery and 54 (29.3%) did not present to any health center during this period.
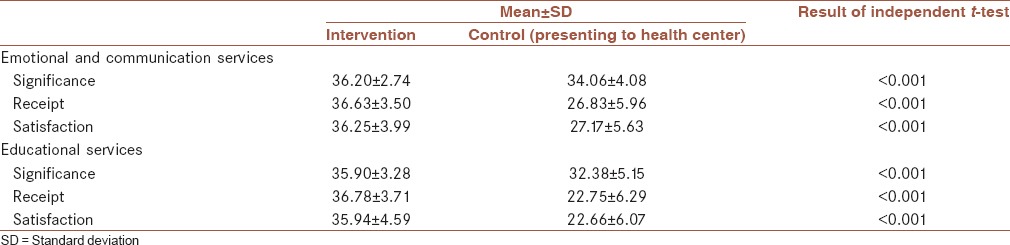
The mean and standard deviation of significance, receipt, and satisfaction of mothers with emotional, communication, and educational postpartum care services received at home were higher compared to controls, and this difference was statistically significant [Table 2].
Table 2.
The mean and standard deviation of significance, receipt, and satisfaction of mothers with emotional, communication, and educational postpartum care services received at home compared to controls (presenting to health center)
DISCUSSION
The results of the first phase of the study revealed that no solution had been provided in the national protocol (currently implemented in health centers) with regard to the prevention or treatment of some common postpartum complications such as fatigue, backache, lumbar pain, headache, constipation, type of sport activities and exercise, and time of starting them and screening for postpartum depression. In Australia and the United States, screening for postpartum depression is performed using Edinburgh questionnaire; however, NICE guideline of the UK did not recommend the use of this questionnaire; instead, it recommended assessing depression by two simple questions, i.e., “have you ever felt hopeless or depressed in the past month?” and “were you interested to do some chores in the past month?” These questions can help assess the mothers’ mood.[16,17] In the guidelines of the South American countries, the UK, and the WHO, some solutions have been offered for common postpartum complications such as fatigue, headache, backache, lumbar pain, and constipation.[18,19,20,21,22] In the Australian guideline, some recommendations existed on how to manage fatigue and constipation, but no recommendation was given for the management of headache, backache, or lumbar pain.[20] With regard to exercise activities in days after delivery, detailed explanations had been provided in the Canadian, Australian, and American guidelines.[22,23,24] However, no instruction was given in the NICE health guide of the UK with regard to postpartum physical activities.[16,17] Based on the results of the second phase of the current study, most pregnancies occurred within the safe age range for pregnancy. In general, of all mothers, 64% had vaginal delivery and 36% had cesarean section, which is in agreement with the results of other studies in Iran. The results of DHS study in 2010 showed that the prevalence of C-section in Iran was much higher than that in the European countries and also higher than the acceptable range recommended by the WHO (5%–15%).[25] Our results showed that the use of supplements and modern birth control methods was higher in the intervention group than controls and this difference was statistically significant. Significance, receipt, and satisfaction of mothers with the emotional, communication, and educational services provided were higher in the intervention group at 60 days’ postpartum. These findings are in accordance with those of a study by Mirmolaei et al., in 2011, in Tehran.[1] Similarly, higher satisfaction of mothers with the services provided at home was also reported in a cluster-randomized trial by Christie and Bunting in 2011.[26] However, Ian in his study in 2011 showed that home visits had no significant effect on satisfaction with services.[27] In the current study, the prevalence of postpartum depression was lower in the intervention group compared to the control group and this difference was statistically significant. With regard to postpartum depression, our findings were in agreement with those of Christie and Bunting; they indicated that the rate of postpartum depression assessed by Edinburgh questionnaire 8 weeks’ postpartum decreased in the group that received home care. In contrast, Ian showed that home visits had no significant effect on postpartum depression.[27]
One strength of the current study was that it enabled visit of mothers at home in the 1st week after delivery, which had a significant effect on mothers’ coping with the new situation because most problems related to the mother and newborn occur in the first 10 days’ postpartum.
The current study also had a limitation. Mothers were only visited twice at 3–5 and 13–15 days’ postpartum, and no other visits were made unto day 60. However, the mothers were allowed to contact the researcher in case of any problem, and midwives and physicians were ready to answer the mothers’ questions.
CONCLUSION
Based on the results of this study, postpartum home visits obviated the needs of the mothers to a great extent and decreased the prevalence of some common physical postpartum complications.[28] The intervention group had higher frequency of the use of supplements and higher satisfaction with the service provided. Thus, it is recommended that the health authorities consider providing mothers with home care services to promote their health. This intervention can also be included in the national protocol of mothers’ health.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We also extend our thanks to all participants and midwives for their cooperation with the researchers.
REFERENCES
- 1.Mirmolaei T, Amel Valizadeh M, Mahmoodi M, Tavakkol Z. The effect of postpartum care at home on maternal received care and satisfaction. J Nurs Midwifery Mashhad Univ Med Sci. 2011;1:35–48. [Google Scholar]
- 2.Mirmolaei ST, Valizadeh MA, Mahmoodi M, Tavakol Z. Comparison of effects of home visits and routine postpartum care on the healthy behaviors of Iranian low-risk mothers. Int J Prev Med. 2014;5:61–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Huang K, Tao F, Liu L, Wu X. Does delivery mode affect women's postpartum quality of life in Rural China? J Clin Nurs. 2012;21:1534–43. doi: 10.1111/j.1365-2702.2011.03941.x. [DOI] [PubMed] [Google Scholar]
- 4.Hill PD, Aldag JC, Hekel B, Riner G, Bloomfield P. Maternal postpartum quality of life questionnaire. J Nurs Meas. 2006;14:205–20. doi: 10.1891/jnm-v14i3a005. [DOI] [PubMed] [Google Scholar]
- 5.Asghar Nia M, Heidar Zadeh A, Zahiri Z, Seyhani AR, Pormehr Yabandeh L, Oudi M. Assessment of women's knowledge regarding postpartum complications and cares. J Med Fac Guilan Univ Med Sci. 2005;14:56–62. [Google Scholar]
- 6.Cronin C. First-time mothers - Identifying their needs, perceptions and experiences. J Clin Nurs. 2003;12:260–7. doi: 10.1046/j.1365-2702.2003.00684.x. [DOI] [PubMed] [Google Scholar]
- 7.Hung CH, Chung HH. The effects of postpartum stress and social support on postpartum women's health status. J Adv Nurs. 2001;36:676–84. doi: 10.1046/j.1365-2648.2001.02032.x. [DOI] [PubMed] [Google Scholar]
- 8.Dennis CL. Breastfeeding initiation and duration: A 1990-2000 literature review. J Obstet Gynecol Neonatal Nurs. 2002;31:12–32. doi: 10.1111/j.1552-6909.2002.tb00019.x. [DOI] [PubMed] [Google Scholar]
- 9.Chen CH. Effects of home visits and telephone contacts on breastfeeding compliance in Taiwan. Matern Child Nurs J. 1993;21:82–90. [PubMed] [Google Scholar]
- 10.McNaughton DB. Nurse home visits to maternal-child clients: A review of intervention research. Public Health Nurs. 2004;21:207–19. doi: 10.1111/j.0737-1209.2004.021303.x. [DOI] [PubMed] [Google Scholar]
- 11.Fenwick J, Butt J, Dhaliwal S, Hauck Y, Schmied V. Western Australian women's perceptions of the style and quality of midwifery postnatal care in hospital and at home. Women Birth. 2010;23:10–21. doi: 10.1016/j.wombi.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Montazeri A, Torkan B, Omidvari S. The Edinburgh Postnatal Depression Scale (EPDS): Translation and validation study of the Iranian version. BMC Psychiatry. 2007;7:11. doi: 10.1186/1471-244X-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 14.Mazhari S, Nakhaee N. Validation of the Edinburgh Postnatal Depression Scale in an Iranian sample. Arch Womens Ment Health. 2007;10:293–7. doi: 10.1007/s00737-007-0204-x. [DOI] [PubMed] [Google Scholar]
- 15.Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119:350–64. doi: 10.1111/j.1600-0447.2009.01363.x. [DOI] [PubMed] [Google Scholar]
- 16.Haran C, van Driel M, Mitchell BL, Brodribb WE. Clinical guidelines for postpartum women and infants in primary care - A systematic review. BMC Pregnancy Childbirth. 2014;14:51. doi: 10.1186/1471-2393-14-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Serruya S, Fescina R, Mucio D, Luis Diaz-Rossello J, Martínez G, Duran P. Sexual and reproductive health guides for the PHC focused continuum of care of women and newborns. Latin Am Center Perinatol, Women Reprod Health. 2009. [Last accessed on 2011 Jan]. Available from: https://www.researchgate.net/publication/280295957_Sexual_and_reproductive_health_guides_for_the_PHC_focused_continuum_of_care_of_women_and_newborns .
- 18.National Institute for Health and Clinical Excellence. NICE clinical guideline 37. 2015 [Google Scholar]
- 19.A Quick Reference Guide for Clinicians. Association of Reproductive Health Professionals. 2013 [Google Scholar]
- 20.Technical consultation on postpartum and postnatal Care. World Health Organization. 2010. [Last accessed on 2010]. Available from: http://apps.who.int/iris/bitstream/10665/70432/1/WHO_MPS_10.03_eng.pdf . [PubMed]
- 21.Society of Obstetricians and Gynaecologists of Canada (SOGC) and Canadian Society for Exercise Physiology, Clinical Practice Guidelines – Exercise in Pregnancy and the Postpartum Period; June. 2003 [Google Scholar]
- 22.Pre and Post-Natal Exercise Guidelines. 2013. [Last accessed on 2013 Sep]. Available from: www.fitness.org.au/guidelines .
- 23.American College of Obstetricians and Gynecologists (ACOG). Exercise During Pregnancy and the Postnatal Period. Washington, DC: ACOG; 2002. [Google Scholar]
- 24.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2008 [Google Scholar]
- 25.Demographic and Health Surve. Iran. 2011 [Google Scholar]
- 26.Christie J, Bunting B. The effect of health visitors’ postpartum home visit frequency on first-time mothers: Cluster randomised trial. Int J Nurs Stud. 2011;48:689–702. doi: 10.1016/j.ijnurstu.2010.10.011. [DOI] [PubMed] [Google Scholar]
- 27.Ian MP. Single Home Visits to Improve Health Outcomes; May. 2011 [Google Scholar]
- 28.Shamshiri Milani H, Shakeri N, Asbaghi T. Application of Repeated Measures Method to Compare Physical Maternal Health Index in a Follow-up Study. Glob J Health Sci. 2017;9:276–82. [Google Scholar]


