Abstract
Objective To evaluate the safety of home births in North America involving direct entry midwives, in jurisdictions where the practice is not well integrated into the healthcare system.
Design Prospective cohort study.
Setting All home births involving certified professional midwives across the United States (98% of cohort) and Canada, 2000.
Participants All 5418 women expecting to deliver in 2000 supported by midwives with a common certification and who planned to deliver at home when labour began.
Main outcome measures Intrapartum and neonatal mortality, perinatal transfer to hospital care, medical intervention during labour, breast feeding, and maternal satisfaction.
Results 655 (12.1%) women who intended to deliver at home when labour began were transferred to hospital. Medical intervention rates included epidural (4.7%), episiotomy (2.1%), forceps (1.0%), vacuum extraction (0.6%), and caesarean section (3.7%); these rates were substantially lower than for low risk US women having hospital births. The intrapartum and neonatal mortality among women considered at low risk at start of labour, excluding deaths concerning life threatening congenital anomalies, was 1.7 deaths per 1000 planned home births, similar to risks in other studies of low risk home and hospital births in North America. No mothers died. No discrepancies were found for perinatal outcomes independently validated.
Conclusions Planned home birth for low risk women in North America using certified professional midwives was associated with lower rates of medical intervention but similar intrapartum and neonatal mortality to that of low risk hospital births in the United States.
Introduction
Despite a wealth of evidence supporting planned home birth as a safe option for women with low risk pregnancies,1-4 the setting remains controversial in most high resource countries. Views are particularly polarised in the United States, with interventions and costs of hospital births escalating and midwives involved with home births being denied the ability to be lead professionals in hospital, with admitting and discharge privileges.5 Although several Canadian medical societies6,7 and the American Public Health Association8 have adopted policies promoting or acknowledging the viability of home births, the American College of Obstetricians and Gynecologists continues to oppose it.9 Studies on home birth have been criticised if they have been too small to accurately assess perinatal mortality, unable to distinguish planned from unplanned home births accurately, or retrospective with the potential of bias from selective reporting. To tackle these issues we carried out a large prospective study of planned home births. The North American Registry of Midwives provided a rare opportunity to study the practice of a defined population of direct entry midwives involved with home birth across the continent. We compared perinatal outcomes with those of studies of low risk hospital births in the United States.
Methods
The competency based process of the North American Registry of Midwives provides a certified professional midwife credential, primarily for direct entry midwives who attend home births, including those educated through apprenticeship. Our target population was all women who engaged the services of a certified professional midwife in Canada or the United States as their primary caregiver for a birth with an expected date of delivery in 2000. In autumn 1999, the North American Registry of Midwives made participation in the study mandatory for recertification and provided an electronic database of the 534 certified professional midwives whose credentials were current. We contacted 502 of the midwives (94.0%); 32 (6.0%) could not be located through email, telephone, post, or local associations, 82 (15.4%) had stopped independent practice, and 11 (2.1%) had retired. We sent a binder with forms and instructions for the study to the 409 practising midwives who agreed to participate.
Data collection
For each new client, the midwife listed identifying information on the registration log form at the start of care; obtained informed consent, including permission for the client to be contacted for verification of information after care was complete; and filled out a detailed data form on the course of care. Every three months the midwife was required to send a copy of the updated registration log, consent forms for new clients, and completed data forms for women at least six weeks post partum. To confirm that forms had been received for each registered client, we linked the entered data to the registration database. We reviewed the clinical details and circumstances of stillbirths and intrapartum and neonatal deaths and telephoned the midwives for confirmation and clarification. To verify this information we obtained reports from coroners, autopsies, or hospitals on all but four deaths. For these four, we obtained peer reviews.
Validation and satisfaction
We contacted a stratified, random 10% sample, of over 500 mothers, including at least one client for every midwife in the study. The mothers were asked about the date and place of birth, any required hospital care, any problems with care, the health status of themselves and their baby, and 11 questions on level of satisfaction with their midwifery care.
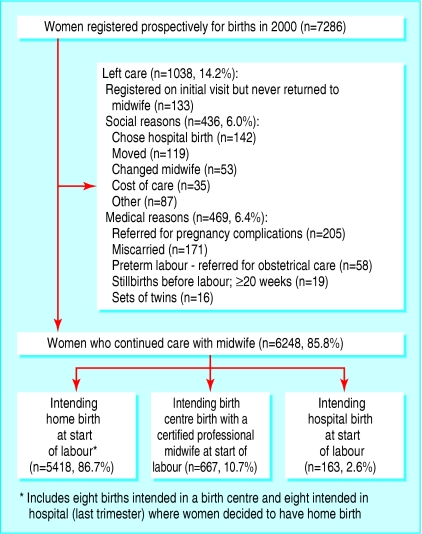
Figure 1.
Flow chart for mothers using certified professional midwives, 2000
Data analysis
Our analysis focused on personal details of the clients, reasons for leaving care prenatally, the rates and reasons for transfer to hospital during labour and post partum, medical interventions, health and admission to hospital of the newborn or mother from birth up to six weeks post partum, intrapartum and neonatal mortality, and breast feeding. We compared medical intervention rates for the planned home births with data from birth certificates for all 3 360 868 singleton, vertex births at 37 weeks or more gestation in the United States in 2000, as reported by the National Center for Health Statistics,10 which acted as a proxy for a comparable low risk group. We also compared medical intervention rates with the listening to mothers survey,5 a national survey weighted to be representative of the US birthing population aged 18-44. Intrapartum and neonatal death rates were compared with those in other North American studies of at least 500 births that were either planned out of hospital or comparable studies of low risk hospital births.
Results
A total of 409 certified professional midwives from across the United States and two Canadian provinces registered 7623 women whose expected date of delivery was in 2000. Eighteen of the 409 midwives (4.4%) and their clients were excluded from the study because they failed to actively participate and had decided not to recertify or left practice. Sixty mothers (0.8%) declined participation. The figure provides an overview of why women left care before labour and their intended place of birth at the start of labour.
Characteristics of the mothers
We focused on the 5418 women who intended to deliver at home at the start of labour. Table 1 compares them with all women who gave birth to singleton, vertex babies of at least 37 weeks or more gestation in the United States in 2000 according to 13 personal and behavioural variables associated with perinatal risk. Women who started birth at home were on average older, of a lower socioeconomic status and higher educational achievement, and less likely to be African-American or Hispanic than women having full gestation, vertex, singleton hospital births in the United States in 2000.
Table 1.
Characteristics of 5418 women planning home births with certified professional midwives in the United States, 2000, compared with all singleton, vertex births at ≥37 weeks' gestation in the United States, 2000. Values are percentages unless stated otherwise
| Characteristics | No (%) of women planning home birth*(n=5418) | All singleton, vertex births at ≥37 weeks gestation in USA, 2000†(n=3 360 86) |
|---|---|---|
| Mother's age: | ||
| ≤19 | 130 (2.4) | 11.6 |
| 20-24 | 930 (17.2) | 25.3 |
| 2-29 | 1554 (28.7) | 27.1 |
| 3-34 | 1423 (26.3) | 22.9 |
| 3-39 | 969 (17.9) | 10.9 |
| ≥40 | 327 (6.0) | 2.1 |
| Parity: | ||
| 0 | 1690 (31.2) | 40.2 |
| 1 | 1295 (23.9) | 32.8 |
| ≥2 | 2415 (44.6) | 27 |
| Mother's formal education: | ||
| High school or less | 2152 (39.2) | 52.4 |
| Any college | 1272 (23.2) | 21.6 |
| College graduate | 1169 (21.3) | 22.7 |
| Postgraduate | 692 (12.7) | 6.0 |
| Partner status at time of birth: | ||
| Has partner | 5169 (95.4) | NA |
| No partner | 164 (3.1) | NA |
| Ethnicity: | ||
| White | 4846 (89.4) | 58.2 |
| Hispanic | 216 (4.0) | 20.2 |
| African-American | 70 (1.3) | 14.1 |
| Other | 140 (2.6) | 5.8 |
| Other special groups: | ||
| Amish | 467 (8.7) | NA |
| Mennonite | 194 (3.6) | NA |
| Socioeconomic status‡: | ||
| Low | 1256 (23.2) | 19 |
| Middle | 3244 (59.9) | 44 |
| Upper | 664 (12.3) | 21 |
| Location: | ||
| City | 1891 (34.9) | NA |
| Small town | 1506 (27.9) | NA |
| Rural | 1734 (32.0) | NA |
| Time (trimester) prenatal care began: | ||
| 1st | 2483 (45.8) | 81.8 |
| 2nd | 2075 (38.2) | 12.6 |
| 3rd | 803 (14.8) | 2.7 |
| Smoked during pregnancy: | ||
| No | 5099 (94.1) | 76.2 |
| Yes: | 164 (3.0) | 8.9 |
| 1-9 cigarettes/day | 86 (1.6) | 6.4 |
| ≥10 cigarettes/day | 78 (1.4) | 2.5 |
| Unknown or not stated | 155 (2.9) | 14.9 |
| Alcohol intake (drinks/week) during pregnancy: | ||
| None | 5162 (95.3) | 85.7 |
| Yes: | 136 (2.5) | 0.8 |
| <2 | 113 (2.1) | NA |
| ≥2 | 23 (0.4) | NA |
| Unknown or not stated | 120 (2.2) | 13.6 |
| Gestational age of infants (weeks): | ||
| <37 | 77 (1.4) | — |
| 37-41 | 4834 (89.2) | 91.7 |
| ≥42 | 361 (6.7) | 8.3 |
| Birthweight (g): | ||
| <2501 | 60 (1.1) | 2.4 |
| 2501-3999 | 3787 (69.8) | 86.5 |
| ≥4000 | 1319 (24.3) | 11.1 |
NA=Not available.
Percentages do not always add up to 100 owing to missing values.
Based on data from birth certificates for all 3 360 868 such births. Data reported by National Center for Health Statistics.10
Based on midwife's evaluation.
Transfers to hospital
Of the 5418 women, 655 (12.1%) were transferred to hospital intrapartum or post partum. Table 2 describes the transfers according to timing, urgency, and reasons for transfer. Five out of every six women transferred (83.4%) were transferred before delivery, half (51.2%) for failure to progress, pain relief, or exhaustion. After delivery, 1.3% of mothers and 0.7% of newborns were transferred to hospital, most commonly for maternal haemorrhage (0.6% of total births), retained placenta (0.5%), or respiratory problems in the newborn (0.6%). The midwife considered the transfer urgent in 3.4% of intended home births. Transfers were four times as common among primiparous women (25.1%) as among multiparous women (6.3%), but urgent transfers were only twice as common among primparous women (5.1%) as among multiparous women (2.6%).
Table 2.
Transfers to hospital among 5418 women intending home births with a certified professional midwife in the United States, 2000, according to timing, urgency, and reasons
| Variable | No (%) needing urgent transfer | No (%) needing transfer |
|---|---|---|
| Timing of transfers | ||
| Stage before delivery: | ||
| 1st* | 62 (1.1) | 380 (7.0) |
| 2nd* | 51 (0.9) | 134 (2.5) |
| Not specified | 4 (0.1) | 32 (0.6) |
| After delivery: | ||
| Maternal transfers | 43 (0.8) | 72 (1.3) |
| Newborn transfers | 25 (0.5) | 37 (0.7) |
| All | 185 (3.4) | 655 (12.1) |
| Reasons for transfer† | ||
| During labour: | ||
| Failure to progress in 1st stage | 4 (0.1) | 227 (4.2) |
| Failure to progress in 2nd stage | 12 (0.2) | 80 (1.5) |
| Pain relief | 4 (0.1) | 119 (2.2) |
| Maternal exhaustion | 1 (<0.1) | 112 (2.1) |
| Malpresentation | 20 (0.4) | 94 (1.7) |
| Thick meconium | 13 (0.2) | 49 (0.9) |
| Sustained fetal distress | 31 (0.6) | 49 (0.9) |
| Baby's condition | 5 (0.1) | 21 (0.4) |
| Prolonged or premature rupture of membranes | 0 | 19 (0.4) |
| Placenta abruptio or placenta previa | 5 (0.1) | 10 (0.2) |
| Haemorrhage | 5 (0.1) | 7 (0.1) |
| Pre-eclampsia or hypertension | 5 (0.1) | 13 (0.2) |
| Cord prolapse | 3 (0.1) | 6 (0.1) |
| Breech | 1 (<0.1) | 3 (0.1) |
| Other | 9 (0.2) | 17 (0.3) |
| Post partum: | ||
| Newborn transfers: | ||
| Respiratory problems | 14 (0.3) | 33 (0.6) |
| Evaluation of anomalies | 2 (<0.1) | 8 (0.1) |
| Other reasons | 9 (0.2) | 17 (0.3) |
| Maternal transfers: | ||
| Haemorrhage | 21 (0.4) | 34 (0.6) |
| Retained placenta | 14 (0.3) | 28 (0.5) |
| Suturing or repair of tears | 1 (<0.1) | 14 (0.2) |
| Maternal exhaustion | 2 (<0.1) | 4 (0.1) |
| Other reasons | 5 (0.1) | 8 (0.1) |
104 of these women were transferred to hospital after midwives' first assessment of labour (1.9% of labours), 38 of which were considered urgent.
Totals for urgent transfers are based on primary reason for transport only, but column for all transfers adds up to more than number transported as both primary and secondary reason (if reported) for transport to hospital are presented.
Medical interventions
Individual rates of medical intervention for home births were consistently less than half those in hospital, whether compared with a relatively low risk group (singleton, vertex, 37 weeks or more gestation) that will have a small percentage of higher risk births or the general population having hospital births (table 3). Compared with the relatively low risk hospital group, intended home births were associated with lower rates of electronic fetal monitoring (9.6% versus 84.3%), episiotomy (2.1% versus 33.0%), caesarean section (3.7% versus 19.0%), and vacuum extraction (0.6% versus 5.5%). The caesarean rate for intended home births was 8.3% among primiparous women and 1.6% among multiparous women.
Table 3.
Intervention rates for 5418 planned home births attended by certified professional midwives and hospital births in the United States
| Intervention | No (%) of intended home births with certified professional midwives in US, 2000 (n=5418) | Singleton, vertex births at ≥37 weeks gestation in US, 2000*(n=3 360 868) (%) | Survey of singleton births in all risk categories in US, 2000-1†(n=1583) (%) |
|---|---|---|---|
| Electronic fetal monitoring | 520 (9.6) | 84.3 | 93 |
| Intravenous | 454 (8.4) | NR | 85 |
| Artificial rupture of membranes | 272 (5.0) | NR | 67 |
| Epidural | 254 (4.7) | NR | 63 |
| Induction of labour‡ | 519 (9.6) | 21.0 | 44 |
| Stimulation of labour | 498 (9.2) | 18.9 | 53 |
| Episiotomy | 116 (2.1) | 33.0 | 35 |
| Forceps | 57 (1.0) | 2.2 | 3 |
| Vacuum extraction | 32 (0.6) | 5.2 | 7 |
| Caesarean section | 200 (3.7) | 19.0 | 24 |
NR=not reported on birth certificate.
Based on data from birth certificates for all 3 360 868 such births in United States in 2000. Data reported by National Center for Health Statistics.10 This subset of birthing women would generally be low risk, but would include a small percentage of higher risk women who would likely require more medical intervention.
Results from listening to mothers survey, October 2002. Percentages weighted to reflect US population of birthing women, aged 18-44.5 Includes about 20% of women not at low risk who may experience higher intervention rates.
For certified professional midwives 2000 study and listening to mothers survey, both attempted and successful inductions were reported; for US birth certificate data only successful inductions are reported.
Outcomes
No maternal deaths occurred. After we excluded four stillborns who died before labour but whose mothers still chose home birth, and three babies with fatal birth defects, five deaths were intrapartum and six occurred during the neonatal period (see box). This was a rate of 2.0 deaths per 1000 intended home births. The intrapartum and neonatal mortality was 1.7 deaths per 1000 low risk intended home births after planned breeches and twins (not considered low risk) were excluded. The results for intrapartum and neonatal mortality are consistent with most North American studies of intended births out of hospital11-24 and low risk hospital births (table 4).14,21,22,24-30
Table 4.
Combined intrapartum and neonatal mortality in studies of planned out of hospital births or low risk hospital births in North America (at least 500 births)
| Type of studies and references | Location, period | No of births | Combined intrapartum and neonatal mortality (per 1000)* |
|---|---|---|---|
| Low risk out of hospital births attended by midwives: | |||
| Burnett et al11 | North Carolina, 1974-6 | 934 | 3.0† |
| Mehl et al12 | United States, 1977 | 1146 | 3.5 |
| Schramm et al13 | Missouri, 1978-84 | 1770 | 2.8 |
| Janssen et al14 | Washington State, 1981-90 | 6944 | 1.7† |
| Sullivan and Beeman15 | Arizona, 1983 | 1243 | 2.4 |
| Tyson16 | Canada, Toronto, 1983-8 | 1001 | 2.0† |
| Hinds et al17 | Kentucky, 1985 | 575 | 3.5† |
| Durand18 | Farm, Tennessee, 1972-92 | 1707 | 2.3 |
| Rooks et al19 | 84 birth centres across United States, 1985-7 | 11 814 | 0.6 |
| Anderson et al20 | 90 home birth practices across United States, 1987-91 | 11 081 | 0.9 |
| Pang et al21 | Washington State, 1989-96 | 6133 | 2.0† |
| Schlenzka22 | California, 1989-90 | 3385 | 2.4 |
| Murphy et al23 | United States, 1993-5 | 1350 | 2.5 |
| Janssen et al24 | Canada, British Columbia, 1998-9 | 862 | 2.3 |
| Johnson and Daviss37 | United States and Canada, 2000 | 5418 | 1.7 |
| Low risk births attended by physicians or obstetricians in hospitals:
|
|
|
|
| Neutra et al25 | One academic hospital in Boston (lowest risk women), 1969-75 | 12 055 | 0.5-1.1† |
| Amato26 | One community hospital, 1974-5 | 4144 | 3.4† |
| Adams27 | 15 hospitals | 10 521 | 1.7 |
| Rooks et al28 | National natality survey, 1980 | 2935 | 2.5† |
| Janssen et al14 | Washington, 1981-90 | 23 596 | 1.7† |
| Leveno et al29 | One academic hospital in Dallas, 1982-5 | 14 618 | 1.0 |
| Eden et al30 | Twelve hospitals Illinois, 1982-5 | 8135 | 1.9 |
| Pang et al21 | Washington State, 1989-96 | 10 593 | 0.7† |
| Schlenzka22 | California 1989-90 | 806 402 | 1.9 |
| Janssen et al24 | Canada, British Columbia, 1998-9 | 733 | 1.4 |
Table is presented for general comparison only. Direct comparison of relative mortality between individual studies is ill advised. as many rates are unstable because of small numbers of deaths, study designs may differ (retrospective versus prospective, assessment and definition of low risk, etc.), the ability to capture and extract late neonatal mortality differs between studies, and significant differences may exist in populations studied with respect to factors such as socioeconomic status, distribution of parity, and risk screening criteria used. For example, see the study by Schlenzka. Although the crude mortality for low risk babies weighing over 2500 g intended at home was 2.4 per 1000 and intended in hospital was 1.9 per 1000, when standard methods were employed to adjust for differences in risk profiles of the two groups (indirect standardisation and logistic regression), both methods showed slightly lower risk for intended home births.
Excludes lethal congenital anomalies.
Neonatal mortality only, intrapartum mortality unreported.
Breech and multiple births at home are controversial among home birth practitioners. Among the 80 planned breeches at home there were two deaths and none among the 13 sets of twins. In the 694 births (12.8%) in which the baby was born under water, there was one intrapartum death (birth at 41 weeks, five days) and one fatal birth defect death.
Apgar scores were reported for 94.5% of babies; 1.3% had Apgar scores below 7 at five minutes. Immediate neonatal complications were reported for 226 newborns (4.2% of intended home births). Half the immediate neonatal complications concerned respiratory problems, and 130 babies (2.4%) were placed in the neonatal intensive care unit.
Health in first six weeks post partum
Health problems in the six weeks post partum were reported for 7% of newborns. Among the 5200 (96%) mothers who returned for the six week postnatal visit, 98.3% of babies and 98.4% of mothers reported good health, with no residual health problems. At six weeks post partum, 95.8% of these women were still breast feeding their babies, 89.7% exclusively.
Outcome validation and client satisfaction
Among the stratified, random 10% sample of women contacted directly by study staff to validate birth outcomes, no new transfers to hospital during or after the birth were reported and no new stillbirths or neonatal deaths were uncovered. Mothers' satisfaction with care was high for all 11 measures, with over 97% reporting that they were extremely or very satisfied. For a subsequent birth, 89.6% said they would choose the same midwife, 9.1% another certified professional midwife, and 1.7% another type of caregiver.
Discussion
Women who intended at the start of labour to have a home birth with a certified professional midwife had a low rate of intrapartum and neonatal mortality, similar to that in most studies of low risk hospital births in North America. A high degree of safety and maternal satisfaction were reported, and over 87% of mothers and neonates did not require transfer to hospital.
A randomised controlled trial would be the best way to tackle selection bias of mothers who plan a home birth, but a randomised controlled trial in North America is unfeasible given that even in Britain, where home birth has been an incorporated part of the healthcare system for some time, and where cooperation is more feasible, a pilot study failed.31 Prospective cohort studies remain the most comprehensive instruments available.
Our results for intrapartum and neonatal mortality are consistent with most other North American studies of intended births out of hospital and studies of low risk hospital birth (table 4). A meta-analysis2 and the latest research in Britain,3,4,32 Switzerland,33 and the Netherlands34 have reinforced support of home birth. Researchers reported high overall perinatal mortality in a study of home birth in Australia,35 qualifying that low risk home births in Australia had good outcomes but that high risk births gave rise to a high rate of avoidable death at home.36 Two prospective studies in North America found positive outcomes for home birth,23,24 but the studies were not of sufficient size to provide relatively stable perinatal death rates. None of this evidence, including ours, is consistent with a study in Washington State based on birth certificates.21 That study reported an increased risk with home birth but lacked an explicit indication of planned place of birth, creating the potential inclusion of high risk unplanned, unattended home births.28,37
Our study has several strengths. Internationally it is one of the few, and the largest, prospective studies of home birth, allowing for relatively stable estimates of risk from intrapartum and neonatal mortality. We accurately identified births planned at home at the start of labour and included independent verification of birth outcomes for a sample of 534 planned home births. We obtained data from almost 400 midwives from across the continent.
Regardless of methodology, residual confounding of comparisons between home and hospital births will always be a possibility. Women choosing home birth (or who would be willing to be randomised to birth site in a randomised trial) may differ for unmeasured variables from women choosing hospital birth. For example, women choosing home birth may have an advantageous enhanced belief in their ability to give birth safely with little medical intervention. On the other hand, women who choose hospital birth may have a psychological advantage in North America associated with not having to deal with the social pressure and fears of spouses, relatives, or friends from their choice of birth place.
Our results may be generalisable to a larger community of direct entry midwives. The North American Registry of Midwives was created in 1987 to develop the certified professional midwife credential—a route for formal certification for midwives involved in home birth who were not nurse midwives and who came from diverse educational backgrounds. Thus the women who chose to become certified professional midwives were a subset of the larger community of direct entry midwives in North America whose diverse educational backgrounds and midwifery practice were similar to certified professional midwives. From 1993 to 1999, using an earlier iteration of the data form, we collected largely retrospective data on a voluntary basis mainly from direct entry midwives involved with home births approached through the Midwives Alliance of North America Statistics and Research Committee and the Canadian Midwives Statistics' Collaboration. This earlier unpublished data of over 11 000 planned home births showed similar demographics, rates of intervention, transfers to hospital, and adverse outcomes.
As with the prospective US national birth centre study19 and the prospective US home birth study,23 the main study limitation was the inability to develop a workable design from which to collect a national prospective low risk group of hospital births to compare morbidity and mortality directly. Forms for vital statistics do not reliably collect the information on medical risk factors required to create a retrospective hospital birth group of precisely comparable low risk,38-40 and hospital discharge summary records for all births are not nationally accessible for sampling and have some limitations, being primarily administrative records.
One exception, and an important adjunct to our study, was Schlenzka's study in California.22 In this PhD thesis, Schlenzka was able to establish a large defined retrospective cohort of planned home and hospital births with similar low risk profiles, because birth and death certificates in California include intended place of birth and these had been linked to hospital discharge abstracts for 1989-90 for a caesarean section study. When the author compared 3385 planned home births with 806 402 low risk hospital births, he consistently found a non-significantly lower perinatal mortality in the home birth group. The results were consistent regardless of liberal or more restrictive criteria to define low risk, and whether or not the analysis involved simple standardisation of rates or extensive adjustment for all potential risk variables collected.22
An economic analysis found that an uncomplicated vaginal birth in hospital in the United States cost on average three times as much as a similar birth at home with a midwife41 in an environment where management of birth has become an economic, medical, and industrial enterprise.42 Our study of certified professional midwives suggests that they achieve good outcomes among low risk women without routine use of expensive hospital interventions. Our results are consistent with the weight of previous research on safety of home birth with midwives internationally. This evidence supports the American Public Health Association's recommendation8 to increase access to out of hospital maternity care services with direct entry midwives in the United States. We recommend that these findings be taken into account when insurers and governing bodies make decisions about home birth and hospital privileges with respect to certified professional midwives.
Categories of intrapartum and postpartum deaths (n=14) among 5418 women intending at start of labour to deliver at home
Intrapartum deaths (n=5)
Term pregnancy, transferred in first stage, cord prolapse discovered with artificial rupture of membranes in hospital
Term pregnancy, breech transported in second stage because of decelerations, delivered during transport
Term pregnancy, breech, transport after birth at home
Term pregnancy, 41 weeks five days. Subgaleal, subdural, subarachnoid haemorrhage. No fetal heart irregularities detected with routine monitoring. Apgar scores 1 and 0
Post-term pregnancy at 42 weeks three days, nuchal cord 6X and a true knot
Neonatal deaths (n=9)
Lethal congenital anomalies (n = 3):
Dwarf and related anomalies
Acrocallosal syndrome
Trisomy 13 Other causes (n = 6):
Term pregnancy, average labour. Apgar scores 6/2. Transported immediately, died at  hours of age in hospital. Autopsy said “mild medial hypertrophy of the pulmonary arterioles which suggest possible persistent pulmonary hypertension of a newborn or persistent fetal circulation...some authorities would argue this is a SIDS and others disagree based on the age. Regardless, infant suffered hypoxia and cardiopulmonary arrest”
hours of age in hospital. Autopsy said “mild medial hypertrophy of the pulmonary arterioles which suggest possible persistent pulmonary hypertension of a newborn or persistent fetal circulation...some authorities would argue this is a SIDS and others disagree based on the age. Regardless, infant suffered hypoxia and cardiopulmonary arrest”
Term pregnancy, Apgar scores 9/10. Suddenly stopped breathing at 15 hours of age. Died at five days in hospital, sudden infant death syndrome
Term pregnancy, transport at first assessment because of decelerations, rupture of vasa previa before membranes ruptured, caesarean section, died in hospital two days after birth
Term pregnancy, Apgar scores 9/10. Baby died at 26 hours. Sudden infant death syndrome
Post-term pregnancy, 42 weeks two days age based on clinical data as mother not aware of last menstrual period and refused ultrasonography. One deceleration during second stage, which resolved with position change. Apgar scores 3/2. Brain damage associated with anoxia, baby died at 16 days
Term pregnancy. Mother and baby transported to hospital because mother, not baby, seemed ill, but both discharged within 24 hours. Mother, not baby, given antibiotics by physician a few days after the birth for general sickness. Baby readmitted from home at 16 days because of nursing problems, died at 19 days of previously undetected Group B streptococcus
What is already known on this topic
Planned home births for low risk women in high resource countries where midwifery is well integrated into the healthcare system are associated with similar safety to low risk hospital births
Midwives involved with home births are not well integrated into the healthcare system in the United States
Evidence on safety of such home births is limited
What this study adds
Planned home births with certified professional midwives in the United States had similar rates of intrapartum and neonatal mortality to those of low risk hospital births
Medical intervention rates for planned home births were lower than for planned low risk hospital births
We thank the North American Registry of Midwives Board for helping facilitate the study; Tim Putt for help with layout of the data forms; Jennesse Oakhurst, Shannon Salisbury, and a team of five others for data entry; Adam Slade for computer programming support; Amelia Johnson, Phaedra Muirhead, Shannon Salisbury, Tanya Stotsky, Carrie Whelan, and Kim Yates for office support; Kelly Klick and Sheena Jardin for the satisfaction survey; members of our advisory council (Eugene Declerq (Boston University School of Public Health), Susan Hodges (Citizens for Midwifery and consumer panel of the Cochrane Collaboration's Pregnancy and Childbirth Group), Jonathan Kotch (University of North Carolina Department of Maternal and Child Health),, Patricia Aikins Murphy (University of Utah College of Nursing), and Lawrence Oppenheimer (University of Ottawa Division of Maternal Fetal Medicine); and the midwives and mothers who agreed to participate in the study.
Contributors: KCJ and B-AD designed the study, collected and analysed the data, and prepared the manuscript. KCJ is guarantor for the paper.
Funding: The Benjamin Spencer Fund provided core funding for this project. The Foundation for the Advancement of Midwifery provided additional funding. Their roles were purely to offset the costs of doing the research. This work was not done under the auspices of the Public Health Agency of Canada or the International Federation of Gynecology and Obstetrics and the views expressed do not necessarily represent those of these agencies.
Competing interests: None declared.
Ethical approval: Ethical approval was obtained from an ethics committee created for the North American Registry of Midwives to review epidemiological research involving certified professional midwives.
References
- 1.Springer NP, Van Weel C. Home birth. BMJ 1996;313: 1276-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Olsen O. Meta-analysis of the safety of home birth. Birth 1997;24: 4-13. [DOI] [PubMed] [Google Scholar]
- 3.Macfarlane A, McCandlish R, Campbell R. Choosing between home and hospital delivery. There is no evidence that hospital is the safest place to give birth. BMJ 2000;320: 798. [PubMed] [Google Scholar]
- 4.Campbell R, Macfarlane A. Where to be born: the debate and the evidence. 2nd ed. Oxford: National Perinatal Epidemiology Unit, 1994.
- 5.Declercq ER, Sakala C, Corry MP, Applebaum S, Risher P. Listening to mothers: report of the first national US survey of women's childbearing experiences [monograph]. New York: Maternity Center Association, 2002. www.maternitywise.org/listeningtomothers/ (accessed 3 Apr 2005).
- 6.College of Physicians and Surgeons of Ontario. Reports from council. Home birth policy rescinded. Toronto: CPSO, 2001.
- 7.Society of Obstetricians and Gynecologists of Canada. Policy statement No 126. Midwifery. J Obstet Gynecol Can 2003;25: 5. [Google Scholar]
- 8.American Public Health Association. 2001-3: increasing access to out-of-hospital maternity care services through state-regulated and nationally-certified direct-entry midwives. Am J Public Health 2002;92: 453-5. [Google Scholar]
- 9.American College of Obstetricians and Gynecologists. Frequently asked questions about having a baby in the 21st century [monograph]. Washington; 12 Dec 2001. www.acog.org/from_home/publications/press_releases/nr12-12-01-4.cfm (accessed 3 Apr 2005).
- 10.Martin JA, Hamilton BE, Ventura SJ, Mencaker F, Park MM. Births: final data for 2000. National vital statistics reports. Hyattsville, MD: National Center for Health Statistics, 2002;50(5). [PubMed]
- 11.Burnett CA III, Jones JA, Rooks J, Chen CH, Tyler CW Jr, Miller CA. Home delivery and neonatal mortality in North Carolina. JAMA 1980;244: 2741-5. [PubMed] [Google Scholar]
- 12.Mehl LE, Peterson GH, Whitt M, Hawes WE. Outcomes of elective home births: a series of 1146 cases. J Reprod Med 1977;19: 281-90. [PubMed] [Google Scholar]
- 13.Schramm WF, Barnes DE, Bakewell JM. Neonatal mortality in Missouri home births, 1978-84. Am J Public Health 1987;77: 930-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Janssen PA, Holt VL, Myers SJ. Licensed midwife-attended, out-of-hospital births in Washington state: are they safe? Birth 1994;21: 141-8. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan DA, Beeman R. Four years' experience with home birth by licensed midwives in Arizona. Am J Public Health 1983;73: 641-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tyson H. Outcomes of 1001 midwife-attended home births in Toronto, 1983-1988. Birth 1991;18: 14-9. [DOI] [PubMed] [Google Scholar]
- 17.Hinds MW, Bergeisen GH, Allen DT. Neonatal outcome in planned v unplanned out-of-hospital births in Kentucky. JAMA 1985;253: 1578-82. [PubMed] [Google Scholar]
- 18.Durand AM. The safety of home birth: the farm study. Am J Public Health 1992;82: 450-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rooks JP, Weatherby NL, Ernst EK, Stapleton S, Rosen D, Rosenfield A. Outcomes of care in birth centers. The National Birth Center study. N Engl J Med 1989;321: 1804-11. [DOI] [PubMed] [Google Scholar]
- 20.Anderson RE, Murphy PA. Outcomes of 11,788 planned home births attended by certified nurse-midwives. A retrospective descriptive study. J Nurse Midwifery 1995;40: 483-92. [DOI] [PubMed] [Google Scholar]
- 21.Pang JW, Heffelfinger JD, Huang GJ, Benedetti TJ, Weiss NS. Outcomes of planned home births in Washington State: 1989-1996. Obstet Gynecol 2002;100: 253-9. [DOI] [PubMed] [Google Scholar]
- 22.Schlenzka P. Safety of alternative approaches to childbirth. PhD thesis, California: Stanford University, 1999.
- 23.Murphy PA, Fullerton J. Outcomes of intended home births in nurse-midwifery practice: a prospective descriptive study. Obstet Gynecol 1998;92: 461-70. [DOI] [PubMed] [Google Scholar]
- 24.Janssen PA, Lee SK, Ryan EM, Etches DJ, Farquharson DF, Peacock D, et al. Outcomes of planned home births versus planned hospital births after regulation of midwifery in British Columbia. CMAJ 2002;166: 315-23. [PMC free article] [PubMed] [Google Scholar]
- 25.Neutra RR, Fienberg SE, Greenland S, Friedman EA. Effect of fetal monitoring on neonatal death rates. N Engl J Med 1978;299: 324-6. [DOI] [PubMed] [Google Scholar]
- 26.Amato JC. Fetal monitoring in a community hospital. A statistical analysis. Obstet Gynecol 1977;50: 269-74. [PubMed] [Google Scholar]
- 27.Adams JL. The use of obstetrical procedures in the care of low-risk women. Women Health 1983;8: 25-34. [DOI] [PubMed] [Google Scholar]
- 28.Rooks JP. Safety of out-of-hospital births in the United States. In: Midwifery and childbirth in America. Philadelphia: Temple University Press, 1997: 345-84.
- 29.Leveno KJ, Cunningham FG, Nelson S, Roark M, Williams ML, Guzick D, et al. A prospective comparison of selective and universal electronic fetal monitoring in 34 995 pregnancies. N Engl J Med 1986;315: 615-9. [DOI] [PubMed] [Google Scholar]
- 30.Eden RD, Seifert LS, Winegar A, Spellacy WN. Perinatal characteristics of uncomplicated postdate pregnancies. Obstet Gynecol 1987;69: 296-9. [PubMed] [Google Scholar]
- 31.Dowswell T, Thornton JG, Hewison J, Lilford RJ, Raisler J, Macfarlane A, et al. Should there be a trial of home versus hospital delivery in the United Kingdom? BMJ 1996;312: 753-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Northern Region Perinatal Mortality Survey Coordinating Group. Collaborative survey of perinatal loss in planned and unplanned home births. BMJ 1996;313: 1306-9. [PMC free article] [PubMed] [Google Scholar]
- 33.Ackermann-Liebrich U, Voegeli T, Gunter-Witt K, Kunz I, Zullig M, Schindler C, et al. Home versus hospital deliveries: follow up study of matched pairs for procedures and outcome. Zurich Study Team. BMJ 1996;313: 1313-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wiegers TA, Keirse MJ, van der ZJ, Berghs GA. Outcome of planned home and planned hospital births in low risk pregnancies: prospective study in midwifery practices in the Netherlands. BMJ 1996;313: 1309-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bastian H, Keirse MJ, Lancaster PA. Perinatal death associated with planned home birth in Australia: population based study. BMJ 1998;317: 384-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bastian H, Keirse MJ, Lancaster PA. Authors reply: Perinatal death associated with planned home birth in Australia. BMJ 1999;318: 605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Johnson KC, Daviss BA. Outcomes of planned home births in Washington State: 1989-1996. Obstet Gynecol 2003;101: 198-200. [PubMed] [Google Scholar]
- 38.Buescher PA, Taylor KP, Davis MH, Bowling JM. The quality of the new birth certificate data: a validation study in North Carolina. Am J Public Health 1993;83: 1163-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Piper JM, Mitchel EF Jr, Snowden M, Hall C, Adams M, Taylor P. Validation of 1989 Tennessee birth certificates using maternal and newborn hospital records. Am J Epidemiol 1993;137: 758-68. [DOI] [PubMed] [Google Scholar]
- 40.Woolbright LA, Harshbarger DS. The revised standard certificate of live birth: analysis of medical risk factor data from birth certificates in Alabama, 1988-92. Public Health Rep 1995;110: 59-63. [PMC free article] [PubMed] [Google Scholar]
- 41.Anderson RE, Anderson DA. The cost-effectiveness of home birth. J Nurse Midwifery 1999;44: 30-5. [DOI] [PubMed] [Google Scholar]
- 42.Perkins BB. The medical delivery business health reform, childbirth and the economic order. New Brunswick, NJ: Rutgers University Press, 2004.