Short abstract
Although relicensing of doctors is well established in the US, systems to evaluate competence rigorously are still some way off
Public pressure for accountability of doctors is increasing in the United States as it is in the United Kingdom. The release of several high profile reports in the 1990s regarding systems based errors and patient safety prompted US medical licensing and regulatory agencies to review their role in assuring the ability of healthcare practitioners to practise safely, not just at the point of initial licensure but over the course of their careers. Before effective systems to assess doctors' continuing competence can be implemented, however, medical licensing authorities need to establish what should be measured and how, and to consider the potential repercussions on medical regulation as a whole.
Figure 1.
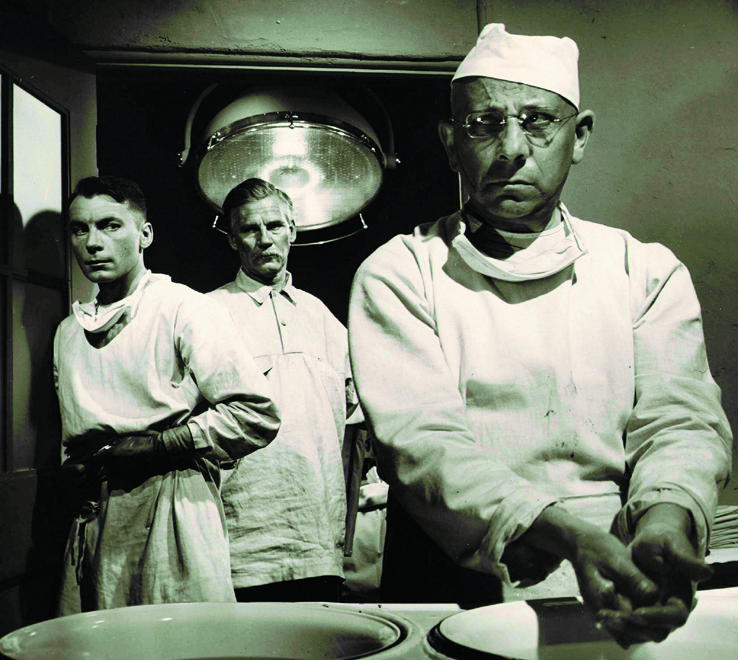
Is he fit for the job?
Credit: KOBAL COLLECTION
US licensing procedures
Medical licensure in the United States is granted by state licensing boards comprising doctors, other health care providers, and public representatives. The licensing board is charged by statute to ensure that only qualified, competent, and ethical doctors are licensed to practise medicine in that state. The medical boards also have a judicial role to protect citizens from being harmed by doctors who do not meet these qualifications or who violate standards of practice. To obtain a medical licence, a doctor must have completed a medical degree from a recognised or accredited medical school, postgraduate training in the United States, and a national, standardised medical licensing examination that includes assessment of clinical skills. Some states have additional requirements, such as passing a jurisprudence or medical ethics examination or a personal interview.
All doctors are required to reregister their licenses every one to three years, depending on the requirements of the state medical board. Currently, licensing authorities use various information sources to document and verify the competence of physicians seeking reregistration (also referred to as relicensure). The main tool is continuing medical education. However, licensing authorities also use hospital privilege reports,1 disciplinary data banks (Federation of State Medical Boards' board action data bank, healthcare integrity and protection data bank, and national practitioner data bank),2 patient complaints, and malpractice reports.1 Although the information currently available helps boards to assess doctors applying for relicensure, it falls short of comprehensive assessment of fitness to practise.
Impetus for change
During the 1990s, a taskforce of the Pew Charitable Trust Health Professions Commission released a series of reports aimed at improving the quality of health care and the profession's responsiveness to consumer safety. A focus of the reports was the regulation of healthcare providers as a means of ensuring high quality services. In its report Reforming Healthcare Workforce Regulation, the taskforce recommended that US states, “Require each licensing board to develop, implement and evaluate continuing competency requirements to assure the continuing competence of regulated health care professionals.”3
In November 1999, the Institute of Medicine released a report that focused on systems based errors in the medical community and made recommendations to improve patient safety.2 The report recommended that medical licensing boards periodically re-examine and relicense doctors “Based on both competence and knowledge of safety practices.” In response, many medical regulatory boards began to evaluate how they monitor doctors' competence.
Barriers to continued competence initiatives
Some professions, such as pharmacy, have attempted to implement continuing competence measures. However, the measures failed because of lack of support from practitioners and lack of trust in the measures and those proposing them.4 Although a few organisations, such as the American Board of Medical Specialties, are implementing programmes to assess practitioners' core competencies, most continue to struggle with how to effectively ensure continuing competence.
The most practical concern to medical licensing boards is determining what skills should be assessed for a doctor to show continued competence. Potential areas for inclusion are medical knowledge, clinical and communication skills, technical skills, professionalism, organisational skills or management of information (such as integration of technological advances into the practice environment), and ability to function in a group environment. A consensus on the definition of competence is essential for implementation of a reassessment programme.
The medical community will also need to determine whether the assessment of competence should focus on general medical skills or those relating to the doctor's specialty and what areas of practice or knowledge will be measured. The continuing medical education system will need to be re-evaluated and restructured (such as implementing interactive sessions, testing to show what participants have learnt, and evaluation of any resulting changes in practice). Another question for the profession is who should be responsible for initiating and implementing continued competence programmes. Should programmes be legislatively mandated or should the profession take a proactive approach?
Cost also needs considering, and the profession will need to decide if the cost of participation should be borne solely by the practitioner. Other key elements include deciding how often the practitioner should be evaluated, obtaining the profession's support, deciding what type of assessment tool(s) will be used, developing remediation programmes, and developing and implementing systems to evaluate and quantify the outcomes of such initiatives.
Implications of continued competence initiatives
Medical boards in the United States have neither the capability nor the resources to be solely responsible for evaluating all areas of a doctor's competence. Such assessment is best accomplished through collaboration with medical societies and other regulatory and certifying authorities. However, the role and responsibility of each organisation will need reviewing and clarifying so that the system is not duplicative or overly burdensome for doctors. Organisations must work together to develop tools and resources.
From a practical standpoint, medical licensing authorities must grapple with issues of how to implement ongoing competence programmes in a manageable fashion, to avoid having to assess all doctors simultaneously. Most importantly, boards must decide what the implications are if a doctor is unable to meet the board's criteria for competence.
The impact of such programmes on medical regulation as a whole must also be evaluated. Medical licensing authorities in the United States issue licenses that allow doctors to engage in the general, undifferentiated practice of medicine. Of particular interest to licensing authorities, then, is whether the evaluation of ongoing competence should occur at the general or specialty level. Would specialty specific reassessment move licensing authorities toward licensure by specialty? What are the implications of granting a doctor an initial license based on general medical knowledge and skills but then requiring him or her to maintain that licence based on specialty knowledge or skills?
The Institute of Medicine recommended that, “Professional licensing bodies consider continuing qualifications over a lifetime of practice, not just at initial licensure.”2 Clearly, licensing authorities recognise that implementing maintenance of licensure programmes is consistent with their mission and duty to protect the public, and is perhaps long overdue from a public safety perspective. However, implementation of an effective system will require boards to discuss and resolve these and other equally important questions.
What the licensing boards are doing
The Federation of State Medical Boards is the membership association of all 70 US medical licensure and regulation boards. In 1997, the federation commissioned a study of public awareness and attitudes about state medical boards. Results indicated that retesting of doctors was emerging as an important issue. It was the second most cited responsibility of state medical boards, with 9.3% of the public mentioning it “top-of-mind” (Federation of State Medical Boards, unpublished data, 1997). A 10% top-of-mind mention signals a national issue.
The federation established a committee in 2003 to make recommendations regarding a system for maintenance of licensure. The committee's first task was to develop a position statement that would declare the responsibility of state medical boards in assuring that doctors maintain competence over the course of their careers. Thus, in 2004, the federation adopted the following policy: “State medical boards have a responsibility to the public to ensure the ongoing competence of physicians seeking relicensure.”
The committee was also charged with developing strategies for state medical boards to use in implementing competency programmes. The committee's work has included investigation of current state statutes and board processes related to relicensure, identification of pertinent stakeholders, review of works in progress by other organisations and healthcare professions, assessment of potential for collaboration, and identification of the tools for assessing competence.
The first of a series of national summits, bringing together leaders from health care, industry, and government was held in March 2005. The purpose was to begin a dialogue on how to coordinate efforts across various fronts and to create a vision for self regulation of doctors that is responsive to the public's calls for increased accountability. The proceedings from the summit, following dissemination to the medical community and other stakeholders, will be used to develop recommendations for state medical boards on how to ensure the ongoing competence of licensed physicians.
Summary points
Pressure to ensure doctors remain fit to practise is growing in the US
Current relicensing procedures are inadequate for this purpose
Licensing authorities need to decide what should be evaluated and how
Focusing reassessment on specialty rather than general skills may have implications for medical regulation and licensure
This is the sixth in a series of articles examining regulation of doctors
Contributors and sources: The authors are all involved at a state and national level in policy regarding licensure and the regulation of medicine. Before joining the Federation of State Medical Boards (FSMB), JNT was dean and university vice president at Wake Forest University School of Medicine. RMB has served 13 years on the Alabama State Board of Medical Examiners and is on the FSMB's board of directors. She has been a member of the US Department of Health and Human Services Council on Graduate Medical Education, which makes recommendations on the nation's physician workforce needs, and is a member of the American Medical Association's council on ethical and judicial affairs. This article arose from efforts by the federation to address the continued competence of licensed physicians.
Competing interests: FEC and JNT are employed by the Federation of State Medical Boards (FSMB), which co-owns the United States Medical Licensing Examination, a national medical licensing examination accepted by state medical boards for initial licensure in the United States.
References
- 1.Wilson JA. Medical errors: how should medical boards be responding? J Med Licensure Discipline 2002;88: 76-80. [Google Scholar]
- 2.Institute of Medicine. To err is human: building a safer health system. Washington, DC: National Academy Press, 1999.
- 3.Finocchio LJ, Dower CM, McMahon T, Gragnola CM, Taskforce on Health Care Workforce Regulation. Reforming health care workforce regulation: policy considerations for the 21st century. San Francisco, CA: Pew Health Professions Commission, 1995.
- 4.LeBuhn RA, Swankin DA. Measuring competence of health care practitioners: where are we now—where are we headed? Proceedings of a Citizen Advocacy Center Conference, June 2000. Washington, DC: Citizen Advocacy Center; 2001.


