Abstract
Aims/Introduction
Previous reviews have revealed uncertainty regarding the effectiveness of home visit interventions for managing diabetes. Therefore, we carried out a quantitative systematic review and meta‐analysis to evaluate the effects of home visit interventions among patients with diabetes.
Materials and Methods
We searched various electronic databases (PubMed, EMBASE, Cochrane Library, Web of Science, CINAHL, Wanfang and Chinese scientific full‐text databases) from their inception until March 2016. We included randomized controlled trials that included patients with diabetes, and evaluated the effects of home visit programs on glycated hemoglobin concentrations. Two reviewers independently used the Cochrane Collaboration methods to assess the included studies’ risk of bias and quality.
Results
We included seven randomized controlled trials with 686 participants. Compared with the usual care, the home visit group showed a greater reduction in glycated hemoglobin concentrations (mean difference −0.79% [−9 mmol/mol], 95% confidence interval [CI]: −0.93 to −0.25% [11 to −3 mmol/mol]; P < 0.05; I 2 = 0%), systolic blood pressure (mean difference −5.94 mmHg, 95% confidence interval −11.34 to −0.54 mmHg) and diastolic blood pressure (mean difference −6.32 mmHg, 95% confidence interval −12.00 to −0.65 mmHg). Furthermore, home visits improved quality of life, high‐density lipoprotein, low‐density lipoprotein, total triglycerides and self‐management. However, there were no significant differences between the two groups in their bodyweight, total cholesterol, body mass index and self‐efficacy.
Conclusion
Home visits were associated with improved glycemic control and reduced cardiovascular risk factors, which shows that it is an effective method for diabetes management.
Keywords: Diabetes, Home visit, Meta‐analysis
Introduction
Diabetes mellitus is a chronic disease with a multifactorial pathogenesis and etiology that are related to the complex interactions between genetic and environmental factors1, 2, 3, 4. Increased life expectancy, a sedentary lifestyle and a poor diet have also contributed to the higher rates of type 2 diabetes mellitus worldwide5. In 2013, an estimated 382 million people had type 2 diabetes mellitus, and this figure is estimated to increase to 592 million in 20356, which will likely increased the overall financial burden of diabetes7. In 2012, the total economic burden of diabetes was >$322 billion in the USA8, and this burden is 48% greater than the $218 billion estimate for 20079. The risk of cardiovascular disease also increases with fasting blood glucose levels, even for levels that do not qualify for a diagnosis of diabetes10, and diabetes can also lead to damage to the kidneys, nerves and eyes, which can create further complications. Thus, chronic complications of type 2 diabetes mellitus progression reduce individuals’ quality of life, create a heavy burden on healthcare systems and increase mortality11, 12, 13.
Different interventions have been developed to control diabetes in primary care without satisfactory results14, 15, 16, 17, showing the need for new strategies for management of this disease. Home visits are considered an economical and effective method for preventing and controlling chronic diseases, as they can provide benefits for the patient, their family and society in general, as well as improve the quality of life among old patients with chronic disease18, 19, 20. This comprehensive and humanized approach to care seeks to improve the patient's knowledge regarding the pathology, which connects them with their treatment and allows them to assume autonomous responsibility for their health21. Furthermore, numerous recent meta‐analyses have shown that nurse‐led interventions can enhance diabetes outcomes22, 23, 24, 25, 26. Nevertheless, there is no clear international evidence regarding the effectiveness of home visit programs for diabetes management, despite their promising results for other conditions. A comparable systematic review and meta‐analysis is currently available in the literature. Therefore, the present quantitative systematic review and meta‐analysis was carried out to evaluate whether home visit programs were an effective method for diabetes management.
Methods
Literature search
We carried out a search of various electronic databases (PubMed, EMBASE, Cochrane Library, Web of Science, CINAHL, Wanfang and Chinese scientific full‐text databases) for randomized controlled trials (RCTs) that evaluated diabetes and home visit programs, and were published between the databases’ inception and March 2016. The search terms were: ‘diabetes mellitus,’ ‘hyperglycemia,’ ‘high blood sugar,’ ‘high blood glucose,’ ‘house call,’ ‘home visit’ and ‘randomized controlled trial.’ The detailed search algorithms are showed in Appendix S1.
Study selection
Two reviewers independently scanned the titles and abstracts, assessed the eligible trials according to the pre‐specified criteria, and assessed the methodological quality of the included trials. Trials that were potentially suitable for inclusion were retrieved for a full‐text review. Any disagreements regarding study inclusion were resolved by discussion. The inclusion criteria were: (i) the participants had to be diagnosed with diabetes mellitus; (ii) the study compared home visits and usual care (usual care contains health education leaflets or pamphlets regarding hypertension); (iii) the primary outcome measures were changes in glycated hemoglobin (HbA1c) levels at the end of the active intervention. The secondary outcome measures were defined as changes in blood pressure (BP), body mass index (BMI), waist circumference, weight, quality of life and levels of high‐density lipoprotein (HDL), low‐density lipoprotein (LDL), triglycerides (TG), total cholesterol (TC) and cost‐effectiveness; (iv) the study used an RCT design (regardless of blinding status); and (v) the full text was published in English or Chinese.
Data extraction and quality appraisal
Two authors independently extracted data from the included studies using standardized electronic forms. Disagreements regarding the data extraction were settled through discussion and consensus of the study group. The extracted data included study design, methodological evaluation, interventions and outcomes, the studied population, and sample size. The studies’ corresponding authors were contacted in cases of missing data.
The Cochrane Collaboration methods were used by two reviewers to independently evaluate study quality and the risk of bias27, based on the studies’ sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting and other sources of biases28, 29. Disagreements were resolved by the study group. According to the Cochrane Collaborations Handbook (version 5.2), each quality factor was classified as yes (low risk of bias), no (high risk of bias) or unclear (moderate risk of bias).
Statistical analysis
The data were pooled and analyzed using Review Manager (version 5.3; The Cochrane Collaboration, Oxford, UK) and Stata software (version 12.0; StataCorp, College Station, Texas, USA). Publication bias was examined based on a funnel plot using Begg's test and Egger's test. The changes in blood glucose were calculated based on the pre‐ and post‐intervention blood glucose values for the home visit interventions and usual care. For dichotomous variables, the intervention effects were calculated as relative risk (RR), and mean differences (MD) with 95% confidence intervals (CIs) were used for continuous variables. Heterogeneity was estimated using the χ2‐test (α = 0.1) and I² statistics (low heterogeneity: 25%, moderate heterogeneity: 50%, and high heterogeneity: 75%). When there was no significant heterogeneity among the studies (P > 0.1, I 2 < 50%), we used a fixed effects model, and a random effects model was used if significant heterogeneity was detected (P < 0.1, I 2 ≥ 50%). Differences were considered statistically significant at a P‐value of 0.05. The meta‐analysis was carried out using Review Manager software (version 5.2) and Stata software 12.0.
Results
Literature search
The searches identified 436 studies. There are 295 studies after duplicates were removed. A total of 273 studies were excluded after the initial screening of the titles and abstracts. The remaining 22 studies were subjected for full‐text review, and seven studies were considered eligible for this review (Figure 1).
Figure 1.
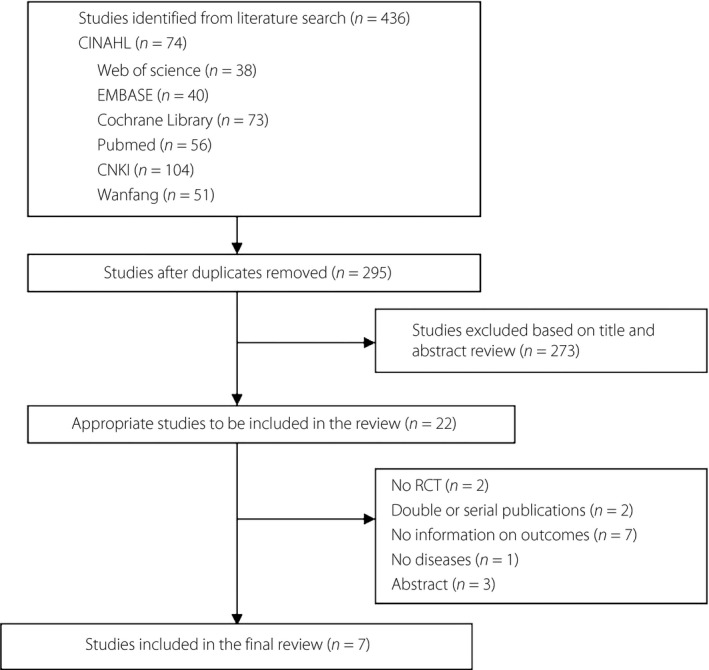
Flowchart of literature search. RCT, randomized controlled trial.
Study characteristics and risks of bias
Table 1 summarizes the main characteristics of the seven RCTs, which included the authors, setting, publication date, study location, sample size, mean age, sex distribution and study duration. The studies included 686 patients (335 patients received home visits, 351 patients received usual care), and were carried out in Canada (1 study), Thailand (1 study), Australia (1 study) and the USA (4 studies). The intervention durations ranged from 3 months to 2 years, and three studies reported outcomes at 6 months. Figure 2 shows the risks of bias for the included studies.
Table 1.
Characteristics of the included randomized controlled trials
| Study | Study location | Type of study | Setting | Sample size (n) | Sex (Female/Male) | Mean age range, years (SD) | Program duration (frequency) | Intervention group | Control group | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Home visit | Usual care | Home visit | Usual care | Home visit | Usual care | |||||||
| Couper (1999)30 | Australia | RCT | Home | 37 | 32 | 19/18 | 22/10 | 14.2 (1.7) | 14.3 (1.9) | 6 months (monthly) | Home visit | Usual care |
| Estey (2015)31 | Canada | RCT | Home | 28 | 25 | 11/17 | 11/14 | _ | _ | 3 months (2 weeks) | Home visit | Usual care |
| Rothschild (2014)32 | USA | RCT | Home | 73 | 71 | 47/26 | 50/21 | 53.76 (11.7) | 53.66 (12.7) | 2 years (20 days) | Home visit | Usual care |
| Spencer (2011)33 | USA | RCT | Home | 59 | 77 | 54/18 | 62/30 | 50 (5) | 55 (4) | 6 months (2 weeks) | Home visit | Usual care |
| Stroup (2003)34 | USA | RCT | Home | 30 | 40 | 20/10 | 17/23 | 58.6 (8.6) | 52.1 (21.2) | 2 years (monthly) | Home visit | Usual care |
| Taylor (2005)35 | USA | RCT | Home | 20 | 19 | 7/13 | 6/13 | 58 | 67 | 3 months (2 weeks) | Home visit | Usual care |
| Wattana (2007)36 | Thailand | RCT | Home | 75 | 72 | 60/15 | 52/20 | 58.40 (10.05) | 55.14 (10.22) | 24 weeks (–) | Home visit | Usual care |
RCT, randomized controlled trial; SD, standard deviation.
Figure 2.
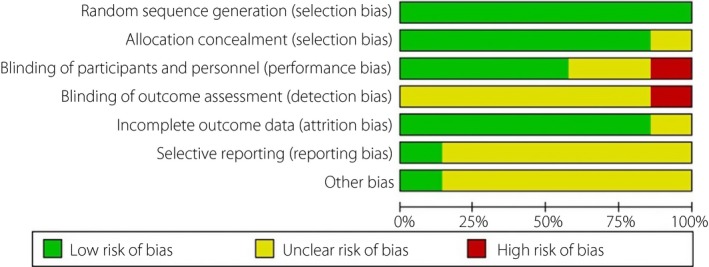
Risk of bias in the included studies.
Primary outcome measure
All seven RCTs30, 31, 32, 33, 34, 35, 36 (335 participants received home visits and 351 participants received usual care) evaluated changes in HbA1c, and a significant reduction in the post‐treatment HbA1c was observed for home visits, compared with usual care (MD −0.79% [−9 mmol/mol], 95% CI: −0.93 to −0.25% [11 mmol/mol to −3 mmol/mol]; P < 0.05; Figure 3). The I 2 statistic (0%) showed no heterogeneity among the seven trials.
Figure 3.
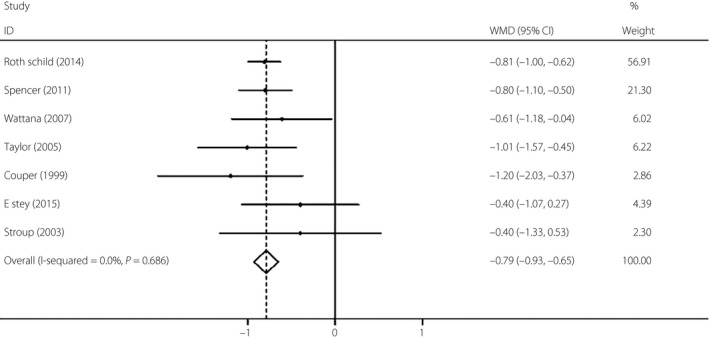
Change in glycated hemoglobin with home visits compared with usual care. WMD, weighted mean difference.
Secondary outcome measures
Among 273 participants in two trials35, 36, participants who received home visits showed significant improvements in quality of life, compared with participants who received usual care (MD 11.81, 95% CI: 7.20 to 16.42; P < 0.001; I 2 = 23%). Two trials34, 35 evaluated systolic blood pressure (SBP) and diastolic blood pressure (DBP) among 109 patients (59 patients received home visits, 50 patients received usual care). The two trials showed heterogeneity (P > 0.1), although the results indicated that home visits provided a significant reduction in SBP (MD −5.94 mmHg, 95% CI: −11.34 to −0.54 mmHg; P < 0.05) and DBP (MD −6.32 mmHg, 95% CI: −12.00 to −0.65 mmHg; P < 0.05). Improvements in fitness were accompanied by differences in post‐intervention bodyweight (123 participants from 2 trials31, 34; MD −5.06 kg, 95% CI: −12.61 to 2.48 kg; P = 0.19; I 2 = 16%) and BMI (164 participants from 1 trial33; MD 1 kg/m2, 95% CI: −0.13 to 2.13 kg/m2; P = 0.08; Table 2).
Table 2.
Summary of meta‐analyses of studies using home visits to manage diabetes
| Outcome measure | Trails | Sample size (intervention/control) | Measure of effects | Intervention effect size (95% CI) | P‐value of effect | Heterogeneity | |
|---|---|---|---|---|---|---|---|
| I 2 (%) | P‐value | ||||||
| SBP (mmHg) | 2 | 109 (59/50) | MD | −5.94 (−11.34, −0.54) | 0.03* | 0 | 0.001 |
| DBP (mmHg) | 2 | 109 (59/50) | MD | −6.32 (−12.00, −0.65) | 0.03* | 48 | 0.001 |
| Quality of life | 2 | 186 (95/91) | SMD | 11.81 (7.20, 16.42) | 0.001** | 23 | 0.25 |
| High density lipoprotein (mg/dL) | 2 | 109 (50/59) | MD | −5.11 (−9.80, −0.43) | 0.03* | 0 | 0.4 |
| Low density lipoprotein (mg/dL) | 2 | 109 (50/59) | MD | −10.12 (−18.23, −2.00) | 0.01** | 0 | 0.75 |
| Weight (kg) | 2 | 123 (58/65) | MD | −5.06 (−12.61, 2.48) | 0.19 | 16 | 0.28 |
| Total cholesterol (mg/dL) | 2 | 109 (50/59) | MD | −4.06 (−18.28, 10.17) | 0.58 | 0 | 0.93 |
| Total triglycerides (mg/dL) | 2 | 109 (50/59) | MD | 50.72 (15.69, 85.75) | 0.005** | 0 | 0.51 |
| Body mass index (kg/m2) | 1 | 164 (72/92) | MD | 1 (−0.13, 2.13) | 0.08 | NA | NA |
| Self‐efficacy | 1 | 120 (56/74) | MD | −1.80 (−5.37, 1.77) | 0.32 | NA | NA |
| Self‐management | 1 | 120 (56/74) | MD | 0.70 (0.51, 0.89) | 0.001** | NA | NA |
*P < 0.05, **P < 0.01. Heterogeneity (I 2): <50% = low, 50–75% = moderate, >75% = high. CI, confidence intervals; MD, mean difference; NA, not applicable; SMD, standardized mean difference.
Just two trials34, 35 evaluated cardiovascular risk factors (levels of HDL, LDL, TG and TC) among 109 patients, and data for the outcomes were not consistently available for the studies. Except for TC, after an analysis with a fixed effects model of two trials34, 35, we achieved the result (MD −4.06 mg/dL, 95% CI: −18.28 to 10.17 mg/dL, P = 0.58), which showed no statistical significance between the two arms. However, home visits provided significant changes in HDL (MD −5.11 mg/dL, 95% CI: −9.80 to −0.43 mg/dL; P = 0.03; I 2 = 0), LDL (MD −10.12 mg/dL, 95% CI: −18.23 to −2.00 mg/dL; P = 0.01; I 2 = 0) and TG (MD 50.72 mg/dL, 95% CI: 15.69 to 85.75 mg/dL; P = 0.005; I 2 = 0; Table 2).
Only one trial that included 120 patients reported self‐efficacy and self‐management outcomes33. Home visits provided a significant difference in self‐management (MD 0.7, 95% CI: 0.51 to 0.89; P = 0.001), but not in self‐efficacy (MD −1.8, 95% CI: −5.37 to 1.77; P = 0.32; Table 2).
We identified there was no study in the literature providing economic analyses of home visit interventions. Because the home visit interventions with cost information differed (e.g., populations targeted, settings, targeted outcomes), determining the typical cost of a home visit intervention is challenging.
Publication bias
We did our best to design the study in order to minimize the publication bias. First, we made a comprehensive search strategy. Second, the inclusion criteria were executed strictly to selected papers. Third, publication bias was detected by several methods. The funnel plot did not identify any publication bias (Begg's test, P = 0.548; Egger's test, P = 0.623; Figure 4).
Figure 4.
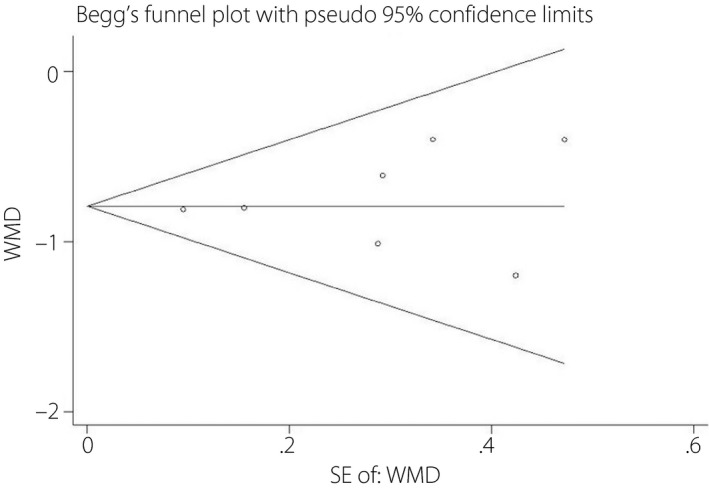
Funnel plot of the meta‐analysis. SE, standard error; WMD, weighted mean difference.
Discussion
To the best of our knowledge, this is the first meta‐analysis to evaluate the association between home visit programs and diabetes management. Compared with usual care, home visit interventions provided significant reductions of HbA1c, SBP, DBP, quality of life, HDL, LDL, TG and self‐management. However, the home visit interventions did not provide significant changes in bodyweight, TC levels, BMI and self‐efficacy. These findings are consistent with the findings of Schwedes et al.37. The absence of significant changes in BMI, bodyweight, TC levels and self‐efficacy might be related to the relatively brief duration of the home visits, which could limit their effect, as most studies used relatively short follow ups, and just two studies followed the participants for 2 years32, 34. Nevertheless, weight loss in obese patients with type 2 diabetes mellitus decreases hepatic glucose production, and improves insulin secretion and sensitivity. Furthermore, even a 5% reduction in weight significantly improves glycemic control (lower HbA1c levels) in obese patients with type 2 diabetes mellitus38. Therefore, future trials of biological and behavioral interventions should be designed with longer follow ups, in order to improve the probability of discovering changes and assessing the long‐term sustainability of blood glucose reductions.
The present findings suggest that home visit interventions have a favorable effect on glycemic control, with a pooled standardized mean reduction of 0.79% in HbA1c levels, compared with usual care. This finding has important implications for current public health, clinical practice and research, as glycemic control is an important predictor of the chronic complications of diabetes39, 40. For example, the United Kingdom Prospective Diabetes Study showed that each 1% reduction in HbA1c levels was associated with a 37% reduction in the risk of microvascular complications, a 14% reduction in the risk of myocardial infarction and a 21% reduction in the risk of diabetes‐related death, with no evidence of a threshold41. The sizes of these proportional reductions were broadly consistent across several major high‐risk patient groups42, which suggests that lowering blood glucose levels provides broad benefits. Therefore, the absolute reduction of 0.79% in HbA1c levels from the present study appears to be clinically significant. Furthermore, the effect from our meta‐analysis is likely underestimated, because the usual care that is provided in RCTs is often better than the usual care that is provided in clinical practice43. Furthermore, two trials in this meta‐analysis allowed control patients to receive low‐level diabetes education or access to some form of self‐management training, in addition to their usual care32, 36.
The present meta‐analysis aimed to examine the effects of home visit programs on measures of glycemic control and cardiometabolic risk factors. Our findings show that home visit programs are more effective for patients who have poor glycemic control, compared with other interventions, such as leisure‐time physical activities (a −0.6% change in HbA1c levels)44, disease‐management programs (−0.51%)43 and peer support (−0.57%)45. In these cases, home visits have emerged as an educational healthcare strategy, which teaches patients with diabetes how to achieve lifestyle changes, monitor their signs and symptoms, and record and interpret their blood glucose levels, blood pressure, and blood lipid levels. Nevertheless, the methods for the home visit interventions are typically multifaceted and complex, which creates difficulty in comparing home visit interventions. Therefore, future studies should develop interventions that are based on a structured treatment algorithm, and should likely compare the usual care that is provided by a primary care team and nurse‐led care. There are also large differences in the length and frequency of home visit interventions, and the role of these variations in the intervention should be explored. Therefore, home visits should be designed to consider the patients’ needs, encourage treatment adherence self‐care practices and increase autonomy46.
The results of the present meta‐analysis highlight two important topics for future research. First, it will be important to evaluate the cost‐effectiveness of home visit programs, especially the specific cost components or the year for which costs were estimated. Second, there is a need for high‐quality multicenter RCTs to more precisely evaluate the outcomes of home visit programs, such as self‐care adherence, patient satisfaction and insulin requirements.
The present meta‐analysis had two strengths. First, this is the first meta‐analysis to evaluate the effects of home visits on diabetes management. Second, the analysis showed that, compared with usual care, home visits led to reductions in HbA1c, SBP, DBP, HDL, LDL and TG among patients with diabetes. However, the present meta‐analysis also had two limitations. First, the calculation of the sample size was not mentioned for most studies, which might have resulted in underpowered analyses. Second, we only evaluated studies that were published in English or Chinese, and it is possible that we excluded relevant studies that were published in other languages. Third, the durations of the included studies seem to be relatively short, and it is not clear if the effectiveness of the home visit intervention was sustained after finishing the programs. Therefore, in the future study, we can consider the major concern about long duration effectiveness of the home visit intervention.
The findings of the present meta‐analysis suggest that home visit programs might be more effective at improving quality of life, self‐management, and levels of HbA1c, SBP, DBP, HDL‐LDL and TG. Despite its limitations, the present systematic review provided some important findings. First, lowering blood glucose levels into the normal range should therefore be routinely considered for the prevention of cardiovascular disease among those deemed to be of sufficient absolute risk. Second, there is a scarcity of high‐quality evidence regarding the effects of home visit programs on diabetes management. Therefore, additional studies are required to provide a greater body of evidence regarding the most clinically‐ and cost‐effective methods for using home visit programs to improve blood glucose control.
Disclosure
The authors declare no conflict of interest.
Supporting information
Appendix S1 ¦ The detailed search algorithms.
Acknowledgments
This study was supported by the National Nature Science Foundation of China (71363004; 71663002) and the Fundamental Research Funds for the Central Universities (grant 31920150046; lzujbky‐2016‐ct14).
J Diabetes Investig 2017; 8: 701–708
References
- 1. Pezzolesi MG, Nam M, Nagase T, et al Examination of candidate chromosomal regions for type 2 diabetes reveals a susceptibility locus on human chromosome 8p23.1. Diabetes 2004; 53: 486–491. [DOI] [PubMed] [Google Scholar]
- 2. Stumvoll M, Goldstein BJ, van Haeften TW. Type 2 diabetes: principles of pathogenesis and therapy. Lancet 2005; 365: 1333–1346. [DOI] [PubMed] [Google Scholar]
- 3. Zheng YY, Xie X, Ma YT, et al Relationship between type 2 diabetes mellitus and a novel polymorphism C698T in C5L2 in the Chinese Han population. Endocrine. 2012; 41: 296–301. [DOI] [PubMed] [Google Scholar]
- 4. Ovayolu O, Ovayolu N, Dogru A, et al The Challenge of Diabetes in the Elderly and Affecting Factors: a Turkish Study. Holist Nurs Pract 2015; 29: 272–279. [DOI] [PubMed] [Google Scholar]
- 5. Albuquerque AB, Bosi MLM. Visita domiciliar no âmbito da Estratégia Saúde da Família: percepções de usuários no Município de Fortaleza, Ceará, Brasil. Cad Saúde Pública 2009; 25: 1103–1112. [DOI] [PubMed] [Google Scholar]
- 6. Guariguata L, Whiting DR, Hambleton I, et al Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014; 103: 137–149. [DOI] [PubMed] [Google Scholar]
- 7. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010; 87: 4–14. [DOI] [PubMed] [Google Scholar]
- 8. American Diabetes Association. . Economic costs of diabetes in the U.S. In 2007. Diabetes Care 2008; 31: 596–615. [DOI] [PubMed] [Google Scholar]
- 9. Dall TM, Yang W, Halder P, et al The economic burden of elevated blood glucose levels in 2012: diagnosed and undiagnosed diabetes, gestational diabetes mellitus, and prediabetes. Diabetes Care 2014; 37: 3172–3179. [DOI] [PubMed] [Google Scholar]
- 10. WHO . Raised fasting blood glucose. 2016.
- 11. Solli O, Stavem K, Kristiansen IS. Health‐related quality of life in diabetes: the associations of complications with EQ‐5D scores. Health Qual Life Outcomes 2010; 8: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang W, Fu CW, Pan CY, et al How do type 2 diabetes mellitus‐related chronic complications impact direct medical cost in four major cities of urban China? Value Health 2009; 12: 923–929. [DOI] [PubMed] [Google Scholar]
- 13. Tharkar S, Devarajan A, Kumpatla S, et al The socioeconomics of diabetes from a developing country: a population based cost of illness study. Diabetes Res Clin Pract 2010; 89: 334–340. [DOI] [PubMed] [Google Scholar]
- 14. Renders CM, Valk GD, Griffin SJ, et al Interventions to improve the management of diabetes in primary care, outpatient, and community settings a systematic review. Diabetes Care 2001; 24: 1821–1833. [DOI] [PubMed] [Google Scholar]
- 15. Compean Ortiz LG, Del Angel Perez B, Resendiz Gonzalez E, et al Self‐care behaviors and glycemic control in low‐income adults in Mexico with type 2 diabetes mellitus may have implications for patients of Mexican heritage living in the United States. Clin Nurs Res 2016; 25: 120–138. [DOI] [PubMed] [Google Scholar]
- 16. Albikawi ZF, Petro‐Nustas W, Abuadas M. Self‐care Management Intervention to Improve Psychological Wellbeing for Jordanian Patients with Type Two Diabetes Mellitus. Issues Ment Health Nurs 2016; 37: 190–201. [DOI] [PubMed] [Google Scholar]
- 17. Bozorgmehr K, Szecsenyi J, Ose D, et al Practice network‐based care management for patients with type 2 diabetes and multiple comorbidities (GEDIMAplus): study protocol for a randomized controlled trial. Trials 2014; 15: 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pastor DK. Home sweet home: a concept analysis of home visiting. Home Healthc Nurse 2006; 24: 389–394. [DOI] [PubMed] [Google Scholar]
- 19. Caldera D, Burrell L, Rodriguez K, et al Impact of a statewide home visiting program on parenting and on child health and development. Child Abuse Negl 2007; 31: 829–852. [DOI] [PubMed] [Google Scholar]
- 20. Edraki M, Moravej H, Rambod M. Effect of home visit training program on growth and development of preterm infants: a double blind randomized controlled trial. Int J Community Based Nurs Midwifery 2015; 3: 12–22. [PMC free article] [PubMed] [Google Scholar]
- 21. Medeiros PAd, Pivetta HMF, Mayer MdS. Contribuições da visita domiciliar na formação em Fisioterapia. Trab educ saúde 2012; 10: 407–426. [Google Scholar]
- 22. Yardley JE, Hay J, Abou‐Setta AM, et al A systematic review and meta‐analysis of exercise interventions in adults with type 1 diabetes. Diabetes Res Clin Pract 2014; 106: 393–400. [DOI] [PubMed] [Google Scholar]
- 23. Iversen MM, Graue M, Leksell J, et al Characteristics of nursing studies in diabetes research published over three decades in Sweden, Norway, Denmark and Iceland: a narrative review of the literature. Scand J Caring Sci 2016; 30: 241–249. [DOI] [PubMed] [Google Scholar]
- 24. Clark CE, Smith LF, Taylor RS, et al Nurse‐led interventions used to improve control of high blood pressure in people with diabetes: a systematic review and meta‐analysis. Diabetic Med 2011; 28: 250–261. [DOI] [PubMed] [Google Scholar]
- 25. Neder S, Nadash P. Individualized education can improve foot care for patients with diabetes. Home Healthc Nurse 2003; 21: 837–840. [DOI] [PubMed] [Google Scholar]
- 26. Vermeire E, Wens J, Van Royen P, et al Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus. Cochrane Database System Rev 2005: p. Cd003638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated September 2008]. 2008.
- 28. Clark CE, Smith LF, Taylor RS, et al Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta‐analysis. BMJ (Clinical research ed) 2010; 341: c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. De Simoni A, Hardeman W, Mant J, et al Trials to improve blood pressure through adherence to antihypertensives in stroke/TIA: systematic review and meta‐analysis. J Am Heart Assoc 2013; 2: e000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Couper JJ, Taylor J, Fotheringham MJ, et al Failure to maintain the benefits of home‐based intervention in adolescents with poorly controlled type 1 diabetes. Diabetes Care 1999; 22: 1933–1937. [DOI] [PubMed] [Google Scholar]
- 31. Estey AL, Tan MH, Mann K. Follow‐up intervention: its effect on compliance behavior to a diabetes regimen. Diabetes Educ 1990; 16: 291–295. [DOI] [PubMed] [Google Scholar]
- 32. Rothschild SK, Martin MA, Swider SM, et al Mexican American trial of community health workers: a randomized controlled trial of a community health worker intervention for Mexican Americans with type 2 diabetes mellitus. Am J Public Health 2014; 104: 1540–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Spencer MS, Rosland AM, Kieffer EC, et al Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. Am J Public Health 2011; 101: 2253–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stroup J, Kane MP, Busch RS, et al The diabetes home visitation program. Am J Pharm Educ 2003; 67: 91. [Google Scholar]
- 35. Taylor KI. Promoting health in type 2 diabetes: nurse‐physician collaboration in primary care. Biol Res Nurs 2005; 6: 207–215. [DOI] [PubMed] [Google Scholar]
- 36. Wattana C, Srisuphan W, Pothiban L, et al Effects of a diabetes self‐management program on glycemic control, coronary heart disease risk, and quality of life among Thai patients with type 2 diabetes. Nurs Health Sci 2007; 9: 135–141. [DOI] [PubMed] [Google Scholar]
- 37. Schwedes U, Siebolds M, Mertes G. Meal‐related structured self‐monitoring of blood glucose: effect on diabetes control in non‐insulin‐treated type 2 diabetic patients. Diabetes Care 2002; 25: 1928–1932. [DOI] [PubMed] [Google Scholar]
- 38. Garvey WT, Ryan DH, Bohannon NJ, et al Weight‐loss therapy in type 2 diabetes: effects of phentermine and topiramate extended release. Diabetes Care 2014; 37: 3309–3316. [DOI] [PubMed] [Google Scholar]
- 39. Zoungas S, Chalmers J, Ninomiya T, et al Association of HbA1c levels with vascular complications and death in patients with type 2 diabetes: evidence of glycaemic thresholds. Diabetologia 2012; 55: 636–643. [DOI] [PubMed] [Google Scholar]
- 40. Hall GC, McMahon AD, Carroll D, et al Observational study of the association of first insulin type in uncontrolled type 2 diabetes with macrovascular and microvascular disease. PLoS One 2012; 7: e49908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Stratton IM, Adler AI, Neil HA, et al Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ (Clinical research ed) 2000; 321: 405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ettehad D, Emdin CA, Kiran A, et al Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta‐analysis. Lancet 2016; 387: 957–967. [DOI] [PubMed] [Google Scholar]
- 43. Pimouguet C, Le Goff M, Thiebaut R, et al Effectiveness of disease‐management programs for improving diabetes care: a meta‐analysis. CMAJ 2011; 183: E115–E127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pai LW, Li TC, Hwu YJ, et al The effectiveness of regular leisure‐time physical activities on long‐term glycemic control in people with type 2 diabetes: a systematic review and meta‐analysis. Diabetes Res Clin Pract 2016; 113: 77–85. [DOI] [PubMed] [Google Scholar]
- 45. Qi L, Liu Q, Qi X, et al Effectiveness of peer support for improving glycaemic control in patients with type 2 diabetes: a meta‐analysis of randomized controlled trials. BMC Pub Health 2015; 15: 471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Torres HdC, Santos LMd, Cordeiro PMCdS. Home visit: an educational health strategy for self‐care in diabetes. Acta Paulista de Enfermagem 2014; 27: 23–28. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 ¦ The detailed search algorithms.


