Summary
Introduction.
The present study aims to characterize personal attitudes and knowledge of a sample of Italian Occupational Physicians (OPh) towards Seasonal Influenza Vaccine (SIV) in healthcare workers (HCWs).
Methods.
In total, 92 OPh (42.4% males, 57.6% females, mean age of 47.3 ± 10.4 years, 50 specialists in Occupational Medicine, 42 specialists in Hygiene and Public Health) were asked about their attitudes towards influenza vaccine, their general knowledge of vaccine practice, their propensity towards vaccines and, eventually, their risk perception about the influenza and influenza vaccine was investigated. A regression analysis was then performed in order to better characterize predictive factors for vaccine propensity.
Results.
Influenza was recognized as a vaccination recommended for HCWs in 89/92 of the sampled OPh (96.7%). However, prevalence of misconceptions about vaccines was relatively high, with 26/92 (28.3%) and 24/92 (26.1%) referring vaccinations as eliciting allergic and autoimmune diseases, respectively and identifying lethargic encephalitis (18/92, 19.6%), autism (17/92, 18.5%), diabetes mellitus (15/92, 16.3%) and multiple sclerosis (13/92, 14.1%) as causatively vaccine-related. Propensity towards influenza vaccination found a significant predictor in the general knowledge (beta coefficient 0.213, p value = 0.043), risk perception (beta coefficient 0.252, p value = 0.018) and general propensity towards vaccinations (beta coefficient 0.384, p value = 0.002).
Discussion.
In spite of a diffuse propensity towards SIV, adherence of OPh was still < 50% of the sample. Moreover, sharing of misbeliefs and misconceptions was significant. As knowledge and risk perceptions were identified as significant predictors of vaccine propensity, our results suggest that information and training programs for OPh should be appropriately designed.
Key words: Healthcare workers, Influenza vaccine, Occupational physicians
Introduction
Seasonal influenza (SI) is a highly contagious vaccine preventable infectious disease (VPD), which can result in debilitating illness and potentially fatal complications in subjects at risk, representing a major public health problem with a heavy impact on National Healthcare Systems [1, 2]. Because of theirs professional duties, healthcare workers (HCWs) not only are at high risk of contracting SI, but also represent a significant source of transmission and circulation of the viruses in the community [3, 4]. SI vaccine (SIV) is safe and usually well-tolerated [5-8], and evidence suggests that policies involving immunization of HCWs may cost-effectively decrease employee absenteeism caused by SI. Moreover, by preventing its transmission between HCWs and patients, SIV would ultimately improve patient safety and decrease influenza- related morbidity and mortality [2, 9]. Since 1981, the United States Centers for Disease Control and Prevention (CDC) have therefore advised that HCWs will receive SIV [3, 10, 11], and in 2002 also the World Health Organization (WHO) began encouraging annual immunization where supported by national data and capacities, furtherly strengthening its recommendations during the 2009 H1N1 influenza pandemic [2, 5-8]. Nowadays, several European Public Health Authorities, such as the Italian National Health Service (in Italian: Servizio Sanitario Nazionale, SSN), have implemented SIV in HCWs through official recommendations (in Italy: National Immunization Prevention Plan / Piano Nazionale di Prevenzione Vaccinale or PNPV) [3, 7, 12-19]. However, vaccination coverage remains heterogeneous and usually unsatisfactory, with rates well below the minimum target of 75% required by the European Commission, as still ranging from about 15% to 50% in different countries [4, 15, 20-23]. Although Italian data on vaccination coverage among HCWs are not routinely available, recent studied have confirmed an inadequate compliance, suggesting that vaccination rates would have significantly declined since 2009 H1N1 pandemic, being presumptively well below 20% [7, 12 15, 19, 24, 25].
A number of studied have examined specific factors influencing SIV uptake by HCWs, identifying major barriers in system failures (e.g. stock-outs, limited availability of vaccination services in terms of time, places, etc.) and in individual factors such as: doubts regarding the preventive usefulness of vaccines and the rationale for vaccination, lack of knowledge regarding natural infection (i.e. actual risk for HCWs) and its potential consequences, misbelieves about vaccine-related risks and vaccine safety, as well as a diffuse lack of trust in the health policies and in the health authorities that promote them [2, 16, 26, 27]. In facts, a significant share of HCWs still understand SI as a mild illness not requiring a specific prophylaxis, and that contracting the disease is somehow safer than getting the vaccine [2, 16, 18, 25-31]. Collectively, aforementioned factors concur to the definition of vaccine hesitancy (VE), i.e. the continuum between full acceptance of vaccines with no doubts and the complete refusal with no doubts [28-31], and VE would in turn impair proactive behaviors, ultimately contributing to low vaccination rates [2, 16, 18, 25-31].
Occupational Physicians (OPh) are the medical professionals responsible for health promotion on the workplaces [32], and may actively contribute to overcome false attitudes and misconceptions supporting VE. Moreover, OPh inform the workers about the pros and cons of recommended vaccinations, and may therefore undermine or even remove the mutual misunderstanding between public health professionals and vaccine hesitant individuals, eventually maximizing the consent for vaccination programs [32]. Unfortunately, although numerous studies have assessed knowledge, attitudes and practices (KAP) of specific occupational groups regarding vaccinations, and such interventions have been proven as quite efficient in designing appropriate vaccination campaigns, ultimately improving immunization rates [20, 23, 26, 33-35], KAP of OPh about influenza vaccine have been scarcely investigated [32, 36, 37]. Moreover, as determinants of VE are vaccine-, VPD- and context-specific [28, 29], available evidence from general studies about vaccine acceptance in HCWs and more specifically in OPh are of limited generalizability [36, 37].
The aim of this study, therefore, to assess KAP of OPh about SIV and vaccination policies, including both general and specific recommendations for HCWs, and how attitudes and knowledge relate to these recommendations. Eventually, we attempted to identify areas that may be targeted for improvement through specific informative and educative campaigns dedicated to OPh.
Materials and methods
Study design
A cross-sectional questionnaire-based study was performed in the second half of 2015, involving OPh operating in the Autonomous Province (AP) of Trento (North- Eastern Italy). Participants were inquired about their KAP towards vaccinations, and more specifically on the SIV. Sampling was performed through convenience, as the initial population included all OPh participating to a seminar on occupational health that took place in the AP of Trento in October 2015 and assisting at least one healthcare provider in the AP of Trento (n = 105, 43.9% of 239 OPh usually operating in the AP of Trento). All participants giving their preventive agreement in the following weeks received a telephonic interview assessing knowledge and attitudes towards SI and SIV in HCWs.
Questionnaire
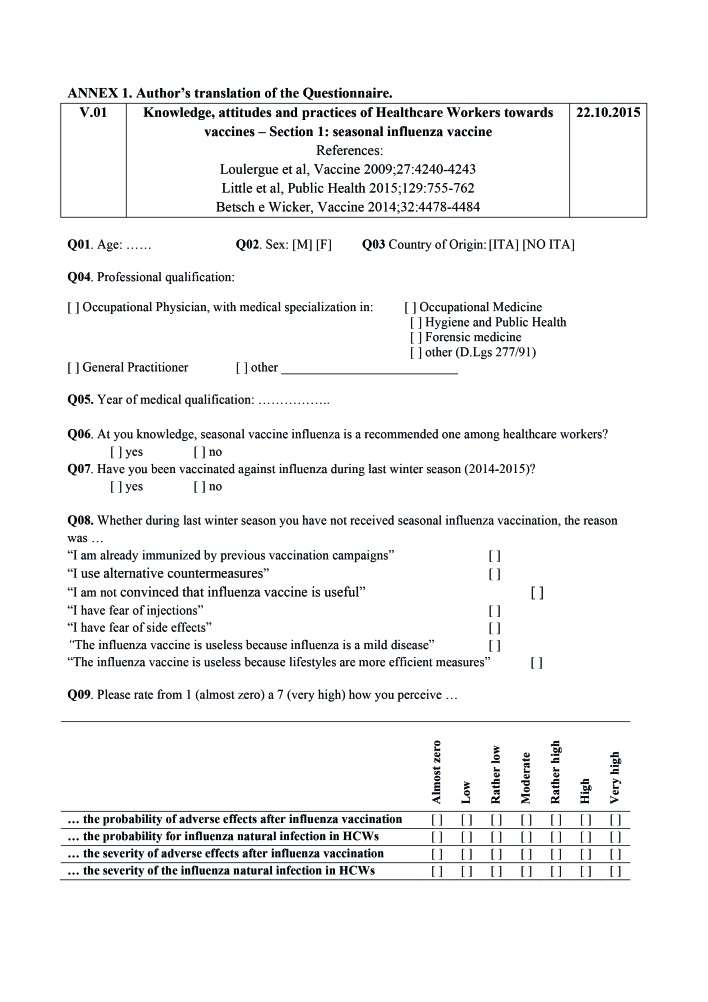
Two specifically formed researchers compiled a structured questionnaire through a telephonic interview. The questionnaire was formulated in Italian (an English translation is presented as the Annex 1), and its test-retest reliability was preventively assessed through a survey on 10 health professionals completing the questionnaire at two different points in time. All questions were self-reported, and not externally validated.
The final questionnaire comprised general demographic information (i.e. age, sex, country of origin) and the following areas of inquiry:
Demographic data. Included: age, sex, country of origin (i.e. Italian born-people vs. foreign-born people), and medical specialization (i.e. in Italy, qualification as OPh is primarily obtained through specialization in occupational medicine, but also specialists in Hygiene and Public Health and in Legal/Forensic Medicine are legally authorized to work as OPh, as well as all physicians who were working as OPh before 1991) [38, 39].
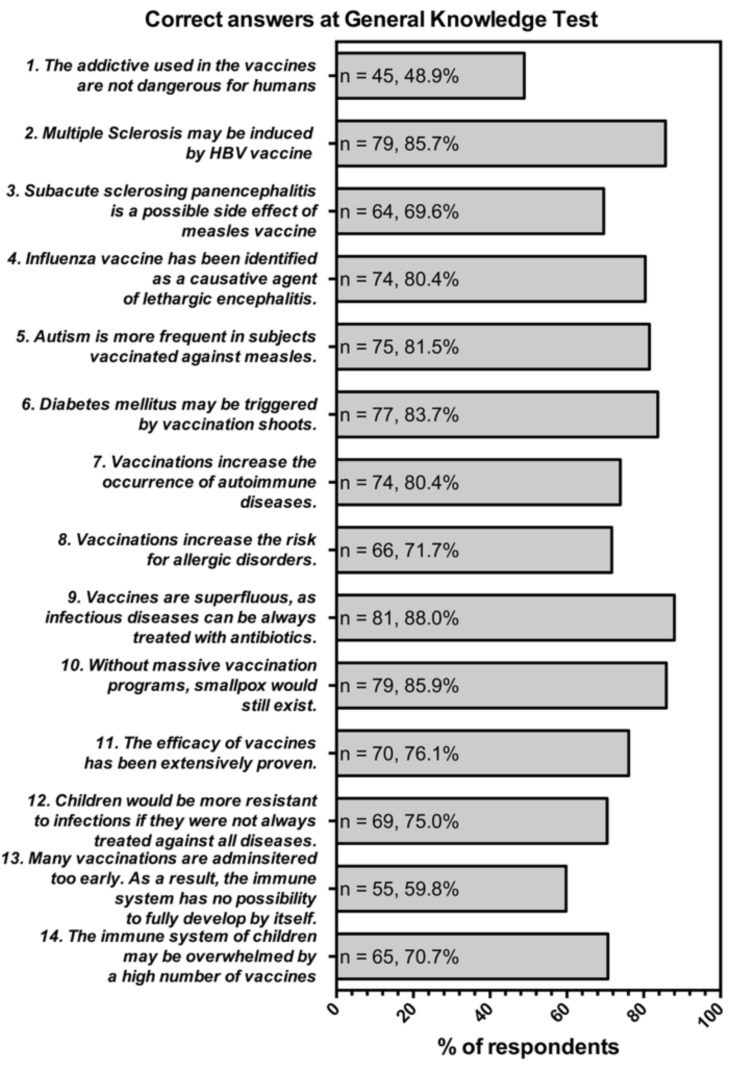
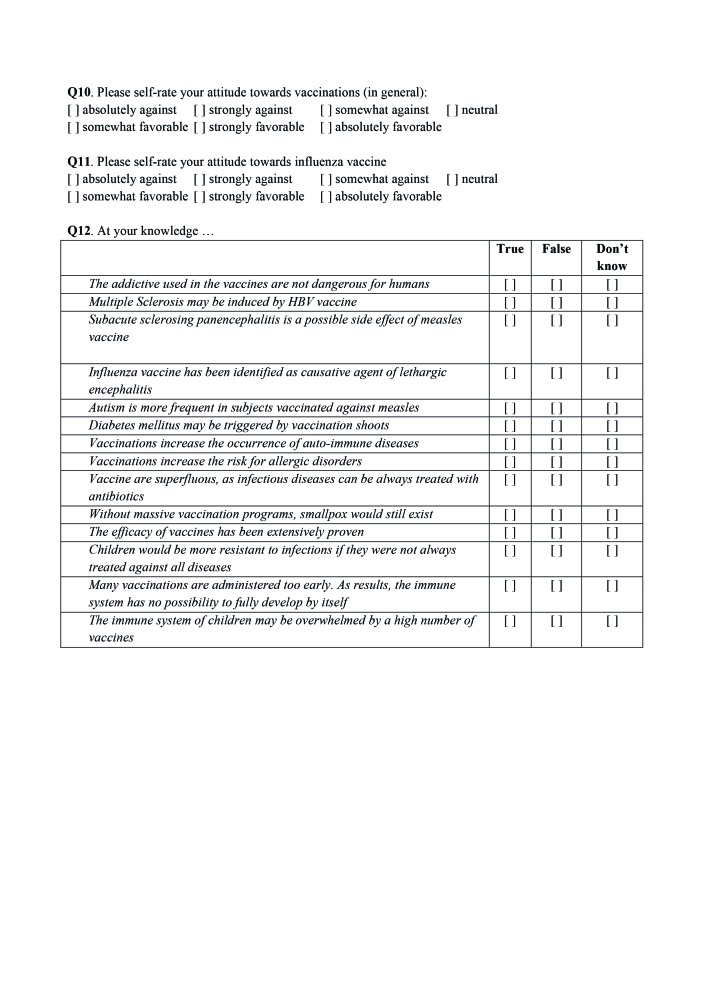
General knowledge. The questionnaire included a general knowledge test originally developed by Zingg and Siegrist [40], and containing a set of true-false statements such as "vaccinations increase the occurrence of allergies" (false) that cover some typical misconceptions on vaccination. General knowledge test was able to successfully predict risk perceptions and vaccination intentions in previous studies [32, 40]. A total of 14 statements (Fig. 1) were eventually presented, including the 9 original items from Zingg's questionnaire and 5 further items about vaccine misconceptions designed to better fit Italian settings (e.g. causative association between HBV vaccine and multiple sclerosis, influenza and lethargic encephalitis etc.). A General Knowledge Score (GKS) was then calculated as the sum of correctly and incorrectly marked recommendations: when the occupational physicians correctly answered, +1 was added to a sum score, whereas a wrong indication or a missing/"don't know" answer added -1 to the sum score.
-
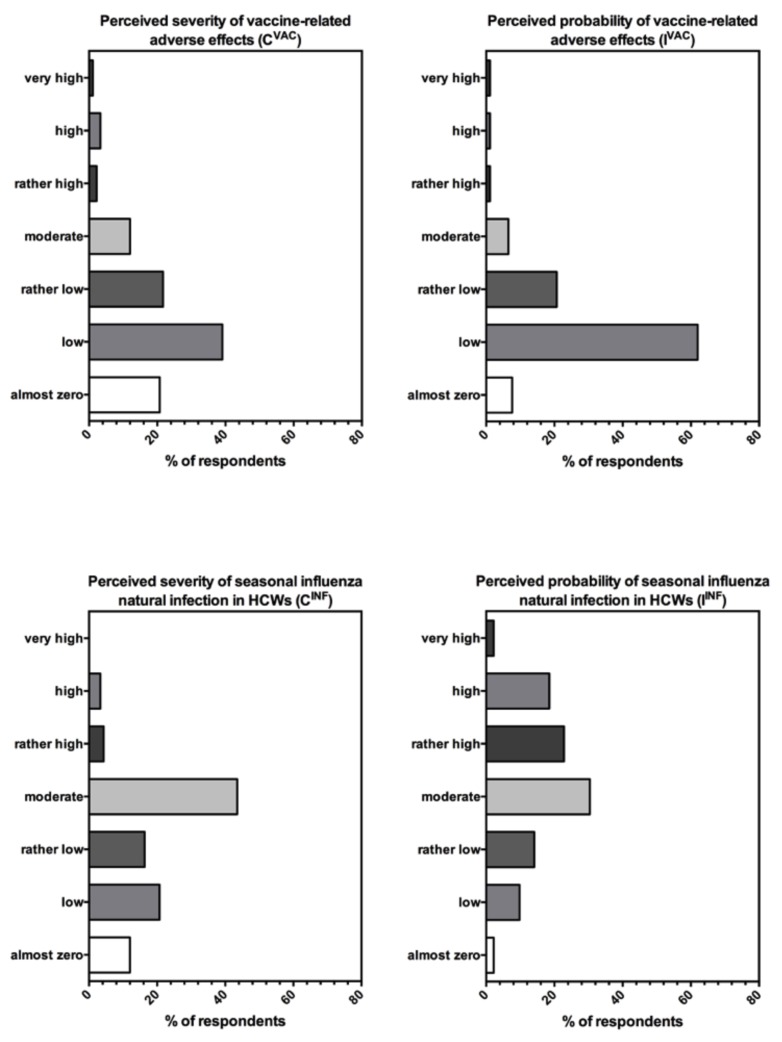
Risk perception. Perceived risk has been defined as a function of the perceived probability of an event and its expected consequences, and therefore assessed as the mathematical product of subjective probability and disease severity [32, 41]. We inquired the risk perception of OPh about influenza by asking the OPh about: the probability that HCWs get influenza infection, the frequency of vaccine-related adverse effects, and whether they perceived the severity of the natural infections and vaccine-related adverse effects. In order to summarize the results, we used a fully labeled 7-point scale (i.e. 1, "almost zero"; 2, "low"; 3, "rather low"; 4, "moderate"; 5, "rather high"; 6, "high"; 7, "very high"). A Risk Perception Score (RPS) was eventually calculated as cumulative score through the formula:
where: IINF = perceived probability of infection in HCWs, CINF = perceived severity of natural infection in HCW, IVAC =perceived probability of vaccine-related adverse, effects CVAC = perceived severity of vaccine-related adverse effects
Attitudes and Practices. Initially, participants rated their general attitudes towards vaccinations, and the answer was a 7-point Likert scale (i.e. 1, "absolutely against vaccinations"; 2, "strongly against vaccinations"; 3, "somewhat against vaccinations"; 4, "neutral"; 5, "somewhat in favor of vaccinations"; 6, "strongly in favor of vaccinations"; 7, "absolutely in favor of vaccinations"). The OPh were then asked to rate their attitudes towards influenza vaccine through a similar fully labeled 7-point Likert scale. A cumulative score (i.e. "propensity score") was calculated, both in general (GPS) and for influenza vaccine (IV-PS).
Fig. 1.
General knowledge test. The original knowledge test [19, 23] was modified including 5 additional items (n. 2 to 6); as disorders cited in items n. 2-6 were previously presented in the original items 2-3, items 7-9 were subsequently modified.
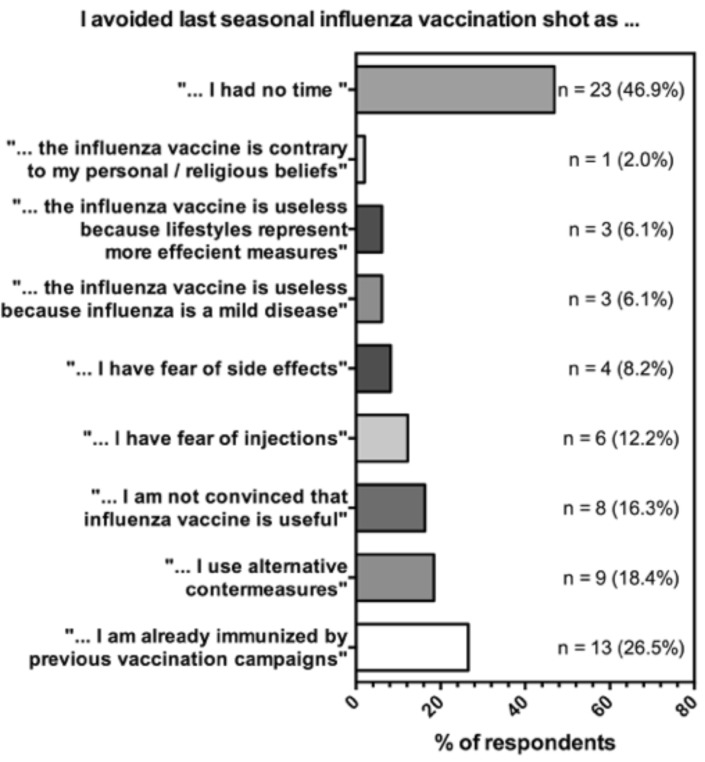
Eventually, participants were asked whether they had received SIV during 2014-2015 winter season. Subjects self-assessed as "not vaccinated" fulfilled a subsequent set of items exploring the reasons for not having been previously vaccinated. In particular, participants were asked whether: (1) they had organization problems (i.e. "not enough time"); (2) they felts themselves as already immunized by previous vaccination campaigns; (3) would prefer recur to alternative countermeasures; (4) are not convinced that IV is useful; (5) have fear of injections or (6) of side effects; (7) they understand vaccination as a mild disease, making therefore useless the vaccine and eventually (8) whether IV is contrary to their personal / religious beliefs.
Ethical considerations
Before they give their consent, participants were informed that all information would be gathered anonymous and handled confidentially. Participation was voluntary, and the questionnaire was collected only in subjects who expressed consent for study participation. As individual participants cannot be identified based on the presented material, this study caused no plausible harm or stigma to participating individuals.
As the study design assured an adequate protection of study participants, and neither include clinical data about patients nor configure itself as a clinical trial, a preliminary evaluation by the Ethical Committee of the Provincial Agency for Health Services (in Italian: Azienda Provinciale per i Servizi Sanitari, APSS) was statutorily not required.
Data analysis
Two independent researchers, one of whom read the responses from each questionnaire while the other researcher reviewed the entered data, ensured the accuracy of data entry. The primary investigator examined unclear responses to determine the correct answer. We calculated the described indices for general knowledge (GKS), risk perception (RPS) and vaccine propensity (G-PS and IV-PS).
Continuous variables (i.e. age, GKS, RPS, G-PS, IVPS) were expressed as mean ± standard deviation. Categorical variables were reported as percent values. Univariate confrontation between continuous variables was performed through Student's t test for unpaired data, whereas proportions were evaluated through Chisquared test (with continuity correction). Association of dichotomous variables was assessed in univariate analysis through calculation of respective Odds Ratios (OR) with their respective 95% Confidence Intervals (95% CI). Relations between the continuous variables were explored through the calculation of the Pearson productmoment correlation coefficient (i.e. Pearson's r). A logistic regression analysis (SPSS 23) was performed in order assessed the relative influence of personal attitudes and general knowledge on personal propensity to vaccinate. The analyses were controlled for age, sex, qualification. Odds Ratios similarly adjusted for age, sex, country of origin, and qualification (adjOR) were calculated through a binary logistic regression analysis for factors that in univariate analysis were associated with dichotomized propensity ("somehow favorable"/"somehow against" influenza vaccination) and previous SIV at p < 0.150. Significance level was 5%.
Results
Demographic data. Overall, 95/105 participants (90.5%) gave their consent to the inquiry and 92/105 compiled the questionnaire regarding IV/SIV (87.6%, i.e. the 38.5% of all OPh operating in the AP of Trento): as shown in Table I, 39 (42.4%) were males, and 53 (57.6%) females, with a mean age of 47.3 ± 10.4 years (50.4 ± 9.3 in males vs. 49.4 ± 8.1 in females, p = 0.582), and 55.4% of the participants (51/92) were > 50 year-old. Among the sampled subjects, 50 (54.3%) were specialists in Occupational Medicine, whereas 42 (45.7%) were qualified as specialist in Hygiene and Public Health.
General knowledge. Overall, 89/92 of the sampled OPh (96.7%) correctly recalled SIV as recommended by PNPV 2012-2014 in HCWs. Focusing on general knowledge test (Fig. 1), despite a potential range of -14 to +14, the actual mean score was 5.9 ± 4.5, and no one among sampled subject reached the maximum score of 14 (actual range: -9 to +11). With the exception of the claims about the safety of vaccine additives, as 47/92 (51.1%) failed to identify them as not dangerous, the majority of participants correctly identified the presented statements. In particular, most of participants were aware that infectious diseases cannot be always treated with antibiotics (88.0%, 81/92), and that without massive vaccination programs, infectious diseases such smallpox would still exist (85.9% of correct answers, 79/92). However, 23.9% of the sample (22/92) questioned the efficiency of vaccines, and 40.2% (37/92) exhibited the misconception that too many vaccinations are administered too early, whereas 29.3% (27/92) claimed that the immune system may be overwhelmed by a high number of vaccines. Eventually, around a fourth of sample erroneously stated that children would be more resistant to infections if they were not always treated against all diseases (23/92, 25.0%), and that vaccines may be causatively related with allergic disorders (28.3%, 26/92) and autoimmune diseases (26.1%, 24/92). More specifically, vaccines were associated with disorders of the immune systems such as diabetes mellitus (15/92, 16.3%) and multiple sclerosis (13/92, 14.1%), but also with neurological diseases such as subacute sclerosing panencephalitis (28/92, 30.4%), lethargic encephalitis (18/92, 19.6%), and even autism (17/92, 18.5%).
Assessment of the risk perception. Despite a potential range -49 to +51, RPS was estimated in 7.5 ± 8.6 (actual range -26 to +27). As shown in Figure 2, not only the majority of participants perceived the potential severity (CINF) of influenza natural infection as "almost zero" to "rather low" (59.8%, 55/92; mean score 3.2 ± 1.3), but also no one among the sample identified influenza as a VPD with a potentially "very high" severity, whereas 26.1% of participants similarly defined potential probability of influenza natural infection in HCWs (IINF) as "almost zero" to "rather low", with a further 30.4% acknowledging a "moderate" probability of natural infection (mean score 4.3 ± 1.4). Regarding the adverse effects, around 90.2% of participants referred to perceive their probability (IVAC) as "almost zero" to "rather low" (mean score 2.4 ± 0.9), and similarly 81.5% of the participants defined their potential severity as mild (i.e. "almost zero" to "rather low"; CVAC, mean score 2.5 ± 1.3).
-
Attitudes and Practices. Mean G-PS was 5.8 ± 1.1, with an actual range of 3 to 7. More specifically, 88/92 (95.6%) identified themselves as somehow favorable to vaccinations. Focusing on IV-PS, a mean score of 3.1 ± 1.8 was identified (actual range: 1 to 7), as 63/92 (68.5%) were somehow favorable to influenza vaccine.
Overall, 46.7% of the participants (43/92) referred to have been vaccinated against seasonal influenza in the previous year, and 49 subjects fulfilled the questionnaire's section exploring the reasons for refusing SIV (Fig. 3). The most frequently referred reason was the lack of time (23/49, 46.9%), followed by the belief to be "already immune because of previous vaccinations" (13/49, 26.5%), whereas 9/49 (18.4%) reported the preferential use of "alternative countermeasures", and 8/49 (16.3%) were "not convinced that influenza vaccine is useful", and 4/49 (8.2%) referred "fear of side effects".
-
Univariate analysis. In univariate analysis, although a greater share of participants younger than 50 years exhibited a somehow favorable attitude towards influenza vaccine (78.0% vs. 60.8% in subjects older than 50 years, p = 0.122; OR 2.294 95% CI 0.906-5.808), no significant association was found between demographic factors (i.e. gender, age group and country of origin), and vaccination status on the one hand and personal attitude towards seasonal influenza vaccine (Table II). However, focusing on the referred medical specialization, participants having a qualification in Occupational Medicine were associated with a significantly greater share of positive attitude towards seasonal influenza vaccine (90.0% vs. 42.9%, p < 0.001; OR 12.000 95% CI 3.964-36.331). Eventually, subjects referring a positive vaccination status more frequently exhibited an attitude somehow against influenza vaccination than participants exhibiting a negative vaccination status (82.9% vs. 56.9%, respectively; p = 0.012, OR 3.816 OR 1.422-10.239).
As shown in Table III, subjects correctly identifying as "true" the statement that "the efficacy of vaccines has been extensively proven" were significantly associated with the recalling of a positive seasonal influenza vaccine status (OR 3.600, 95% CI 1.169-10.83) and a positive attitude towards influenza vaccine (OR 3.741, 95% CI 1.374-10.19).
A positive attitude towards SIV was also significantly associated with the denying of misconceptions as the association between vaccines and autism (p < 0.001; OR 8.188 95%CI 2.528-26.52), the greater resistance to infections of children achieving a "natural" immunity (p = 0.007; OR 4.306; 95% CI 1.590-11.663), and the increased occurrence of auto-immune diseases after receiving vaccinations (p = 0.044; OR 3.000 95% CI 1.137-7.918).
On the contrary, as shown in Table IV, previous vaccination against SI and a favorable attitude towards SIV were not associated with a significantly higher share of the factors included in the assessment of risk perception. As shown in Table V, both GKS and RPS were significantly higher in subjects younger than 50 y.o. (7.1 ± 3.1 vs. 4.9 ± 4.1, p = 0.009; and 9.6 ± 7.7 vs. 5.9 ± 8.9, p = 0.033, respectively), in foreign-born participants than in Italian-born ones (8.7 ± 2.7 vs. 5.7 ± 4.3, p = 0.013; and 11.7 ± 10.4 vs. 7.2 ± 8.4, p = 0.023, respectively), and eventually in participants referring a specialization in Occupational Medicine than in participants specialists in Hygiene and Public Health (7.0 ± 3.0 vs. 4.6 ± 5.1, p = 0.008; and 9.6 ± 7.4 vs. 5.1 ± 9.3, p = 0.011, respectively). No significant differences were identified in GPS throughout assessed demographic factors (all comparison p > 0.05), whereas focusing on IV-PS, subjects younger than 50 y.o. had a significantly higher score than older participants (4.1 ± 1.0 vs. 3.5 ± 1.4, p = 0.020).
Bivariate Pearson's correlations among GKS, RPS, GPS and IV-PS are shown in Table VI. More specifically, GKS was positively correlated with RPS (r =0.317, p = 0.002) and propensity scores, (r = 0.315, p = 0.022 and r = 0.492, p < 0.001 for G-PS and IV-PS, respectively). Focusing on the two propensity scores, GPS and IV-PS were positively correlated (r = 0.451, p < 0.001). Whereas IV-PS was in turn correlated with RPS (r = 0.280, p = 0.007), G-PS was not (r = 0.203, p = 0.053).
-
Multivariate analysis. Binary logistic regression confirmed that subjects somehow favorable to influenza vaccination more frequently had a positive SIV status (adjOR 5.806 95% CI 1.242-27.15), and correctly identified as misconceptions the association between vaccines and autism (adjOR 25.05 95% CI 2.538-247.3), and that children would be more resistant to infections if they were not always vaccinated against all diseases (adjOR 15.77 95% CI 2.364-105.2). Similarly, participants acknowledging that the efficacy of vaccines has been extensively proven had significant positive association with positive immunization status towards seasonal influenza (adjOR 3.999 95% CI 1.245-12.84).
Linear regression model included IV-PS dependent variable, GKS, RPS and G-PS as independent variables, and age, sex, medical specialization and immunization status as covariates. Eventually, GKS (beta coefficient 0.213, p value = 0.043), RPS (beta coefficient 0.252, p value = 0.018) and G-PS (beta coefficient 0.384, p value = 0.002) were identified as significant predictors of IV-PS.
Tab. I.
Demographic characteristics and qualification of sampled OPh (n = 95).
| Characteristics | N (%) |
|---|---|
| Gender | |
| Males | 39 (42.4%) |
| Females | 53 (57.6%) |
| Age (years) | |
| ≤ 29 | 3 (3.3%) |
| 30 – 39 | 8 (8.7%) |
| 40 – 49 | 30 (32.6%) |
| 50 – 59 | 44 (47.8%) |
| ≥ 60 | 7 (7.6%) |
| Country of origin | |
| Italian-born people | 86 (93.5%) |
| Foreign-born people | 6 (6.5%) |
| Medical Specialization | |
| Occupational Medicine | 50 (54.3%) |
| Hygiene and Public Health | 42 (45.7%) |
| Legal / Forensic Medicine | - |
| Other | - |
Fig. 2.
Components of the Risk Perception Score in 92 Occupational Physicians participating to the survey (HCWs = health care workers).
Fig. 3.
Reasons advocated by subjects not vaccinated against seasonal influenza during winter season 2014-2015. Because more than a single choice was possible, sum of percentages is not equal to 100%.
Tab. II.
Univariate association of influenza vaccination practice and attitude regarding influenza vaccine, with recalled demographic factors in 92 OPh participating to the study (OR = Odds Ratio; 95% CI = 95% Confidence Interval).
| Previously vaccinated against seasonal influenza | Somewhat favorable to influenza vaccination | |||||
|---|---|---|---|---|---|---|
| N (%) | P value | OR (95% CI) | N (%) | P value | OR (95% CI) | |
| Gender | ||||||
| Males | 20 (51.3%) | 0.368 | 1.604 | 30 (76.9%) | 0.205 | 2.020 |
| Females | 21 (39.6%) | (0.696 – 3.697) | 33 (62.3%) | (0.798 – 5.116) | ||
| Age group | ||||||
| < 50 y.o. | 16 (39.0%) | 0.455 | 0.666 | 32 (78.0%) | 0.122 | 2.294 |
| ≥ 50 y.o. | 25 (49.0%) | (0.289 - 1.532) | 31 (60.8%) | (0.906 – 5.808) | ||
| Country of origin | ||||||
| Italian-born people | 39 (45.3%) | 0.883 | 1.660 | 58 (67.4%) | 0.722 | 0.414 |
| Foreign-born people | 2 (33.3%) | (0.288 – 9.547) | 5 (83.3%) | (0.046 – 3.716) | ||
| Specialization | ||||||
| Occupational Medicine | 25 (50.0%) | 0.350 | 1.625 | 45 (90.0%) | < 0.001 | 12.000 |
| Hygiene and Public Health | 16 (38.1%) | (0.706 – 3.741) | 18 (42.9%) | (3.964 – 36.33) | ||
| Vaccination status towards seasonal influenza | ||||||
| Previously vaccinated | - | - | - | 34 (82.9%) | 0.014 | 3.685 |
| Not vaccinated | - | - | - | 29 (56.9%) | (1.377 – 9.860) | |
Tab. III.
Univariate analysis of the association between the correct answer to the statements included in the general knowledge test, positive vaccination status and attitude towards seasonal influenza vaccine.
| Statement | Previously vaccinated against influenza vaccine (n = 41) | Somehow favorable attitude towards influenza vaccine (n = 63) | ||
|---|---|---|---|---|
| Unadjusted OR (95% CI) | P value | Unadjusted OR (95% CI) | P value | |
| 1. The addictive used in the vaccines are not dangerous for humans (TRUE) | 0.830 (0.364 – 1.892) | 0.816 | 1.038 (0.430 – 2.503) | 0.888 |
| 2. Multiple Sclerosis may be induced by HBV vaccine (FALSE) | 1.544 (0.475 – 5.014) | 0.671 | 0.960 (2.280 – 3.418) | 0.796 |
| 3. Subacute sclerosing panencephalitis is a possible side effect of measles vaccine (FALSE) | 0.905 (0.370 – 2.217) | 1.000 | 0.316 (0.514 – 3.372) | 0.742 |
| 4. Influenza vaccine has been identified as causative agent of lethargic encephalitis (FALSE) | 1.734 (0.614 – 4.896) | 0.434 | 2.700 (0.938 – 7.770) | 0.110 |
| 5. Autism is more frequent in subjects vaccinated against measles (FALSE) | 0.451 (0.145 – 1.408) | 0.262 | 8.188 (2.528 – 26.52) | < 0.001 |
| 6. Diabetes mellitus may be triggered by vaccinations shoot (FALSE) | 0.800 (0.259 – 2.467) | 0.916 | 2.188 (0.708 – 6.763) | 0.282 |
| 7. Vaccinations increase the occurrence of auto-immune diseases (FALSE) | 1.072 (0.421 – 2.730) | 1.000 | 3.000 (1.137 – 7.918) | 0.044 |
| 8. Vaccinations increase the risk for allergic disorders (FALSE) | 1.357 (0.546 – 3.374) | 0.671 | 2.471 (0.957 – 6.378) | 0.099 |
| 9. Vaccine are superfluous, as infectious diseases can be always treated with antibiotics (FALSE) | 0.424 (0.105 – 1.715) | 0.365 | 3.026 (0.840 – 10.90) | 0.160 |
| 10. Without massive vaccination programs, smallpox would still exist (TRUE) | 0.928 (0.286 – 3.012) | 1.000 | 1.856 (0.459 – 7.498) | 0.616 |
| 11. The efficacy of vaccines has been extensively proven (TRUE) | 3.600 (1.169 – 10.83) | 0.034 | 3.741 (1.374 – 10.19) | 0.016 |
| 12. Children would be more resistant to infections if they were not always treated against all diseases (FALSE) | 0.943 (0.364 – 2.441) | 1.000 | 4.306 (1.590 – 11.66) | 0.007 |
| 13. Many vaccinations are administered too early. As results, the immune system has no possibility to fully develop by itself (FALSE) | 0.914 (0.395 – 2.117) | 1.000 | 1.997 (0.817 – 4.882) | 0.194 |
| 14. The immune system of children may be overwhelmed by a high number of vaccines (FALSE) | 1.227 (0.499 – 3.020) | 0.830 | 1.125 (0.432 – 2.993) | 0.996 |
Tab. IV.
Univariate analysis of the association between participants' risk perception about influenza and influenza vaccine, positive vaccination status and attitude towards seasonal influenza vaccine.
| Variable | Previously vaccinated against influenza vaccine (n = 41) | Somehow favorable attitude towards influenza vaccine (n = 63) | ||
|---|---|---|---|---|
| Unadjusted OR (95% CI) | P value | Unadjusted OR (95% CI) | P value | |
| Perceived severity of vaccine related adverse effects (CVAC) as rather high to very high | 1.263 (0.241 – 6.616) | 1.000 | 0.205 (0.035 – 1.191) | 0.144 |
| Perceived probability of vaccine related adverse effects (IVAC) as rather high to very high | 0.613 (0.054 – 7.003) | 1.000 | 0.218 (0.019 – 2.505) | 0.484 |
| Perceived severity of seasonal influenza natural infection in HCWs (CINF) as rather high to very high | 1.730 (0.365 – 8.208) | 0.763 | 0.588 (0.123 – 2.814) | 0.804 |
| Perceived probability of seasonal influenza natural infection in HCWs (IINF) as rather high to very high | 2.123 (0.916 – 4.920) | 0.120 | 1.396 (0.568 – 3.429) | 0.616 |
Tab. V.
Univariate comparison of General Knowledge Score (GKS), Risk Perception Score (RPS), Propensity Score towards vaccines in general (G-PS) and influenza vaccination (IV-PS) by recalled demographic factors in 92 OPh participating to the study.
| GKS | RPS | G-PS | IV-PS | |||||
|---|---|---|---|---|---|---|---|---|
| Mean ± S.D. | P value | Mean ± S.D. | P value | Mean ± S.D. | P value | Mean ± S.D. | P value | |
| Gender | ||||||||
| Males | 6.3 ± 3.4 | 0.397 | 9.4 ± 8.3 | 0.079 | 5.8 ± 1.1 | 0.639 | 4.1 ± 1.1 | 0.055 |
| Females | 5.6 ± 4.9 | 6.2 ± 8.6 | 5.7 ± 1.1 | 3.6 ± 1.4 | ||||
| Age group | ||||||||
| < 50 y.o. | 7.1 ± 3.1 | 0.009 | 9.6 ± 7.7 | 0.033 | 5.9 ± 1.1 | 0.256 | 4.1 ± 1.0 | 0.020 |
| ≥ 50 y.o. | 4.9 ± 4.8 | 5.9 ± 8.9 | 5.7 ± 1.1 | 3.5 ± 1.4 | ||||
| Country of origin | ||||||||
| Italian-born people | 5.7 ± 4.3 | 0.013 | 7.2 ± 8.4 | 0.023 | 5.8 ± 1.1 | 0.365 | 3.8 ± 1.3 | 0.672 |
| Foreign-born people | 8.7 ± 2.7 | 11.7 ± 10.4 | 6.2 ± 1.0 | 4.0 ± 1.1 | ||||
| Specialization | ||||||||
| Occupational medicine | 7.0 ± 3.0 | 0.008 | 9.6 ± 7.4 | 0.011 | 5.9 ± 0.9 | 0.377 | 4.4 ± 0.8 | < 0.001 |
| Hygiene and Public Health | 4.6 ± 5.1 | 5.1 ± 9.3 | 5.7 ± 1.3 | 3.1 ± 1.4 | ||||
Tab. VI.
Bivariate Pearson's correlation among General Knowledge Score (GKS), Risk Perception Score (RPS), Propensity Score towards vaccines in general (G-PS) and influenza vaccination (IV-PS).
| GKS | RPS | G-PS | IV-PS | |
|---|---|---|---|---|
| GKS | - | r = 0.317
p = 0.002 |
r = 0.315
p = 0.022 |
r = 0.492
p < 0.001 |
| RPS | r = 0.317
p = 0.002 |
- | r = 0.203
p = 0.053 |
r = 0.280
p = 0.007 |
| G-PS | r = 0.315
p = 0.022 |
r = 0.203
p = 0.053 |
- | r = 0.451
p < 0.001 |
| IV-PS | r = 0.492
p < 0.001 |
r = 0.280
p = 0.007 |
r = 0.451
p < 0.001 |
- |
Tab. VII.
Multivariate analysis. The binary logistic regression analysis model evaluated variables that in univariate analysis were associated with vaccination status and favorable attitude towards influenza vaccine having a p value < 0.150, and included age, sex, medical specialization as covariates. Moreover, positive vaccination status was included as a covariate in the multivariate analysis about attitude towards influenza vaccine.
| Statement | Previously vaccinated against influenza vaccine (n = 41) | Somehow favorable attitude towards influenza vaccine (n = 63) | ||
|---|---|---|---|---|
| Adjusted OR (95% CI) | P value | adjusted OR (95% CI) | P value | |
| Previous vaccination against seasonal influenza vaccine | - | - | 5.806 (1.242 – 27.15) | 0.025 |
| 4. Influenza vaccine has been identified as causative agent of lethargic encephalitis (FALSE) | - | - | 3.578 (0.760 – 16.86) | 0.107 |
| 5. Autism is more frequent in subjects vaccinated against measles (FALSE) | - | - | 25.05 (2.538 –247.3) | 0.006 |
| 7. Vaccinations increase the occurrence of auto-immune diseases (FALSE) | - | - | 3.810 (0.641 – 22.64) | 0.141 |
| 8. Vaccinations increase the risk for allergic disorders (FALSE) | - | - | 1.363 (0.370 – 6.378) | 0.222 |
| 11. The efficacy of vaccines has been extensively proven (TRUE) | 3.999 (1.245 – 12.84) | 0.034 | 0.433 (0.078 – 2.412) | 0.339 |
| 12. Children would be more resistant to infections if they were not always treated against all diseases (FALSE) | - | - | 15.77 (2.364 – 105.2) | 0.004 |
| Perceived severity of vaccine related adverse effects (CVAC) as rather high to very high | - | - | 0.117 (0.008 – 1.681) | 0.115 |
| Perceived probability of seasonal influenza natural infection in HCWs (IINF) as rather high to very high | 2.380 (0.439 – 12.91) | 0.120 | - | - |
Discussion
While in European Countries vaccination rates of HCWs against SI remain far below the target objective of 75%, still ranging between unsatisfactory rates of 14% and 50% [1, 42, 43], a growing number of authorities have developed initiatives aimed to increase SIV uptake among HCWs [2]. Addressing the factors that explain insufficient adherence of HCWs to official recommendation about SIV has consequently become a growing focus of attention [15, 18, 25, 44-46]. Sound evidences do suggest that HCWs may share with the general population significant fears of side effects, misconceptions about vaccine safety, and even poor knowledge of vaccine's benefits, ultimately leading them to lower vaccination rates [16, 18, 47]. Moreover, a significant share of HCWs would underestimate not only the actual severity of seasonal influenza natural infection, but also their potential role in transmitting VPDs to the patients [3, 4, 10, 18, 23, 26, 48-51].
Despite the growing number of studies performed in recent years, at our knowledge few researches specifically evaluated KAP of OPh: overall, their knowledge of vaccines and vaccine recommendations were not consistently satisfactory [32,36, 37]. Also in our study, OPh were affected by a relatively high prevalence of misconceptions about vaccines [9]: interestingly enough, participants OPh shared false beliefs and misunderstandings about presumptive association between vaccines and autoimmune diseases (i.e. multiple sclerosis, diabetes), and also between certain immunizations and disorders such as autism, subacute sclerosing panencephalitis, and lethargic encephalitis. Worries about such associations were actually raised in the previous decades being then criticized or even largely disproved in the following years [52-54]. Although a significant base of evidence ultimately denies a causality between vaccinations, autoimmune and neuropsychiatric disorders, aforementioned warnings still receive diffuse emphasis on conventional media, remaining very influential on the "new media" (i.e. social media, personal blogs, etc.) [14, 15, 30, 31, 55, 56]. Interestingly enough, a greater share of false beliefs and misconceptions was identified in older subjects: we could tantalizingly suppose that such information gaps may be understood as a consequence of an insufficient continuous medical education and, as risk perception follows the acquisition of the knowledge [32, 60-62]. Such information gaps may in turn explain why the majority of sampled OPh identified influenza as a substantially indolent disease, and similarly around a quarter of the sample underestimated the probability for HCWs to develop seasonal influenza natural infection (26.1%). Actually, some international reports suggest that HCWs may avoid SIV as they understood its potential adverse effects as more severe and frequent than the avoided consequences of the natural infection [3, 18,20, 43].
Although in our sample doubts inherent vaccine safety were somehow reduced, as 90.2% of participants perceived probability of adverse effects as "almost zero" to "rather low", and the main reason referred by the participants to have not been vaccinated against SI was the lack of time, OPh with a better trust on the proven efficacy of vaccines, as defined by general knowledge test, more frequently reported vaccination against seasonal influenza (adjOR 3.999 95% CI 1.245-12.84), whereas no significant effect was found on individual vaccine propensity. Regarding the organization issues referred by participants, it should be recalled that Italian OPh are HCWs that usually work as private practitioner: in other words, their adherence to official recommendation towards SIV could have been significantly impaired by factors other than personal beliefs and misconceptions, as the limited availability of vaccination services [4, 11, 14-19].
Similarly, we found a significant correlation between GKS and RPS (r = 0.317, p = 0.002), and such correlation was not unexpected [32, 36], as well as that of both cumulative score with propensity towards SIV (r = 0.492, p < 0.001 and r = 0.280, p = 0.007, respectively). Consistently with previous researches in KAP in HCWs towards vaccinations [4, 11, 14-18, 32, 36], all factors presumptively involved in the building up of personal attitudes (i.e. GKS, G-PS, RPS) were then identified as significant predictors of the propensity towards SIV. In other words, a greater knowledge (i.e. less misconceptions and/or less personal attitudes guiding the vaccine decisions) of vaccine and vaccine-related disorders on the one hand, and a more accurate risk perception of SI on the other hand were associated with a better attitude towards SIV. In effect, there is a considerable evidence that a better awareness and a greater trust in vaccines increase the individuals' propensity to be vaccinated, and in OPh the latter would be in turn associated with a greater propensity to perform and promote vaccinations on the workplaces [14-16, 32, 67, 68]: in other words, any information gap in OPh would ultimately lead to diffusely hold and diffuse doubts or false beliefs about vaccines rejection of some vaccines [26, 56-59], being significant drivers of a more extended VE in HCWs and in turn in the general population with devastating consequences [32, 36].
However, it should be stressed that several factors not necessarily included in the knowledge and risk perception assessment contribute to building up vaccine confidence (and conversely VE) [63]: although adhesion to the official recommendations is usually characterized as weak driving factors [18, 25, 28, 29], attitudes of OPh may be significantly influenced by concerns about potential legal consequences of their actual implementation. In other words, participants may have reported behaviors unrelated with actual knowledge and risk perception, exhibiting a sort of "social desirability bias", i.e. the tendency of research subjects to give socially desirable responses instead of choosing responses that are reflective of their true feelings [64, 65]. Also the higher propensity towards SIV in specialists in Occupational Medicine than in specialists in Hygiene and Public Health, the latter assed as a dichotomous attitude (OR 12.000 95% CI, 3.964-36.33) and as a cumulative score as well (IV-PS, 4.4 ± 0.8 vs. 3.1 ± 1.4, p < 0.001), and better performances in both the general knowledge tests (7.0 ± 3.0 vs. 4.6 ± 5.1, p = 0.008) and in the assessment of the risk perception (9.6 ± 7.4 vs. 5.1 ± 9.3, p = 0.011) may be similarly explained. These results were otherwise unexpected, as vaccinology represents a cornerstone of the core curriculum of specialization courses in Hygiene and Public Health, and a significantly higher share of positive attitudes and appropriate knowledge was previously reported in residents in Hygiene and Public Health [66].
As risk perception may be understood as an intermediate step between knowledge and the developing of an attitude [32, 60-62], a self-reported positive vaccination status was unsurprisingly associated with a positive attitude towards vaccination (adjOR 5.806 95% CI 1.242-27.15). In this regard, although vaccination rate was well below 50% (43/92, 46.7%), our survey is consistent with previous studies on HCWs: despite data on European HCWs clearly show a very low compliance towards SIV, physicians have been usually described as more receptive to influenza vaccination than other HCWs, ultimately exhibiting similar vaccination rates [9, 18].
Limits of the study
Several major limitations of the study have to be addressed. For instance, we assessed a sample of relatively small size, gathered through convenience sampling and a regional basis. As Italy is highly heterogeneous in term of vaccination rates and vaccine acceptance, our sample may therefore not represent the whole Italian OPh populations [12]. Second, our sample was drawn from a very selected population that presumptively included OPh more sensitive to medical education themes (i.e. subjects participating to a Continuous Medical Education course): a significant selection bias cannot therefore be ruled out, ultimately suggesting that our sample overestimated actual vaccine acceptance of the parent occupational group. Moreover, as our questionnaire did not investigated the information sources from which assessed knowledge and elements of risk perceptions were drawn, we are unable to evaluate whether these results are a serendipitous association in the context of a small sample, or rather the actual consequence of a different post-graduate formation, and this may be acknowledged as another weakness of this study. Generalization of our results may be furtherly compromised by the very same design of the survey. In other words, not only participants may have overrated their actual vaccine propensity and similarly assessed the items of the general knowledge test in terms of "social desirability", but we cannot rule out a substantial lack of specificity in the recalling of vaccination status [9].
Conclusions
In conclusion, our results are consistent with previous reports on HCWs and with the limited available evidence on OPh. More specifically, the majority of OPh were somehow favorable to SIV, but a significant share of misbeliefs and false knowledge were also identified. As knowledge and risk perception were identified as significant predictors of vaccine propensity, our results suggest that that filling information gaps may significantly improve vaccine propensity of OPh, and possibly increase the vaccination rates in HCWs and, in turn, in the general population. Moreover, our results suggest that a significant share of HCWs may benefit from more flexibility, in term of time and accessibility, by healthcare providers performing SIV, and in particular with vaccination services. Their better interaction with OPh would be also useful in order to address personal misconceptions and target false beliefs, ultimately increasing the awareness of the potential of SIV, in the HCWs and, subsequently, in the general population.
ACKNOWLEDGMENTS
The authors thank the subjects whose participation made this study possible.
All person who meet authorship criteria are listed as authors, and all authors certify that they have no affiliation with or involvement in any organization or entity with any financial interest, or non-financial interest (such as personal or professional relationship, affiliation, knowledge of beliefs) in the subject matter or material discussed in the manuscript.
Appendix
References
- 1.Giannattasio A, Mariano M, Romano R, Chiatto F, Liguoro I, Borgia G, Guarino A, Vecchio A. Sustained low influenza vaccination in health care workers after H1N1 pandemic: a cross sectional study in an Italian health care setting for at-risk patients. BMC Infect Dis. 2015;15:329–329. doi: 10.1186/s12879-015-1090-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Music T. Protecting patients, protecting healthcare workers: a review of the role of influenza vaccination. Int Nurs Rev. 2012;59:161–167. doi: 10.1111/j.1466-7657.2011.00961.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonaccorsi G, Santomauro F, Porchia B, Niccolai G, Pellegrino E, Bonanni P, Lorini C. Beliefs and Opinions of Health Care Workers and Students Regarding Influenza and Influenza Vaccination in Tuscany, Central Italy. Vaccines (Basel) 2015;3:137–147. doi: 10.3390/vaccines3010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albano L, Matuozzo A, Marinelli P, Giuseppe G. Knowledge, attitudes and behaviour of hospital health-care workers regarding influenza A/H1N1: a cross sectional survey. BMC Infectious Diseases. 2014;14:208–208. doi: 10.1186/1471-2334-14-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gasparini R, Amicizia D, Lai PL, Bragazzi NL, Panatto D. Compounds with anti-influenza activity: present and future of strategies for the optimal treatment and management of influenza. Part I: influenza life-cycle and currently available drugs. J Prev Med Hyg. 2014;55:69–85. [PMC free article] [PubMed] [Google Scholar]
- 6.Gasparini R, Amicizia D, Lai PL, Bragazzi NL, Panatto D. Compounds with anti-influenza activity: present and future of strategies for the optimal treatment and management of influenza Part II: Future compounds against influenza virus. J Prev Med Hyg. 2014;55:109–129. [PMC free article] [PubMed] [Google Scholar]
- 7.Gasparini R, Amicizia D, Lai PL, Panatto D. Influenza vaccination: from epidemiological aspects and advances in research to dissent and vaccination policies. J Prev Med Hyg. 2016;57:E1–E4. [PMC free article] [PubMed] [Google Scholar]
- 8.Barberis I, Myles P, Ault SK, Bragazzi NL, Martini M. History and evolution of influenza control through vaccination: from the first monovalent vaccine to universal vaccines. J Prev Med Hyg. 2016;57:E115–E120. [PMC free article] [PubMed] [Google Scholar]
- 9.Gazmararian JA, Coleman M, Prill M, Hinman AR, Ribner BS, Washington ML, et al. Influenza vaccination of health care workers: Policies and practices of hospitals in a community setting. Am J Infect Control. 2007;35:441–447. doi: 10.1016/j.ajic.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Bonfiglioli R, Vignoli M, Guglielmi D, Depolo M, Violante FS. Getting vaccinated or not getting vaccinated? Different reasons for getting vaccinated against seasonal or pandemic influenza. BMC Public Health. 2013;13:1221–1221. doi: 10.1186/1471-2458-13-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Centers for Disease Control and Prevention , author. General Recommendations on Immunization --- recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR Recomm Rep. 2011;60:1–64. [PubMed] [Google Scholar]
- 12.Bonanni P, Ferro A, Guerra R, Iannazzo S, Odone A, Pompa MG, Rizzuto E, Signorelli C. Vaccine coverage in Italy and assessment of the 2012- 2014 National Immunization Prevention Plan. Epidemiol Prev. 2015;39:146–158. [PubMed] [Google Scholar]
- 13.Barbadoro P, Marigliano A, Tondo E, Paolis M, Martini E, Prospero E, D'Errico MM. Measles among Healthcare Workers in a Teaching Hospital in Central Italy. J Occup Health. 2012;54:336–339. doi: 10.1539/joh.12-0016-br. [DOI] [PubMed] [Google Scholar]
- 14.Maltezou HC, Gargalianos P, Nikolaidis P, Katerelos P, Tedoma N, Maltezos E, Lazanas M. Attitudes towards mandatory vaccination and vaccination coverage against vaccine-preventable diseases among health-care workers in tertiary-care hospitals. J Infect. 2012;64:319–324. doi: 10.1016/j.jinf.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Tafuri S, Gallone MS, Cappelli MG, Martinelli D, Prato R, Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine. 2014;32:4860–4865. doi: 10.1016/j.vaccine.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 16.Barrière J, Vanjak D, Kriegel I, Otto J, Peyrade F, Estève M, Chamorey E. Acceptance of the 2009 A(H1N1) influenza vaccine among hospital workers in two French cancer centers. Vaccine. 2010;28:7030–7034. doi: 10.1016/j.vaccine.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 17.To K-W, Lee S, Chan T-O, Lee S-S. Exploring determinants of acceptance of the pandemic influenza A (H1N1) 2009 vaccination in nurses. Am J Infect Control. 2010;38:623–630. doi: 10.1016/j.ajic.2010.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Durando P, Alicino C, Dini G, Barberis I, Bagnasco AM, Iudici R, Zanini M, Martini M, Toletone A, Paganino C, et al. Determinants of adherence to seasonal influenza vaccination among healthcare workers from an Italian region: results from a cross-sectional study. BMJ Open. 2016;6:e010779–e010779. doi: 10.1136/bmjopen-2015-010779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leone Roberti Maggiore U, Scala C, Toletone A, Debarbieri N, Perria M, D'Amico B, Montecucco A, Martini M, Dini G, Durando P. Susceptibility to vaccine-preventable diseases and vaccination adherence among healthcare workers in Italy: A crosssectional survey at a regional acute-care university hospital and a systematic review. Hum Vaccin Immunother. 2017;13:470–476. doi: 10.1080/21645515.2017.1264746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals--A review of studies on attitudes and predictors. Vaccine. 2009;27:3935–3944. doi: 10.1016/j.vaccine.2009.03.056. [DOI] [PubMed] [Google Scholar]
- 21.Patricia Nowalk M, Chyongchiou JL, Mahlon R, Bialor J, Zimmerman RK. Impact of hospital policies on health care workers’ influenza vaccination rates. Am J Infect Control. 2013;41:697–701. doi: 10.1016/j.ajic.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 22.Lu P-J, Euler GL. Influenza, hepatitis B, and tetanus vaccination coverage among health care personnel in the United States. Am J Infect Control. 2011;39:488–494. doi: 10.1016/j.ajic.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 23.Hofmann F, Ferracin C, Marsh G, Dumas R. Influenza Vaccination of Healthcare Workers: a Literature Review of Attitudes and Beliefs. Infection. 2006;34(3):142–147. doi: 10.1007/s15010-006-5109-5. [DOI] [PubMed] [Google Scholar]
- 24.Fortunato F, Tafuri S, Cozza V, Martinelli D, Prato R. Low vaccination coverage among italian healthcare workers in 2013. Hum Vaccin Immunother. 2015;11:133–139. doi: 10.4161/hv.34415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scatigna M, Fabiani L, Micolucci G, Santilli F, Mormile P, Giuliani AR. Attitudinal variables and a possible mediating mechanism for vaccination practice in health care workers of a local hospital in L'Aquila (Italy) Hum Vaccin Immunother. 2017;13:198–205. doi: 10.1080/21645515.2016.1225638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review. Soc Sci Med. 2014;112:1–11. doi: 10.1016/j.socscimed.2014.04.018. [DOI] [PubMed] [Google Scholar]
- 27.Takayanagi IJ, Cardoso MRA, Costa SF, Araya MES, Machado CM. Attitudes of health care workers to influenza vaccination: Why are they not vaccinated? Am J Infect Control. 2007;35(1):56–61. doi: 10.1016/j.ajic.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 28.MacDonald NE SAGE Working Group on Vaccine Hesitancy, author. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 29.Schuster M, Eskola J, Duclos P SAGE Working Group on Vaccine Hesitancy, author. Hesitancy. Review of vaccine hesitancy: Rationale, remit and methods. Vaccine. 2015;33:4157–4160. doi: 10.1016/j.vaccine.2015.04.035. 14. [DOI] [PubMed] [Google Scholar]
- 30.Odone A, Signorelli C. What are we told? A news media monitoring model for public health and the case of vaccines. Eur J Public Health. 2016;26:533–534. doi: 10.1093/eurpub/ckw002. [DOI] [PubMed] [Google Scholar]
- 31.Odone A, Signorelli C. When vaccine hesitancy makes headlines. Vaccine. 2017;35:1209–1210. doi: 10.1016/j.vaccine.2015.11.051. [DOI] [PubMed] [Google Scholar]
- 32.Betsch C, Wicker S. Personal attitudes and misconceptions, not official recommendations guide occupational physicians' vaccination decisions. Vaccine. 2014;32:4478–4484. doi: 10.1016/j.vaccine.2014.06.046. [DOI] [PubMed] [Google Scholar]
- 33.Vasilevska M, Ku J, Fisman DN. Factors Associated with Healthcare Worker Acceptance of Vaccination: A Systematic Review and Meta-analysis. Infect Control Hosp Epidemiol. 2014;35(06):699–708. doi: 10.1086/676427. doi: 10.1086/676427. [DOI] [PubMed] [Google Scholar]
- 34.Loulergue P, Moulin F, Vidal-Trecan G, Absi Z, Demontpion C, Menager C, Menager C, Gorodetsky M, Gendrel D, Guillevin L, et al. Knowledge, attitudes and vaccination coverage of healthcare workers regarding occupational vaccinations. Vaccine. 2009;27:4240–4243. doi: 10.1016/j.vaccine.2009.03.039. [DOI] [PubMed] [Google Scholar]
- 35.Dinelli MIS, Neves Fraga Moreira das T, Regina Cruz Paulino E, Pereira da Rocha MC, Bracale Graciani F, Moraes-Pinto MI. Immune status and risk perception of acquisition of vaccine preventable diseases among health care workers. Am J Infect Control. 2009;37:858–860. doi: 10.1016/j.ajic.2009.04.283. [DOI] [PubMed] [Google Scholar]
- 36.Riccò M, Cattani S, Casagranda F, Gualerzi G, Signorelli C. Knowledge, attitudes, beliefs and practices of Occupational Physicians towards vaccinations of Health Care Workers: a cross sectional pilot study from North-Eastern Italy. Int J Occup Med Environ Health. 2017;30 doi: 10.13075/ijomeh.1896.00895. in press. [DOI] [PubMed] [Google Scholar]
- 37.Calabrese G, Gallone MS, Tafuri S. Knowledge, attitudes, and practices of occupational health physicians in the promotion of vaccinations recommended for health care workers: An Italian study. Am J Infect Control. 2016;44:1758–1759. doi: 10.1016/j.ajic.2016.05.042. [DOI] [PubMed] [Google Scholar]
- 38.Abbritti G, Apostoli P, Iavicoli S, Murgia N, Persechino B, Soleo L, Ambrosi L. Needs, education and accreditation in occupational medicine in Italy. Int Arch Occup Environ Health. 2004;78:75–78. doi: 10.1007/s00420-004-0552-z. [DOI] [PubMed] [Google Scholar]
- 39.Ramistella E, Maviglia A. Professional activity of "competent physician" actual troubles and future perspectives. G Ital Med Lav Erg. 2010;32:441–444. [PubMed] [Google Scholar]
- 40.Zingg A, Siegrist M. Measuring people's knowledge about vaccination: Developing a one-dimensional scale. Vaccine. 2012;30:3771–3777. doi: 10.1016/j.vaccine.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 41.Reyna VF. Risk perception and communication in vaccination decisions: A fuzzy-trace theory approach. Vaccine. 2012;30(25):3790–3797. doi: 10.1016/j.vaccine.2011.11.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Awali RA, Samuel PS, Marwaha B, Ahmad N, Gupta P, Kumar V, Ellsworth J, Flanagan E, Upfal M, Russell J, et al. Understanding health care personnel's attitudes toward mandatory influenza vaccination. Am J Infect Control. 2014;42:649–652. doi: 10.1016/j.ajic.2014.02.025. [DOI] [PubMed] [Google Scholar]
- 43.Alicino C, Iudici R, Barberis I, Paganino C, Cacciani R, Zacconi M, Battistini A, Bellina D, Bella AM, Talamini A, et al. Influenza vaccination among healthcare workers in Italy. Hum Vaccin Immunother. 2014;11:95–100. doi: 10.4161/hv.34362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Black S, Rappuoli R. A Crisis of Public Confidence in Vaccines. Sci Transl Med. 2010;2:61mr1–61mr1. doi: 10.1126/scitranslmed.3001738. [DOI] [PubMed] [Google Scholar]
- 45.Gilca V, Boulianne N, Dubé E, Sauvageau C, Ouakki M. Attitudes of nurses toward current and proposed vaccines for public programs: A questionnaire survey. Int J Nurs Stud. 2009;46:1219–1235. doi: 10.1016/j.ijnurstu.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 46.Leask J. Target the fence-sitters. Nature. 2011;473:443–445. doi: 10.1038/473443a. [DOI] [PubMed] [Google Scholar]
- 47.Rachiotis G, Mouchtouri VA, Kremastinou J, Gourgoulianis K, Hadjichristodoulou C. Low acceptance of vaccination against the 2009 pandemic influenza A(H1N1) among healthcare workers in Greece. Euro Surveill. 2010;15 pii=19486. [PubMed] [Google Scholar]
- 48.Cadeddu C, Thiene D, Ricciardi W, Boccia A, La Torre G. Knowledge about pandemic flu among Italian health care workers (HCWs) an Italian survey. J Prev Med Hyg. 2011;52:127–130. [PubMed] [Google Scholar]
- 49.Falato R, Ricciardi S, Franco G. [Influenza risk perception and vaccination attitude in medical and nursing students during the vaccination campaigns of 2007-2008 (seasonal influenza) and 2009/2010 (H1N1 influenza)]. Med Lav. 2011;102:208–215. [PubMed] [Google Scholar]
- 50.Spadea A, Unim B, Ursillo P, Saulle R, Giraldi G, Miccoli S, Barbato A, Corda B, D'Amici AM, Boccia A, et al. [Effectiveness of a training course on influenza vaccination in changing medical students" and healthcare workers" attitudes towards vaccination]. Ig Sanita Pubbl. 2013;69:387–402. [PubMed] [Google Scholar]
- 51.Boccia A, Thiene D, Giusti M, La Torre G. Seasonal and pandemic influenza: the role of communication and preventive strategies. J Prev Med Hyg. 2011;52:124–126. [PubMed] [Google Scholar]
- 52.Hayase Y, Tobita K. Influenza virus and neurological diseases. Psychiatry Clin Neurosci. 1997;51:181–184. doi: 10.1111/j.1440-1819.1997.tb02580.x. [DOI] [PubMed] [Google Scholar]
- 53.Dale RC. Encephalitis lethargica syndrome: 20 new cases and evidence of basal ganglia autoimmunity. Brain. 2004;127:21–33. doi: 10.1093/brain/awh008. [DOI] [PubMed] [Google Scholar]
- 54.Bellini WJ, Rota JS, Lowe LE, Katz RS, Dyken PR, Zaki SR, Shieh WJ, Rota PA. Subacute Sclerosing Panencephalitis: More Cases of This Fatal Disease Are Prevented by Measles Immunization than Was Previously Recognized. J Infect Dis. 2005;192:1686–1693. doi: 10.1086/497169. [DOI] [PubMed] [Google Scholar]
- 55.Leslie DL, Kobre RA, Richmand BJ, Aktan Guloksuz S, Leckman JF. Temporal Association of Certain Neuropsychiatric Disorders Following Vaccination of Children and Adolescents: A Pilot Case-Control Study. Front Psychiatry. 2017;8:1–8. doi: 10.3389/fpsyt.2017.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pasquale A, Bonanni P, Garçon N, Stanberry LR, El-Hodhod M, Silva FT. Vaccine safety evaluation: Practical aspects in assessing benefits and risks. Vaccine. 2016;34:6672–6680. doi: 10.1016/j.vaccine.2016.10.039. [DOI] [PubMed] [Google Scholar]
- 57.Rose SB, Lanumata T, Lawton BA. Promoting uptake of the HPV Vaccine: the knowledge and views of school staff. J Sch Health. 2011;81:680–687. doi: 10.1111/j.1746-1561.2011.00644.x. [DOI] [PubMed] [Google Scholar]
- 58.Goldstein ST, Cassidy WM, Hodgson W, Mahoney FJ. Factors associated with student participation in a schoolbased hepatitis B immunization program. J Sch Health. 2001;71:184–187. doi: 10.1111/j.1746-1561.2001.tb07313.x. [DOI] [PubMed] [Google Scholar]
- 59.Tung CS, Middleman AB. An evaluation of school-level factors used in a successful school-based hepatitis B immunization initiative. J Adolesc Health. 2005;37:61–68. doi: 10.1016/j.jadohealth.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 60.Verger P, Flicoteaux R, Schwarzinger M, Sagaon-Teyssier L, Peretti-Watel P, Launay O, Sebbah R, Moatti JP. Pandemic Influenza (A/H1N1) Vaccine Uptake among French Private General Practitioners: a Cross Sectional Study in 2010. PLoS ONE. 2012;7:e41837–e41838. doi: 10.1371/journal.pone.0041837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Flicoteaux R, Pulcini C, Carrieri P, Schwarzinger M, Leport C, Verger P. Correlates of general practitioners' recommendations to patients regarding vaccination for the 2009-2010 pandemic influenza (A/H1N1) in France: Implications for future vaccination campaigns. Vaccine. 2014;32:2281–2287. doi: 10.1016/j.vaccine.2014.02.074. [DOI] [PubMed] [Google Scholar]
- 62.Betsch C, Korn L, Holtmann C. Don't try to convert the antivaccinators, instead target the fence-sitters. Proc Natl Acad Sci U S A. 2015;112:E6725–E6726. doi: 10.1073/pnas.1516350112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Larson HJ, Jarrett C, Schulz WS, Chaudhuri M, Zhou Y, Dubé E, Schuster M, MacDonald NE, Wilson R Sage Working Group on Vaccine Hesitancy, author. Measuring vaccine hesitancy: The development of a survey tool. Vaccine. 2015;33:4165–4175. doi: 10.1016/j.vaccine.2015.04.037. [DOI] [PubMed] [Google Scholar]
- 64.Phillips DL, Clancy KJ. Some effects of "Social Desirability" in Survey Studies. Am J Sociol. 1972;77:921–940. [Google Scholar]
- 65.Sheth J, Malhotra NK, editors. Chapter 2: Grimm P. Social Desirability Bias Chichester, UK: John Wiley & Sons, Ltd; 2010. Wiley International Encyclopedia of Marketing. [Google Scholar]
- 66.Gregori V, Franchino G, Marcantoni C, Simone B, Costantino C. Logistic regression of attitudes and coverage for influenza vaccination among Italian Public Health medical residents. J Prev Med Hyg. 2014;55:152–157. [PMC free article] [PubMed] [Google Scholar]
- 67.Quach S, Pereira JA, Heidebrecht CL, Kwong JC, Guay M, Crowe L, Quan S, Bettinger JA Public Health Agency of Canada/ Canadian Institutes of Health Research Influenza Research Network (PCIRN) Vaccine Coverage Theme Group, author. Health care worker influenza immunization rates: The missing pieces of the puzzle. Am J Infect Control. 2013;41:685–690. doi: 10.1016/j.ajic.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 68.Quach S, Pereira JA, Kwong JC, Quan S, Crowe L, Guay M, Bettinger JA Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) Program Delivery and Evaluation Theme Group, author. Immunizing health care workers against influenza: A glimpse into the challenges with voluntary programs and considerations for mandatory policies. Am J Infect Control. 2013;41:1017–1023. doi: 10.1016/j.ajic.2013.05.016. [DOI] [PubMed] [Google Scholar]