Summary
Introduction.
Hospital infections, or "healthcare associated infections" (HAI) represent the most common and serious complications of healthcare. Adoption of safe care practices able to prevent or control the transmission of infections, both in hospitals and in other healthcare settings is crucial. The aim of the study is to assess the awareness about the risk factors and the most effective measures of prevention of HAI in the University of Ferrara nursing school students, giving particular attention to the hand hygiene practices and the use of standard precautions.
Methods.
339 students attending all the three years of course of the same academic year were enrolled. An anonymous questionnaire was administered in order to investigate the knowledge about three specific areas: infections associated with healthcare practices (HAI), standard precautions (SP) and hand hygiene (HH).
Results.
A sufficient level of knowledge by all the three groups of students was observed only in the SP area. A barely sufficient score was reached only by the third year students with regard to the proper HH. The level of knowledge about HAI was inadequate.
Conclusions.
A periodically check of nursing students' knowledge would be advisable in order to fill any gaps, improve training, reduce HAI and increase prevention measures compliance.
Key words: healthcare associated infections, nursing students, hand hygiene, standard precautions
Introduction
Healthcare associated infections (HAI) also referred to as "nosocomial" or "hospital" infections represent the most frequent and serious complications of healthcare [1, 2].
They are defined as infections, occurring in a patient 48 hours or more after admission to a hospital, that was not present or incubating at the time of admission. The infection can be acquired during the process of care in a hospital or other healthcare facility (primary care, nursing home care and outpatient services) [1].
HAI affect primarily patients and, less often, hospital staff, students and trainees [3]. Nurses and students that perform invasive procedures are particularly at risk. An Italian survey [4] showed a lower percentage of occupational injuries with biological risk in nursing students than in nurses (18.82% versus 81.18% respectively), that could be related to suitable and recent university training and proper use of personal protective equipment.
Around the 80% of HAI involves four main areas: the urinary tract (accounting for 35-40% of all HAI), surgical wounds, the respiratory system and systemic infections (sepsis, bacteremia) [3]. However, in the last fifteen years, a rising number of cases of bacteremia and pneumonia were observed and this can be the consequence of a progressive increase in specific risk factors, in particular, the frequent and or inappropriate use of antibiotics and vascular catheterizations. In 2011-2012, 29 EU member states and Croatia participated in a prevalence study on HAI and the use of antibiotics in acute care hospitals, coordinated by the European Centre for Disease Prevention and Control (ECDC) [5]. The prevalence of HAI varied from 4.8% in first-level hospitals to 7.2% in those of the third level. The patients of intensive care units were more affected, 19.5% of them having at least one infection than an average value of 5.2% of other clinical units.
The most frequently isolated microorganisms were Escherichia coli (15.9%), Staphylococcus aureus (12.3%), Enterococcus spp (9.6%) and Pseudomonas aeruginosa (8.9%). A considerable antibiotic resistance was observed. The HAI prevalence in Italy (6.6%) was similar to the European average (6.0%, with values ranging from 2.3% to 10.8% in the different countries), while the incidence of some infections (for example, the infections related with vascular catheterizations) was higher than in other European countries. However, in Italy, the problem is even more dramatic because of the spread of multidrug resistant microorganisms [5]. According to a recent Italian survey on HAI [6], Escherichia coli was the most common pathogen isolated in microbiological samples, followed by Klebsiella pneumoniae and Enterococcus faecalis.
The World Health Organization (WHO) [7, 8] indicated some key factors for the management and control of HAI: the improvement of reporting and surveillance systems both at national and local level as part of a prevention program; the implementation of preventive measures, particularly adequate hand hygiene practices, principally at the bedside and during invasive procedures; the promotion of healthcare workers training and responsibility.
Hand hygiene is a critical issue in HAI prevention. This preventive procedure is strongly recommended by WHO that recently promoted a worldwide campaign in order to encourage hand washing [9]. Nonetheless the use of alcohol-based products for hand hygiene should be further promoted: a study on 49 Italian hospitals showed a consumption lower than 10 litres per 1,000 days of hospitalization (the lowest category in Europe), against an European average of 18.7 litres/1,000 with peaks of 40 in the Scandinavian countries [5].
Major consequences of HAI are the delay of patients' recovery, extended hospitalization and the need of subsequent outpatient controls (e.g. for surgical wound infections). According to the Centre for Disease Control (CDC) [10], the hospitalization is prolonged up to 4 days for urinary tract infection, up to 3 weeks for sepsis and up to a month for pneumonia.
In addition, HAI represent a cost, not only a financial burden for the utilization of healthcare service but also for human suffering of patients, families and personnel. About 450,000-700,000 infections are annually acquired in Italian hospitals (first of all urinary infections, followed by surgical wound infections, pneumonia and sepsis). Of these, about 30% of cases (135,000-210,000), and 1% of deaths (1,350-2,100 deaths/year) are potentially preventable, respectively [11].
The adoption of safe healthcare practices, able to prevent or control the transmission of infections both in hospitals and in other healthcare setting are strongly required. Despite new emerging microorganisms that the healthcare workers are facing (e.g., hepatitis B and C viruses, human immunodeficiency virus, vancomycin-resistant enterococci [VRE], methicillin resistant Staphylococcus aureus [MRSA], avian or pandemic influenza viruses), the standard precautions still remain essential [12] and the nursing staff quality of training is a key element in the prevention and control of HAI [13].
As the potential infectious condition of a hospitalized patient is unknown, nursing students, as the healthcare workers, are at an elevated risk of exposure to biological agents [14]. It is therefore particularly important that not only the professionals but also the students early acquire knowledge of the possible risks of infection connected to healthcare and acquire skills regarding the use of main preventive measures.
The aim of the study was to assess the knowledge about the risk and the most effective measures of prevention of HAI in students of an Italian university nursing school during their 3 years of course, giving particular attention to hand hygiene practices and the use of standard prophylactic precautions. Moreover, potential areas of major criticisms were explored in order to offer useful guidance for the improvement of the training (both theoretical and practical activities).
Methods
The study was carried out by first, second and third year nursing students of the same academic year attending the University of Ferrara (Italy). All students have completed at least one training course (theoretical and or practical) learning information about HAI.
Preliminary information about the purpose, the protocol and the method of the study, including guarantee of anonymity was supplied (according to Legislative Decree no. 196/2003 "Code concerning the protection of personal data").
The research was carried on in accordance with the World Medical Association Declaration of Helsinki. It does not report any experiment on human or biological samples, nor research on identifiable human material and data because it is an observational survey conducted by an anonymous questionnaire among university students. Indeed, in order to protect the privacy of the subjects and confidentiality of their personal information and to minimize the impact of the study on their physical, mental and social integrity (stated in the article n. 23 of the above mentioned Helsinki declaration) the research was wholly conducted anonymously; thus no identifiable personal data are reported. Verbal informed consent was obtained from all subjects.
Characteristics of the questionnaire
An anonymous questionnaire was used in order to investigate students' knowledge about three specific areas: Healthcare Associated Infections (HAI), Standard Precautions (SP) and Hand Hygiene (HH). The questionnaire was developed on the model of that used by Tavolacci et al., 2008 [15], with slight modification in order to adapt to Italian epidemiological situation. The first part was dedicated to the demographic aspects (age, gender, year of attendance), followed by a question concerning the correct definition of HAI. The second section was composed of six questions, each of which contains statements that require a dichotomous response (true, false) for a total of 25 responses. Each area had a maximum of 10 points for an overall score of 30, excluding the first question on HAI definition that received no score. In detail, HAI area consisted of a single question with 5 dichotomous responses (2 points per response); SP consisted of 3 questions each with four answers (0.83 points per response) and HH was composed by 2 questions each with four answers (1.25 points per response). Acceptable score was arbitrarily set at ≥ 7, according to Tavolacci et al., 2008 [15].
Statistical analysis
The answers have been collected in a database using Microsoft Excel 2007. The obtained data were analysed by Statview® 5.0.1 software (Abacus Concepts, Berkeley, CA, USA). ANOVA was applied to reveal the difference in the average score of the three different areas, according to the year of attendance. The chi-square test was used to detect the differences in students' knowledge according to year of attendance for each question. A value of p < 0.05 was considered statistically significant.
Results
The study recruited 339 students attending a degree course in nursing (with a response rate of 51% considering the total number of students enrolled in the three years of course), of whom 203 (59.9%) at the first year, 88 (25.9%) at the second year and 48 (14.2%) at the third year, respectively. The 64.3% of the participants were aged less than 22 and 74.6% were female (Table I). The percentage of correct answers to HAI section is reported in Table II. The majority of the students of all the three years precisely identified age and invasive procedure as risk factors for HAI onset (with a statistically significant difference between the years of course of 0.0044 and 0.0117 respectively). The awareness of environment as source of infection increased with the continuation of the training (p < 0.0001). Surprisingly the third year students gave the correct answer to HAI associated mortality to a lesser extent than the students of first and second year (p = 0.0130). No difference was found about knowledge of HAI prevalence rate.
Tab. I.
Characteristics of the sample of the 339 nursing students.
| Socio-demographic characteristics | Frequency N (%) | First year N (%) | Second year N (%) | Third year N (%) |
|---|---|---|---|---|
| Age | ||||
| < 22 years | 218 (64.3) | 158 (77.8) | 52 (59.1) | 8 (16.7) |
| ≥ 22 years | 121 (35.7) | 45 (22.2) | 36 (40.9) | 40 (83.3) |
| Gender | ||||
| Females | 253 (74.6) | 154 (75.9) | 63 (71.5) | 36 (75.0) |
| Males | 86 (25.4) | 49 (24.1) | 25 (28.5) | 12 (25.0) |
| Total | 339 (100) | 203 (59.9) | 88 (25.9) | 48 (14.2) |
Tab. II.
Percentages of correct answers to the healthcare associated infections section according to the year of course.
| HAI Section | First year | Second year | Third year | p value |
|---|---|---|---|---|
| The environment is the major source of bacteria | 20.2% | 39.8% | 45.8% | <0.0001 |
| Advanced age or very young age increases the risk | 70.4% | 87.5% | 85.4% | 0.0044 |
| Invasive procedures increase the risk | 89.7% | 96.6% | 100% | 0.0117 |
| Nosocomial infection has a prevalence ranging between 5% to 10% in Italy | 44.8% | 47.7% | 41.7% | 0.7320 |
| Nosocomial infections are responsible for approximately 5,000 deaths per year in Italy | 50.7% | 47.7% | 27.1% | 0.0130 |
The features regarding the adoption of standard precautions and the risk of contamination with biological fluids (SP section) were well known by students of all three years of course with correct response rates very close or up to 100% (Table III). The indications for the use of gloves have been well known without any differences between the students attending all years of training, except for the recommendation on the use of gloves for all procedures that, although with an upward trend, was correctly indicated only by half of the third year students with a statistically significant difference between the three years of the course (p < 0.0001).
Tab. III.
Percentages of correct answers to the standard precautions section according to the year of course.
| SP Section | First year | Second year | Third year | p value |
|---|---|---|---|---|
| Standard precautions | ||||
| Include recommendations to protect only the patients | 93.6% | 95.5% | 100% | 0.1790 |
| Include recommendations to protect the patients and the healthcare workers | 97.5% | 98.9% | 100% | 0.4368 |
| Apply for all the patients | 95.1% | 97.7% | 35.4% | 0.4297 |
| Apply for only healthcare workers who have contact with body fluid | 93.1% | 94.3% | 91.7% | 0.8268 |
| Use of gloves is recommended | ||||
| For each procedure | 23.2% | 61.4% | 50% | <0.0001 |
| When there is a risk of contact with the blood or body fluid | 95.6% | 95.5% | 100% | 0.3279 |
| When there is a risk of a cut | 82.3% | 69.3% | 75% | 0.0527 |
| When healthcare workers have a cutaneous lesion | 94.1% | 96.6% | 95.8% | 0.9040 |
| When there is a risk of splashes or spray of blood and body fluids, the healthcare workers must wear | ||||
| Only mask | 97.5% | 95.5% | 100% | 0.2866 |
| Only eye protection | 97.5% | 95.5% | 97.9% | 0.6974 |
| Only a gown | 95.6% | 97.7% | 100% | 0.2423 |
| Mask, goggles and gown | 98% | 98.9% | 97.9% | 0.8640 |
The recommendations for hand hygiene were correctly recognised by almost all the students without statistically significant difference between the years of attendance (Tab. IV). Low percentages of corrected answer were observed for all questions regarding the use of alcoholbased solutions. The notions about the substitution of traditional handwashing and that alcohol-based products do not require association with traditional handwashing increased with training progression, with a statistically significant difference of 0.0038 and 0.0247 respectively. The availability of substitute antiseptic handwashing with alcohol-based products was known by less than the half of students in all the three years of course (p = 0.0407). A very scarce knowledge about the possible substitution of surgical handwashing was observed with a statistically significant difference between the years of attendance (p < 0.0001).
Tab. IV.
Percentages of correct answers to the hand hygiene section according to the year of course.
| HH Section | First year | Second year | Third year | p value |
|---|---|---|---|---|
| Recommendations for hand hygiene | ||||
| Before or after a contact with (or care of) a patient | 87.2% | 85.2% | 93.8% | 0.3476 |
| Before and after a contact with (or care of) a patient | 99.0% | 100.0% | 100.0% | 0.5055 |
| Between patient contacts | 96.6% | 97.7% | 95.8% | 0.8012 |
| After the removal of gloves | 85.2% | 79.5% | 87.5% | 0.4019 |
| Directions for use of alcoholic solutions | ||||
| instead of a traditional handwashing (30 s) | 43.3% | 62.5% | 62.5% | 0.0038 |
| instead of a antiseptic handwashing (30 s) | 49.8% | 33.0% | 47.9% | 0.0407 |
| instead of surgical handwashing (3 min) | 30.5% | 5.7% | 12.5% | < 0.0001 |
| A traditional handwashing must be done before handwashing with alcohol-based hand rub | 42.9% | 39.8% | 62.5% | 0.0247 |
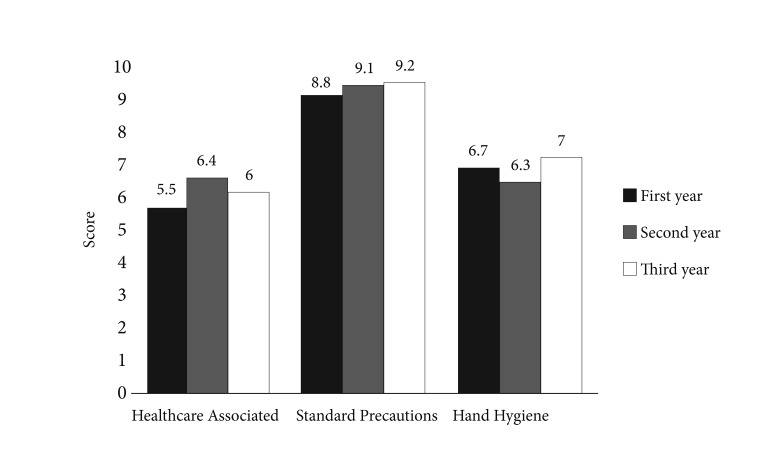
According to Tavolacci et al. [15], the total score reached in the different areas was calculated considering acceptable a value greater or equal to 7 (Table V, Fig. 1). Overall score was sufficient for all investigated students but insufficient scores were achieved for HAI and HH areas. A satisfactory score was obtained only for SP area in all the years of course. The score in HAI area did not reach an adequate level not even at the third year, while knowledge about HH just reached the sufficiency at the last year of training.
Tab. V.
Score for each area according to year of course.
| HAI | SP | HH | Total Score | |
|---|---|---|---|---|
| First year | 5.5 | 8.8 | 6.7 | 21.0 |
| Second Year | 6.4 | 9.1 | 6.3 | 21.8 |
| Third year | 6.0 | 9.2 | 7.0 | 22.2 |
| Total | 5.8 | 8.9 | 6.6 | 21.4 |
Fig. 1.
Scores obtained in the 3 investigated sections (HAI, SP, HH).
Discussion
In agreement with the results obtained by Tavolacci et al. in 2008 [15], a sufficient level of knowledge, identified by a score ≥ 7, was reached by all three groups of students, only in the section regarding SP.
This finding implies a good level of preparation already from the first year of the course about this topic. A barely sufficient score was reached only by the third year students with regard to the proper HH. For all the other areas, the level of knowledge shown by the students belonging to the three years was inadequate. This is particularly true for the section regarding the HAI. This outcome is once more in agreement with Tavolacci et al. [15], which reported lower scores concerning the knowledge of HAI not only by the nursing school students, but also by the medical, physiotherapy and assistant radiologist students. Also another study, conducted in 2014 by Mitchell et al. [16] on nursing school students, showed a higher level of knowledge on SP, with a percentage of 88.9% of correct answers.
The worst knowledge involved mainly prevalence and mortality associated to HAI and the role of the setting in their onset, while the role of age and invasive procedure were more recognised. More efforts should be undertaken to emphasize the severity of HAI so that students do not underestimate the burden and importance of this topic.
An excellent level of knowledge emerges with regards to SP from all three years of the course; nevertheless an insufficient awareness of the necessity to wear gloves for all the patients was observed. A previous study conducted on nursing school students of the same University identified as main gap the belief that the SP (in particular the use of gloves) are necessary for a self-protection and not to prevent hospital infections [17].
As for the proper HH, all the students show lack of knowledge mainly regarding appropriate use of alcohol-based solutions, particularly in substitution of traditional and surgical handwashing. Nonetheless, the observed differences between the students are not due to different training programs because all the students attended the same university and healthcare settings. The better awareness about standards precautions than other issues can be attributed to the practical experience already started from the first year, while more theoretical topics, such as epidemiology, tend to be undersupplied. D'Alessandro et al. [18] evaluated, by means of a questionnaire, the knowledge of both nursing and medical students in the same areas. This study involved 607 medical students and 854 nursing school students, from 9 Italian universities and revealed better knowledge from the nursing school students than the medical students on the three examined topics and, among the same nursing school students, a better level of knowledge by the younger subjects (< 24 years of age). This finding is opposite to our result that showed better scores from the students at the last year of course, in agreement with Cheung et al. [19] that revealed a better compliance towards SP within the students of the second and third years of the course.
Conclusions
The nursing personnel play an important role in the prevention and management of HAI and the combination of the theoretical and practical training can improve the knowledge of the nurses and the quality of assistance. To date, literature data confirm how the awareness about HAI of future nursing school graduates is often already inadequate.
The information for the prevention of HAI should be reiterated to the students after the completing of each procedure with the aim of increasing the awareness of their own role in reducing HAI [20].
It would be advisable to periodically check the knowledge of the students to improve training and consequently reduce HAI, giving the students more responsibility in the area of healthcare and increasing their compliance with prevention, giving more scope to on the field training through the support of a tutor demonstrating in practice what they have learned in theory.
Limits of the study
The study was carried out on students attending the lessons of the degree course who were administered the questionnaire; the difference in the numbers of the three years is due to that the practical training gradually increases and the students attend the theoretical lessons to a lesser extent.
Nevertheless, the results obtained are in line with those reported in other studies in the literature.
ACKNOWLEDGMENTS
GG received grants from GlaxoSmithKline Biologicals SA, Sanofi Pasteur MSD, Novartis, Crucell/Janssen, Sequirus, Sanofi Pasteur MSD Italy and Pfizer for being consultant or taking part in advisory board, expert meetings, being a speaker or an organizer of congresses/conferences, and acting as investigator in clinical trials; BF, KP, SA, GE, LS, SN, BM have no conflicts to disclose.
References
- 1.Bello AI, Asiedu EN, Adegoke BO, Quartey JN, Appiah-Kubi KO, Owusu-Ansah B. Nosocomial infections: knowledge and source of information among clinical healthcare students in Ghana. Int J Gen Med. 2011;4:571–574. doi: 10.2147/IJGM.S16720. doi: 10.2147/IJGM. S16720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pittet D. Infection control and quality health care in the new millennium. Am J Infect Control. 2005;33:285–267. doi: 10.1016/j.ajic.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 3. Epicentro. Infezioni Correlate all'Assistenza. Avalaible at: http://www.epicentro.iss.it/problemi/infezioni_correlate/infezioni.asp [Accessed 25/10/2016].
- 4.Stefanati A, Boschetto P, Previato S, Kuhdari P, Paris P, Nardini M, Gabutti G. A survey on injuries among nurses and nursing students: a descriptive epidemiologic analysis between 2002 and 2012 at a University Hospital. Med Lav. 2015;106:216–229. [PubMed] [Google Scholar]
- 5. European Centre for Disease Prevention and Control. Point prevalence survey of healthcare associated infections and antimicrobial use in European acute care hospitals. Stockholm ECDC 2013. doi 10.2900/86011.
- 6.Antonioli P, Manzalini MC, Stefanati A, Bonato B, Verzola A, Formaglio A, Gabutti G. Temporal trends of healthcare associated infections and antimicrobial use in 2011-2013, observed with annual point prevalence surveys in Ferrara University Hospital, Italy. J Prev Med Hyg. 2016;57:E135–E141. [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization. Health care without avoidable infections The critical role of infection prevention and control. Avalaible at: http://apps.who.int/iris/bitstream/10665/246235/1/WHO-HIS-SDS-2016.10-eng.pdf?ua=1 [Accessed 06/03/2017].
- 8. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. First Global Patient Safety Challenge Clean Care is Safer Care. Available at: http://www.who.int/gpsc/5may/tools/9789241597906/en/. Accessed [06/03/2017].
- 9. World Health Organization. Summary Report: Hand Hygiene Self-Assessment Framework Survey 2015/2016. WHO 2016. Avalaible at: http://www.who.int/gpsc/5may/hand-hygiene-report.pdf. Accessed [06/03/2017].
- 10.Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20:250–278. doi: 10.1086/501620. quiz 279-80. [DOI] [PubMed] [Google Scholar]
- 11. Epicentro. Infezioni correlate all'assistenza. Avalaible at: http:// www.epicentro.iss.it/problemi/infezioni_correlate/epid.asp. Accessed [25/10/2016].
- 12.Siegel JD, Rhinehart E, Jackson M, Chiarello L the Healthcare Infection Control Practices Advisory Committee, author. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. 2007. Avalaible at: http://www.cdc.gov/hicpac/pdf/isolation/isolation2007.pdf. Accessed [06/03/2017]. [DOI] [PMC free article] [PubMed]
- 13.Yokoe DS, Mermel LA, Anderson DJ, Arias KM, Burstin H, Calfee DP, Coffin SE, Dubberke ER, Fraser V, Gerding DN, et al. A compendium of strategies to prevent health care associated infections in acute care hospitals. Infect Control Hosp Epidemiol. 29:S12–S21. doi: 10.1086/591060. [DOI] [PubMed] [Google Scholar]
- 14. World Health Organization. Health worker occupational health. Available at: http://www.who.int/occupational_health/topics/hcworkers/en/index.html. Accessed [06/03/2017].
- 15.Tavolacci MP, Ladner J, Bailly L, Merle V, Pitrou I, Czernichow P. Prevention of nosocomial infection and standard precautions: knowledge and source of information among healthcare students. Infect Control Hosp Epidemiol. 2008;29:642–647. doi: 10.1086/588683. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell BG, Say R, Wells A, Wilson F, Cloete L, Matheson L. Australian graduating nurses' knowledge, intentions and beliefs on infection prevention and control: a cross-sectional study. BMC Nursing. 2014;13(1):43–43. doi: 10.1186/s12912-014-0043-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergamini M, Cucchi A, Stefanati A, Cavallaro A, Gabutti G. Knowledge of preventive measures against occupational risks and spread of healthcare-associated infections among nursing students. An epidemiological prevalence study from Ferrara, Italy. J Prev Med Hyg. 2009;50:96–101. [PubMed] [Google Scholar]
- 18.D'Alessandro D, Agodi A, Auxilia F, Brusaferro S, Calligaris L, Ferrante M, Montagna MT, Mura I, Napoli C, Pasquarella C, et al. Prevention of healthcare associated infections: medical and nursing students' knowledge in Italy. Nurse Educ Today. 2014;34:191–195. doi: 10.1016/j.nedt.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Cheung K, Chan CK, Chang MY, Chu PH, Fung WF, Kwan KC, Lau NY, Li WK, Mak HM. Predictors for compliance of standard precautions among nursing students. Am J Infect Control. 2015;43:729–734. doi: 10.1016/j.ajic.2015.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang R. Investigating the prevention of hospital-acquired infection through standardized teaching ward rounds in clinical nursing. Genet Mol Res. 2015;14:3753–3759. doi: 10.4238/2015.April.22.3. [DOI] [PubMed] [Google Scholar]