Abstract
Papua New Guinea (PNG) is a culturally, environmentally and ethnically diverse country of 7.3 million people experiencing rapid economic development and social change. Such development is typically associated with an increase in non-communicable disease (NCD) risk factors.
Aim
To establish the prevalence of NCD risk factors in three different regions across PNG in order to guide appropriate prevention and control measures.
Methods
A cross-sectional survey was undertaken with randomly selected adults (15–65 years), stratified by age and sex recruited from the general population of integrated Health and Demographic Surveillance Sites in West Hiri (periurban), Asaro (rural highland) and Karkar Island (rural island), PNG. A modified WHO STEPS risk factor survey was administered along with anthropometric and biochemical measures on study participants.
Results
The prevalence of NCD risk factors was markedly different across the three sites. For example, the prevalences of current alcohol consumption at 43% (95% CI 35 to 52), stress at 46% (95% CI 40 to 52), obesity at 22% (95% CI 18 to 28), hypertension at 22% (95% CI 17 to 28), elevated levels of cholesterol at 24% (95% CI 19 to 29) and haemoglobin A1c at 34% (95% CI 29 to 41) were highest in West Hiri relative to the rural areas. However, central obesity at 90% (95% CI 86 to 93) and prehypertension at 55% (95% CI 42 to 62) were most common in Asaro whereas prevalences of smoking, physical inactivity and low high-density lipoprotein-cholesterol levels at 52% (95% CI 45 to 59), 34% (95% CI 26 to 42) and 62% (95% CI 56 to 68), respectively, were highest in Karkar Island.
Conclusion
Adult residents in the three different communities are at high risk of developing NCDs, especially the West Hiri periurban population. There is an urgent need for appropriate multisectoral preventive interventions and improved health services. Improved monitoring and control of NCD risk factors is also needed in all regions across PNG.
Keywords: Papua New Guinea, Cross-sectional study, Non-communicable diseases, Risk factors
Key questions.
What is already known about this topic?
The prevalence of non-communicable diseases (NCDs) and their risk factors in Papua New Guinea is increasing but varied based on ethnicity, lifestyle and the living environment.
Current prevalence of NCD and their risk factors is unknown in West Hiri, a community impacted by a gas mining project and two rural non-project impact areas, Asaro and Karkar Island.
What are the new findings?
Our study provided a baseline prevalence of NCD risk factors in West Hiri and an up-to-date prevalence of NCD risk factors in Asaro and Karkar Island.
Results suggest that socioeconomic and nutrition transition may be under way in all sites but more apparent in the West Hiri population.
Recommendations for policy
The results strongly suggest an introduction of control measures particularly in West Hiri and continuous monitoring across the country.
Introduction
Non-communicable diseases (NCDs) are the leading cause of death and morbidity throughout the world, with the greatest burden in low and middle-income countries (LMICs), where nearly 80% of NCD-related deaths and 82% of all NCD premature deaths occur.1 2 According to the WHO, approximately 46% of all NCD-related deaths in 2012 were due to cardiovascular diseases (CVDs), followed by cancers (22%), respiratory disease (11%) and diabetes (4%).2 Furthermore, the global burden of diseases study reported that CVDs, such as ischaemic heart disease and stroke, continue to be among the top three leading causes of death globally.3
Papua New Guinea (PNG) is a country of approximately 7.3 million people located in the Western Pacific and renowned for its environmental, cultural and biological diversity.4 5 PNG is categorised as a lower-middle-income country according to the World Bank criteria6 and is experiencing rapid economic growth as a result of large-scale mineral and gas resource developments.7 Rapid economic growth in other LMICs has been associated with an epidemiological transition characterised by an increasing prevalence of NCDs and their risk factors with an often concomitant reduction in infectious disease.8 9 While infectious diseases such as acute respiratory tract infections, tuberculosis, malaria and HIV/AIDS are the leading causes of morbidity and mortality in PNG,10 the available evidence suggests this pattern is changing among those adult populations with longer exposure to modernisation. The latter is leading to rapid lifestyle changes associated with increases in CVD and diabetes.11–23 In addition, PNG still has high rates of childhood stunting,24–26 a risk factor for NCDs in adulthood.27 The cost of treating and managing a growing NCD burden is already posing a substantial challenge to the country’s economy, particularly given the challenges of the PNG health system, which include deteriorating infrastructure, poor governance, an ageing and inadequate healthcare workforce, and a paucity of specialist services.28
NCDs and associated risk factors, such as smoking, excessive alcohol consumption, stress, unhealthy diet, physical inactivity, obesity, hypertension and abnormal lipid profiles, have not been well investigated in PNG. Several small studies conducted among specific populations over the past few decades have identified an increasing, or relatively high, prevalence of NCDs and NCD risk factors.18 19 21 29–34 They suggest variations in NCD risks within PNG based on lifestyle and living environment18 19 21 29 and on ethnic origin.33 34 Furthermore, a lack of physical activity, particularly among urban migrants, increases the risk of acquiring an NCD19 21; and urban dwellers of any ethnic origin in PNG are at higher risk of CVDs and diabetes relative to their rural peers.19 21 31 32 35 The 2007/2008 PNG NCD Risk Factor STEPS study reported that the majority of surveyed adults were at risk of developing NCDs.36 Since the STEPS survey, there has been limited up-to-date information on the prevalence of NCD risk factors across the diverse populations of PNG. Major resource developments have occurred since the STEPS survey last decade, and there is a need for a comprehensive NCD risk survey during this period of development. Currently in PNG, there is no systematic monitoring of NCD prevalence, or the associated risk factors, to measure the anticipated epidemiological transition across the country.
The present study was undertaken during the construction phase of a large-scale gas development which was projected to more than double the gross domestic product of PNG.7 Our study was designed to provide baseline prevalence data on NCD risk factors in the initial years of a gas project impact site (West Hiri) and in two non-project impact sites (Asaro and Karkar). It was also anticipated that the study findings would provide up-to-date NCD prevalence data to help the national government plan services and develop cost-effective interventions. In this paper, we describe the methods used and present the initial findings for NCD risk factors in a survey of three different sociodemographic populations of PNG.
Methods
Study design
Between April 2013 and October 2014, we undertook a cross-sectional, community-based survey in three integrated Health and Demography Surveillance Sites (iHDSS) set up by the PNG Institute of Medical Research (PNGIMR).37 38 The study included the completion of a standardised questionnaire based on the WHO STEPwise approach for NCD Risk Factor surveillance,39 which included physical measurements and biological sample collection from randomly selected adults (aged 15–65 years) from the general population of each iHDSS. Information on health service utilisation was not collected but can be incorporated and reported in future NCD risk factor surveys and analysis. Further cross-sectional surveys of NCD risk factors and prevalence are planned for each iHDSS in the future, pending additional funding.
Sample size and selection
Using a simple random sampling procedure, a total of 300 adult participants, stratified by sex and age (15–29, 30–44, 45–65 years), were sought from each iHDSS (ie, 100 participants from each of the three age groups, 50 male and 50 female) and invited to take part in the study. The sampling frame was a full population census of the adult general population of each iHDSS. The target sample size (n=900) was estimated to confer 80% power to detect a 10% absolute difference in the proportion of most risk factors for all ages combined between each site or a 10% relative difference in means at the 0.05 significance level (two sided).
Study sites
The three iHDSS were West Hiri (Central Province), Asaro (Eastern Highlands Province) and Karkar Island (Madang Province) as shown in figure 1. The West Hiri iHDSS comprises villages with a baseline (2011) population of 11 531 people37 of Austronesian ancestry,40 distributed along a 20–30 km stretch of coastline north-west of Port Moresby, the national capital and largest city in PNG. The West Hiri site was selected because it represents a periurban population affected by a large gas development project. The villages surround a gas processing plant and their close proximity to Port Moresby has changed the traditional diet, social cohesion and skilled activities such as fishing and gardening.41 The Asaro iHDSS comprises a baseline (2011) population of 10 034 people37 38 of non-Austronesian ancestry,40 situated 40–45 km north-east of Goroka, the largest town in the Eastern highlands. People in Asaro are primarily subsistence farmers, but earn cash through smallholder production of coffee, employment on plantations and selling garden produce.42 The Karkar Island iHDSS comprises a rural baseline population of 18 623 people37 38 of both Austronesian and non-Austronesian ancestries43 located 30 km off the northern coastline of Madang Province. Most adult residents of Karkar Island are subsistence farmers and/or unskilled labourers. The island’s soil is fertile and large plantations produce the island’s main exports of cocoa and coconut and provide most of the local employment opportunities.37 38 The majority of PNG’s population live in rural areas and about 87% of the adult population is engaged in both subsistence farming and commercial activities.5 44 Therefore, Asaro and Karkar Island populations reflect rural communities that largely depend on subsistence farming and cash cropping in highlands and lowlands/coastal PNG, respectively.
Figure 1.
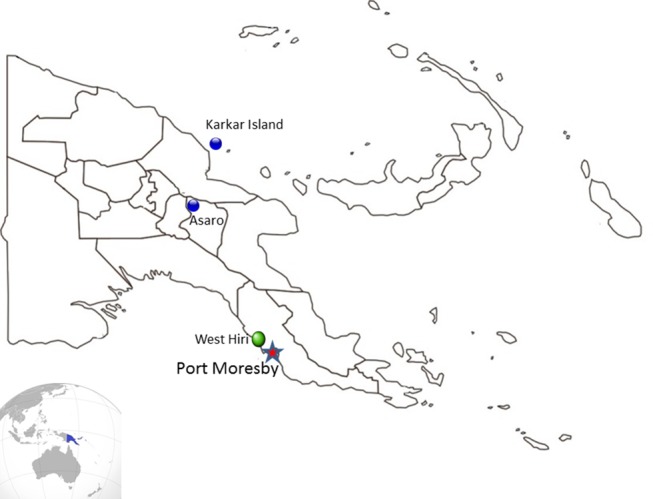
Map of Papua New Guinea showing the three survey sites: West Hiri (periurban) and two rural communities, Asaro and Karkar Island.
Study measures and collection methods
Interviews were conducted at participants’ homes or community health facilities. Eligibility criteria included recorded residence within the respective iHDSS and ages between 15 and 65 years at the time of survey. Women were excluded if they were pregnant at the time of recruitment. All survey forms and procedures were completed at a single time point by the survey team.
Interviews
The NCD study tool was adapted from the WHO STEPS NCD Risk Factor Survey.39 Question domains included: participant demographics; self-reported health status; self-reported stress; consumption of vegetables, fruits, protein, fried food, salt and sugar; food security; tobacco, betel nut and alcohol use; physical activity; participant history of NCD and/or associated treatments. The self-reported stress, diet and physical activity questions were all developed specifically for this study and for use with PNG-based populations. The questionnaire was available in English and Tok Pisin, the local creole language that the interviewers could speak fluently. All questionnaires were piloted extensively prior to survey commencement.
Measurement
Weight in kilograms (kg) was measured using a Seca digital scale to 100 g precision and height (cm) to 0.1 cm precision using a Seca Leicester stadiometer. Participants were able to wear light clothes, but no shoes. A Seca figure finder constant tension tape was used to measure to 0.1 cm precision the hip (level of widest part of the buttocks) and waist circumferences (midpoint between lower rib and iliac crest) in centimetre (cm). After participants had rested for 10 min in a sitting position their blood pressures (BP) were measured using an OMRON T9P digital automated sphygmomanometer. Three readings were taken at 1 min intervals using appropriate cuff sizes and the average of the three readings was used for the analysis.
Biochemical measures
Capillary blood from a finger prick was taken on the spot and analysed for haemoglobin levels using a HemoCue device (HemoCue Hb201+, Angelholm, Sweden). If haemoglobin levels were above 6 g/dL, a further 30 mL of non-fasting venous blood was collected. The initial 10 mL of blood was collected using EDTA vacutainers and analysed for haemoglobin A1c (HbA1c) levels using the DCA Vantage Analyzer from Siemens Healthcare Australia and New Zealand. The remaining 20 mL was collected using two 10 mL serum vacutainers which were aliquoted and stored initially at −20°C in each study site before they were transported to the Port Moresby PNGIMR laboratory. The serum samples were analysed for lipids (cholesterol and high-density lipoprotein-cholesterol (HDL-C)) using Vitros 250/350 Biochemistry System from Ortho Clinical Diagnostics, in batches within a month of collection. After analysis, aliquots of plasma, serum and cell pallets were stored initially at −20°C freezer in Port Moresby before archiving in −80°C freezer for long-term storage.
Measurement of NCD risk factors
Daily tobacco smoking was defined as current tobacco smoking on a daily basis and current alcohol consumption was defined as alcohol consumption within the last 30 days. Betel nut chewing which consists of areca nut, betel leaf/bean and slaked lime is widely practised across PNG and current use was defined as betel nut chewing within the last 30 days. Insufficient physical activity was defined as spending less than 75 or 150 min/week on vigorous and moderate physical activities, respectively.45 Body mass index (BMI) was calculated as weight (kg) divided by height in metres squared (m2). Overweight and obesity were defined as BMI ≥25–29.9 kg/m2 and ≥30 kg/m2, respectively.46 Central obesity in men and women was defined as a waist-to-hip ratio ≥0.90 and ≥0.85 for men and women, respectively.47 Hypertension was defined as the average of the three systolic and/or diastolic BP readings of ≥140 mm Hg and/or ≥90 mm Hg, respectively or diagnosed hypertensive cases on antihypertensive drugs.48 Prehypertension was defined as systolic and diastolic BPs of >120–139.9 mm Hg and >80–89.9 mm Hg, respectively.48 Elevated cholesterol levels were defined as cholesterol levels of >6.2 mm/L. Low HDL-C levels were defined as <1 mmol/L and <1.3 mmol/L for men and women, respectively.49 50 Participants with elevated HbA1c were defined to have HbA1c levels ≥5.7%. In accordance with the American Diabetes Association Standards of Medical Care in Diabetes, diabetes mellitus type 2 (DMT2) was diagnosed if the participant was on antidiabetic drugs or when the participants’ HbA1c was ≥6.5%.51
Data analysis
STATA/SE V.13.0 (StataCorp LP) was used for all data analyses. Analysis was limited to descriptive summaries of all major measures and inferential analyses to assess intersite differences for major outcome variables using Pearson’s χ2 test, Fisher’s exact test and one-way analysis of variance where appropriate. Risk factor prevalence with 95% CI for binary variables and the means with SD for continuous variables were examined by study site. More detailed analyses exploring relationships between specified risk factors and NCDs as well as lung function, haemoglobin and urine microalbumin levels, detailed dietary and physical activity results will be presented in subsequent publications. The totals (No.) presented in all tables are denominators unless otherwise stated. Tobacco, betel nut and alcohol questions were not originally included in the NCD questionnaire, and as a result, these questions were not asked of all participants. To address missing values, available case analysis was used.
Ethics approval
The study was given ethical approval by the PNGIMR Institutional Review Board (IRB) and the PNG Medical Research Advisory Committee (MRAC) (IRB No. 1208, 23 March 2012; MRAC No. 12.34, November 2012). Written, informed consent was obtained prior to study participation. Any participant identified with hypertension, DMT2, hyperlipidaemia or chronic obstructive pulmonary disease was referred to the local general hospital for further investigation and management.
Results
Of the total 900 randomly selected participants, 785 (87.2%) adults participated in the survey. Here we present the results of the 772 participants who completed the survey and had their blood collected. Table 1 presents the demographic characteristics of the overall study population and by iHDSS. The three study sites were comparable in terms of participants’ age and sex. Overall, 33% of study participants received an education past primary school level and only 16% were engaged in paid employment. Across the sites, West Hiri participants were better educated and more likely to be in paid employment compared with participants from Asaro and Karkar Island, where the majority were subsistence farmers/cash croppers.
Table 1.
Demographic characteristics of the participants of the non-communicable disease study by iHDSS. The values are numbers and percentages (95% CI)
| Overall (n=772) |
West Hiri (n=266) |
Asaro (n=254) |
Karkar Island (n=252) |
|||||
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | |
| Sex | ||||||||
| Male | 361 | 47 (43 to 50) | 114 | 43 (37 to 49) | 130 | 51 (45 to 58) | 117 | 46 (40 to 53) |
| Female | 411 | 53 (50 to 57) | 152 | 57 (51 to 63) | 124 | 49 (43 to 55) | 135 | 54 (48 to 60 |
| Age group (years) | ||||||||
| 15–29 | 216 | 28 (25 to 31) | 73 | 27 (22 to 33) | 69 | 27 (22 to 33) | 74 | 29 (24 to 35) |
| 30–44 | 261 | 34 (31 to 37) | 93 | 35 (29 to 41) | 88 | 35 (29 to 41) | 30 | 32 (8 to 17) |
| 45–65 | 295 | 38 (35 to 42) | 100 | 38 (32 to 44) | 97 | 38 (32 to 45) | 98 | 39 (33 to 45) |
| Education | ||||||||
| Primary or lower | 519 | 67 (64 71) | 119 | 45 (39 to 51) | 198 | 78 (72 to 83) | 202 | 80 (75 to 85) |
| Some/complete secondary | 159 | 21 (18 to 24) | 92 | 35 (29 to 41) | 28 | 11 (8 to 16) | 39 | 16 (11 to 21) |
| Vocational/tertiary | 26 | 3 (2 to 5) | 20 | 8 (5 to 11) | 3 | 1 (0 to 3) | 3 | 1 (0 to 3) |
| Don’t know | 68 | 9 (7 to 11) | 35 | 13 (9 to 18) | 25 | 10 (7 to 14) | 8 | 3 (1 to 6) |
| Employment | ||||||||
| Home duties | 157 | 20 (18 to 23) | 92 | 35 (29 to 41) | 15 | 6 (3 to 10) | 50 | 20 (15 to 25) |
| Subsistence/cash cropper | 349 | 45 (42 to 49) | 23 | 9 (6 to 13) | 179 | 71 (64 to 76) | 147 | 58 (52 to 65) |
| Paid employment | 121 | 16 (13 to 18) | 89 | 34 (28 to 40) | 15 | 6 (3 to 10) | 17 | 7 (4 to 11) |
| Unemployed/retired/student | 114 | 15 (12 to 18) | 55 | 21 (16 to 26) | 24 | 10 (6 to 14) | 35 | 14 (10 to 19) |
| Not given | 31 | 4 (3 to 6) | 7 | 3 (1 to 5) | 21 | 8 (5 to 12) | 3 | 1 (0 to 3) |
| Marital status | ||||||||
| Single/never married | 155 | 20 (17 to 23) | 62 | 23 (18 to 29) | 38 | 15 (11 to 20) | 55 | 22 (17 to 27) |
| Married | 508 | 66 (62 to 29) | 167 | 63 (57 to 69) | 157 | 62 (56 to 68) | 184 | 73 (67 to 78) |
| Separated/divorced | 33 | 4 (3 to 6) | 6 | 2 (1 to 5) | 22 | 9 (6 to 13) | 5 | 2 (1 to 5) |
| Widowed | 33 | 4 (3 to 6) | 14 | 5 (3 to 9) | 14 | 6 (3 to 9) | 5 | 2 (1 to 5) |
| Not given | 43 | 6 (4 to 7) | 17 | 6 (4 to 10) | 23 | 9 (6 to 13) | 3 | 1 (0 to 3) |
Participants were asked about their weekly consumption of vegetables, fruits, protein, sugar, salt and fried food. As shown in table 2, 65% and 58% of all participants reported the consumption of root and green vegetables, respectively, for at least 5 days of the week but this varied across sites (p<0.001). Residents of West Hiri reported the lowest percentage of root vegetable (17%) and greens (14%) consumption; however, they reported the highest percentage of fruit (24%) and animal protein (canned 52% and fresh 48%) consumption. The addition of at least 6 teaspoons of sugar in a hot drink daily was highest in both Asaro (20%) and West Hiri (20%) compared with Karkar Island (11%) (p<0.03). Fried food consumption also varied across the sites with Asaro participants (43%) recording the highest consumption of fried food at home, 5 or more days per week, relative to West Hiri (16%) and Karkar Island (0%) (p<0.001). The lowest salt consumption was reported by Karkar Island participants (22%) compared with those in West Hiri and Asaro.
Table 2.
Study participants’ self-reported food consumption in a typical week by iHDSS. Values are in numbers and percentages (95% CI)
| Food consumption | Overall n=772 |
West Hiri n=266 |
Asaro n=254 |
Karkar Island n=252 |
p Value* | ||||
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | ||
| Root vegetables >5 days/week† | 503 | 65 (62 to 69) | 46 | 17 (13 to 22) | 211 | 83 (78 to 88) | 245 | 98 (94 to 99) | <0.001 |
| Greens >5 days/week† | 451 | 58 (54 to 62) | 36 | 14 (10 to 18) | 168 | 66 (60 to 72) | 247 | 98 (95 to 99) | <0.001 |
| Fruits >5 days/week† | 97 | 13 (10 to 15) | 64 | 24 (19 to 30) | 33 | 13 (9 to 18) | 0 | 0 (0 to 1) | <0.001 |
| Fresh protein 5 days/week† | 216 | 28 (25 to 31) | 128 | 48 (42 to 54) | 4 | 2 (0.4 to 4) | 84 | 33 (28 to 40) | <0.001 |
| Canned protein 5 days/week† | 181 | 23 (21 to 27) | 138 | 52 (46 to 58) | 26 | 10 (7 to 15) | 17 | 7 (4 to 11) | <0.001 |
| Teaspoon sugar >6 tsp daily | 132 | 17 (15 to 20) | 53 | 20 (15 to 25) | 51 | 20 (15 to 26) | 28 | 11 (8 to 16) | 0.026 |
| Sugary drinks 3+ days/week‡ | 43 | 6 (4 to 7) | 34 | 13 (9 to 17) | 9 | 4 (2 to 7) | 0 | 0 (0 to 1) | <0.001 |
| Purchased fried food >5 days/week† | 18 | 2 (1 to 4) | 4 | 2 (0 to 4) | 14 | 6 (3 to 9) | 0 | 0 (0 to 1) | <0.001 |
| Home fried food >5 days/week† | 151 | 20 (17 to 23) | 41 | 16 (11 to 20) | 109 | 43 (37 to 49) | 1 | 0.4 (0 to 2) | <0.001 |
| Stock cube 7 days/week§ | 5 | 1 (0 to 2) | 2 | 1 (0.1 to 2.7) | 1 | 0 (0 to 2) | 2 | 1 (0 to 3) | 0.377 |
| Salt directly on food 7 days/week§ | 361 | 47 (43 to 50) | 162 | 61 (55 to 67) | 144 | 57 (50 to 63) | 55 | 22 (17 to 27) | <0.001 |
*p Values were obtained by Pearson’s χ2test and Fisher’s exact test where appropriate, †Consumed for at least 5 days in a typical week, ‡Consumption of soft drink for at least 3 days in a typical week, §Consumption for 7 days of the week.
iHDSS, integrated Health and Demographic Surveillance Sites.
Participants were asked if a health worker had previously diagnosed them with one or more of a range of specified NCDs. Overall, as shown in table 3, very few participants reported having received a diagnosis of any of the stated conditions and all diagnoses, except hypertension, chronic lung disease and cancer, were from West Hiri. Participants from Karkar and Asaro reported the least number of NCD diagnoses.
Table 3.
Study participants’ self-reported diagnoses of non-communicable diseases and risk factors by iHDSS. Values are numbers and percentages (95% CI)
| Diseases | Overall | West Hiri | Asaro | Karkar Island | p Value* | ||||||||
| N | n | % (95% CI) | N | n | % (95% CI) | N | n | % (95% CI) | N | n | % (95% CI) | ||
| Stroke | 769 | 3 | 0.4 (0 to 1) | 266 | 3 | 1 (0 to 3) | 253 | 0 | 0 (0 to 1) | 250 | 0 | 0 (0 to 1) | 0.111 |
| Heart disease | 767 | 4 | 1 (0 to 1) | 265 | 4 | 2 (0 to 4) | 252 | 0 | 0 (0 to 1) | 250 | 0 | 0 (0 to 1) | 0.037 |
| Diabetes mellitus T2 | 771 | 5 | 1 (0 to 2) | 266 | 5 | 2 (1 to 4) | 254 | 0 | 0 (0 to 1) | 251 | 0 | 0 (0 to 1) | 0.012 |
| Chronic lung disease/asthma | 772 | 16 | 2 (1 to 3) | 266 | 10 | 4 (2 to 7) | 254 | 4 | 2 (0 to 4) | 252 | 2 | 1 (0 to 3) | 0.065 |
| Hypercholesterolaemia | 769 | 1 | 0.1 (0 to 1) | 264 | 1 | 0.4 (0, 2.) | 254 | 0 | 0 (0 to 1) | 251 | 0 | 0 (0 to 1) | 1.00 |
| Hypertension | 767 | 26 | 3 (2 to 5) | 266 | 20 | 8 (5 to 11) | 250 | 5 | 2 (1 to 5) | 251 | 1 | 0.4 (0 to 2) | <0.001 |
| Cancer | 771 | 2 | 0.3 (0 to 1) | 266 | 1 | 0.4 (0 to 2) | 254 | 0 | 0 (0 to 1) | 251 | 1 | 0.4 (1 to 2) | 0.772 |
*p Value obtained by performing Fisher’s exact test.
iHDSS, integrated Health and Demographic Surveillance Sites.
Table 4 presents data on behavioural and clinical NCD risk factors. Tobacco smoking was common across all three sites but we found significant differences between the sites in the type of tobacco smoked. West Hiri participants only smoked manufactured tobacco, but Karkar Island and Asaro reported higher prevalence of smoking home-grown tobacco as compared with manufactured tobacco. Prevalence of betel nut use was also high across all three sites, although current alcohol consumption was comparatively lower, especially in Karkar Island (7%). Higher proportions of men than women smoked tobacco and drank alcohol. Overall, 32% of participants reported currently feeling stressed. The prevalence of stress was significantly higher in West Hiri and Asaro compared with Karkar Island (p<0.001). The prevalence of insufficient physical activity was highest in Karkar Island (34%) compared with Asaro (6%) and West Hiri (23%) (p<0.001). Overall, 19% and 11% of participants were categorised as overweight or obese, respectively. There was a statistically significant difference between the sites with higher prevalence of overweight (25%) and obesity (22%) in West Hiri compared with the other two sites (p<0.001). However, Asaro had a higher percentage (90%) of participants with central obesity, based on the waist-to-hip ratio, than the other two sites and this difference was statistically significant (p<0.001). There was also a statistically significant difference in the prevalence of hypertension between the sites, with Karkar Island participants having the lowest prevalence of hypertension (5%) compared with West Hiri (22%) and Asaro (22%) (p<0.001). Higher percentages of elevated cholesterol (24%) and HbA1c (34%) were observed among West Hiri participants compared with Asaro and Karkar.
Table 4.
Overall distribution of prevalence of major non-communicable disease risk factors by iHDSS. The values are numbers and percentages (95% CI) and means (SD)
| NCD risk factors | Overall | West Hiri | Asaro | Karkar Island | p Value* | ||||||||
| N | n | % (95% CI) | N | n | % (95% CI) | N | n | % (95% CI) | N | n | % (95% CI) | ||
| Daily tobacco smokers† | 526 | 253 | 48 (44 to 53) | 155 | 64 | 41 (34 to 50) | 171 | 85 | 50 (42 to 57) | 200 | 104 | 52 (45 to 59) | 0.170 |
| Male | 248 | 171 | 69 (63 to 75) | 71 | 47 | 66 (54 to 77) | 90 | 62 | 69 (58 to 78) | 87 | 62 | 71 (61 to 80) | 0.588 |
| Female | 278 | 82 | 29 (24 to 35) | 84 | 17 | 20 (12 to 30) | 81 | 23 | 28 (19 to 40) | 113 | 42 | 37 (28 to 47) | 0.035 |
| Types of tobacco smoked | 224 | 60 | 76 | 88 | |||||||||
| Manufactured filtered cigarette | 27 | 12 (8 to 17) | 21 | 35 (23 to 48) | 6 | 8 (3 to 17) | 0 | 0 (0 to 4) | <0.001 | ||||
| Unfiltered dark tobacco (spear/mutrus) | 42 | 19 (14 to 25) | 39 | 65 (52 to 77) | 2 | 3 (0 to 9) | 1 | 1 (0 to 6) | <0.001 | ||||
| Home-grown tobacco (brus) | 155 | 69 (58 to 70) | 0 | 0 (0 to 6) | 68 | 89 (80 to 95) | 87 | 99 (94 to 100) | <0.001 | ||||
| Current alcohol consumption‡ | 523 | 118 | 23 (19 to 26) | 152 | 66 | 43 (35 to 52) | 171 | 38 | 22 (16 to 29) | 200 | 14 | 7 (4 to 12) | 0.001 |
| Male | 248 | 96 | 39 (33 to 45) | 71 | 49 | 69 (57 to 79) | 90 | 33 | 37 (27 to 47) | 87 | 14 | 16 (9 to 26) | 0.002 |
| Female | 275 | 22 | 8 (5 to 12) | 81 | 17 | 21 (13 to 31) | 81 | 5 | 6 (2 to 14) | 113 | 0 | 0 (0 to 3) | 0.004 |
| Alcohol frequency past 12 months | 185 | 89 | 60 | 36 | |||||||||
| Daily | 5 | 3 (1 to 6) | 0 | 0 (0 to 4) | 5 | 8 (3 to 18) | 0 | 0 (0 to 10) | 0.023 | ||||
| 5–6 days/week | 7 | 4 (2 to 8) | 0 | 0 (0 to 4) | 7 | 12 (5 to 23) | 0 | 0 (0 to 10) | 0.004 | ||||
| 1–4 days/week | 12 | 6 (3 to 11) | 6 | 7 (3 to 14) | 5 | 8 (3 to 18) | 1 | 3 (0 to 15) | 0.513 | ||||
| 1–3 days/month | 58 | 31 (25 to 39) | 40 | 45 (34 to 56) | 12 | 20 (11 to 32) | 6 | 17 (6 to 33) | 0.004 | ||||
| Less than once a month | 103 | 55 (48 to 63) | 43 | 48 (38 to 59) | 31 | 52 (38 to 65) | 29 | 81 (64 to 92) | 0.016 | ||||
| Chewing betel nut§ | 520 | 386 | 74 (70 to 78) | 155 | 145 | 94 (89 to 97) | 168 | 93 | 55 (47 to 63) | 197 | 148 | 75 (68 to 81) | <0.001 |
| Male | 245 | 179 | 73 (67 to 79) | 71 | 64 | 90 (81 to 96) | 89 | 52 | 58 (47 to 69) | 85 | 63 | 74 (63 to 83) | <0.001 |
| Female | 275 | 207 | 75 (70 to 80) | 84 | 81 | 96 (90 to 99) | 79 | 41 | 52 (40 to 63) | 112 | 85 | 76 (67 to 83) | <0.001 |
| Betel nut with betel bean and slaked lime | 386 | 357 | 92 (89 to 95) | 145 | 128 | 88 (82 to 93) | 93 | 84 | 90 (83 to 96) | 148 | 145 | 98 (94 to 100) | 0.012 |
| Stress | 771 | 246 | 32 (29 to 35) | 266 | 122 | 46 (40 to 52) | 254 | 112 | 44 (38 to 50) | 252 | 12 | 5 (2 to 8) | <0.001 |
| Male | 360 | 115 | 33 (28 to 38) | 114 | 49 | 43 (34 to 53) | 130 | 61 | 47 (38 to 56) | 117 | 5 | 4 (1 to 10) | <0.001 |
| Female | 411 | 131 | 31 (26 to 35) | 152 | 73 | 48 (40 to 56) | 124 | 51 | 41 (32 to 50) | 135 | 7 | 5 (2 to 10) | <0.001 |
| Insufficient physical activity¶ | 504 | 101 | 20 (17 to 24) | 169 | 39 | 23 (17 to 30) | 186 | 12 | 6 (4 to 11) | 149 | 50 | 34 (26 to 42) | <0.001 |
| Male | 233 | 37 | 16 (11 to 21) | 76 | 14 | 18 (10 to 29) | 94 | 5 | 5 (2 to 12) | 63 | 18 | 29 (18 to 41) | <0.001 |
| Female | 271 | 64 | 24 (19 to 29) | 93 | 25 | 27 (18 to 37) | 92 | 7 | 8 (3 to 15) | 86 | 32 | 37 (27 to 48) | <0.001 |
| Mean (SD) BMI (kg/m2) | 767 | 23.9±5.7 | 264 | 26±7.1 | 252 | 24.0±4.4 | 251 | 21.5±4.0 | <0.001 | ||||
| Overweight (BMI ≥25–29.9 kg/m2) | 767 | 144 | 19 (16 to 22) | 264 | 65 | 25 (20 to 30) | 252 | 59 | 23 (18 to 29) | 251 | 20 | 8 (5 to 12) | <0.001 |
| Male | 356 | 67 | 19 (15 to 23) | 112 | 32 | 29 (20 to 38) | 128 | 29 | 23 (16 to 31) | 116 | 6 | 5 (2 to 11) | <0.001 |
| Female | 411 | 77 | 19 (15 to 23) | 152 | 33 | 22 (15 to 29) | 124 | 30 | 24 (17 to 33) | 135 | 14 | 10 (6 to 17) | 0.009 |
| Obesity (BMI ≥30 kg/m2) | 767 | 82 | 11 (9 to 13) | 264 | 59 | 22 (18 to 28) | 252 | 16 | 6 (4 to 10) | 251 | 7 | 3 (1 to 6) | <0.001 |
| Male | 356 | 20 | 6 (3 to 9) | 112 | 15 | 13 (8 to 21) | 128 | 3 | 2 (0.5 to 7) | 116 | 2 | 2 (0.2 to 6) | <0.001 |
| Female | 411 | 62 | 15 (12 to 19) | 152 | 44 | 29 (22 to 37) | 124 | 13 | 10 (6 to 17) | 135 | 5 | 4 (1 to 8) | <0.001 |
| Mean (SD) WHR | 758 | 0.91±0.09 | 264 | 0.88±0.12 | 250 | 0.94±0.08 | 244 | 0.90±0.06 | <0.001 | ||||
| Central obesity (WHR, M≥0.9/F≥0.85) | 758 | 514 | 68 (64 to 71) | 264 | 138 | 52 (46 to 58) | 250 | 225 | 90 (86 to 93) | 244 | 151 | 62 (56 to 68) | <0.001 |
| Male | 351 | 218 | 62 (57 to 67) | 112 | 50 | 45 (35 to 54) | 128 | 125 | 98 (93 to 100) | 111 | 43 | 39 (30 to 48) | <0.001 |
| Female | 407 | 296 | 73 (68 to 77) | 152 | 88 | 58 (50 to 66) | 122 | 100 | 82 (74 to 88) | 133 | 108 | 81 (74 to 87) | <0.001 |
| Mean (SD) SBP (mm Hg) | 738 | 123±17.5 | 264 | 125.7±19.8 | 222 | 126.7±16.8 | 252 | 116.8±13.3 | <0.001 | ||||
| Mean (SD) DBP (mm Hg) | 738 | 75.3±10.9 | 264 | 77±12.4 | 222 | 78.4±9.7 | 252 | 70.7±8.5 | <0.001 | ||||
| Prehypertension** | 738 | 339 | 46 (42 to 50) | 264 | 120 | 46 (39 to 52) | 222 | 123 | 55 (42 to 62) | 252 | 96 | 38 (32 to 44) | 0.001 |
| Male | 344 | 189 | 55 (50 to 60) | 112 | 65 | 58 (48 to 67) | 115 | 67 | 58 (49 to 67) | 117 | 57 | 49 (39 to 58) | 0.25 |
| Female | 394 | 150 | 38 (33 to 43) | 152 | 55 | 36 (29 to 44) | 107 | 56 | 52 (42 to 62) | 135 | 39 | 29 (21 to 37) | 0.001 |
| Hypertension (≥140/90 mm Hg) | 738 | 118 | 16 (13 to 19) | 264 | 58 | 22 (17 to 28) | 222 | 48 | 22 (16 to 28) | 252 | 12 | 5 (3 to 8) | <0.001 |
| Male | 344 | 65 | 19 (15 to 23) | 112 | 32 | 29 (20 to 38) | 115 | 28 | 24 (17 to 33) | 117 | 5 | 4 (1 to 10) | <0.001 |
| Female | 394 | 53 | 13 (10 to 17) | 152 | 26 | 17 (14 to 24) | 107 | 20 | 19 (12 to 27) | 135 | 7 | 5 (2 to 10) | <0.001 |
| Mean (SD) cholesterol (mmol/L) | 708 | 4.6±1.8 | 258 | 5.0±1.8 | 218 | 4.7±1.7 | 232 | 4.2±1.7 | <0.001 | ||||
| Elevated cholesterol (>6.2 mmol/L) | 708 | 123 | 17 (15 to 20) | 258 | 61 | 24 (19 to 29) | 218 | 35 | 16 (11 to 22) | 232 | 27 | 12 (8 to 17) | 0.002 |
| Male | 321 | 50 | 16 (12 to 20) | 108 | 22 | 20 (13 to 29) | 108 | 18 | 17 (10 to 25) | 105 | 10 | 10 (5 to 17) | 0.086 |
| Female | 387 | 73 | 19 (15 to 23) | 150 | 39 | 26 (19 to 34) | 110 | 17 | 15 (9 to 24) | 127 | 17 | 13 (8 to 21) | 0.016 |
| Mean (SD) HDL-C (mmol/L) | 709 | 1.2±0.6 | 258 | 1.3±0.5 | 218 | 1.1±0.5 | 233 | 1.0±0.6 | <0.001 | ||||
| Low HDL-C†† | 709 | 388 | 55 (51 to 58) | 258 | 116 | 45 (39 to 51) | 218 | 127 | 58 (51 to 65) | 233 | 145 | 62 (56 to 68) | <0.001 |
| Male | 322 | 142 | 44 (39 to 50) | 108 | 33 | 31 (22 to 40) | 108 | 49 | 45 (36 to 55) | 106 | 60 | 57 (47 to 66) | 0.001 |
| Female | 387 | 246 | 64 (59 to 68) | 150 | 83 | 55 (47 to 63) | 110 | 78 | 71 (61 to 79) | 127 | 85 | 67 (58 to 75) | 0.023 |
| Mean (SD) HbA1c | 712 | 5.4±0.8 | 253 | 5.7±1.2 | 220 | 5.3±0.3 | 239 | 5.2±0.4 | <0.001 | ||||
| Prediabetes HbA1c (≥5.7%–6.4%) | 712 | 107 | 15 (13 to 18) | 253 | 65 | 26 (20 to 32) | 220 | 25 | 11 (8 to 16) | 239 | 17 | 7 (4 to 11) | <0.001 |
| Male | 323 | 41 | 13 (9 to 17) | 107 | 20 | 19 (12 to 27) | 109 | 13 | 12 (7 to 20) | 107 | 8 | 7 (3 to 14) | 0.052 |
| Female | 386 | 66 | 17 (13 to 21) | 146 | 45 | 31 (23 to 39) | 111 | 12 | 11 (6 to 18) | 132 | 9 | 7 (3 to 13) | <0.001 |
| DMT2 HbA1c (≥6.5%) | 712 | 24 | 3 (2 to 5) | 253 | 22 | 9 (6 to 13) | 220 | 0 | 0 (0 to 2) | 239 | 2 | 1 (0 to 3) | <0.001 |
| Male | 323 | 8 | 2 (1 to 5) | 107 | 8 | 7 (3 to 14) | 109 | 0 | 0 (0 to 3) | 107 | 0 | 0 (0 to 3) | <0.001 |
| Female | 386 | 16 | 4 (2 to 7) | 146 | 14 | 10 (5 to 16) | 111 | 0 | 0 (0 to 3) | 132 | 2 | 2 (0.2 to 5) | <0.001 |
*p Values were obtained by Pearson’s χ2 test and Fisher’s exact test where appropriate for categorical variables and one-way ANOVA for continuous variables, †Current tobacco smoking on a daily basis, ‡Consumption of alcohol within last 30 days.
§Chewed betel nut within last 30 days, ¶Vigorous physical activity <75 min and moderate physical activity <150 min/week, **Prehypertension=SBP>120–139.9 mm Hg and/or DBP 80–89 mm Hg, ††Low HDL-C=<1 mmol/L men and ≤1.3 mmol/L women.
ANOVA, analysis of variance; BMI, body mass index; DBP, diastolic blood pressure; DMT2, diabetes mellitus type 2; HbA1c, haemoglobin A1c; HDL-C, high-density lipoprotein-cholesterol; iHDSS, integrated Health and Demographic Surveillance Sites; NCD, non-communicable disease; SBP, systolic blood pressure; WHR, waist-to-hip ratio.
Discussion
The results from our study provide baseline prevalence of NCD risk factors in three sites in PNG. Combined with earlier data from Asaro and Karkar sites, there is evidence of an increase in some key NCD risk factors; however, there is substantial variation among the three communities due to demographic and socioeconomic differences. The NCD risk appears greatest in the periurban site of West Hiri, relative to the rural sites of Asaro and Karkar Island. Similar rural-urban differences have been seen in other PI nations such as Fiji and Western Samoa.52 53 Previous studies found non-Austronesian populations to be less susceptible to developing diabetes and other NCDs.34 54 The Asaro population of non-Austronesian origin, however, recorded the highest central obesity and prehypertension prevalence, indicating a rural population at very high risk of developing CVDs. West Hiri, an Austronesian population, as expected, had a higher prevalence of CVD and DMT2 risk factors. Karkar Island, a mixed Austronesian and non-Austronesian population, had low prevalence of some risk factors such as overweight and obesity, hypertension and elevated HbA1c levels. It also recorded the highest prevalence of tobacco smoking, insufficient physical activity and low HDL-C levels, indicating an increased risk for developing NCDs.
This is the first NCD study in West Hiri and having a diet low in vegetables compared with Asaro and Karkar Island reflects limited subsistence farming. However, more participants are in paid employment with regular income, which may explain the comparatively high alcohol and cigarette use and a diet high in sugar, salt and animal protein. Its close proximity to Port Moresby has resulted in a longer exposure to modernisation and the consequent increased risk of developing DMT2 and other NCDs.9 32 52 This study provides evidence of an existing high prevalence of NCD risk factors in the West Hiri population. The NCD risk factor burden is expected to increase further, especially with the socioeconomic transition occurring in this population, which may be accelerated due to its Austronesian ancestry and close proximity to PNG’s fastest growing city, and through the steep increase in local disposable incomes (via salaries, wages and royalty payments from the gas project).
The prevalence of daily tobacco smoking in our study (41%) is far higher than the 26.3% prevalence reported in the 2009/2010 national Household Income and Expenditure Survey (HIES),55 yet consistent with the 43.7% and 47.7% in the 2007/2008 PNG STEPS and Global Youth Tobacco Survey, respectively.36 56 Our findings confirm that tobacco smoking rates have been high for a long period. There are even higher prevalences of current tobacco smokers in other Pacific countries, some of which were very high as in Kiribati, Wallis and Futuna, Tokelau and Fiji.57 As tobacco smoking increases the risk of developing CVDs and other NCDs,58 59 our findings suggest public health efforts are needed to identify appropriate measures to reduce the consumption of both manufactured and home-grown tobacco. Increasing tobacco tax has reduced consumption of manufactured tobacco elsewhere,60 but may not be effective in populations where home-grown tobacco is widely used. Accordingly, in addition to WHO’s ‘Best Buy’ interventions,61 public awareness campaigns highlighting the harmful effects of smoking, inclusive of home-grown tobacco, are required throughout PNG.
The prevalence of betel nut chewing was highest in the two coastal communities, where it is grown, compared with the highlands community of Asaro, and this is similar to a 1968 study which showed very high prevalence of betel nut chewing in two coastal communities, compared with a highlands community whose betel nut use was far lower.62 The overall prevalence of betel nut chewing is higher than the 2009/2010 national HIES,55 but supports the 2007/2008 STEPS36 prevalence. Even reported prevalences from other countries as Taiwan and Malaysian Borneo were lower than the findings from our study.63 Chewing of betel nut has been associated with oral cancer, elevated glucose and increased risk of CVDs.64–67 It is deeply embedded into PNG’s social and cultural traditions and is prevalent across the country,36 55 62 even among pregnant women.68 Therefore, it will be important to monitor the impacts of this habit and provide appropriate public health messages combined with stronger and sustainable measures to reduce its use. A betel nut ban has recently been implemented in Port Moresby69 and a robust evaluation should be conducted in order to establish the public health benefit, if any, from this intervention.
Our study found a higher prevalence of current alcohol use among the periurban West Hiri (43%) relative to rural Asaro (22%) and Karkar (7%) and this may be due to the high employment rate and increased availability of cash among the West Hiri population. A similar pattern reported in 1977 saw an increased alcohol use among men with high social status in the two communities of Karkar Island and Lufa.70 However, our results showed a similar ‘binge drinking’ pattern (low frequency, high volume consumption) across all sites which was a common finding among Pacific youths in New Zealand.71 The national HIES (9%) and STEPS (15%) survey reported lower prevalence of alcohol consumption than our findings. Studies from neighbouring PI nations, however, recorded much higher alcohol consumption rates.57 This binge drinking pattern in PNG previously reported to contribute to law and order problems affecting one’s health, work and family.72 As such, adoption of appropriate measures such as WHO’s ‘best buys’61 is needed to control excessive alcohol consumption in the country which may include increased tax in the manufacture and sale of alcohol, ban on alcohol advertisement and awareness through education.
The findings from our study reveal that one in every three participants reported stress. However, there were significant differences across the sites, where Karkar participants reported the least percentage of stress relative to West Hiri and Asaro. Karkar participants live on an island further away from the nearest town compared with West Hiri and Asaro who are closer to towns, relying more on cash economy for the purchase of goods and services. A recent study identified two major sources of stress among PNG women: one is economic and supply instability and the other is stress associated with relationships with others.73 Changes associated with urbanisation are likely to affect both. Further studies are needed to investigate the degree of stress as well as identify the stress vulnerable groups faced in PNG.
Our study found a higher prevalence of physical inactivity in both Karkar Island and West Hiri, compared with Asaro. The overall prevalence of insufficient physical activity is higher than that reported in the STEPS survey. PNG has one of the lowest prevalences of physical inactivity in the Pacific region where rates greater than 50% in both women and men have been reported.57 Culturally appropriate interventions are needed to promote sufficient physical activity across PNG to help reduce the risk of developing NCDs. With towns and urban areas becoming unsafe for walking or jogging, most people commute only by vehicle,74 pointing to a need for urban planners to incorporate safety plans to enable the use of public space for leisure activities.
Our results showed a higher prevalence of overweight and obesity in periurban West Hiri relative to rural Asaro and Karkar Island. Norgan in 1995 reported overweight and obesity prevalence in Karkar and Lufa communities was less than 10%,75 which is lower than our findings. In addition, the overall obesity prevalence (11%) in our study is higher than that reported in the PNG STEPS survey.36 Although the West Hiri obesity rates (22%) are comparable to that reported for Port Moresby residents (21%), it is lower than that in some neighbouring Pacific Islands.35 57 Despite the low prevalence of obesity, especially in Asaro and Karkar Island, our results showed very high prevalence of central obesity (waist-to-hip ratio) across all sites, but more so in Asaro. Central obesity, based on waist-to-hip ratio, has been reported to substantially increase the risk of CVDs and is a preferred measure of obesity for predicting CVD and all-cause deaths.76 77 The high prevalence of central obesity in Asaro indicates a different propensity for fat distribution to West Hiri. This finding further indicates the standard BMI thresholds may not be suitable for use in PNG, as has also been suggested for other ethnic groups in the Asia Pacific region.46 Some countries have introduced taxes on unhealthy food and beverages to reduce their consumption.78 Health promotion via media, education in schools and workplaces as that in New Zealand79 may also help reduce overweight and obesity prevalence. PNG may need to consider adopting such initiatives to help reduce and control the availability and sales of high sugar, salt and fat content foods in the country.
Other CVD risk factors, such as elevated BP and hyperlipidaemia, were higher across the three sites in our study compared with the earlier PNG STEPS survey. High rates of prehypertension (55%) in the Asaro population are concerning as studies conducted between the 1950s and 1980s in the highlands population showed low levels of elevated BP.80–82 According to previous studies in Asaro, the prevalence of hypertension was14 83 lower than our findings (22%). Similarly, in the 1960s–1980s hypertension was absent or very low in Karkar as elsewhere in the country.14 84–86 However, our results showed increased prevalence of both prehypertension (38%) and hypertension (5%) among the Karkar population. Over the last two decades, hypertension has been recorded at very high levels in other parts of the country, such as the Purari Delta, Manus and urban Port Moresby.13 29
Inter-regional differences in NCD risks have been previously observed for hypercholesterolaemia. Some parts of the country inclusive of Asaro and rural Central Province recorded zero or low prevalence of hypercholesterolaemia from the late 1980s to early 1990s,17 87 88 yet very high in certain populations such as urban Port Moresby and group of male miners in Bougainville.17 23 89 The prevalence of hypercholesterolaemia (24%) in our periurban West Hiri population was slightly lower than that of urban Port Moresby, although a lower cut-off (≥5.2 mmol/L) was used in the latter study. Our results combined with these previous studies suggest an urgent need for interventions to control CVD risk factors across all populations of PNG. In addition to WHO’s ‘best buys,’61 and a country appropriate adaptation of the Green Prescription,90 enabling health education programmes to promote activity and healthy lifestyle in schools and communities would be beneficial for PNG.
Previous studies have reported a variable prevalence of DMT2 in parts of PNG. According to studies conducted in the 1980s–1990s, DMT2 was absent or existed at very low prevalence in many parts of PNG including Karkar Island and Asaro communities.33 34 54 DMT2 prevalences in these communities have remained low over a long period of time and our findings are consistent with the earlier studies; however, prediabetes data from our study may suggest this is changing. Indeed, studies conducted in Koki, in urban Port Moresby, Wanigela village in Central Province and residents of Port Moresby between the 1970s and 2000 reported very high prevalences of DMT2.16 18 31 32 Based on genetics and longer exposure to modernisation, it is not surprising that West Hiri population had a higher prevalence of both prediabetes (26%) and DMT2 (9%) than Asaro and Karkar. Together with previous studies, our findings indicate limited change in DMT2 in recent history but continued marked disparity between populations, although the percentage of adults with elevated HbA1c across sites should be of significant concern. Control measures should include restrictions on imported high-sugar and fat content foods as well as the use of mass media and other education and public awareness raising activities.
Strengths and limitations
The study had a number of strengths and limitations. Strengths include an up-to-date prevalence of NCD risk factors in three sites at different stages of social and economic development; and the collection of NCD risk factor data during the early stages of a huge gas development project which provides a baseline for future longitudinal studies to monitor NCDs and risk factors. The limitations are as follows: First, this was a cross-sectional study and provides a snapshot of the risk and disease burden at a particular moment in time. Second, the study was conducted in only three locations across PNG and is therefore not nationally representative. Third, the full sample size was not achieved and younger people were undersampled, which could have led to an overestimation of NCD risk factor burden. Fourth, the study relied on the participants’ self-report for some measures, possibly resulting in recall bias (eg, self-reported 7-day food consumption). Fifth, biological samples were not collected from all participants therefore interpretation of results was limited only to those with biological samples.
Conclusion
Although not nationally representative, our study is suggestive of a socioeconomic and nutrition transition being under way in all three sites, especially in periurban West Hiri, which had a higher NCD risk factor burden compared with the rural sites. However, some risk factors were common across sites, suggesting these populations are at heightened risk of developing CVDs. Few participants had received an NCD diagnosis despite the high prevalence of NCD risk factors, suggesting that current NCD screening and prevention as well as treatment services are inadequate in the sites taking part in this study. Training on NCDs and their risk factors as well as appropriate lifestyle interventions need to be incorporated into existing health training curriculum. Such training would facilitate appropriate screening, monitoring and control of NCDs at the primary healthcare setting. In addition, facilities need to be provided with the basic equipment/tools for screening. This calls for an urgent need to mobilise appropriate and multisectoral preventive interventions and upskill health services. Regular monitoring of these populations would provide up-to-date information and feedback on the effectiveness of any interventions for the emerging NCD epidemic in PNG.
Acknowledgments
The authors wish to thank all research participants, Provincial Government, church health authorities and community representatives in the respective sites. The authors are grateful to the dedicated NCD Study field and laboratory staff members. The authors also acknowledge the PNGIMR for providing the administrative and technical support to conduct this study. Lastly, we acknowledge the financial support via an unrestricted grant provided by PNG ExxonMobil to conduct this survey in the three sites. The governance and management of the study was completely independent from the funders.
Footnotes
Contributors: RS, CB, IR, GM, AM, MU, IHK, JP, GV, HG, SP and PR were responsible for study design. PR, JP, GV, HG and SP helped conduct the study and were responsible for data collection. PR conducted the data analysis and was responsible for drafting the manuscript. JP, RS, CB, AM, MU, HG, BO and BM critically revised the manuscript. The final draft was approved by all authors.
Competing interests: None declared.
Patient consent: All study participants signed a consent form prior to being recruited into the study.
Ethics approval: PNG Institute of Medical Research Institutional Review Board and PNG Medical Research Advisory Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Requests for data access should be directed to the corresponding author and will be granted subject to approval by the Medical Research Advisory Council of Papua New Guinea.
References
- 1. WHO, Global status report on noncommunicable diseases 2010. Geneva, Switzerland: World Health Organization, 2011:176. [Google Scholar]
- 2. WHO. Global status report on noncommunicable disease 2014. Geneva, Switzerland: WHO, 2014:298. [Google Scholar]
- 3. Collaborators GMaC. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease study 2013. Lancet 2015;385:117–71. 10.1016/S0140-6736(14)61682-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Statistical Office PNG. Final Figures. Papua New Guinea. National Population and Housing Census 2011. Port Moresby: National Statistical Office, 2013. [Google Scholar]
- 5. National Statistical Office PnG. Papua New Guinea Demographic and Health Survey 2006. Port Moresby: National Statistical Office, 2009. [Google Scholar]
- 6. Group WB. Data. World Bank Country and Lending Groups 2015. http://data.worldbank.org/about/country-and-lending-groups (cited Nov 2015).
- 7. Tasman A. PNG LNG Economic Impact Study. An assessment of the direct and indirect impacts of the proposed PNG LNG project on the economy of Papua New Guinean. 2009.
- 8. Amuna P, Zotor FB. Epidemiological and nutrition transition in developing countries: impact on human health and development. Proc Nutr Soc 2008;67:82–90. 10.1017/S0029665108006058 [DOI] [PubMed] [Google Scholar]
- 9. Zimmet P, Globalization ZP. Globalization, coca-colonization and the chronic disease epidemic: can the Doomsday scenario be averted? J Intern Med 2000;247:301–10. 10.1046/j.1365-2796.2000.00625.x [DOI] [PubMed] [Google Scholar]
- 10. WHO. Papua New Guinea: WHO Statistical Profile. Papua New Guinea: WHO, 2015. [Google Scholar]
- 11. Vines AP. An epidemiological sample survey of the highlands, mainland and islands regions of the Territory of Papua and New Guinea. An epidemiological sample survey of the highlands, mainland and islands regions of the Territory of Papua and New Guinea. 1970.
- 12. King H, Collins AM. A modernity score for individuals in Melanesian society. P N G Med J 1989;32:11–22. [PubMed] [Google Scholar]
- 13. Ulijaszek SJ. Hypertension among adults of the Purari delta of the Gulf Province, Papua New Guinea. P N G Med J 1998;41:65–71. [PubMed] [Google Scholar]
- 14. King H, Collins V, King LF, et al. Blood pressure, hypertension and other cardiovascular risk factors in six communities in Papua New Guinea, 1985-1986. P N G Med J 1994;37:100–9. [PubMed] [Google Scholar]
- 15. Schall JI. Sex differences in the response of blood pressure to modernization. American Journal of Human Biology 1995;7:159–72. 10.1002/ajhb.1310070204 [DOI] [PubMed] [Google Scholar]
- 16. Dowse GK, Spark RA, Mavo B, et al. Extraordinary prevalence of non-insulin-dependent diabetes mellitus and bimodal plasma glucose distribution in the Wanigela people of Papua New Guinea. Med J Aust 1994;160:767–74. [DOI] [PubMed] [Google Scholar]
- 17. Hodge AM, Dowse GK, Erasmus RT, et al. Serum lipids and modernization in coastal and highland Papua New Guinea. Am J Epidemiol 1996;144:1129–42. 10.1093/oxfordjournals.aje.a008891 [DOI] [PubMed] [Google Scholar]
- 18. Benjamin AL. Community screening for diabetes in the National Capital District, Papua New Guinea: is betelnut chewing a risk factor for diabetes? P N G Med J 2001;44:101–7. [PubMed] [Google Scholar]
- 19. Kende M. Superiority of traditional village diet and lifestyle in minimizing cardiovascular disease risk in Papua New Guineans. P N G Med J 2001;44:135–50. [PubMed] [Google Scholar]
- 20. Saweri W. The rocky road from roots to rice: a review of the changing food and nutrition situation in Papua New Guinea. P N G Med J 2001;44:151–63. [PubMed] [Google Scholar]
- 21. Yamauchi T, Umezaki M, Ohtsuka R. Influence of urbanisation on physical activity and dietary changes in Huli-speaking population: a comparative study of village dwellers and migrants in urban settlements. Br J Nutr 2001;85:65–73. 10.1079/BJN2000208 [DOI] [PubMed] [Google Scholar]
- 22. Ulijaszek SJ. Socio-economic factors associated with physique of adults of the Purari delta of the Gulf Province, Papua New Guinea. Ann Hum Biol 2003;30:316–28. 10.1080/0301446031000086004 [DOI] [PubMed] [Google Scholar]
- 23. Iser DJ, Avera K. Has westernization influenced serum cholesterol levels in Bougainvillian males? P N G Med J 1993;36:311–5. [PubMed] [Google Scholar]
- 24. H X. Stagnant stunting rate despite rapid economic growth in Papua New Guinea-factors correlated with malnutrition among children under five. 2015.
- 25. King SE, Nicholas Mascie-Taylor CG. Nutritional status of children from Papua New Guinea: associations with socioeconomic factors. Am J Hum Biol 2002;14:659–68. 10.1002/ajhb.10080 [DOI] [PubMed] [Google Scholar]
- 26. Gibson J. Nutritional status of Papua New Guinea's population and its determinants. Papua New Guinea Food and Nutrition 2000 Conference, PNG University of Technology;2000; [Google Scholar]
- 27. DeBoer MD, Lima AA, Oría RB, et al. Early childhood growth failure and the developmental origins of adult disease: do enteric infections and malnutrition increase risk for the metabolic syndrome? Nutr Rev 2012;70:642–53. 10.1111/j.1753-4887.2012.00543.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Health PNGNDo. Health sector review 2001-2009 Report. Port Moresby: PNG National Department of Health, 2009. [Google Scholar]
- 29. Benjamin A. Community screening for high blood pressure among adults in urban and rural Papua New Guinea. PNG Med J 2006;49:137–46. [PubMed] [Google Scholar]
- 30. Kevau IH. Clinical documentation of twenty cases of acute myocardial infarction in Papua New Guineans. P N G Med J 1990;33:275–80. [PubMed] [Google Scholar]
- 31. Patel M, Jamrozik K, Allen O, et al. A high prevalence of diabetes in a rural village in Papua New Guinea. Diabetes Res Clin Pract 1986;2:97–103. 10.1016/S0168-8227(86)80066-3 [DOI] [PubMed] [Google Scholar]
- 32. Martin FI, Wyatt GB, Griew AR, et al. Diabetes mellitus in urban and rural communities in Papua New Guinea. Studies of prevalence and plasma insulin. Diabetologia 1980;18:369–74. [DOI] [PubMed] [Google Scholar]
- 33. King H, Finch C, Koki G, et al. Glucose tolerance in Papua New Guinea: comparison of Austronesian and non-Austronesian communities of Karkar Island. Diabet Med 1991;8:481–8. 10.1111/j.1464-5491.1991.tb01636.x [DOI] [PubMed] [Google Scholar]
- 34. King H, Finch C, Collins A, et al. Glucose tolerance in Papua New Guinea: ethnic differences, association with environmental and behavioural factors and the possible emergence of glucose intolerance in a highland community. Med J Aust 1989;151:204–10. [DOI] [PubMed] [Google Scholar]
- 35. Benjamin AL. Body size of Papua New Guineans: a comparison of the body mass index of adults in selected urban and rural areas of Papua New Guinea. P N G Med J 2007;50:163–71. [PubMed] [Google Scholar]
- 36. National Department of Health P, HOPE Worldwide P, WHO. Papua New Guinea NCD Risk Factor STEPS Report. Port Moresby: National Department of Health, 2014. [Google Scholar]
- 37. Gouda H, Vengiau G, Phuanukoonnon S, et al. Report of Partnership in Health Project (PiHP) 2011-2012. Report. PNG Institute of Medical Research, 2013. [Google Scholar]
- 38. Pham B, Maraga S, Kumai J, et al. PNGIMR PiH progress report: Reporting period January - June 2015. PNG Institute of Medical Research, 2015. [Google Scholar]
- 39. WHO. STEPwise approach to noncommunicable disease risk factor surveillance (STEPS). http://www.who.int/chp/steps/instrument/en/. [DOI] [PMC free article] [PubMed]
- 40. Wurm SA. Linguistic prehistory in the New Guinea area. J Hum Evol 1983;12:25–35. 10.1016/S0047-2484(83)80011-6 [DOI] [Google Scholar]
- 41. Dutton TE. The Hiri in History: Further aspects of long distance Motu trade in Central Papua. Australian National University, 1982. [Google Scholar]
- 42. Benediktsson K. Harvesting development: The construction of fresh food markets in Papua New Guinea. Denmark: NIAS Press, 2002. [Google Scholar]
- 43. Boyce AJ, Harrison GA, Platt CM, et al. Migration and Genetic Diversity in an Island Population: Karkar, Papua New Guinea. Proceedings of the Royal Society B: Biological Sciences 1978;202:269–95. 10.1098/rspb.1978.0067 [DOI] [Google Scholar]
- 44. Kambuou R. Papua New Guinea: Country Report to the FAO International Technical Conference on Plant Genetic Resources. Country Report. Konedobu 1995. [Google Scholar]
- 45. WHO. Global recommendations on physical activity for health. Geneva, Swtizerland: World Health Organization, 2010. [PubMed] [Google Scholar]
- 46. Committee S. The Asia-Pacific perspective: Redefining obesity and its treatment. Australia Health Communications Australia 2000. [Google Scholar]
- 47. Expert Consultation W. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation 2008, Report. Geneva, Switzerland: WHO, 2011. [Google Scholar]
- 48. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–52. 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- 49. Panel NE. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002;106:3143. [PubMed] [Google Scholar]
- 50. Lauer MS, Fontanarosa PB. Updated guidelines for cholesterol management. JAMA 2001;285:2508–9. 10.1001/jama.285.19.2508 [DOI] [PubMed] [Google Scholar]
- 51. American Diabetes Association. Standards of medical care in diabetes--2010. Diabetes Care 2010;33(Supplement 1):S11–61. 10.2337/dc10-S011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Zimmet P, Taylor R, Ram P, et al. Prevalence of diabetes and impaired glucose tolerance in the biracial (Melanesian and Indian) population of Fiji: a rural-urban comparison. Am J Epidemiol 1983;118:673–88. 10.1093/oxfordjournals.aje.a113678 [DOI] [PubMed] [Google Scholar]
- 53. Zimmet P, Faaiuso S, Ainuu J, et al. The prevalence of diabetes in the rural and urban Polynesian population of Western Samoa. Diabetes 1981;30:45–51. 10.2337/diab.30.1.45 [DOI] [PubMed] [Google Scholar]
- 54. King H, Heywood P, Zimmet P, et al. Glucose tolerance in a highland population in Papua New Guinea. Diabetes Res 1984;1:45–51. [PubMed] [Google Scholar]
- 55. National Statistical Office P. 2009-2010 Papua New Guinea Household Income and Expenditure Survey. PNG National Statistical Office, 2013. [Google Scholar]
- 56. Centers for Disease Control and Prevention. Population Survey - Global Youth Tobacco Survey (GYTS), 2007. [Google Scholar]
- 57. Kessaram T, McKenzie J, Girin N, et al. Noncommunicable diseases and risk factors in adult populations of several Pacific Islands: results from the WHO STEPwise approach to surveillance. Aust N Z J Public Health 2015;39:336–43. 10.1111/1753-6405.12398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Woodward M, Lam TH, Barzi F, et al. Smoking, quitting, and the risk of cardiovascular disease among women and men in the Asia-Pacific region. Int J Epidemiol 2005;34:1036–45. 10.1093/ije/dyi104 [DOI] [PubMed] [Google Scholar]
- 59. Martiniuk AL, Lee CM, Lam TH, et al. The fraction of ischaemic heart disease and stroke attributable to smoking in the WHO Western Pacific and South-East Asian regions. Tob Control 2006;15:181–8. 10.1136/tc.2005.013284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Abascal W, Esteves E, Goja B, et al. Tobacco control campaign in Uruguay: a population-based trend analysis. Lancet 2012;380:1575–82. 10.1016/S0140-6736(12)60826-5 [DOI] [PubMed] [Google Scholar]
- 61. World Health Organization. From burden to "best busy": Reducing the economic impact of NCDs in low-and middle-income countries. Executive summary 2011. Geneva: WHO, 2011. [Google Scholar]
- 62. Pindborg JJ, Barmes D, Roed-Petersen B. Epidemiology and histology of oral leukoplakia and leukoedema among Papuans and New Guineans. Cancer 1968;22:379–84. [DOI] [PubMed] [Google Scholar]
- 63. Gupta PC, Warnakulasuriya S. Global epidemiology of areca nut usage. Addict Biol 2002;7:77–83. 10.1080/13556210020091437 [DOI] [PubMed] [Google Scholar]
- 64. Javed F, Bello Correra FO, Chotai M, et al. Systemic conditions associated with areca nut usage: a literature review. Scand J Public Health 2010;38:838–44. 10.1177/1403494810379291 [DOI] [PubMed] [Google Scholar]
- 65. Thomas SJ, Bain CJ, Battistutta D, et al. Betel quid not containing tobacco and oral cancer: a report on a case-control study in Papua New Guinea and a meta-analysis of current evidence. Int J Cancer 2007;120:1318–23. 10.1002/ijc.22304 [DOI] [PubMed] [Google Scholar]
- 66. Tung TH, Chiu YH, Chen LS, et al. A population-based study of the association between areca nut chewing and type 2 diabetes mellitus in men (Keelung Community-based Integrated Screening programme No. 2). Diabetologia 2004;47:1776–81. 10.1007/s00125-004-1532-2 [DOI] [PubMed] [Google Scholar]
- 67. Lin WY, Chiu TY, Lee LT, et al. Betel nut chewing is associated with increased risk of cardiovascular disease and all-cause mortality in Taiwanese men. Am J Clin Nutr 2008;87:1204–11. [DOI] [PubMed] [Google Scholar]
- 68. Ome-Kaius M, Unger HW, Singirok D, et al. Determining effects of areca (betel) nut chewing in a prospective cohort of pregnant women in Madang Province, Papua New Guinea. BMC Pregnancy Childbirth 2015;15:177. 10.1186/s12884-015-0615-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. National Capital District Commision. National District Betelnut Control Law 2013: Port Moresby National Capital District Commision, 2013. [Google Scholar]
- 70. Hornabrook RW, Serjeantson S, Stanhope JM. The relationship between socioeconomic status and health in two Papua New Guinean populations. Hum Ecol 1977;5:369–82. 10.1007/BF00889177 [DOI] [Google Scholar]
- 71. Teevale T, Robinson E, Duffy S, et al. Binge drinking and alcohol-related behaviours amongst Pacific youth: a national survey of secondary school students. N Z Med J 2012;125:1352. [PubMed] [Google Scholar]
- 72. Marshall M. Alcohol consumption as a public health problem in Papua New Guinea. Int J Addict 1988;23:573–89. 10.3109/10826088809039220 [DOI] [PubMed] [Google Scholar]
- 73. Hinton R, Earnest J, Stressors EJ. Stressors, coping, and social support among women in Papua New Guinea. Qual Health Res 2010;20:224–38. 10.1177/1049732309357572 [DOI] [PubMed] [Google Scholar]
- 74. Vengiau G, Umezaki M, Phuanukoonnon S, et al. Diet and physical activity among migrant Bougainvilleans in Port Moresby, Papua New Guinea: association with anthropometric measures and blood pressure. Am J Hum Biol 2012;24:716–8. 10.1002/ajhb.22299 [DOI] [PubMed] [Google Scholar]
- 75. Norgan NG. Changes in patterns of growth and nutritional anthropometry in two rural modernizing Papua New Guinea communities. Ann Hum Biol 1995;22:491–513. 10.1080/03014469500004162 [DOI] [PubMed] [Google Scholar]
- 76. Asia Pacific Cohort Studies Collaboration. Central obesity and risk of cardiovascular disease in the Asia Pacific Region. Asia Pac J Clin Nutr 2006;15:287–92. [PubMed] [Google Scholar]
- 77. Welborn TA, Dhaliwal SS. Preferred clinical measures of central obesity for predicting mortality. Eur J Clin Nutr 2007;61:1373–9. 10.1038/sj.ejcn.1602656 [DOI] [PubMed] [Google Scholar]
- 78. Brownell KD, Frieden TR. Ounces of prevention--the public policy case for taxes on sugared beverages. N Engl J Med 2009;360:1805–8. 10.1056/NEJMp0902392 [DOI] [PubMed] [Google Scholar]
- 79. Sundborn G, Merriman T, Thornley S, et al. An ‘End-Game’for sugar sweetened beverages? Pacific health dialog 2014;20:1. [PubMed] [Google Scholar]
- 80. Whyte HM. Body fat and blood pressure of natives in New Guinea: reflections on essential hypertension. Australas Ann Med 1958;7:36–46. [DOI] [PubMed] [Google Scholar]
- 81. Maddocks I. Blood pressures in Melanesians. Med J Aust 1967;1:1123. [DOI] [PubMed] [Google Scholar]
- 82. King H, Collins A, King LF, et al. Blood pressure in Papua New Guinea: a survey of two highland villages in the Asaro Valley. J Epidemiol Community Health 1985;39:215–9. 10.1136/jech.39.3.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Carvalho JJ, Baruzzi RG, Howard PF, et al. Blood pressure in four remote populations in the INTERSALT Study. Hypertension 1989;14:238–46. 10.1161/01.HYP.14.3.238 [DOI] [PubMed] [Google Scholar]
- 84. Boyce AJ, Attenborough RD, Harrison GA, et al. Variation in blood pressure in a New Guinea population. Ann Hum Biol 1978;5:313–9. 10.1080/03014467800002961 [DOI] [PubMed] [Google Scholar]
- 85. Maddocks I, Vines AP. The influence of chronic infection on blood-pressure in New Guinea males. Lancet 1966;2:262–4. 10.1016/S0140-6736(66)92545-1 [DOI] [PubMed] [Google Scholar]
- 86. Stanhope J. Blood pressures of the Tinam-Aigram people, near Simbai, Madang District. PNG Med J 1968;11:60–1. [Google Scholar]
- 87. Scrimgeour EM, McCall MG, Smith DE, et al. Levels of serum cholesterol, triglyceride, HDL-cholesterol, apoproteins A-I and B, and plasma glucose, and prevalence of diastolic hypertension and cigarette smoking in Papua New Guinea highlanders. Pathology 1989;21:46–50. 10.3109/00313028909059530 [DOI] [PubMed] [Google Scholar]
- 88. Lindeberg S, Nilsson-Ehle P, Terént A, et al. Cardiovascular risk factors in a Melanesian population apparently free from stroke and ischaemic heart disease: the Kitava study. J Intern Med 1994;236:331–40. 10.1111/j.1365-2796.1994.tb00804.x [DOI] [PubMed] [Google Scholar]
- 89. Erasmus RT, Sinha AK, Nathaniel K. Serum lipid concentrations in the Koki community: a preliminary report. P N G Med J 1993;36:306–10. [PubMed] [Google Scholar]
- 90. Swinburn BA, Walter LG, Arroll B, et al. The green prescription study: a randomized controlled trial of written exercise advice provided by general practitioners. Am J Public Health 1998;88:288–91. 10.2105/AJPH.88.2.288 [DOI] [PMC free article] [PubMed] [Google Scholar]


