Abstract
Purpose
Superiority of non-operative versus operative treatment of clavicle shaft fractures remains unclear. We aimed to assess shoulder function in adolescents following shortened clavicle fracture and compare operative versus non-operative treatment.
Methods
Patients aged 12 to 18 years at the time of fracture and minimum 1.5 years post injury were identified for this institutional review board (IRB)-approved study. For this retrospective cohort study, patients were frequency-matched for age, gender, shortening of the clavicle fracture and activity level. The dominant arm was controlled in the statistical model. Initial radiographs were used to measure clavicle shortening. At follow-up, isokinetic testing of both shoulders was performed in flexion, external rotation and the plane of scapular motion. Maximum number of isotonic repetitions and average isometric torque were recorded, as were ASES and DASH scores. Data were analysed comparing non-operative and operative groups and involved and uninvolved shoulders.
Results
Twenty patients were recruited (18 male, 2 female), with ten in each group. Median clavicle shortening was 17.5 mm (11.4 to 23.6). There was no statistical difference in average ASES (100 vs 99; p = 0.84) or DASH (0.0 vs 1.7; p = 0.08) between non-operative and operative groups, respectively. Results of isokinetic testing comparison between non-operative and operative groups showed no statistical difference for any individual association, controlling for the dominant arm. Among the non-operative group, the involved arm had decreased functional measures compared with the uninvolved arm on all measures, when controlling for dominant arm, and there was increased variability of the functional estimate.
Conclusions
The increased variability in functional measures for the non-operative group suggests some patients may have dysfunction.
Keywords: clavicle fracture, adolescent, function, patient-reported outcomes, biomechanics
Introduction
Fractures of the shaft of the clavicle are common in both adults and children.1 Many fractures heal with non-operative treatment without adverse sequelae, but there exists a subset of patients who may benefit from operative intervention.2-4 In particular, controversy exists about optimal treatment of a midshaft clavicle fracture in the presence of significant displacement, comminution or shortening of the fracture in adolescents.2-5
Recent studies in the adult literature have indicated that improved functional outcomes are achieved after open reduction and internal fixation of the clavicle.2,3,5 McKee et al examined 111 patients with midshaft clavicle fractures randomised to either traditional non-operative treatment or open reduction and internal fixation with a plate.5 That study found superiority of operative fixation, with superior surgeon-based (Constant shoulder score) and patient-based (Disabilities of the Arm, Shoulder and Hand (DASH) score) outcome measures at every time-point in the study. Patients who underwent operative fixation had an earlier return to normal function.5 Additionally, a multicentre randomised controlled trial performed in Canada also suggested that operative fixation of displaced clavicle shaft fractures resulted in improved Constant and DASH scores among adults compared with non-operative treatment.3 In addition, operative fixation yielded a faster time to union and lower rate of nonunion.
The literature on this topic among children and adolescents remains less clear. One study found that adolescent patients who underwent operative fixation of closed midshaft clavicle fracture had shorter time to union and low complication rates.4 Patients who underwent non-operative fixation were more likely to report subjective complaints related to malunion, particularly those with increased shortening. Namdari et al also recently reported high functional outcomes in skeletally immature patients treated with operative fixation for displaced clavicle fractures; however, there was no control group to compare outcomes.6 On the other hand, more recent studies have suggested no subjective or functional deficit among small series of adolescent patients with displacement or shortening following midshaft clavicular fracture.7-9
The primary aim of this study was to assess shoulder function and patient-reported physical functioning outcomes in children and adolescents following clavicle fractures. We sought to compare patients who presented with clavicle shortening and underwent operative intervention compared with patients who presented with clavicle shortening and underwent non-operative intervention. We compared the operative and non-operative groups, as well as the injured versus uninjured arms within patients.
Patients and methods
Patient selection
Patients who sustained a clavicle fracture and sought treatment at our institution were selected for this institutional review board (IRB)-approved cohort study. At the start of the study, all patients who were treated for a clavicle fracture between 1 January 2009 and 31 December 2012 were identified (n = 506). A thorough chart review was performed for all patients identified to determine eligibility for the study. Included patients were those who sustained a midshaft clavicle fracture, were aged 12 to 18 years at the time of fracture (median age = 13 years), and had clavicle shortening ≥ 10 mm at the time of the injury. Patients were excluded if they had clavicle shortening < 10 mm or initial injury radiographs were not available. Other exclusion criteria were open fracture, pathological fracture, physeal fracture, bilateral fractures, sternoclavicular or acromioclavicular dislocation, previous injury or surgery of the clavicle or shoulder, associated neurovascular injury and < 1.5 years post injury. Patients who met the inclusion criteria were included in the source study population.
A total of 56 patients met the inclusion criteria. Patients were aged 15 to 22 years at the time of follow-up (median age = 17 years). In total, 22 patients (39%) underwent surgical fixation of the clavicle fracture and 34 patients (61%) underwent non-operative treatment. Of these patients, ten patients who underwent surgical fixation were available for participation in the study. In addition, ten patients who underwent non-operative treatment were frequency-matched to the operative cohort on age at injury, current age, gender, clavicle shortening and activity level as a control group. Patients and parents/guardians were contacted by telephone and invited to come for a study visit to complete a subjective questionnaire and undergo biomechanical testing of the upper extremities.
Surgical technique
Patients who underwent surgical fixation of the clavicle fracture generally underwent stabilisation by a similar surgical technique. The fracture was first reduced by open reduction. In most patients, the fracture was fixed with an intramedullary screw. The lateral aspect of the clavicle was prepared with a clavicle step drill, and a 3-mm Dual-Trak clavicle screw (Acumed, Hillsboro, OR, USA) was inserted laterally. In some patients, the fracture was fixed with a modular clavicle plate (DePuy Synthes, West Chester, PA, USA). The plate was placed to allow for proper contour of the clavicle. Locking screws were used to secure the fracture.
Rehabilitation
All patients, regardless of treatment group, underwent a similar rehabilitation protocol following injury or surgery. Patients were placed in a sling for two weeks following surgery and two to four weeks following injury for the non-operatively treated patients. Range of motion was progressed gradually, with immediate range of motion pursued for the hand, wrist and elbow. Typically, gradual return to sport began eight weeks following injury for the non-operative group or eight weeks following surgery for the operative group.
Data collection
Radiographs from the first office visit for the injury were obtained for all patients treated for a clavicle fracture between 1 January 2009 and 31 December 2012 (n = 506) to determine inclusion in the study. Measurements were taken by four experienced clinicians to determine amount of clavicle shortening. Shortening was measured using cortex to corresponding cortex rather than total shortening, which was felt to be less likely to overestimate shortening. A paediatric orthopaedic surgery fellow measured all radiographs first. Six weeks following the initial measurement of all radiographs, the same orthopaedic surgery fellow measured all radiographs again to determine intra-rater reliability. Three board-certified, attending orthopaedic surgeons also measured all of the radiographs (one-third each). When agreement was not obtained on clavicle length measurement (all measurements within 2 mm), the orthopaedic surgery fellow measured the radiograph a fourth time. If at least three measurements were within 2 mm of each other, the patient was included and the average measurement was used. If fewer than three measurements were within 2 mm of each other, the patient was excluded.
Patient demographic information was collected by chart review and at the time of the study visit. Information collected by chart review included date of birth, date of injury, injured side, dominant hand, gender and date of surgery (if applicable). Activity level was collected as sport(s) participated in at the time of injury. At the time of the study visit, patients and parents/guardians (if patient were aged < 18 years) consented to participate in the research study. Patients were then asked to complete a detailed subjective questionnaire, which included information about patient weight, subsequent surgical treatment for the clavicle and current activity level. Patients also completed an American Shoulder and Elbow Surgeons standardised shoulder form patient self-report section (ASES),10 a DASH score11 and additional questions about clavicle cosmetic deformity, chronic pain and weakness (included as supplemental information).
Following consent to participate and completion of the questionnaire, patients performed isokinetic and functional testing of the injured and uninjured shoulders. Isokinetic testing was performed using a Biodex isokinetic testing system (Biodex Medical Systems, New York, NY, USA). One investigator completed six weeks of training with a Biodex representative and a physical therapist, passed a competency examination on testing performed for the purposes of this study, and performed all study participant isokinetic testing. Testing was performed in the seated position on both upper extremities in flexion, the plane of scapular motion (scaption-abduction) and external rotation. Isokinetic maximum torque, maximum number of isotonic repetitions and average isometric torque were recorded.
A strict protocol was followed for all participants to ensure consistency in testing. Testing started with the uninvolved arm. Maximum isokinetic torque was obtained by instructing the participant to pull up into the handle of the Biodex as hard as possible while lifting the arm from 0° of shoulder flexion to 180° of shoulder flexion five times. Patients were instructed to use consistent pressure and speed throughout the motion. Maximum isokinetic torque was recorded if the test variance was ≤ 15%. If the test variance was > 15%, the test was repeated and instructions to use consistent pressure and speed throughout the motion were reiterated. Isotonic testing was performed in flexion using the involved arm first. Baseline torque was set to 50% of the maximum recorded isokinetic torque. Patients were instructed to perform as many repetitions as possible prior to fatigue. Repetitions were counted until the patient was unable to perform the motion with consistent form or until the patient reported pain or extreme fatigue. The third and final test of shoulder flexion was of isometric strength, starting with the uninvolved arm. The Biodex was placed stationary at 90° of shoulder flexion and baseline torque was set to 50% of the maximum isokinetic torque. The patient was instructed to grip the handle and pull up into the handle as hard as possible for 5 seconds, followed by a 10-second rest, repeated three times. Average isometric torque was recorded if the test variance was ≤ 15%. If the test variance was > 15% the test was repeated and instructions were given to use consistent pressure throughout the 5-second test period. These same procedures were repeated in the plane of scapular motion and in external rotation. A 1-minute rest break was given between all tests.
Statistical analyses
All statistical analyses were performed using SAS 9.4 (SAS Institute, Cary, NC, USA). Prior to the start of the study, several variables were identified as potential confounders of the association between the non-operative versus operative treatment groups and the functional testing outcomes. Age at injury, current age, gender, clavicle shortening and activity level were controlled for using a frequency-matched sampling design. Affected clavicle (dominant vs non-dominant) was controlled in the statistical model.
Fisher’s exact test was used to compare the presence of cosmetic deformity, chronic pain and weakness. Wilcoxon rank sum tests were used to compare ASES and DASH scores between the operative and the non-operative groups. Significance was assessed in two ways: 95% confidence intervals (CI) were used to assess significance of an effect estimate, where a statistically significant result was a confidence interval that did not include the null value, in addition to using a two-tailed p-value < 0.05.
The primary analysis involved comparison of non-operative and operative groups for functional and subjective outcomes, controlling for dominant arm. A secondary analysis, comparing each participant’s involved versus uninvolved extremity, controlling for dominant arm and stratified by non-operative group or operative group, was also performed. There were six unique functional outcomes of interest: flexion maximum number of isotonic repetitions; flexion average isometric torque; scaption-abduction maximum number of isotonic repetitions; scaption-abduction average isometric torque; external rotation maximum number of isotonic repetitions; and external rotation average isometric torque. Isotonic maximum torque was used to standardise the resistance of the Biodex machine for all other tests so that the results could be compared between participants. Univariable analysis was performed to determine the distribution of all variables of interest. Linear regression modelling was used to test the association between the exposure (operative vs non-operative) and the functional outcome, controlling for dominant arm. Generalised estimating equations (GEE) modelling with a linear specification was used to test the association between the exposure of involved versus uninvolved arms and the functional outcomes of interest, controlling for dominant arm and stratified by operative versus non-operative group, since the data were highly correlated within each individual. Beta coefficients and 95% CIs were recorded.
Results
There were 20 patients enrolled in this study, with ten in the operative group and ten in the non-operative group. The groups were balanced on age at injury, current age, gender, clavicle shortening and activity level due to intentional frequency matching during sampling (Table 1).
Table 1.
Results of analysis of matching variables between the operative and non-operative groups (n = 20).
| Variable | Operative group (n = 10) | Non-operativegroup (n = 10) | p-value |
|---|---|---|---|
| Age at injury (years) | 14.6 ± 1.8 | 14.1 ± 0.9 | 0.60 |
| Current age (years) | 18.1 ± 2.0 | 17.9 ± 1.7 | 0.84 |
| Clavicle shortening (mm)* | 17.2 ± 3.5 | 17.8 ± 3.1 | 0.53 |
| Male gender | 9 (90%) | 9 (90%) | 1.00 |
Clavicle shortening was measured at the time of the initial office visit for the clavicle fracture.
In the operative group, there were three non-athletes, three baseball players, two soccer players, one football player and one BMX biker/gymnast. In the non-operative group, there were two non-athletes, two baseball players, one lacrosse player, three football players, one biker and one ice skater. Of those who underwent surgical fixation, eight patients underwent fixation with an intramedullary screw and two with a plate. One patient was scheduled for hardware removal following participation in the research study; no others reported hardware removal procedures. There were no nonunions reported in either group.
The median time to follow-up was 2.6 years (1.4 to 5.2). There was no significant difference in follow-up time by group (non-operative: median = 2.6 (1.4 to 4.2); operative: median = 3.4 (1.5 to 5.2); p = 0.25). There was a significant difference in report of cosmetic deformity with two (20%) reports of deformity in the operative group and nine (90%) in the non-operative group (p < 0.01). There was no significant difference in report of chronic pain (0 vs 1; p = 1.00) or weakness (0 vs 3; p = 0.21) in the operative group compared with the non-operative group, respectively. There was also no statistically significant difference in ASES (99 vs 100; p = 0.84) or DASH (1.7 vs 0.0; p = 0.08) between the operative and non-operative groups, respectively.
Results of isokinetic testing comparison between groups (non-operative vs operative) showed no statistical difference for any individual association between the operative group and the non-operative group, controlling for dominant arm (Fig. 1; Table 2). For comparison of involved to uninvolved, the operative group showed significant differences in functional measurement between arms when controlling for dominant arm (Fig. 2a). The involved arm was significantly stronger than the uninvolved arm (Fig. 2a), when controlling for dominant arm, for scaption-abduction isometric average peak torque (β = 4.0; 95% CI 2.9 to 5.1; p < 0.01) and external rotation isometric average peak torque (β = 1.3; 95% CI 0.7 to 1.9; p < 0.01). However, the involved arm was significantly weaker than the uninvolved arm, when controlling for dominant arm, for scaption-abduction isotonic maximum repetitions (β = –3.3; 95% CI -5.0 to -1.7; p < 0.01) and external rotation isotonic maximum repetitions (β = –2.1; 95% CI -3.2 to –1.0; p < 0.01). There was very little variability between participants within each testing measure for the comparison between involved and uninvolved arm among the operative group, as noted by the narrow confidence intervals.
Fig. 1.
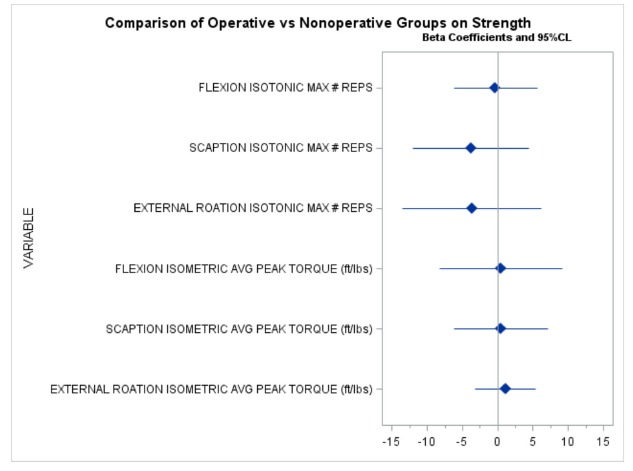
Comparison of non-operative versus operative group for six functional strength measures (n = 20). a) Negative beta (β) indicates the non-operative group had lower average values. b) Statistically significant differences were those where the 95% CI did not include the null value (β = 0).
Table 2.
Functional outcome data with comparison between the operative and non-operative groups (n = 20).
| Strength values* | Percent of uninvolved side | |||||
|---|---|---|---|---|---|---|
| Variable | Operative group (n = 10) | Non-operative group (n = 10) | p-value | Operative group (n = 10) | Non-operative group(n = 10) | p-value |
| Flexion max reps | 15.3 ± 9.5 | 14.5 ± 5.2 | 1.00 | 91.4 ± 23.9 | 90.3 ± 31.5 | 0.82 |
| Scaption max reps | 18.8 ± 8.8 | 23.4 ± 12.2 | 0.38 | 79.1 ± 15.9 | 78.4 ± 29.3 | 0.79 |
| ER max reps | 24.2 ± 15.3 | 27.2 ± 9.4 | 0.29 | 82.1 ± 16.2 | 85.9 ± 14.8 | 0.63 |
| Flexion avg torque | 28.5 ± 11.4 | 29.7 ± 9.6 | 0.97 | 97.4 ± 7.8 | 93.7 ± 13.9 | 0.91 |
| Scaption avg torque | 21.9 ± 10.1 | 23.1 ± 7.8 | 0.74 | 94.2 ± 22.3 | 96.1 ± 24.3 | 0.91 |
| ER avg torque | 14.9 ± 5.0 | 14.2 ± 4.7 | 0.63 | 95.4 ± 16.3 | 93.0 ± 18.7 | 0.85 |
Reps presented as counts, torque presented in ft/lbs
Fig. 2.
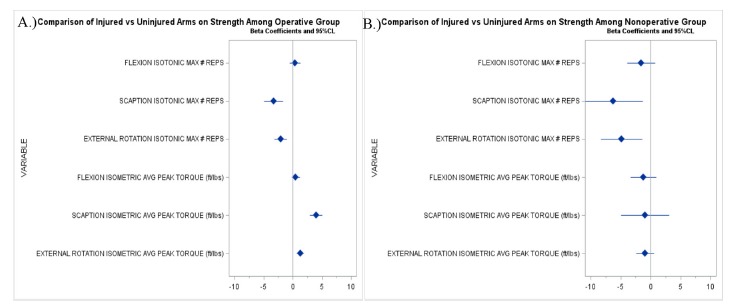
Comparison of involved versus uninvolved arm for six functional strength measures in the a) operative group (n = 10) and b) non-operative group (n = 10). a) Negative beta (β) indicates the involved arm had lower average values. b) Statistically significant differences were those where the 95% CI did not include the null value (β = 0).
Among the non-operative group, there was also a significant decrease in functional measurement for scaption-abduction isotonic maximum repetitions (β = -6.3; 95% CI -11.3 to -1.3; p = 0.01) and external rotation isotonic maximum repetitions (β = -4.9; 95% CI -8.3 to -1.4; p = 0.01) between the involved and uninvolved arm, when controlling for dominant arm (Fig. 2b; Table 3). There was increased variability between participants within each functional measure when comparing the involved with the uninvolved arm for all six functional measures among the non-operative group, as indicated by the wide confidence intervals around the point estimates. In addition, all six functional estimates for the involved arm were below zero for the non-operative group, suggesting possible decreased strength in the involved arm compared with the uninvolved arm.
Table 3.
Functional outcome data with comparison between the injured and uninjured extremities (n = 20).
| Operative group | Non-operative group | |||||
|---|---|---|---|---|---|---|
| Variable | Injured arm (n = 10) | Uninjured arm (n = 10) | p-value | Injured arm (n = 10) | Uninjured arm (n = 10) | p-value |
| Flexion max reps (count) | 15.3 ± 9.5 | 16.3 ± 8.7 | 0.77 | 14.5 ± 5.2 | 16.4 ± 6.1 | 0.82 |
| Scaption max reps (count) | 18.8 ± 8.8 | 24.8 ± 12.2 | 0.28 | 23.4 ± 12.2 | 30.4 ± 13.2 | 0.25 |
| ER max reps (count) | 24.2 ± 15.3 | 28.8 ± 14.3 | 0.48 | 27.2 ± 9.4 | 32.8 ± 12.6 | 0.35 |
| Flexion avg torque (ft/lbs) | 28.5 ± 11.4 | 29.1 ± 10.9 | 0.71 | 29.7 ± 9.6 | 31.3 ± 7.6 | 0.74 |
| Scaption avg torque (ft/lbs) | 21.9 ± 10.1 | 23.1 ± 9.2 | 0.88 | 23.1 ± 7.8 | 24.2 ± 7.9 | 1.00 |
| ER avg torque (ft/lbs) | 14.9 ± 5.0 | 15.4 ± 4.2 | 0.94 | 14.2 ± 4.7 | 15.1 ± 3.5 | 0.60 |
Discussion
Clavicle fractures that present with significant shortening can be a challenging clinical problem, particularly among children and adolescents. Surgery often places a burden on the patient and family. Additionally, the propensity for healing fractures non-operatively in a young, healthy patient population is high, so surgical intervention is often deemed unnecessary.12,13 However, in recent years, emphasis has been placed on restoring native anatomical structure after various orthopaedic injuries. Therefore, surgical fixation that improves clavicle position and anatomy may be beneficial in the long term. This study sought to analyse the functional outcomes following clavicle fractures that resulted in significant shortening, comparing operative versus non-operative treatment, in an effort to add to the literature on treatment decision-making in adolescent patients with clavicle fracture.
Overall, the results of this study suggest that there is no difference in objective function or subjective patient-reported physical functioning outcome between operatively and non-operatively treated patients with shortened, midshaft clavicle fracture. However, the results of isokinetic testing also suggest that there is increased variability in functional measurements for the involved arm compared with the uninvolved arm among patients treated non-operatively, when controlling for dominant arm. Among the operative group, there was very little variability between patients in the mean functional measurement for the involved compared with the uninvolved arm, when controlling for dominant arm. These results suggest that some patients who are treated non-operatively may have decreased function in the involved arm compared with the uninvolved arm. In contrast, patients treated operatively may have a more stable, reliable objective functional outcome in the involved arm compared with the uninvolved arm, as indicated by the precise point estimates obtained for functional measures in this group. In addition, for all six isokinetic tests the mean functional measure for the involved arm was below zero in the non-operative group (Fig. 2b). Although not statistically significant in this study, this also indicates that the non-operative group may have decreased function in the involved arm compared with the uninvolved arm, when controlling for dominant arm. In contrast, the operative group had increased functional measurement in the involved compared with the uninvolved arm, when controlling for dominant arm, for both scaption-abduction and external rotation average isometric torque. Both the operative and non-operative groups had significantly decreased values for the involved compared with the uninvolved arm for scaption-abduction isotonic maximum repetitions and external rotation isotonic maximum repetitions.
In terms of the clinical relevance of these functional measurements, the isotonic maximum repetitions require the patient to perform the maximum number of repetitions with resistance set to 50% of the patient’s maximum torque. Consequently, we believe the data from these tests represent endurance rather than strength. On the other hand, average isometric torque is calculated from maximum torque applied to an immobile dynamometer in short bursts (5 seconds each). Therefore, we believe these data indicate measures of strength. Given these assumptions, it appears that both the operative and non-operative groups had significantly decreased endurance in the involved arm compared with the uninvolved arm. The operative group had increased strength in the involved arm compared with the uninvolved arm.
As with other similar studies on this topic, it is difficult to understand the true clinical relevance of these findings. The functional assessment suggests that both groups had a significant decrease in isotonic maximum repetition measurement for the involved arm compared with the uninvolved arm; however, the average patient-reported outcome scores for each group indicate nearly perfect scores on both the ASES and DASH outcome tools. While at first glance this may seem to suggest that the functional findings are not clinically relevant, it is also possible that these findings highlight limitations with the patient-reported outcome tools used. In particular, the results of the ASES and DASH scores provide information on upper extremity functioning in activities of daily living for a typical adult, rather than physical activities that may be pertinent to this age group. Furthermore, these scores have not been validated in children and adolescents. The findings may suggest a propensity for ceiling effects with these scores, particularly in a young, relatively healthy population such as the one studied here. In fact, the range of the ASES in our population was 78 to 100, with a median of 100 and only one patient scoring below 90. The range of the DASH was 0 to 12, with a median of 0.9 and only one patient scoring above 7. Additionally, one patient in our study subjectively reported experiencing weakness of the injured arm; however, this patient scored 100 on the ASES score and zero on the DASH, indicating perfect scores. Another patient indicated pain with repetitive motion during the testing session. This patient also had perfect outcome scores of 100 on the ASES and zero on the DASH. Therefore, we believe it is possible that these tools are not measuring the physical functioning domains that are relevant to this population and likely are not sensitive enough to identify subtle but important functional deficits that may be experienced by young, active patients. Consequently, there is a need for valid, reliable and responsive outcome tools for the upper extremity specific to the young, active population in order to better understand patient-reported physical functioning outcomes.
Recently, two similar studies have assessed functional outcomes following non-operative versus operative treatment of midshaft clavicle fractures in children and adolescents. One study assessed adolescents with completely displaced, shortened fractures and compared the injured arm with the uninjured arm.8 The study found a significant decrease in maximal shoulder external rotation strength and shoulder abduction endurance strength; however, the authors concluded that these findings were irrelevant because the patient-reported outcome scores and satisfaction were very high. The second study also analysed functional outcomes following displaced, shortened midshaft clavicular fractures among adolescents.7 That study also concluded that patients had excellent functional and patient-reported outcomes, regardless of treatment. Interestingly, all but one patient had a perfect score on the QuickDASH and Constant outcome scores.
The results of our study add to the literature by providing additional evidence for functional outcomes comparing operative and non-operative treatment of shortened midshaft clavicular fractures in adolescents. Given that these fractures represent a minority of patients who present to a typical paediatric orthopaedic practice, the sample sizes reported are often small. With further reports on this topic, ideally systematic reviews and meta-analyses can be performed to further understand the benefits of each treatment in this patient population.
Different from the two previous reports, this study also provides an analysis that controls for dominant arm. Hand dominance is important for understanding the functional outcome in this population, as it has been shown to affect function.14,15 In non-randomised studies such as this one, there is potential for residual confounding or incomparable patient populations between the operative and non-operative groups. With this research question, in particular, it is difficult to tease out the patients’ and physicians’ motivations for treatment retrospectively. It is possible that patients who injure their dominant arm are more likely to undergo operative treatment of a shortened clavicle fracture. Therefore, we chose to control for arm dominance in the statistical model.
There are limitations to the data collected. First, the sample size is very small due to the limited number of patients who met the inclusion criteria at our institution and who could be contacted. While the sample size is small, the addition to the existing literature will provide a basis for future systematic reviews and meta-analyses on this topic; however, future multicentre studies are important to understand better the pros and cons of each treatment option. Second, the patients who agreed to participate may not be generalisable to the group of all patients who meet the criteria for this study. The requirement of an additional testing session and use of a specific patient population may result in selection bias within our study. Third, the functional measures obtained may not accurately represent upper extremity function in these patients. The strict testing protocol and laboratory environment may not be representative of daily functioning. In addition, the 1-minute rest break between tests may not have been sufficient to obtain accurate strength measures. However, care was taken to ensure that each patient was tested in a systematic and reliable way, which we believe allows for comparison of groups regardless of reported strength measures. Fourth, we did not record information on clavicle length at the time of follow-up due to desire to minimise risks, including exposure to radiation. It is possible that clavicle length after healing could have affected the results; however, the aim of the study was to compare two groups of patients based on initial clavicle injury findings. Therefore, we believe this patient population provides insight into a clinically relevant question about optimal treatment given shortening at the time of injury. We also did not collect information on skeletal maturity. Finally, there may be residual confounding between the operative and non-operative groups that was uncontrolled in the analysis. As stated above, given the retrospective nature of this research study, we were unable to identify patient motivation for treatment choice. Therefore, there may be inherent differences between the operative and non-operative groups that we did not control. It is possible that sport participation may influence treatment choices and outcomes. While sports participation was relatively balanced between groups in our study, future studies should specifically address this important variable.
Compliance with ethical standards
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
No funding was received for this study.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study. This study was approved by the Children’s Healthcare of Atlanta Institution Review Board under IRB# 12-133.
ICMJE Conflict of interest statement
MH is a paid employee of QuintilesIMS. MB is a paid educator for OrthoPediatrics and Arthrex. SCW is a consultant for Smith & Nephew. All other authors declare no conflict of interest.
References
- 1.Nordqvist A, Petersson C.. The incidence of fractures of the clavicle. Clin Orthop Relat Res 1994;300:127-132. [PubMed] [Google Scholar]
- 2.McKee MD, Pedersen EM, Jones C, et al. Deficits following nonoperative treatment of displaced midshaft clavicular fractures. J Bone Joint Surg [Am] 2006;88-A:35-40. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Orthopaedic Trauma Society Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg [Am] 2007;89-A:1-10. [DOI] [PubMed] [Google Scholar]
- 4.Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop 2010;30:307-312. [DOI] [PubMed] [Google Scholar]
- 5.McKee RC, Whelan DB, Schemitsch EH, McKee MD. Operative versus nonoperative care of displaced midshaft clavicular fractures: a meta-analysis of randomized clinical trials. J Bone Joint Surg [Am] 2012;94-A:675-684. [DOI] [PubMed] [Google Scholar]
- 6.Namdari S, Ganley TJ, Baldwin K, et al. Fixation of displaced midshaft clavicle fractures in skeletally immature patients. J Pediatr Orthop 2011;31:507-511. [DOI] [PubMed] [Google Scholar]
- 7.Parry JA, Van Straaten M, Luo TD, et al. Is there a deficit after nonoperative versus operative treatment of shortened midshaft clavicular fractures in adolescents? J Pediatr Orthop 2017;37:227-233. [DOI] [PubMed] [Google Scholar]
- 8.Schulz J, Moor M, Roocroft J, Bastrom TP, Pennock AT. Functional and radiographic outcomes of nonoperative treatment of displaced adolescent clavicle fractures. J Bone Joint Surg [Am] 2013;95:1159-1165. [DOI] [PubMed] [Google Scholar]
- 9.Hagstrom LS, Ferrick M, Galpin R. Outcomes of operative versus nonoperative treatment of displaced pediatric clavicle fractures. Orthopedics 2015;38:e135-e138. [DOI] [PubMed] [Google Scholar]
- 10.Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg 2002;11:587-594. [DOI] [PubMed] [Google Scholar]
- 11.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996;29:602-608. [DOI] [PubMed] [Google Scholar]
- 12.Kubiak R, Slongo T. Operative treatment of clavicle fractures in children: a review of 21 years. J Pediatr Orthop 2002;22:736-739. [PubMed] [Google Scholar]
- 13.Carry PM, Koonce R, Pan Z, Polousky JD. A survey of physician opinion: adolescent midshaft clavicle fracture treatment preferences among POSNA members. J Pediatr Orthop 2011;31:44-49. [DOI] [PubMed] [Google Scholar]
- 14.Gallagher MA, Cuomo F, Polonsky L, Berliner K, Zuckerman JD. Effects of age, testing speed, and arm dominance on isokinetic strength of the elbow. J Shoulder Elbow Surg 1997;6:340-346. [DOI] [PubMed] [Google Scholar]
- 15.Ozaras N, Cidem M, Demir S, et al. Shoulder pain and functional consequences: does it differ when it is at dominant side or not? J Back Musculoskelet Rehabil 2009;22:223-225. [DOI] [PubMed] [Google Scholar]


