Abstract
Purpose
Complete fibula absence often presents with significant lower-limb deformity. Parental counselling regarding management is paramount in achieving the optimum functional outcome. Amputation offers a single surgical event with minimal complications. This study compares outcomes with an amputation protocol to those using an extension prosthesis.
Method
Thirty-two patients were identified. Nine patients (2 males, 7 females; median age at assessment of 23.5 years) used an extension prosthesis. Twenty-three patients (16 males, 7 females; median age at assessment of eight years) underwent 25 amputations during childhood. Mobility was assessed using SIGAM and K scores. Quality of life was assessed using the PedsQL inventory questionnaire; pain by a verbal severity score.
Results
The 19 Syme and one Boyd amputation in 19 patients were performed early (mean age 15 months). Four Syme and one trans-tibial amputation in four patients took place in older children (mean age 6.6 years). Only two underwent tibial kyphus correction to aid prosthetic fitting. K scores were significantly higher (mean 4 vs 2) and pain scores lower in the amputation group allowing high impact activity compared with community ambulation with an extension prosthesis. The SIGAM and PedsQL scores were all better in the amputation group, but not significantly so.
Conclusion
Childhood amputation for severe limb length inequality and foot deformity in congenital fibula absence offers excellent short-term functional outcome with prosthetic support. The tibial kyphus does not need routine correction and facilitates prosthetic suspension. Accommodative extension prostheses offer reasonable long-term function but outcome scores are lower.
Keywords: fibula hemimelia, congenital absence of fibula, Syme amputation, extension prosthesis
Introduction
Congenital deficiency of the fibula is the most common long bone deficiency.1,2 The term fibula hemimelia describes a post axial longitudinal deficiency which has a wide spectrum of clinical and radiological presentation ranging from minor hypoplasia of the fibula to complete absence. In severe cases, limb deformity is portrayed by significant limb shortening, anterior tibial bowing and foot deformity including tarsal coalition, formation of a ball and socket ankle joint, absent rays and a fixed equinovalgus or rarely equinovarus foot position. Other more proximal anomalies may also be present such as femoral deformity (proximal varus, valgus and retroversion, hypoplasia of the lateral femoral condyle and absent cruciate ligaments) with acetabular dysplasia. Upper limb deformities include ulna hemimelia or amelia and syndactyly.
Classification systems have focused on these parameters in order to aid parental counselling and surgical decision-making.3-6 Treatment options include orthotic and prosthetic support of the affected limb, amputation to assist in prosthetic support and limb reconstruction techniques to produce limbs of equal length with a functional weight-bearing foot at skeletal maturity.
Complete absence of the fibula is often associated with a more significant limb length discrepancy and more severe foot deformities and the consensus opinion would consider amputation in these patients.4-13 The decision to undertake an amputation in early childhood remains one of the most difficult a parent can make for the wellbeing of their child. The long-term optimum function of the child is paramount and a clear discussion on risk versus benefit in any surgical procedure is required. An amputation potentially offers a single surgical event with low risk of complications. Limb reconstruction utilising the Ilizarov method as an alternative to amputation has been reported.14-20 This technique, however, requires multiple operations with prolonged treatment times in the external fixator and is frequently associated with significant complications and in several cases residual limb length discrepancy and foot deformity (equinus and valgus) following surgery. Several studies have compared amputation with limb reconstruction, favouring amputation on the basis of fewer surgical events, less pain and better satisfaction.9,10,12,13
At our institution, the preferred management of a child presenting with congenital absence of the fibula is based on predicted leg length discrepancy and severity of the foot deformity. With a predictive leg length discrepancy of greater than 20 cm a Syme disarticulation is the treatment of choice. A stiff equinovalgus foot deformity with absence of two or three rays, where achieving a plantigrade functioning weight-bearing foot is extremely difficult, is also an indication for amputation. It is also accepted that fibula deficiency with similar limb length discrepancy and foot deformity can be considered for amputation. Similarly, absence of the fibula can be associated with limb shortening that is suitable for reconstruction and present with feet that are clinically normal. In some cases, parents opt for no surgical intervention, preferring to rely on an extension prosthesis to maintain limb length equality. The aim of this study was to evaluate the outcome of amputation against extension prosthetic management and to identify any effect on function if the amputation was delayed. We anticipated that this would provide further information that would help parents’ decision-making in the management of severe lower-limb congenital deformity.
Patients and methods
On referral to our institution, a child with a congenital limb deformity is first seen by a Consultant Paediatric Orthopaedic Surgeon with a specialist interest in limb reconstruction. A diagnosis is confirmed with clinical and radiological examination. The relevant clinical deformities are documented and a prediction of leg length discrepancy is made.21 Surgical options are then described based on the clinical findings following an algorithm agreed with the Limb Rehabilitation Unit.22 In those children with severe deformity, the information provided includes the timing, number of surgical interventions and the risk of complications for both amputation and limb reconstruction techniques, thus allowing parents to make an informed decision on treatment.
All patients for consideration of amputation are then seen in the Limb Rehabilitation department for further counselling on the functional expectation with both non-surgical extension prosthesis and amputation, including the different prostheses available. Once a decision for amputation is made, our preference is to perform a Syme disarticulation using a similar technique as previously published.23,24 The fibula anlage is simply divided at the level of the ankle joint and the tibial anterior bow (kyphus) is not primarily corrected.
The study was approved by the research and development department as a service review of patients attending the prosthetic rehabilitation unit. From an electronic patient database, 176 active case records were listed as having congenital limb deficiency. Thirty-eight patients with total absence of the fibula (Achterman and Kalamchi type II,4 International Standards Organisation longitudinal deficiency, fibula totally absent with associated absence of rays25) were identified. Six patients had undergone limb lengthening and were excluded from analysis.
The remaining 32 patients were divided into two groups: nine patients with nine affected extremities were treated with extension prostheses and 23 with 25 affected extremities underwent amputation. Validated outcome measures were used to look at comfort, function and prosthetic use. These included the SIGAM (Special Interest Group in Amputee Medicine) scale for grading mobility in a patient with a lower-limb amputation,26 and the ‘K activity levels’.27
The SIGAM scale describes the level of mobility achieved using a lower-limb prosthesis with a focus on walking distance and need for walking aids (Table 1), whereas the K level is a rating system used by Medicare to indicate an individual’s ability or potential to ambulate and navigate their environment with a focus on quality of gait (Table 2). Quality of life was assessed using the PedsQL quality of life inventory questionnaire, evaluating physical, emotional, social and school function, which is applicable for children aged two years and older and into adulthood.28 The patients were also asked to score lower-limb pain from zero to ten, zero being no pain and ten severe pain.
Table 1.
The Special Interest Group in Amputee Medicine (SIGAM) scale for grading mobility in a patient with a lower-limb amputation
| Grade | Clinical finding |
|---|---|
| A | Does not wear a limb prosthesis or Only wears a limb prosthesis for cosmetic purposes |
| B | Only wears a limb prosthesis for transfers or to assist nursing or only walks indoors or needs assistance from someone else |
| C | Only walks on level ground ≤ 50 m with or without the use of a walking aid |
| D | Walks on level ground outdoors in good weather ≥ 50 m with or without the use of a walking aid |
| E | Walks > 50 m independent of walking aid (may use walking aid to improve confidence or in inclement weather or for difficult terrain) |
| F | Normal or near normal gait |
Grades C and D can be subgraded based on the walking aids: a) frame; b) 2 crutches or sticks; c) 1 crutch or stick; d) none.
Table 2.
Outcome measures in lower-limb prosthetics - K-Level description
| Level | Description |
|---|---|
| K0 | No ability or potential to ambulate or transfer safely with or without assistance and a prosthesis does not enhance their quality of life or mobility. |
| K1 | Ability or potential to use a prosthesis for transfers or ambulation on level surfaces at fixed cadence - a typical limited or unlimited household ambulator. |
| K2 | Ability or potential for ambulation with the ability to traverse low-level environmental barriers such as curbs, stairs or uneven surfaces - a typical community ambulator. |
| K3 | Ability or potential for ambulation with variable cadence: a typical community ambulator with the ability to traverse most environmental barriers and may have vocational, therapeutic or exercise activity that demands prosthetic use beyond simple locomotion. |
| K4 | Ability or potential for prosthetic ambulation that exceeds basic ambulation skills, exhibiting high impact, stress or energy levels - typical of the prosthetic demands of the child, active adult or athlete |
The amputation group was further assessed by time of amputation into early, less than three years of age, and late.
Statistical analysis was undertaken using SPSS (v23; SPSS Inc., USA); Mann-Whitney U-tests were undertaken to compare the outcome of each group due to non-parametric data.
Results
Extension prostheses as primary treatment
Nine patients had been treated with extension prostheses alone (Table 3). Two male and seven female patients underwent assessment at a median age of 23.5 years (interquartile range (IQR) 50.25 years). Two female patients underwent lower-limb surgery at the age of two years to aid prosthetic fitting: one osteotomy to correct the tibial kyphus and one ankle fusion to position the foot in equinus. Both these patients currently suffer with significant foot pain and are awaiting amputation surgery to reduce pain and improve prosthetic fitting. One patient aged 69 years with an isolated unilateral fibula absence had historically not been offered amputation. Three patients with multiple congenital deformities including proximal femoral focal deficiency (PFFD) were also not offered amputation. Three patients declined amputation based on ethnic beliefs.
Table 3.
Patient demographics
| Extension prostheses | Surgical amputation | |||
|---|---|---|---|---|
| n = 9 | n = 25 in 23 patients | |||
| Gender | M 2 : F 7 | M 16 : 7 F | ||
| Median age at review (yrs) | 23.5 (IQR 50.25) | 8 (IQR 12) | ||
| Median follow-up (yrs) | 5.5 | 3.3 | ||
| Treatment | Amputation not offered | 4 | Early Symes | 19* |
| Amputation refused | 3 | Late Symes | 4 | |
| Additional surgery | 2 | Boyd | 1* | |
| Trans-tibial (late) | 1 | |||
| Rays in foot (n) | ||||
| Unknown | 1 | |||
| 1 | 2 | |||
| 2 | 1 | 7 | ||
| 3 | 3 | 10 | ||
| 4 | 4 | 2 | ||
| 5 | 1 | 3 |
One child at the time of Boyd amputation underwent a tibial osteotomy to correct the kyphus, the second child in the early Syme group underwent kyphus correction aged two years
Amputation as primary treatment
A total of 25 amputations were performed in 23 patients (Table 3). There was a significant difference in the age of referral and initial assessment at the limb rehabilitation unit in comparison to those patients who underwent prosthetic treatment only (median age 10 months vs 22 years, p = 0.01). They were predominantly male (n = 16) with a median age at assessment of eight years (IQR 12 years).
The 19 Syme amputations in 18 patients were performed early at a mean age of 15 months (7 to 36) following referral to our unit under the age of three years. The mean leg length discrepancy at presentation was 5.46 cm (4.6 to 6.1) with a predicted discrepancy at skeletal maturity of 19.9 cm (16 to 25). Other associated deformities included two cases of PFFD and seven cases with shortening of the femur. Six patients also had significant genu valgum.
In one girl, a Boyd amputation was performed at another institution at the age of 15 months with a concomitant osteotomy to correct the tibial kyphus: she had associated shortening of the femur and a genu valgum deformity and was referred to the limb rehabilitation unit for long-term follow-up.The late amputation group included four children (two males, two females) who presented to the unit at a mean age of 6.6 years (4 to 13). There were two cases with associated femoral shortening, one of which also had genu valgum. Four Syme amputations were performed in three children. A trans-tibial amputation was performed in the remaining 13-year-old boy with a painful two ray foot fixed in equino-valgus with a skeletally mature tibia. The decision was based on the remaining stump being an optimal length for the below-knee prosthesis and low risk for further overgrowth complications.
Further surgery and complications
One patient in the early Syme group had a residual remnant of the calcaneal apophysis which grew in size over time and eventually required surgical excision due to socket irritation and pain at the age of seven (Fig. 1). One patient from the same group has undergone a corrective tibial osteotomy due to a significant kyphus of 45° and difficulty with prosthetic fitting at the age of two years.
Fig. 1.
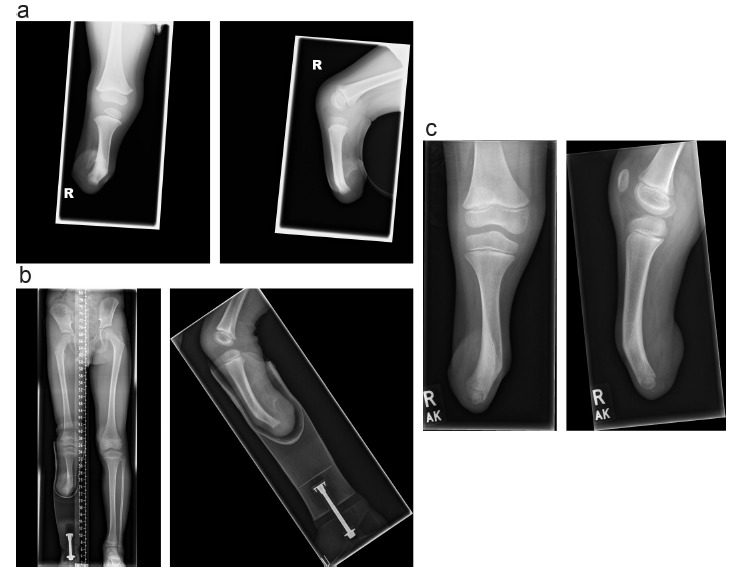
(a) Remnant of calcaneal apophysis. (b) Pain when wearing prosthesis over tibial kyphus and remnant. (c) Post excision.
The single Boyd amputation failed due to pain and difficulty with prosthetic fitting over the lateral position of the calcaneum. This was converted to a Syme type disarticulation and the genu valgum deformity corrected with guided growth using an ‘8’ plate (Orthofix, TX, USA; Fig. 2). There were four stump complications. Two patients from the early Syme group presented with recurrent folliculitis and one patient developed a post-operative infection which responded to oral antibiotics. One patient who underwent late Syme amputation mobilised full weight-bearing on the unprotected stump following hospital discharge and presented with a wound breakdown at ten days following surgery. This was treated conservatively and healed by secondary intention with no further complications.
Fig. 2.
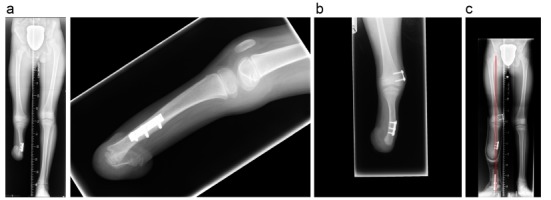
(a) Post Boyd amputation, difficulty with prosthetic fitting and genu valgum. (b) Post calcaneum excision and insertion of eight plate for guided growth. (c) Mechanical axis correction prior to plate removal.
Outcome
There was a significantly higher K activity level and lower pain scores in the amputation group compared with those patients who utilised an extension prosthesis (p = 0.02 and p = 0.012). The higher K scores (mean 4 vs 2) and lower pain scores in the amputation group would allow patients to take part in high-impact activity and if maintained into adulthood would compare favourably with the level of community ambulation only currently undertaken by the extension prosthesis group.
There was no significant difference in the SIGAM scale between the extension prosthesis group and the amputation group. Similarly, for all domains of the PedsQI there was no significant difference between the groups but all the scores were higher with better results in the amputation group (Fig. 3). There were two cases of severe bullying at school in the early Syme group. There was no difference in any of the domains including the psychological scores between those who underwent an early or late amputation.
Fig. 3.
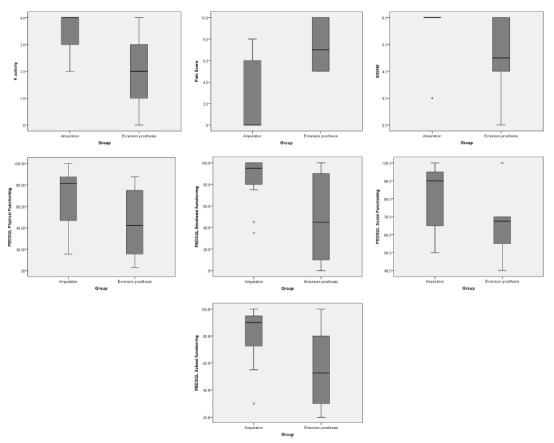
Outcome scores for amputation and extension prosthesis groups.
Discussion
The management of children who present with congenital absence of the fibula remains a dilemma both for clinicians and parents. The difficulty in deciding between no surgery, amputation or limb reconstruction remains, and we believe that an understanding of functional outcome will aid in this process. It is clear from the literature that all options achieve reasonable or good function and therefore the ultimate decision will come down to surgical preference and parental understanding of the risks and benefits of the treatment. Increasing acceptance of disability in society and technical developments in modern prosthetics are also likely to be influencing factors.
This study confirms the excellent early functional results achieved following amputation surgery in childhood. An understanding of the natural history of a progressive limb length discrepancy21,29,30 and the difficulty in achieving a functional foot are the influential factors that have guided our decision-making process. The actual leg length discrepancy that merits amputation remains a debate. Before limb lengthening was an accepted routine procedure, 3 inches (~7.5 cm) was an acceptable limit.7 A discrepancy of 20 cm has been chosen, by our unit, based on the probability that more than three episodes of lengthening surgery, with or without epiphysiodesis of the longer leg, would be required to achieve limb equalisation. From our study, some patients were predicted to have a leg length discrepancy less than 20 cm (but all were greater than 16 cm) and 14 of the 25 amputated feet had at least three rays present. Despite this, following consultation their parents still opted for amputation influenced by the number of operations required and risks associated with limb reconstruction. Birch et al6 proposed a simple classification based on the clinical status of the foot combined with the magnitude of the leg length discrepancy. They reported that limb reconstruction with foot preservation was undertaken in the majority of patients with a foot of three rays or more. They did emphasise, however, that this observation should be seen as a guideline.
We believe that, in this particular condition, a Syme amputation is technically easier to perform than a Boyd amputation. Both have been shown to have good long-term results.7,8,11,23,24,31-33 In principle, a disarticulation prevents complications such as stump overgrowth and potentially produces an end-bearing stump that can bear weight. At skeletal maturity, the expectant overall length of the tibia, however, will result in the adult having a limb segment length similar to the optimum length of a trans-tibial amputation. This stump will not be expected to be used as an end-bearing stump and therefore the position of the heel-pad is not an essential requirement. The calcaneum is often fixed posteriorly and therefore placing it below the tibia is difficult. Choi et al preferred a Boyd amputation as they felt it was easier to preserve the weight-bearing heelpad.9 They did, however, concede that if the heel is fixed in equinus, and technically it is not feasible to centre the calcaneus under the tibia, then a Syme amputation should be performed. In our study, the one case that underwent a Boyd amputation developed difficulties with prosthetic fitting and required revision to a Syme amputation. We accept that conclusions over the choice of amputation cannot be made from this one example.
The bowing of the tibia also raises debate on management. Only one osteotomy was performed in our study for an angulation of 45° which caused difficulty with prosthetic fitting. This was similar to the findings of Farmer and Laurin who performed a corrective osteotomy on two occasions out of 32 limbs.7 In our opinion, the kyphus aids suspension of the prosthesis without compromising the shape of the prosthesis or cosmeses. There were no cases of skin irritation or abrasions over the apex of the deformity as previously reported.23 We therefore do not recommend correction of the tibial deformity at the time of amputation. We do perform a simple division of the fibrous anlage distally if present.
Performing amputation early may offer psychological advantages as the foot does not become incorporated into the body image of the child.5 Our study demonstrated no differences in outcome scores between those children who underwent ablation early compared with those aged older than three years: the small numbers in the late group however limit our ability to extrapolate on this. The psychological impact remains unpredictable and two of the early amputation group experienced bullying at school as a direct consequence of their condition.
Significantly higher K-activity and lower pain scores were observed in the amputation group in comparison with those treated with an extension prosthesis. There were no significant differences in the SIGAM scale or the PedsQl domains although the findings demonstrated better scores following amputation. One of the major weaknesses of this study is the difference in patient numbers, age and follow-up of the two groups. The lower outcome measures in the extension prosthesis group could be explained by the higher number of associated lower-limb congenital deformities seen in the patients in this group which could limit activity (one-third in the extension prosthesis group had PFFD compared with two out of 23 in the amputation group). The amputation group is much younger with a short follow-up period preventing us from reporting and comparing the long-term effects. Long-term results have already been demonstrated following childhood amputation6 but we must remain cautious that the amputation scores will remain excellent for the long-term future.
In conclusion, we have demonstrated excellent functional results following amputation with type II fibula deficiency associated with significant leg length discrepancy and foot deformity. We recommend thorough discussion with parents highlighting the natural history and treatment options for amputation versus limb reconstruction procedures. In those cases where surgical intervention is not agreed upon, we have shown reasonable long-term results with adaptable extension prosthesis but functional outcome scores were slightly lower in comparison to the amputation group.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. No funding was received for this study.
References
- 1.Froster UG, Baird PA. Congenital defects of lower limbs and associated malformations: a population based study. Am J Med Genet 1993;45:60–64. [DOI] [PubMed] [Google Scholar]
- 2.Rogala EJ, Wynne-Davies R, Littlejohn A, Gormley J. Congenital limb anomalies: frequency and aetiological factors. Data from the Edinburgh Register of the Newborn (1964–68). J Med Genet 1974;11:221-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coventry MB, Johnson EW Jr. Congenital absence of the fibula. J Bone Joint Surg [Am] 1952;34 A:941–955. [PubMed] [Google Scholar]
- 4.Achterman C, Kalamchi A.. Congenital deficiency of the fibula. J Bone Joint Surg [Br] 1979;61-B:133–137. [DOI] [PubMed] [Google Scholar]
- 5.Letts M, Vincent N. Congenital longitudinal deficiency of the fibula (fibular hemimelia). Parental refusal of amputation. Clin Orthop Relat Res 1993;287:160–166. [PubMed] [Google Scholar]
- 6.Birch JG, Lincoln TL, Mack PW, Birch CM. Congenital fibular deficiency: a review of thirty years’ experience at one institution and a proposed classification system based on clinical deformity. J Bone Joint Surg [Am] 2011;93-A:1144–1151. [DOI] [PubMed] [Google Scholar]
- 7.Farmer AW, Laurin CA. Congenital absence of the fibula. J Bone Joint Surg [Am] 1960;42-A:1–12. [PubMed] [Google Scholar]
- 8.Kruger LM, Talbott RD. Amputation and prosthesis as definitive treatment in congenital absence of the fibula. J Bone Joint Surg [Am] 1961;43-A:625–642. [PubMed] [Google Scholar]
- 9.Choi IH, Kumar SJ, Bowen JR. Amputation or limb-lengthening for partial or total absence of the fibula. J Bone Joint Surg [Am] 1990;72-A:1391–1399. [PubMed] [Google Scholar]
- 10.Naudie D, Hamdy RC, Fassier F, Morin B, Duhaime M. Management of fibular hemimelia. Amputation or limb lengthening. J Bone Joint Surg 1997;79-B:58–65. [DOI] [PubMed] [Google Scholar]
- 11.Birch JG, Walsh SJ, Small JM, et al. Syme amputation for the treatment of fibular deficiency. An evaluation of long-term physical and psychological functional status. J Bone Joint Surg [Am] 1999;81-A:1511–1518. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy JJ, Glancy GL, Chnag FM, Eilert RE. Fibular hemimelia: comparison of outcome measurements after amputation and lengthening. J Bone Joint Surg [Am] 2000;82-A:1732–1735. [DOI] [PubMed] [Google Scholar]
- 13.Walker JL, Knapp D, Minter C, et al. Adult outcomes following amputation or lengthening for fibular deficiency. J Bone Joint Surg [Am] 2009;91-A: 797-804. [DOI] [PubMed] [Google Scholar]
- 14.Miller LS, Bell DF. Management of congenital fibular deficiency by Ilizarov technique. J Pediatr Orthop 1992;12:651–657. [PubMed] [Google Scholar]
- 15.Gibbons PJ, Bradish CF. Fibular hemimelia: a preliminary report on management of the severe abnormality. J Pediatr Orthop B 1996;5:20–26. [PubMed] [Google Scholar]
- 16.Cheng JC, Cheung KW, Ng BK. Severe progressive deformities after limb lengthening in type-II fibular hemimelia. J Bone Joint Surg [Br] 1998;80-B:772–776. [DOI] [PubMed] [Google Scholar]
- 17.Zarzycki D, Jasiewicz B, Kacki W, et al. Limb lengthening in fibular hemimelia type II: can it be an alternative to amputation? J Pediatr Orthop B 2006;15: 147-153. [DOI] [PubMed] [Google Scholar]
- 18.El-Sayed MM, Correll J, Pohlig K. Limb sparing reconstructive surgery and Ilizarov lengthening in fibular hemimelia of Achterman-Kalamchi type II patients. J Pediatr Orthop B 2010;19:55–60. [DOI] [PubMed] [Google Scholar]
- 19.Catagni MA, Radwan M, Lovisetti L, Guerreschi F, Elmoghazy NA. Limb lengthening and deformity correction by the Ilizarov technique in type III fibular hemimelia: an alternative to amputation. Clin Orthop Relat Res 2011;469:1175–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oberc A, Sułko J. Fibular hemimelia - diagnostic management, principles, and results of treatment. J Pediatr Orthop B 2013;22:450–456. [DOI] [PubMed] [Google Scholar]
- 21.Paley D, Bhave A, Herzenberg JE, Bowen JR. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg [Am] 2000;82-A:1432–1446. [DOI] [PubMed] [Google Scholar]
- 22.Calder P, Hanspal RS. Management of the limb deficient child. In: Bulstrode C. ed.Oxford textbook of trauma and orthopaedics. 2nd ed. Oxford: Oxford University Press; 2011;13.14:1532–1540.[[bibmisc]] [Google Scholar]
- 23.Wood WL, Zlotsky N, Westin GW. Congenital absence of the fibula. Treatment by Syme Amputation – indication and technique. J Bone Joint Surg [Am] 1965;47-A:1159–1169. [PubMed] [Google Scholar]
- 24.Anderson L, Westin GW, Oppenheim WL.. Syme amputation in children: indications, results, and long-term follow-up. J Pediatr Orthop 1984;4:550–554. [PubMed] [Google Scholar]
- 25.Day HJ. The ISO/ISPO classification of congenital limb deficiency. Prosthet Orthot Int 1991;15:67–69. [DOI] [PubMed] [Google Scholar]
- 26.Ryall NH, Eyres SB, Neumann VC, Bhakta BB, Tennant A. The SIGAM mobility grades: a new population-specific measure for lower limb amputees. Disabil Rehabil 2003;25:833–844. [DOI] [PubMed] [Google Scholar]
- 27.Gailey RS, Roach KE, Applegate EB, et al. The amputee mobility predictor: an instrument to assess determinants of the lower-limb amputee ability to ambulate. Arch Phys Med Rehabil 2002;83:613–627. [DOI] [PubMed] [Google Scholar]
- 28.Varni JW, Limbers CA. The pediatric quality of life inventory: measuring pediatric health-related quality of life from the perspective of children and their parents. Pediatr Clin North Am 2009;56:843–863. [DOI] [PubMed] [Google Scholar]
- 29.Amstutz HC. Natural history and treatment of congenital absence of the fibula. J Bone Joint Surg [Am] 1972;54-A:1349. [Google Scholar]
- 30.Hootnick D, Boyd NA, Fixsen JA, Lloyd-Roberts GC. The natural history and management of congenital short tibia with dysplasia or absence of the fibula. A preliminary report. J Bone Joint Surg [Br] 1977;59-B:267–271. [DOI] [PubMed] [Google Scholar]
- 31.Herring JA, Barnhill B, Gaffney C. Syme amputation. An evaluation of the physical and psychological function in young patients. J Bone Joint Surg [Am] 1986;68-A:573–578. [PubMed] [Google Scholar]
- 32.Fergusson CM, Morrison JD, Kenwright J. Leg-length inequality in children treated by Syme’s amputation. J Bone Joint Surg [Br] 1987;69-B:433–436. [DOI] [PubMed] [Google Scholar]
- 33.Epps CH. Jr, Schneider PL. Treatment of hemimelias of the lower extremity. Long-term results. J Bone Joint Surg [Am] 1989;71-A:273–277. [PubMed] [Google Scholar]
- 34.Thompson TC, Straub LR, Arnold WD. Congenital absence of the fibula. J Bone Joint Surg [Am] 1957;39-A:1229–1237. [PubMed] [Google Scholar]


