Abstract
Background
The Vascular Quality Initiative Varicose Vein Registry (VQI VVR) represents a patient-centered database launched in January 2015. Previous work describing overall trends and outcomes of varicose vein procedures across the United States demonstrates a benefit from these procedures. The existing gaps in evidence to support current and future Medicare coverage of varicose vein procedures necessitate further description of clinical outcomes in patients ≥ 65 years old compared to the < 65 year old population.
Methods
This study analyzed prospectively captured anatomic, procedural, and outcome data for all patients in a national cohort of all VQI VVR-participating centers. The VQI VVR database was queried for all patients undergoing varicose vein procedures between January 2015 and July 2016. Pre-procedural and post-procedural CEAP classification, venous clinical severity score (VCSS), and patient reported outcomes (PROs) were compared between patients < 65 and ≥ 65 years old. Univariate descriptive statistics of demographic and procedural data were performed. Student’s t tests were then performed on change in CEAP classification, VCSS score and PROs (heaviness, achiness, throbbing, swelling, itching, appearance and impact on work) for each group.
Results
There were 4,841 varicose vein procedures performed from January 2015 to May 2016. There were 3,441 procedures performed in 2,691 patients (3631 limbs) in the < 65 years old group and 1,400 procedures performed in 1,068 patients (1467 limbs) in the ≥ 65 years old group. Truncal veins alone were the most common veins treated in both groups. The majority of patients were white and female in both groups. Most of the demographic characteristics were clinically similar, (although statistically different), in both groups with the exception of a higher BMI is the < 65 group and a history of bilateral varicose vein treatment, and anticoagulation being more common among patients ≥ 65. Patients in both groups experience statistically significant improvement in VCSS, PROs and CEAP. There was no difference in overall complications between age groups.
Conclusion
All patients demonstrated an associated improvement in both clinical outcomes (CEAP, VCSS), and PROs. There was no significant difference in the improvement in CEAP and VCSS between patients less than and greater than 65 years old, although the younger population reported greater improvement in PROs. Given these findings, patients older than 65 appear to benefit from varicose vein procedures and should not be denied interventions on their varicose veins and venous insufficiency based only on their age.
Introduction
Varicose veins are estimated to affect up to 30% of Americans in the United States, and up to 10% of those patients develop skin changes.1–5 While varicose veins are very common, they are often overlooked by providers due to an under appreciation of the associated morbidity. Nonetheless, venous disease is associated with significant functional limitations and decreased health-related quality of life.6 Despite national SVS/AVF guidelines on treatment recommendation for varicose veins, there is currently a wide variation of interventions for varicose veins7. The Vascular Quality Initiative Varicose Vein Registry (VQI VVR) was developed with an incentive to query patient outcomes of various venous procedures and facilitate physician decision making in developing a treatment strategy with patients for optimal vein care.
Initial data from the VQI VVR suggests that despite the wide variation in clinical practice and physician preference, there is consistent benefit to varicose vein procedures.7 Overall, patients experience improved Clinical, Etiology, Anatomy and Pathophysiology (CEAP) class, Venous Clinical Severity Score (VCSS), and Patient Reported Outcomes (PROs), suggesting that these procedures be an important tool for providers in the treatment of varicose veins.7–9 However, there is a paucity of data describing age related benefit to varicose vein procedures despite overwhelming evidence to suggest the prevalence of varicose veins increases with age.3, 4
Presently, Medicare reimburses varicose vein procedures only after a period of conservative management.10 The appropriateness of this requirement is currently a topic of significant debate, as this is contrary to SVS-AVF evidence based guidelines (1B), which recommend against compression therapy as primary treatment of symptomatic varicose veins.1 The potential exists that Medicare aged patients will not be covered at all. This issue was recently discussed at a Medicare Evidence Development and Coverage Advisory Committee (MEDCAC) meeting.10 To better inform these decisions; it is imperative to explore the outcomes of varicose vein procedures in older patients. Our objective was to investigate clinical outcomes based on age, those ≥ 65 years of age compared to those < 65 years old in regards to (1) CEAP class, (2) Venous clinical severity score (VCSS), (3) patient reported outcomes (PROs) and (4) overall complication rates. Our hypothesis is that patients ≥ 65 years of age benefit to the same extent as the patients < 65 years old in clinical outcomes without higher complication rates.
Methods
Data source and data capture
The Vascular Quality Initiative Varicose Vein Registry (VQI VVR) is one of the 12 registries under the umbrella of the Vascular Quality Initiative (VQI). This registry started in January 2015 and currently has 24 participating centers within 13 regions across 46 states and Ontario. This registry includes all superficial varicose vein procedures for ≥ C2 disease and excludes the treatment of deep veins, veins treated for trauma and superficial veins in patients with C0–C1 disease. Once a center agrees to participate, every consecutive superficial varicose vein procedure is captured. Either the physician who performs the procedure or a designated trained individual for that center completes the data entry. Each data entry has a preoperative assessment, procedure related assessment which includes the assessment of systemic complications as well as whether or not a patient requires hospitalization after the procedure, and post-procedural follow up at two time points, early (0–3 months) and late (>3 months). The follow up then determines if the patient is either discharged or returns to clinic for an additional evaluation of other varicose vein procedures.
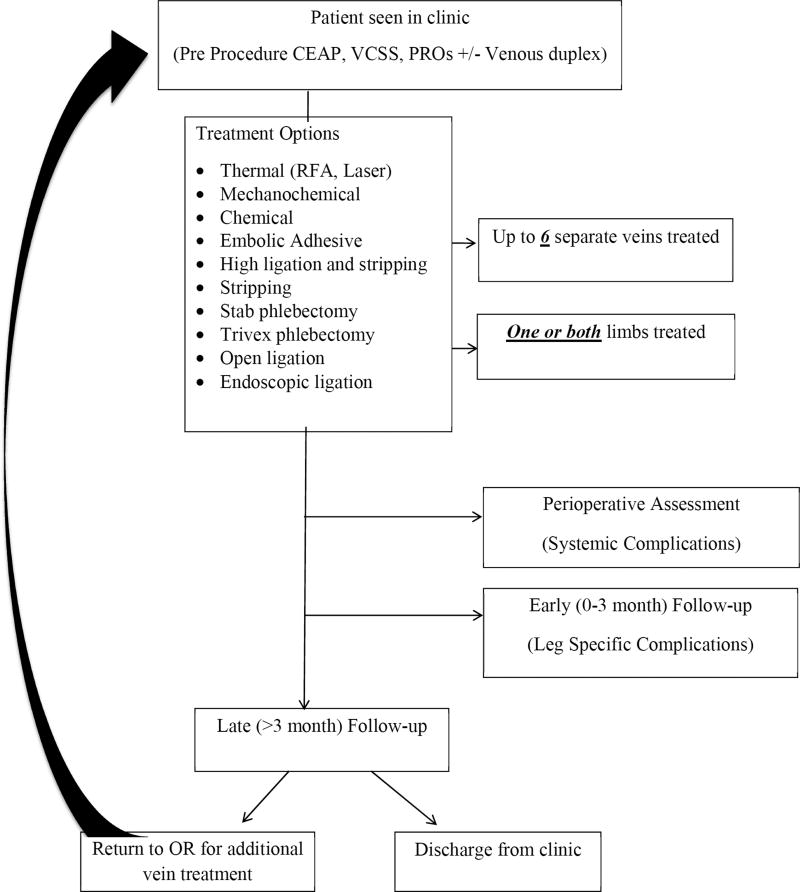
The preoperative assessment includes the recording of a pre-procedure Clinical Etiology Anatomy and Pathophysiology (CEAP) class, Venous Clinical Severity Score (VCSS), and Patient Reported Outcomes (PRO). At this time if a preoperative ultrasound study is performed, this is also recorded. Following the preoperative assessment, the patient proceeds to the operating or procedure room for the varicose vein procedure. During the isolated varicose vein procedure, a patient can have up to 6 veins treated in either one or both limbs. Procedures performed on each vein are recorded as either ablation or surgery. We define ablation as “minimally invasive” procedures and include radiofrequency ablation (RFA), laser ablation, mechanicochemical ablation, chemical ablation (by way of sclerosing agents) and embolic adhesive. Within the VQI VVR, surgery is defined as high ligation and stripping, stripping, stab phlebectomy, trivex phlebectomy, open ligation and endoscopic ligation. During the periprocedural period, systemic complications are assessed and include mild or severe allergic reactions, migraine, visual disturbance, cough/chest tightness, systemic infection, PE, TIA, stroke, and death. Of note, systemic complications are not assessed again at any point in the follow up period. Finally, the patient is then seen in clinic for follow up at two time points, early (0–3 months) and late (>3 months) during which time post-procedure CEAP class, VCSS and PROs are assessed (Figure 1). The post-procedure CEAP class, VCSS and PROs scores that are captured in the VQI VVR dataset are the values recorded at the most recent follow-up.
Figure 1.
Flow chart demonstrating patient flow in the VQI VVR.
Procedure selection
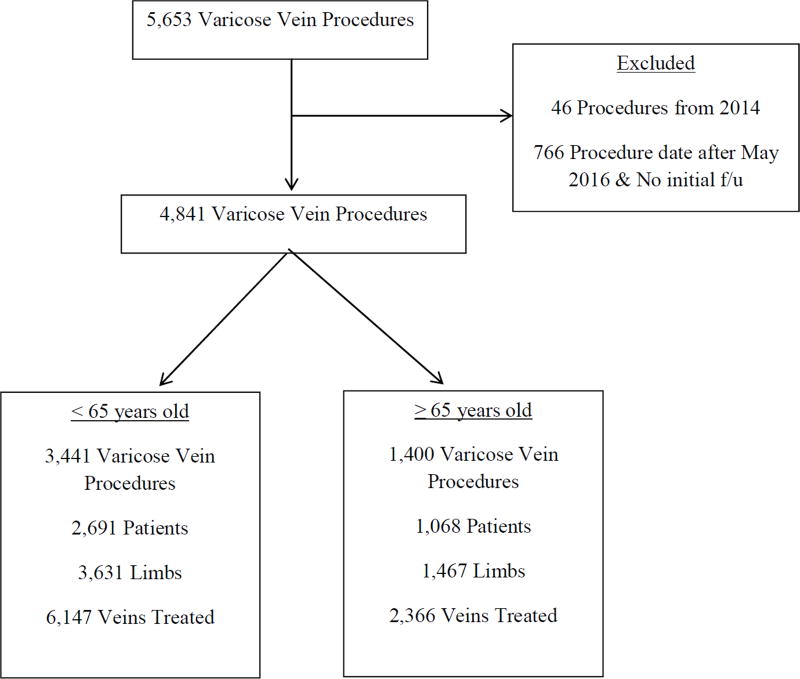
The use of the VQI VVR was granted after submission and approval of the scientific protocol through the national VQI application process and through a local standard institutional review board (IRB) approval. All patient information was de-identified and did not require informed consent. Once access was granted, the dataset of all procedures in the VQI VVR from January 2015 to August 2016 was made available. On initial review of the database, we found 46 procedures from 2014. Given these were likely “back logged” as the VVR VQI was initiated in January 2015 we excluded these procedures. We also excluded all procedures that occurred after May 2016 and did not have an early follow-up documented. This exclusion avoided case capture appearing to be missing follow up, when in reality insufficient time had passed to allow for early follow up (0–3 months) after the procedure (Figure 2).
Figure 2.
Flow diagram of procedure breakdown in each age group.
Outcomes
Our primary endpoints were CEAP class improvement, which we defined as moving from a higher C class to a lower C class, VCSS and PROs score improvement. Our secondary endpoints were systemic and leg specific complication rates as well as overall mean improvement between the two age groups (< 65 years old and ≥ 65 years old). All outcomes are assessed by thorough chart review of operative, progress, and clinic notes by the physician or the designated trained clinical data abstractor. VCSS scores are broken into 10 different components that include: pain, varicose veins, edema, pigmentation, inflammation, induration, active ulcers, ulcer duration, ulcer size, and use of compression.11 Each component is scored on a scale of 0–3 and the total VCSS is determined by adding the various components. PROs scores are based off of 7 components including: heaviness, achiness, swelling, throbbing, itching, appearance and impact on work.12, 13 These are assessed on a scale 0–5 via patient survey that is given to the patient during each clinic follow up (early and late). These scores are then combined to create the overall PROs score. The VQI VVR then captures the most recent VCSS and PROs score. For the primary endpoints we only analyzed procedures that had pre and post procedure scores and excluded all procedures missing this data from the analysis. Systemic complications are recorded only in the immediate perioperative period whereas leg specific complications are only recorded at the early follow up clinic appointment. Finally, the overall mean improvement comparing both age groups used the average improvement in VCSS and PROs for both cohorts.
Statistical analysis
Statistical analysis was performed using Stata 14.0 software (StataCorp LP, College Station, TX). Univariate analysis was performed to evaluate baseline demographics and patient characteristics. The X2 was used for comparison of categorical variables. Student t-test was used for continuous variables as they were normally distributed. All primary and secondary outcomes were compared using X2. A p value of < .05 was considered statistically significant.
Results
In total there were 4,841 varicose vein procedures performed from January 2015 to May 2016. There were 3,441 procedures performed in 2,691 patients (3631 limbs) in the < 65 years old group and 1,400 procedures performed in 1,068 patients (1467 limbs) in the ≥ 65 years old group. Bilateral procedures were performed in 190 patients < 65 years old and in 67 patients ≥ 65 years old. The total number of veins treated in each age group was 6,147 in the younger group compared to 2,366 veins treated in the older group (Figure 2).
Patient characteristics and clinical presentation
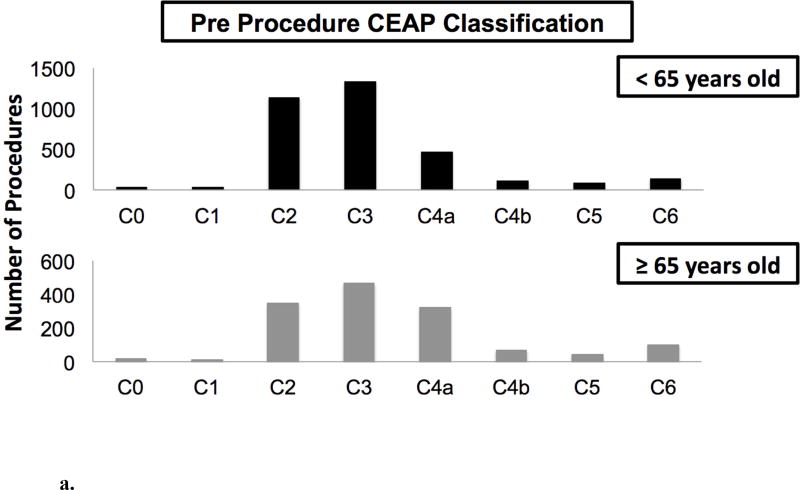
Table I examines the differences in patient demographics between both age groups. The < 65 group had a higher percentage of females and an overall higher BMI. The ≥ 65 group had a higher percentage of Caucasians, were more likely to have a history of bilateral varicose vein procedures and be on prior anticoagulation. Other patient demographics and characteristics were similar between both groups. The most common pre-procedural CEAP classification was C3 in both groups (Figure 3A). Patients < 65 years old presenting to clinic had C3 disease 40% (N=1,329) of the time, followed by C2 disease in 34.17% (N=1,135) of procedures and C4a disease in 14.09% (N=468). Patients in the ≥ 65 group presenting to clinic had 33.92% (N=466) with C3 disease, 25.40% (N=349) with C2 disease and 23.22% (N=319) with C4a disease. Only 4.09% (N=136) of procedures performed in patients < 65 had active ulceration, whereas a higher percentage, 7.13% (N=98) of procedures performed were for active ulceration in the ≥ 65 year old group.
Table I.
Demographics of patients above and below 65 years of age.
| < 65 years old (n=2691), No. (%) |
≥ 65 years old (n=1068), No. (%) |
P value | |
|---|---|---|---|
| Age, years (SD)a | 48.89 ±10.24 | 71.94 ± 5.93 | <.001 |
| Sex (female) | 1967 (73.10) | 742 (69.48) | .026 |
| Raceb | |||
| White | 2084 (77.44) | 885 (82.87) | <.001 |
| Black | 180 (6.69) | 45 (4.21) | .004 |
| Asian | 41 (1.52) | 10 (.94) | .160 |
| Other | 363 (13.49) | 126 (11.8) | .164 |
| BMI (SD)c | 30.11 ± 7.58 | 29.45 ± 6.39 | .013 |
| Prior VV treatmentd | |||
| Unilateral | 517 (19.23) | 208 (19.49) | .855 |
| Bilateral | 295 (10.97) | 142 (13.31) | .044 |
| History of DVTe | |||
| Unilateral | 140 (5.22) | 72 (6.77) | .063 |
| Bilateral | 26 (.97) | 16 (1.51) | .160 |
| Receiving Anticoagulationf | |||
| No | 2555 (95.02) | 897 (84.07) | <.001 |
| Yes - continued | 115 (4.28) | 124 (11.62) | <.001 |
| Yes - stopped perioperatively | 19 (.71) | 46 (4.31) | <.001 |
(SD) indicates continuous variables with summary measure of mean (standard deviation) and P value from Student’s t-test.
Data missing on 2 individuals.
Data missing on 8 individuals.
Data missing on 4 individuals.
Data missing on 13 individuals.
Data missing on 3 individuals. Categorical variables are summarized by No. (%), and P values are calculated from the X2 test. Anticoagulation in the VQI VVR includes: warfarin, dabigatran, rivaroxaban, unfractionated heparin, low molecular weight heparin (LMWH) or other anticoagulation and does not include aspirin.
Figure 3.
A. Number of procedures performed for each pre procedure CEAP class within each age group for all procedures (N=4,841).
B. Pre and post procedure CEAP classification in patients < 65 years old and ≥ 65 years old. Note: Only procedures with both a pre and post procedural CEAP are included (N=2,697).
Anatomic and Procedure Breakdown
The breakdown of procedures based on anatomy is described in Table II. Truncal treatment refers to treatment of axial veins and cluster treatment refers to treatment of varicose vein tributaries. The most frequent varicose vein procedure in the VVR during the time period examined was a truncal only procedure (48.9% for patients < 65, 51.6% for those patients ≥ 65), followed by truncal + cluster procedures for both age groups (39.6% of patients < 65, 36% for patients ≥ 65). The least common procedure for patients < 65 years old was a cluster + perforator procedure. The least common procedure performed on patients ≥ 65 years old was truncal + perforator procedure. Of all procedures performed, every anatomic segment was treated individually or in conjunction with treatment of truncal, cluster and perforators in each age group. In other words, all possible combinations of treatment were seen in each group. When examining the types of procedures performed between the two age groups, the patients ≥ 65 years old were treated with a significantly higher percentage of “minimally invasive” procedures compared to the patients < 65 (62.3% vs. 52.1%, p < .001).
Table II.
Breakdown of anatomic segment treated during a single procedure performed in patients < 65 years old and ≥ 65 years old.
| < 65 years old (n=3441), No. (%) |
≥ 65 years old (n=1400), No. (%) |
P value | |
|---|---|---|---|
| Truncal Only | 1682 (48.88) | 722 (51.57) | .090 |
| Cluster Only | 256 (7.44) | 120 (8.57) | .182 |
| Perforator Only | 65 (1.89) | 21 (1.50) | .353 |
| Truncal-Cluster Only | 1363 (39.61) | 504 (36) | .019 |
| Truncal-Perforator Only | 19 (.55) | 9 (.64) | .706 |
| Cluster-Perforator Only | 16 (.46) | 12 (.86) | .103 |
| Truncal-Cluster-Perforator | 40 (1.16) | 12 (.86) | .350 |
Truncal refers to treatment of axial veins. Cluster refers to treatment of varicose vein tributaries.
Outcomes
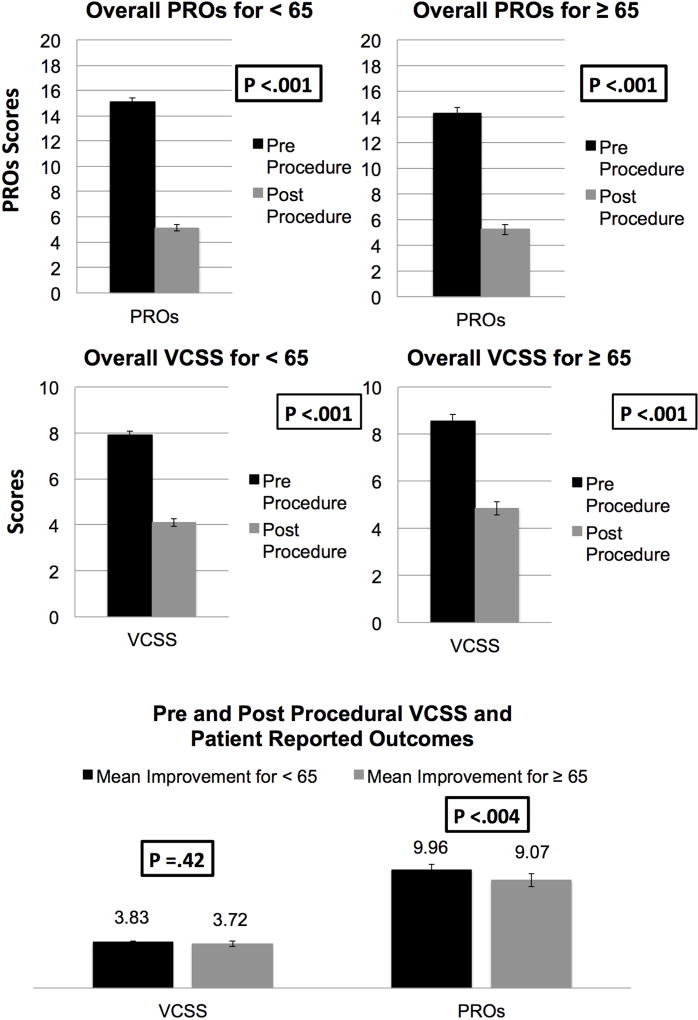
CEAP class improvement was examined for all patients that had a pre-procedural and post-procedural CEAP class assessment (Figure 3B). For all procedures performed in patients < 65 years old, 57.4% had an improvement (95% improved or stable) and for procedures performed in patients ≥ 65 years old 52% had an improvement (92% improved or stable). VCSS and PROs score improvement was also examined in all patients that had a pre and post10 procedural assessment. VCSS improvement was seen in both patients < 65 years old undergoing procedures of 3.83 (CI 3.67–3.98, p < .001) and patients ≥ 65 years old undergoing procedures of 3.72 (CI 3.46–3.98, p < .001) (Figure 4A). PROs score improvement was seen in both age groups, with a mean improvement of 9.96 (CI 9.61–10.31, p < .001) for procedures performed in < 65 and 9.07 (CI 8.58–9.56, p < .001) for procedures ≥ 65 (Figure 4B). When examining the breakdown of VCSS and PROs scores pre to post-procedural for both age groups all components had a significant improvement (Supplemental Table I and II). When comparing the mean improvement between age groups in regards to VCSS and PROs scores we found that there was no difference for VCSS (3.83 vs. 3.72, p= .42); however, with PROs scores (9.96 vs. 9.07, p < .004), the patients < 65 years old had a higher mean improvement (Figure 4C). The full breakdown of components in regards to mean improvement is described in Table III.
Figure 4.
A. Pre and post procedure VCSS in patients < 65 years old and ≥ 65 years old. Note: Only procedures with both a pre and post procedural VCSS are included (N=2,623).
B. Pre and post procedure PROs in patients < 65 years old and ≥ 65 years old. Note: Only procedures with both a pre and post procedural PROs are included (N=2,342).
C. Overall mean improvement of pre and post procedural clinical score and patient reported outcomes in patients < 65 years old compared to patients ≥ 65 years old.
Table III.
Mean improvement in VCSS and PROs with corresponding component breakdown for patients < 65 years old and ≥ 65 years old.
| Mean Improvement for < 65 |
Mean Improvement for ≥ 65 |
≥ 65 vs. < 65 P value |
|
|---|---|---|---|
| VCSS Scorea | 3.83 (p<.001*) | 3.72 (p<.001*) | .420 |
| Pain | 1.10 (p<.001*) | 1.05 (p<.001*) | .234 |
| Varicose veins | 1.24 (p<.001*) | 1.05 (p<.001*) | <.001 |
| Venous edema | .47 (p<.001*) | .51 (p<.001*) | .233 |
| Skin pigmentation | .13 (p<.001*) | .21 (p<.001*) | <.001 |
| Inflammation | .20 (p<.001*) | .24 (p<.001*) | .138 |
| Induration | .15 (p<.001*) | .19 (p<.001*) | .139 |
| Active ulcers | .03 (p<.001*) | .04 (p<.001*) | .688 |
| Ulcer duration | .04 (p<.001*) | .04 (p=.0005*) | .952 |
| Active ulcer size | .03 (p<.001*) | .05 (p=.0002*) | .330 |
| Compression therapy | .44 (p<.001*) | .33 (p<.001*) | .026 |
| PROs Scoreb | 9.96 (p<.001*) | 9.07 (p<.001*) | <.004 |
| Heaviness | 1.61 (p<.001*) | 1.37 (p<.001*) | <.001 |
| Achiness | 1.70 (p<.001*) | 1.53 (p<.001*) | .018 |
| Swelling | 1.53 (p<.001*) | 1.50 (p<.001*) | .736 |
| Throbbing | 1.44 (p<.001*) | 1.19 (p<.001*) | <.001 |
| Itching | .92 (p<.001*) | .77 (p<.001*) | .020 |
| Appearance | 1.60 (p<.001*) | 1.48 (p<.001*) | .064 |
| Impact on work/activity | 1.09 (p<.001*) | 1.18 (p<.001*) | .168 |
VCSS Data missing on 1,636 procedures in the < 65 group and 582 procedures in the ≥ 65 group.
PROs Data missing on 1,855 procedures in the < 65 group and 644 procedures in the ≥ 65 group.
P value signifies that there was significant improvement from pre procedure to post procedure VCSS and PROs scores for each age group.
Complications
Complications recorded in the VQI VVR are systemic and leg specific and are captured at different time points. Systemic complications are documented during the periprocedural period and were overall low and not statistically different for patients < 65 years of age and ≥ 65 years of age and were 0.70% and 0.79% respectively (p= .742) (Table IV). Leg specific complications are documented during the early (0–3 month) follow up appointment. Leg specific complications were also low at < 2% for each leg complication. The overall rate of any leg complication for patients < 65 years of age was 6.71% (N=101) and 6.17% (N=39) for patients ≥ 65 years of age. The most common complication for both age groups was paresthesia followed by DVT. The only leg complication that was statistically different between age groups was wound infection (.20% vs. .95%, p= .015) although this occurred extremely infrequent (Table V).
Table IV.
Systemic complications of procedures performed on patients above and below 65 years of age.
| < 65 years old (n=3441), No. (%) |
≥ 65 years old (n=1400), No. (%) |
P value | |
|---|---|---|---|
| Overall systemic complication | 24 (.70) | 11 (.79) | .742 |
| Mild allergic reaction | 4 (.12) | 1 (.07) | .660 |
| Severe allergic reaction | 1 (.03) | 0 | .524 |
| Migraine | 1 (.03) | 0 | .524 |
| Visual disturbances | 1 (.03) | 0 | .524 |
| Cough/chest tightness | 1 (.03) | 0 | .524 |
| Systemic infection | 0 | 1 (.07) | .117 |
| PE | 2 (.06) | 0 | .367 |
| TIA | 0 | 0 | -- |
| Stroke | 0 | 0 | -- |
| Death | 0 | 0 | -- |
| Other | 16 (.46) | 8 (.64) | .434 |
PE, pulmonary embolism; TIA, transient ischemic attack. Systemic complications are recorded in the perioperative period (day of procedure until discharge from the hospital or outpatient facility).
Table V.
Leg specific complications of procedures performed on patients above and below 65 years of age.
| <65 years old (n=1505), No. (%) |
65 years old (n=632), No. (%) |
P value | |
|---|---|---|---|
| Any leg complications | 101 (6.71) | 39 (6.17) | .645 |
| Bleeding requiring reintervention | 0 | 0 | -- |
| Skin blistering | 3 (.20) | 1 (.16) | .841 |
| DVT | 12 (.80) | 9 (1.42) | .180 |
| Hematoma | 8 (.53) | 2 (.32) | .506 |
| Paresthesia | 30 (1.99) | 10 (1.58) | .522 |
| Pigmentation | 10 (.66) | 3 (.47) | .607 |
| Superficial phlebitis | 11 (.73) | 1 (.16) | .106 |
| Induced ulcer | 1 (.07) | 0 | .517 |
| Wound infection | 3 (.20) | 6 (.95) | .015 |
| Proximal thrombus extension (EHIT) | 14 (.93) | 6 (.95) | .967 |
2,646 procedures did not have early follow-up. Of the 2,195 procedures that did have early follow-up, leg specific complication data missing in 58 procedures (44 from < 65 and 14 from ≥ 65). Leg specific complications are only recorded in early (0–3) follow-up. EHIT, endothermal heat induced thrombosis.
Follow-Up
Of 4,841 procedures, 45.3% (N=2,195) of procedures had early follow-up (within 3 months), 16.9% (N=820) of procedures had late follow-up and 37.7% (N=1,826) procedures were missing follow up.
Discussion
Our study addresses an important, timely question of whether or not patients ≥ 65 years of age benefit from varicose vein procedures and if the benefit is to the same extent as patients < 65 years old. This data demonstrates that not only do patients ≥ 65 years of age have improvement of clinical and patient reported outcomes, this group has just as much of a positive response as their younger counterparts in regards to VCSS. Importantly, this benefit does not come with a higher risk of complications and in fact, the older patient group had no associated increased risk of complications with the exception of wound complications. Ultimately, these results have the potential to directly impact federal policy on Medicare coverage in this vulnerable patient population.
Not only a problem of the young
Varicose veins affect approximately 23% of adults in the United States, with a mean age of 33–55 reported in the literature and affects both men and women.12, 14–16 Although many overlook the significant morbidity varicose veins cause, the prevalence increases with age and increases in severity with time.17 With all of these factors to consider, it is surprising to see such a potential gap in coverage. Thus, we set out to confirm or refute the hypothesis that older patients ≥ 65 benefit to the same extent as the patients < 65 years old in clinical outcomes without higher complication rates.
Clinical improvement and patient reported outcomes
One potential concern for treating patients ≥ 65 is the concern for associated increased risk without similar benefit seen in the younger patient population. However, our data does not support this assumption. On the contrary, in our study the procedures performed in patients ≥ 65 years of age had statistically significant improvements in VCSS (OR 3.72, CI 3.46–3.98, p < .001), and PROs (OR 9.07, CI 8.58–9.56, p < .001). When comparing the two age groups mean improvement in VCSS and PROs, we found that there was no difference for VCSS, however the younger population had a greater mean improvement in PROs. When examining potential reasons to explain this phenomenon, we broke down the PROs into the different components to see what were the largest contributors to this difference (Table III). The five components that were significant clinical contributors to the higher mean improvement in the younger population are the exact components that we believe are the main clinical factors aligning with varicose veins, which happens to be C2 in the CEAP classification. These included heaviness, achiness, throbbing, itching, and appearance. In addition, when accounting for types of procedures performed, the older age group did have a higher percentage of “minimally invasive” procedures (62.3%), which was significantly different (p value < .001) than the younger < 65 patient cohort (52.1%). The association of type of treatment on outcome is unclear and warrants further investigation. However, it is interesting to speculate that this data would indicate that older patients are more often treated for symptoms of chronic venous insufficiency (pain and swelling) and not for their varicosities while younger patients are more often treated for their branch varicosities. Additionally, this may help to explain the difference in mean improvement in VCSS component score for varicose veins before and after treatment (Table III).
Comparing complications
Overall complications were low amongst all patients and not associated with any significant difference between the two groups of patients. This finding supports the safety of the varicose vein procedures in patients ≥ 65; although it is important to note that we did find a higher percentage of “minimally invasive” procedures being performed in the older cohort. Despite this finding, current practice patterns appear to be safe and effective in pateints over the age of 65. The overall incidence of the complications seen in VQI VVR is similar to rates published in the literature.1, 14, 18, 19 The only complication that was higher within the older group was wound infection, although the rate was extremely low (<1%) and much lower than the approximate 3–6% wound infection rate seen in the literature. Although we do not have the granularity within this dataset to know specific reasons behind the wound infection, we did note that 11% of patients in the ≥ 65 group were on perioperative anticoagulation, which may be one potential reason this occurred. On the other hand, knowing that approximately 16% of elderly patients treated in our cohort, were on perioperative anticoagulation and still had a low complication rate may ease some clinicians when approached with an older patient who is on anticoagulation for a comorbid condition in their pre-procedure clinic. Another potential explanation of the increased wound infection rate in the older population could be immunosuppression secondary to comorbid conditions such as diabetes that are unfortunately not captured in the VQI VVR.
Limitations
One of the main limitations is the poor follow up within the VVR VQI with only 62.2% of procedures had follow up. This became apparent after our first look at the registry7 and has not been a unique problem with the VQI VVR as other studies have had similar problems with lost to follow up rates as high as 50%.18 We have been in the process of working with the VQI in an effort to establish quality measure metrics for the VQI VVR. Our proposal includes a number of measures: the percentage of patients with pre-procedure VCSS, the percentage of patients with a pre-procedure venous duplex assessing reflux, the percentage of perforator procedures in patients with C5 or C6 disease to ensure proper patient selection for perforator vein ablation, the percentage of patients avoiding hospital admission after varicose vein procedures, and lastly, the percentage of phlebectomy procedures that have prescribed post-procedure compression therapy. Ultimately, many of these measures aim to improve the “trackable” outcomes and reduce the number of unindicated procedures, with the goal of improving overall clinical venous care. Another limitation of the study is the potential for selection bias as this is a procedural registry only capturing patients undergoing varicose vein procedures. With the VQI VVR we do not have the true denominator of patients with venous disease that present to clinic and are treated with conservative management and never go onto have a procedure. This is potentially very important in the ≥ 65 group, as many that did not subsequently undergo a procedure could have extensive comorbidites. What we can say however is that the patients ≥ 65 that are currently being selected over the study period for varicose vein procedures are achieving significant benefit with low complication rates. Finally, VCSS and PRO scores are based on subjective components that rely on both patient and provider input and reporting that may be biased in favor of improvement following varicose vein procedures. However this subjective bias would likely occur across both patient age groups and there is no evidence to suggest this bias would differentially affect age groups.
Conclusion
In summary, all patients demonstrated an associated improvement in both clinical outcomes (CEAP, VCSS), and PROs. There was no significant difference in the improvement in CEAP and VCSS between patients less than and greater than 65 years old. Although patients < 65 years old had a statistically significant mean improvement in PROs compared to the patients ≥ 65 years old, it remains unclear whether or not this is clinically significant result. Given these findings, patients older than 65 appear to benefit from appropriate varicose vein procedures and should not be denied interventions on their varicose veins and venous insufficiency based only on their age.
Supplementary Material
Type of Research: Retrospective review of prospectively collected data of the VQI Varicose vein registry
Take Home Message: Procedures for varicose veins in 1,068 patients > 65 years of age resulted in similar improvement in CEAP class and VCSS than in 2,691 younger patients. Younger patients had more improvement in patient reported outcomes.
Recommendation: The authors recommend that Medicare beneficiaries should not be denied vein procedures based on age alone.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented in part at the 29th Annual American Venous Forum, New Orleans, LA, February 17, 2017.
Conflicts of Interest: None
References
- 1.Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, Gloviczki ML, et al. The care of patients with varicose veins and associated chronic venous diseases: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2011;53(5 Suppl):2S–48S. doi: 10.1016/j.jvs.2011.01.079. [DOI] [PubMed] [Google Scholar]
- 2.McLafferty RB, Passman MA, Caprini JA, Rooke TW, Markwell SA, Lohr JM, et al. Increasing awareness about venous disease: The American Venous Forum expands the National Venous Screening Program. J Vasc Surg. 2008;48(2):394–9. doi: 10.1016/j.jvs.2008.03.041. [DOI] [PubMed] [Google Scholar]
- 3.Beebe-Dimmer JL, Pfeifer JR, Engle JS, Schottenfeld D. The epidemiology of chronic venous insufficiency and varicose veins. Ann Epidemiol. 2005;15(3):175–84. doi: 10.1016/j.annepidem.2004.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Abelyan G, Abrahamyan L, Yenokyan G. A case-control study of risk factors of chronic venous ulceration in patients with varicose veins. Phlebology. 2017 doi: 10.1177/0268355516687677. 268355516687677. [DOI] [PubMed] [Google Scholar]
- 5.Hamdan A. Management of varicose veins and venous insufficiency. JAMA. 2012;308(24):2612–21. doi: 10.1001/jama.2012.111352. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan RM, Criqui MH, Denenberg JO, Bergan J, Fronek A. Quality of life in patients with chronic venous disease: San Diego population study. J Vasc Surg. 2003;37(5):1047–53. doi: 10.1067/mva.2003.168. [DOI] [PubMed] [Google Scholar]
- 7.Obi A. First 10-month results of the Vascular Quality Initiative Varicose Vein Registry. Journal of Vascular Surgery: Venous and Lymphatic Disorders. 2017 doi: 10.1016/j.jvsv.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Michaels JA, Campbell WB, Brazier JE, Macintyre JB, Palfreyman SJ, Ratcliffe J, et al. Randomised clinical trial, observational study and assessment of cost-effectiveness of the treatment of varicose veins (REACTIV trial) Health Technol Assess. 2006;10(13):1–196. iii–iv. doi: 10.3310/hta10130. [DOI] [PubMed] [Google Scholar]
- 9.Brittenden J, Cotton SC, Elders A, Ramsay CR, Norrie J, Burr J, et al. A randomized trial comparing treatments for varicose veins. N Engl J Med. 2014;371(13):1218–27. doi: 10.1056/NEJMoa1400781. [DOI] [PubMed] [Google Scholar]
- 10.Medicare Local Coverage Determination LCD L33454: Varicose Veins of the Lower Extremities [Google Scholar]
- 11.Vasquez MA, Rabe E, McLafferty RB, Shortell CK, Marston WA, Gillespie D, et al. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. 2010;52(5):1387–96. doi: 10.1016/j.jvs.2010.06.161. [DOI] [PubMed] [Google Scholar]
- 12.Paty J, Elash CA, Turner-Bowker DM. Content Validity for the VVSymQ(R) Instrument: A New Patient-Reported Outcome Measure for the Assessment of Varicose Veins Symptoms. Patient. 2017;10(1):51–63. doi: 10.1007/s40271-016-0183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paty J, Turner-Bowker DM, Elash CA, Wright D. The VVSymQ(R) instrument: Use of a new patient-reported outcome measure for assessment of varicose vein symptoms. Phlebology. 2016;31(7):481–8. doi: 10.1177/0268355515595193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murad MH, Coto-Yglesias F, Zumaeta-Garcia M, Elamin MB, Duggirala MK, Erwin PJ, et al. A systematic review and meta-analysis of the treatments of varicose veins. J Vasc Surg. 2011;53(5 Suppl):49S–65S. doi: 10.1016/j.jvs.2011.02.031. [DOI] [PubMed] [Google Scholar]
- 15.Beale RJ, Gough MJ. Treatment options for primary varicose veins--a review. Eur J Vasc Endovasc Surg. 2005;30(1):83–95. doi: 10.1016/j.ejvs.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 16.Siribumrungwong B, Noorit P, Wilasrusmee C, Attia J, Thakkinstian A. A systematic review and meta-analysis of randomised controlled trials comparing endovenous ablation and surgical intervention in patients with varicose vein. Eur J Vasc Endovasc Surg. 2012;44(2):214–23. doi: 10.1016/j.ejvs.2012.05.017. [DOI] [PubMed] [Google Scholar]
- 17.Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation. 2014;130(4):333–46. doi: 10.1161/CIRCULATIONAHA.113.006898. [DOI] [PubMed] [Google Scholar]
- 18.Leopardi D, Hoggan BL, Fitridge RA, Woodruff PW, Maddern GJ. Systematic review of treatments for varicose veins. Ann Vasc Surg. 2009;23(2):264–76. doi: 10.1016/j.avsg.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 19.van Rij AM, Chai J, Hill GB, Christie RA. Incidence of deep vein thrombosis after varicose vein surgery. Br J Surg. 2004;91(12):1582–5. doi: 10.1002/bjs.4701. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.