Abstract
Background
Understanding epidemiology and the factors leading to thyroid nodule diagnosis might help alter the course of the thyroid cancer epidemic.
Methods
Population based study using the Rochester Epidemiology Project database between 2003 and 2006. Patients with thyroid nodules who underwent ultrasound guided biopsy (USFNA) were included.
Results
We identified 453 patients with 520 thyroid nodules undergoing USFNA. Patients were mostly women (n: 349, 77%) with a mean age of 52(SD 17) years. The age- and sex-adjusted incidence of USFNA-thyroid nodules between 2003 and 2006 was 89 (95% CI, 80–97) per 100,000 person-years (p-y); the incidence in women was 130 (95% CI, 117–144), and for men 43 (95% CI, 35–52) per 100,000 p-y. The incidence of USFNA-thyroid nodules increased by 42%, from 68 (95% CI, 54–82) in 2003 to 97 (95% CI, 80–113) per 100,000 p-y in 2006. The group with the highest incidence was patients between 70–79 years of age, 258 per 100,000 p-y. Most USFNA-thyroid nodules were found in asymptomatic patients (n: 371, 82%) by physical examination (n: 197, 43%) or on imaging studies performed for non-thyroid issues (n: 108, 24%). Women were more likely to have nodules detected by palpation (45%), whereas imaging and physical examination contributed similarly in men (39% and 38%).
Conclusion
There is a large and rapid increase in the USFNA-thyroid nodules, particularly among women and elderly patients which mirrors the trends observed in thyroid cancer. Most thyroid nodules were found in asymptomatic patients as a result of routine physical examination or imaging.
Keywords: thyroid nodule, incidence, triggers
INTRODUCTION
There is a large reservoir of thyroid nodules; 30–60% of the adult population harbors at least one thyroid nodule. [1–3] This frequency is higher with advancing age, among females and in patients living in iodine deficient areas. [4] Conservatively, these estimates translate into ~150–180 million Americans with at least one thyroid nodule. Most of these patients will remain undiagnosed and asymptomatic. Over the last decade, however, the increased detection of this large thyroid nodule reservoir has led to a series of harmful effects on patients and on the health care system.
One of the effects of the increase in the detection of thyroid nodules is the worldwide upsurge in thyroid cancer diagnosis. In the United States, the incidence of thyroid cancer has increased from 4.9 cases per 100,000 persons in 1975 to 14.3 cases per 100,000 in 2009. [5] In South Korea, where the increase has been more pronounced, the incidence rose from 11.9 cases per 100,000 in 1999 to 120.4 cases per 100 000 per year in 2012. [6] [7] In South Korea, thyroid cancer has become the most frequently diagnosed cancer among women. [7]
Given that the majority of the new thyroid cancer lesions are small papillary thyroid cancers of indolent course with no impact on disease- specific mortality, patients doubtfully benefit from this diagnosis. [5,8] In fact, individuals carrying the thyroid cancer diagnosis struggle with the substantial financial and psychological effects of the treatment associated with this condition. For example, thyroid cancer survivors have higher rates of bankruptcy due to healthcare disruptions and costs than the general population. [9] In addition, reported quality of life of thyroid cancer survivors is similar to, or worse than, that of survivors of other types of cancer that have a worse prognosis [10]. The burden of this epidemic of thyroid cancer also impacts the health care system. In the United States, thyroid cancer care cost $1.4 billion in 2010 and will increase to $20 billion over the next 10 years. [9]
Despite the vast reservoir of thyroid nodules and their potential effects on the epidemic of thyroid cancer, little is known about the true incidence of thyroid nodules and how these nodules are initially detected. Using a population based design we examined a subset of thyroid nodules undergoing ultrasound guided fine needle aspiration (USFNA) biopsy to estimate incidence as well as to identify triggers for diagnosis. Understanding how cases are detected may help to identify strategies for reducing overdiagnosis and curbing the epidemic of thyroid cancer.
METHODS
To study the incidence of thyroid nodules and triggers of diagnosis, we used the Rochester Epidemiology Project (REP). The REP medical records linkage system was initiated to study disease epidemiology and patterns of health care among the residents of Olmsted County. This database includes patients from all medical care facilities accessed by all residents of Olmsted County, Minnesota (an estimated population in 2012 of 164,129) including the Mayo Clinic, the Olmsted Medical Center and several private practices. The REP gives investigators the ability to examine the health care of Olmsted County’s residents regardless of age, sex, ethnicity, insurance or socioeconomic status or the setting of care delivery. Therefore, it allows us to estimate the incidence of medical conditions within a community. [11] [12]
Our study was approved by the institutional review boards of the Mayo Foundation and Olmsted Medical Center. We used the REP to identify all cases of thyroid nodules that were confirmed by neck ultrasound and underwent USFNA with available cytology from pathology department records from January 1st, 2003 to December 31st, 2006. Patients with thyroid nodules not undergoing USFNA were excluded. This identification method allowed us to reliably enroll patients with a confirmed diagnosis of thyroid nodule and to determine the outcome of their work up. In addition, the results of this study are a secondary outcome of a study evaluating the long term outcome of patients with benign thyroid nodules; the selected time period allowed enough follow-up time to assess the primary outcome of interest (medical record review through October/2014). Three reviewers individually extracted from each chart: the size of the thyroid nodule that was evaluated by USFNA, the results of the cytology and demographic data, family history of thyroid cancer or neck radiation, nodularity of the gland, results from the USFNA and histology (when patients required surgery), and surgical information to allow us to classify patients as low or high risk of mortality based on MACIS score (distant Metastasis, patient Age, Completeness of resection, local Invasion, and tumor Size). [13] To identify the mechanism of detection for each patient with a thyroid nodule, reviewers followed a prespecified framework (Table 1).
Table 1.
Definition of mechanism of detection
| Asymptomatic nodule | Physical exam finding | When a thyroid nodule is found during a physical exam (thyroid palpation) of a patient without symptoms concerning for thyroid disorder. |
| Imaging finding | When a thyroid nodule is found during an imaging test requested for reasons unrelated to a thyroid disorder or symptom. | |
| Diagnostic work up | When a thyroid nodule is found during the work up of clinical symptoms or abnormal laboratory tests that could be suggestive of thyroid disease or known thyroid disease (e.g., patient with weight loss where a TSH and US are performed, patient with hyperthyroidism who has a thyroid ultrasound positive for a nodule, patients with history of previous nodule followed by US, patient with abnormal TSH that results in ordering US). | |
| Case finding | When a thyroid nodule is found on a US performed for thyroid cancer screening (e.g setting of strong family history of thyroid cancer or neck radiation) | |
| Symptomatic nodule | When a thyroid nodule is found in a symptomatic patient (e.g., neck pressure or mass, voice change, dysphagia) | |
Analytic Plan
We summarized continuous variables using means, standard deviation (SD), median and interquartile range (IQR) and categorical variables using percentages. We used two-sample t-tests and Pearson’s chi-squared tests to test hypotheses of differences between groups on continuous and categorical variables, respectively. For incidence analysis, age- and sex-adjusted incidence rates were based on direct standardization against the 2010 US white population, for the 2003–2006 cohort, with the corresponding denominators derived from annual census figures for Olmsted County, assuming that the entire population was at risk. We estimated 95% confidence intervals (CIs) assuming the Poisson distribution for number of cases.
RESULTS
We identified 453 patients with 520 thyroid nodules undergoing USFNA for at least one thyroid nodule between 2003 and 2006. Most patients harboring these nodules were women (n: 349, 77%) and the mean age at the time of USFNA was 52 years (SD, 17 years). From this cohort, 327 (72%) patients with 363 thyroid nodules had benign cytology and 136 (30%) patients underwent thyroidectomy at any point during the follow up.
Malignancy frequency
Malignancy was found histologically in 45 (9%) patients. One patient had family of thyroid cancer and one patient had history of neck radiation. Most detected thyroid cancers were papillary thyroid cancer at low risk of mortality, MACIS <6 (n: 36, 87%) including 7 micropapillary thyroid cancer. In addition, we found three papillary thyroid cancers with MACIS> 6; in one case the score was given based on the age of patient, and the two remaining cases were patients who presented with metastasis. Furthermore, we found nne medullary thyroid cancer with local metastasis, and 2 follicular thyroid cancers with no vascular invasion(considered low risk) and one Hurthle cell cancer considered low risk due to absence of invasion and presence of metastasis.
Incidence of thyroid nodules undergoing USFNA
The age- and sex–adjusted incidence of thyroid nodules between 2003 and 2006 was 89 per 100,000 persons-years (p-y) (95% CI, 80–97). The age-adjusted incidence in women was 130 per 100,000 p-y (95% CI, 117–144); while for men it was 43 per 100,000 p-y (95% CI, 35–52). The highest thyroid nodule incidence was seen in patients between 70 and 79 years of age for women and men respectively (258 and 145 per p-y), Figure 1, and for nodule size between 1 and 1.9 cm in size, 31 per 100,000 p-y (95% CI, 26–36), Figure 2. Overall the age-sex adjusted incidence increased 42%, from 68 per 100,000 p-y (95% CI, 54–82) in 2003 to 97 per 100,000 p-y (95% CI, 80–113) in 2006.
Figure 1.

Incidence of thyroid nodules undergoing USFNA in Olmsted County, Minnesota, from 2003 to 2006
Figure 2.
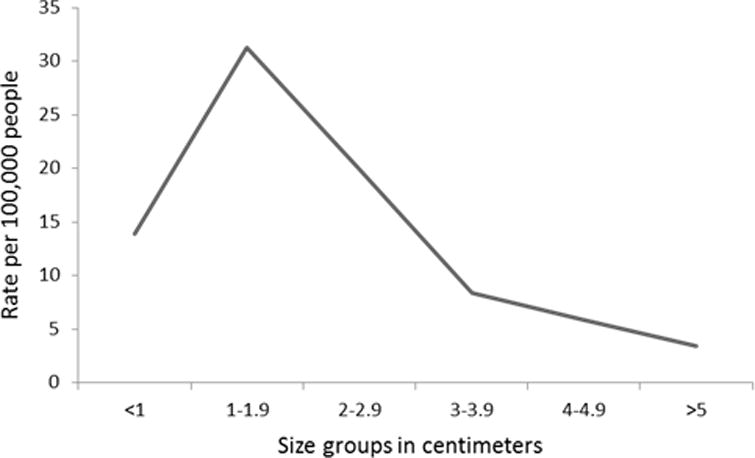
Age-adjusted incidence of thyroid nodules undergoing USFNA by size in Olmsted County, Minnesota, from 2003 to 2006
Mechanism of detection
Thyroid nodule detection was most common in asymptomatic individuals (incidentally on imaging, physical exam, diagnostic work up and case findings), 371 (82%) with a minority being found in symptomatic patients 76 (17%). In 6 patients (1%) we could not find enough documentation to classify them. Symptomatic patients underwent thyroid surgery more often and had a higher malignancy rate than asymptomatic patients with thyroid nodules, Table 2.
Table 2.
Clinical features of patients with thyroid nodule stratified by presence of symptoms
| Asymptomatic (371) | Symptomatic (76) | P value | |
|---|---|---|---|
| Age, mean in years (SD) | 52(17) | 49(16) | 0.11 |
| Females, N (%) | 278 (75) | 65(86) | 0.02 |
| Size, mean in cm (SD) | 2 (1.3) | 2.4 (1.4) | 0.10 |
| Family history of thyroid cancer, N (%) | 15(4) | 4(5) | 0.5 |
| History of neck radiation, N (%) | 10 (2) | 0(0) | 0.2 |
| Multinodularity, N (%) | 265 (73) | 56 (74) | 0.8 |
| Presence of at least one ultrasound worrisome feature, N(%) | 115 (31) | 24 (32) | 0.8 |
| Thyroidectomy N(%) | 103(28) | 29(38) | 0.06 |
| History of Hyperthyroidism | 11 (3) | 0(0) | NA |
| History of Hypothyroidism | 27(7) | 6(8) | 0.7 |
| Malignancy ratea, N(%) | 32 (9) | 13 (17) | 0.02 |
| Papillary Type, N(%)b | 28(8) | 9(12) | 0.2 |
| MACIS score, mean (SD) | 4.45 (1.1) | 5.1 (2) | 0.33 |
Using complete population as gold standard (those with surgery and with long term follow up with clinical findings of thyroid malignancy);
percentage based on total malignancy rate
The most common mechanism of detection for the asymptomatic group was routine physical examination (n: 197, 43%), followed by incidental findings on imaging tests performed for non-thyroid related reasons (n: 108, 24%). The thyroid nodules diagnosed by imaging were most commonly found on CT scan (63%) or on MRI (11%) performed for non-thyroid reasons. Thyroid nodules incidentally found on imaging were on average larger, 2.5 cm (SD 1.7) than nodules found through other mechanisms Table 3. However, within this group the mean size was skewed by the presence of three individuals with very large (7 cm and two of 10 cm in size) and asymptomatic thyroid nodules identified by chest X rays.
Table 3.
Methods of thyroid nodule detection
| Diagnostic work up (59) | Imaging finding (108) | Case finding(7) | Physician exam finding (197) | P value | |
|---|---|---|---|---|---|
| Women (N,%) | 47(80) | 62(62) | 6(86) | 158(80) | 0.01a |
| Mean size in cm (SD) | 1.7 (1) | 2.5(1.8) | 1.7 (1.2) | 2(1.1) | 0.02b |
| Malignancy | 3(5) | 9 (8) | 1(14) | 15(8) | 0.2 |
P value represents that there are less females on incidentaloma on imaging group than the other groups
P value represents a larger thyroid nodule size on incidental finding on imaging group than the other groups
When stratified by age, the most frequent mechanism of detection for most age groups was physical exam, except for patients older than 70 years. In these older individuals the frequency of incidental findings on imaging was higher than on physician exam, 34(45%) vs. 24(32%), p=0.09 Figure 3. Furthermore, the mechanism of detection was also influenced by gender. Thyroid nodules were more frequently found through neck palpation in women (158[45%]), whereas for men imaging was the most common mechanism of detection (41 [39%]) followed by neck palpation (39[38%]). Figure 4
Figure 3.

Relevant mechanism of detection by age groups
Figure 4.

Relevant mechanism of detection by gender
DISCUSSION
Thyroid nodules are common. Thyroid nodules are common; 4%–7% of adults have palpable nodules, and more than 67% have nodules on ultrasound [1–3] and up to 50% on autopsy studies. Despite the widespread nature of this condition, the incidence of thyroid nodules undergoing USFNA was unknown. In this population-based study, we found that the incidence of thyroid nodules undergoing USFNA is 88.6 per 100,000 p-y; an estimate six times higher the current incidence of thyroid cancer in the USA. Mirroring the trends observed in thyroid cancer, the majority of the new cases occurred in females, patients with thyroid nodule sizes less than 2cm, and in the elderly. [5,8]Likewise, in the short period between 2003 and 2006, we detected that the incidence of thyroid nodules undergoing USFNA increased by 43%. About 9% of these new thyroid nodules, regardless of the mechanism of detection, were found to have cancer. Thus, more thyroid nodule diagnosis equals more thyroid cancer diagnosis. Indeed, the age-adjusted incidence of thyroid cancer in the same population increased from 9 per 100,000 p-y in 2002 to 13 per 100,000 p-y in 2007. [8]
The majority of new thyroid nodules undergoing USFNA were found among asymptomatic patients. In only 17% of the patients the diagnosis was due to symptoms triggered by the nodules. While it is believed that the most important trigger of thyroid nodule detection is the increased use of imaging technology (e.g., incidental findings in CT, MRI), our findings suggest that at least for thyroid nodules undergoing USFNA the most common mechanism of detection was the palpation of the neck by a clinician. Assuming that the physical examination skills of clinicians have not changed substantially over time, one possible explanation may support this conclusion: currently, clinicians do not have to be certain about the presence of a thyroid nodule, the mere suspicion of a thyroid nodule during palpation would trigger an ultrasound of the thyroid that may confirm the palpable abnormality and will often find, incidentally, other thyroid nodules. The impact of neck palpation as a trigger of diagnosis was also suggested by a recent study conducted in the same population from 2000 to 2012 among thyroid cancers. In this study the most important mechanisms that ultimately led to the discovery of a thyroid cancer was physical examination on an asymptomatic patient (36%). [8] Finally, neck palpation predominance as a trigger among women implies important differences in health care delivery by gender. For example, high thyroid cancer frequencies among females have been attributed to more access to health care. [14] [15,16]Likewise, due to differences in body habitus thyroid glands in women, on average, are palpated with higher sensitivity for nodules than in men. [14]
Implication for practice and research
Thyroid nodule diagnosis fuels and precedes the overdiagnosis of thyroid cancer. Thus, strategies to curtail the excessive diagnosis of thyroid nodules likely will have a significant impact on reducing the increasing incidence of thyroid cancer. The American Thyroid Association guidelines have tried to address this issue, by recommending against biopsy in nodules less than 1 cm. [17] Also, to avoid the excessive use of thyroid ultrasonography as a consequence of diagnostic cascades, the Choosing Wisely Campaign - an initiative of the American Board of Internal Medicine Foundation to reduce unnecessary tests - recommends, “Don’t routinely order a thyroid ultrasound in patients with abnormal thyroid function tests if there is no palpable abnormality of the thyroid gland”. [18]. We have found that physical exam in asymptomatic patients and incidental imaging findings contribute to thyroid nodule detection. There are clearly many instances in which a presumed palpable abnormality on examination is not confirmed when ultrasound is performed, but such study may lead to the detection of other unsuspected nodules (e.g. contralateral lobe). In other cases, such palpable nodules may be confirmed on ultrasound warranting further investigation (e.g. large nodule with suspicious sonographic features). The extent to which the observed rate of nodule detection must be an accepted consequence of these practices needs to be examined carefully.
Strengths and Limitations
We conducted a population based study that allowed us to calculate the incidence of thyroid nodules undergoing USFNA and their mechanisms of detection. However, the study period from 2003 to 2006 was short, limiting our ability to analyze diagnostic trends over a longer interval. For example, we found an increase in incidence of thyroid nodules undergoing USFNA; this finding is prone to statistical uncertainty compared to estimates obtained from cohorts followed by a longer period of time. For instance, Sosa et al found in a population based analysis that the use of thyroid fine needle aspiration more than doubled during a 5 year study period (16 % annual growth). [19] Thus, further research should confirm our estimates. Likewise, given that our cohort included patients diagnosed between 2003 and 2006, our results may not reflect more current incidence rates of thyroid nodule diagnosis and mechanisms of detection. Our rationale to study this period of time was to allow a sufficient follow-up time to capture the outcomes of the work-up of all these thyroid nodules even when they did not have immediate thyroid surgery. We also followed a predefined framework to classify the mechanism of detection and were able to assign a category for the majority of our sample (99%). Additionally, our estimates are based on thyroid nodules undergoing USFNA evaluation; while this strategy allows us to identify accurately patients with thyroid nodules in this population, it provides results that underestimate the true incidence of thyroid nodules, because only an unknown percentage of thyroid nodules required USFNA. Similarly, the exact criteria for whether to conduct or not a USFNA evaluation was not extracted, and thus, it is possible that the estimates here are reflection of selected patients presenting with one or more features that raised clinicians and patients concerns.Furthermore, the mechanism of detection for thyroid nodules not undergoing USFNA evaluation may be different that those described here. Finally, the use of the REP, a less ethnically diverse population with high access to health care, may raise concerns over the generalizability of these findings. Thus, it is possible that the incidence of thyroid nodules and their mechanism of detection may vary depending on the source of data. [20] Other studies are needed to confirm our findings.
Conclusions
There is a large and rapid increase in the incidence of thyroid nodules, particularly among women and the elderly which mirrors the trends observed in thyroid cancer. Most thyroid nodules were found in asymptomatic patients as a result of routine physical examination or as incidental findings on imaging. To our knowledge, this is the first study in the United States to describe the incidence rate of thyroid nodule diagnosis and to examine the drivers of thyroid nodule detection.
Acknowledgments
Funding source: This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under award number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Competing of Interest: No competing financial interests exist.
References
- 1.Mortensen JD, Woolner LB, Bennett WA. Gross and microscopic findings in clinically normal thyroid glands. J Clin Endocrinol Metab. 1955;15(10):1270–1280. doi: 10.1210/jcem-15-10-1270. [DOI] [PubMed] [Google Scholar]
- 2.Tan GH, Gharib H. Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. Ann Intern Med. 1997;126(3):226–231. doi: 10.7326/0003-4819-126-3-199702010-00009. [DOI] [PubMed] [Google Scholar]
- 3.Reiners C, Wegscheider K, Schicha H, Theissen P, Vaupel R, Wrbitzky R, Schumm-Draeger PM. Prevalence of thyroid disorders in the working population of Germany: ultrasonography screening in 96,278 unselected employees. Thyroid. 2004;14(11):926–932. doi: 10.1089/thy.2004.14.926. [DOI] [PubMed] [Google Scholar]
- 4.Belfiore A, La Rosa GL, La Porta GA, Giuffrida D, Milazzo G, Lupo L, Regalbuto C, Vigneri R. Cancer risk in patients with cold thyroid nodules: relevance of iodine intake, sex, age, and multinodularity. The American journal of medicine. 1992;93(4):363–369. doi: 10.1016/0002-9343(92)90164-7. [DOI] [PubMed] [Google Scholar]
- 5.Davies L, Welch H. CUrrent thyroid cancer trends in the united states. JAMA Otolaryngology–Head & Neck Surgery. 2014 doi: 10.1001/jamaoto.2014.1. [DOI] [PubMed] [Google Scholar]
- 6.Ahn HS, Kim HJ, Welch HG. Korea’s thyroid-cancer “epidemic”–screening and overdiagnosis. N Engl J Med. 2014;371(19):1765–1767. doi: 10.1056/NEJMp1409841. [DOI] [PubMed] [Google Scholar]
- 7.Kweon SS, Shin MH, Chung IJ, Kim YJ, Choi JS. Thyroid Cancer is the Most Common Cancer in Women, Based on the Data from Population-based Cancer Registries, South Korea. Jpn J Clin Oncol. 2013;43(10):1039–1046. doi: 10.1093/jjco/hyt102. doi:hyt102 [pii] 10.1093/jjco/hyt102. [DOI] [PubMed] [Google Scholar]
- 8.Brito JP, AlNofal A, Montori V, Hay ID, Morris JC., 3rd The impact of subclinical disease and mechanism of detection on the rise in thyroid cancer incidence: a population-based study in Olmsted County, Minnesota during 1935 through 2012. Thyroid. 2015 doi: 10.1089/thy.2014.0594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aschebrook-Kilfoy B, Schechter RB, Shih YC, Kaplan EL, Chiu BC, Angelos P, Grogan RH. The clinical and economic burden of a sustained increase in thyroid cancer incidence. Cancer Epidemiol Biomarkers Prev. 2013;22(7):1252–1259. doi: 10.1158/1055-9965.EPI-13-0242. [DOI] [PubMed] [Google Scholar]
- 10.Applewhite MK, James BC, Kaplan SP, Angelos P, Kaplan EL, Grogan RH, Aschebrook-Kilfoy B. Quality of Life in Thyroid Cancer is Similar to That of Other Cancers with Worse Survival. World J Surg. 2015 doi: 10.1007/s00268-015-3300-5. [DOI] [PubMed] [Google Scholar]
- 11.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Pankratz JJ, Brue SM, Rocca WA. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41(6):1614–1624. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol. 2011;173(9):1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery. 1993;114(6):1050–1057. discussion 1057–1058. doi:0039-6060(93)90321-4[pii] [PubMed] [Google Scholar]
- 14.Davies L, Randolph G. Evidence-based evaluation of the thyroid nodule. Otolaryngol Clin North Am. 2014;47(4):461–474. doi: 10.1016/j.otc.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Merzel C. Gender differences in health care access indicators in an urban, low-income community. Am J Public Health. 2000;90(6):909–916. doi: 10.2105/ajph.90.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hunt K, Adamson J, Hewitt C, Nazareth I. Do women consult more than men? A review of gender and consultation for back pain and headache. J Health Serv Res Policy. 2011;16(2):108–117. doi: 10.1258/jhsrp.2010.009131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, Pacini F, Randolph GW, Sawka AM, Schlumberger M, Schuff KG, Sherman SI, Sosa JA, Steward DL, Tuttle RM, Wartofsky L. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Choosing Wisely. www.choosingwisely.org. Accessed 11/2015.
- 19.Sosa JA, Hanna JW, Robinson KA, Lanman RB. Increases in thyroid nodule fine-needle aspirations, operations, and diagnoses of thyroid cancer in the United States. Surgery. 2013;154(6):1420–1426. doi: 10.1016/j.surg.2013.07.006. discussion 1426–1427. [DOI] [PubMed] [Google Scholar]
- 20.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clinic proceedings. 2012;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]


