Managing war injury is no longer the exclusive preserve of military surgeons. Increasing numbers of non-combatants are injured in modern conflicts, and peacetime surgical facilities and expertise may not be available. This article addresses the management of war wounds by non-specialist surgeons with limited resources and expertise. One of the hallmarks of war injury is the early lethality of wounds to the head, chest, and abdomen; therefore, limb injuries form a high proportion of the wounds that present at hospitals during conflicts.
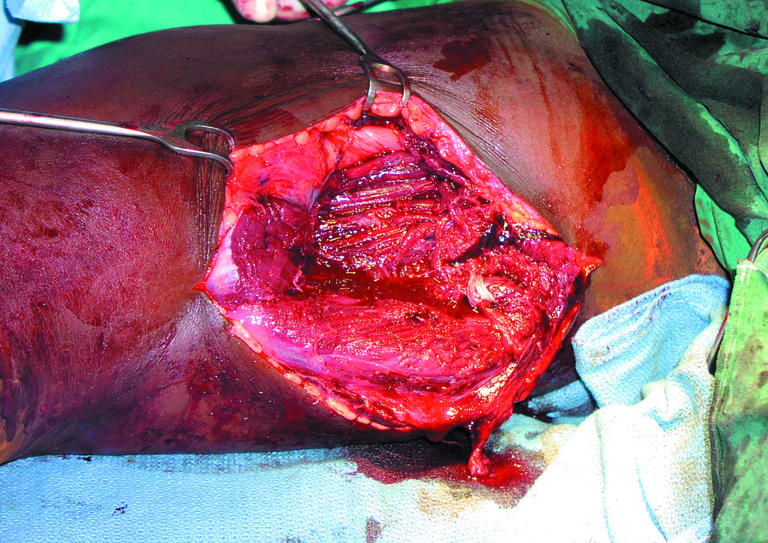
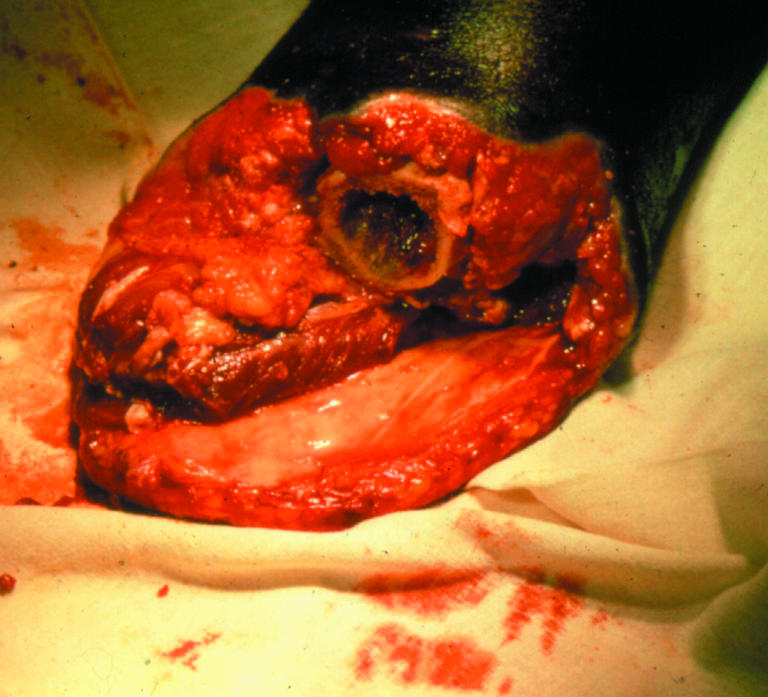
Figure 1.

Healing amputation stump
Wounding patterns
Gunshot wounds
The incidence of gunshot wounds in conflict depends on the type and intensity of the fighting. In full scale war the proportion of casualties injured by gunshot is generally less than in low intensity or asymmetric warfare.
Figure 2.
Cavitation secondary to high energy transfer bullet wound
Bullets cause injury by:
Direct laceration of vital structures
Stretching of tissue (cavitation), causing fracturing of blood vessels and devitalisation of tissue
Secondary contamination.
The nature and extent of ballistic wounding is related to the energy transfer between bullet and tissue and the characteristics of the organs affected. Bullets cause injury by transferring their energy into the body tissues; the design of the bullet influences this process, with hollow nosed or dumdum bullets being designed to maximise energy transfer.
Table 1.
Types of injury in modern warfare
| • High energy transfer bullet wounds |
| • Fragmentation injury |
| • Blast injury |
| • Burns |
A high velocity bullet from a military rifle has more energy, and therefore greater wounding potential, than a handgun round. However, if it passes cleanly through a limb without striking bone, it may impart little of its energy to the victim and therefore cause a relatively minor wound.
Figure 3.

Lower limb disruption due to blast injury
Blast injury
Wounding may also be inflicted by explosive munitions such as rockets, aerial bombardment, mortars, and grenades. A small volume of explosive is converted to a large volume of gas in a very short time. This results in high pressure at the point of detonation, leading to the acceleration of gas molecules away from the explosion, a so called blast wind, the leading edge of which is the shock front.
Primary blast injury is typically experienced by casualties close to the explosion and is due to the interaction of this shock front on air-filled cavities within the body (middle ear, lung, bowel).
Secondary blast injury is due to impact on the body of items energised by the explosion. Modern munitions contain preformed metallic fragments; lacking aerodynamic features, such fragments rapidly lose velocity, resulting in low energy transfer pattern wounds.
Tertiary blast injury is seen when the victim is accelerated by the blast and thrown against a fixed object such as a wall.
Quaternary blast injury is that caused by collapse of any building secondary to a blast event.
Victims of blast often have multisystem injury, complicated by the presence of blunt and penetrating injury and burns.
Potential wounding energy of a missile:
 |
Where m is the mass of the missile and v is its velocity
Treating war injury
Initial measures
Initial measures for treating war injury are similar to those for any severe injury. Assessment and resuscitation of patients has traditionally been along the priorities of ABC—airway, breathing, and arrest of haemorrhage. Increasingly, however, prehospital military practice is to arrest haemorrhage first. This is because of the high incidence of death from exsanguination in war injured patients and the potential for simple first aid measures to prevent this.
Figure 4.

Acute landmine injury
Intravenous opiate analgesia and antibiotics should be given: the International Committee of the Red Cross (ICRC) recommends 6 MU (3600 mg) benzylpenicillin intravenously for an adult patient. In the developing world patients might not have been immunised against tetanus. Grossly contaminated wounds containing devitalised tissue are at risk of infection with Clostridium tetani, and antitetanus serum and tetanus toxoid should be available.
Table 2.
Typical characteristics of war wounds
| • Contaminated |
| • Contain devitalised tissue |
| • Affect more than one body cavity |
| • Often involve multiple injuries to the same patient |
| • 75% affect the limbs |
| • Often present late |
Radiography, if available, is helpful in delineating fractures and detecting haemopneumothorax.
Wound assessment
After resuscitation, a careful top to toe survey must be done. Care must be taken to identify any truncal penetrating injury, without forgetting the back and buttocks, perineum, and axillae. Each wound must then be assessed and recorded. Wound assessment should include
Site and size
Presence of a cavity and degree of contamination
Anatomical structures that may have been injured
Distal perfusion
Presence of fractures
Whether a limb is so severely wounded as to be unreconstructable.
Wound excision
Wound excision involves removal of dead and contaminated tissue that, if left, would become a medium for infection. For limb wounds, a pneumatic tourniquet should be used if possible to reduce blood loss.
Figure 5.

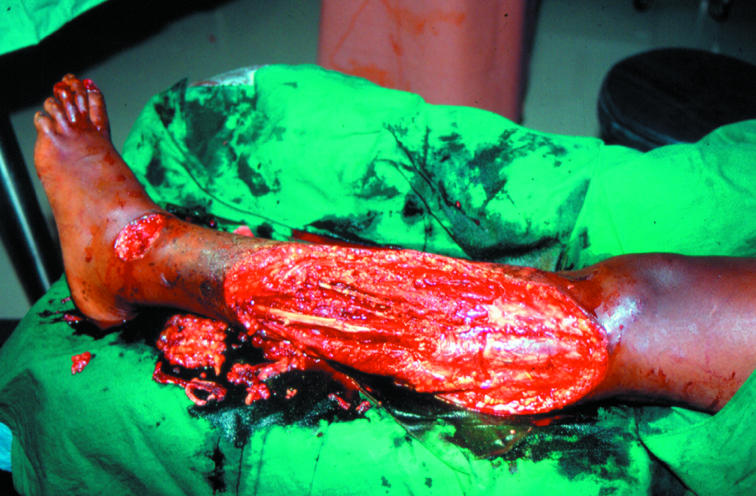
Blast injury before wound excision (top) and after wound excision (bottom)
The first stage of the procedure is axial skin incision (debridement) in order to decompress the wound and allow post-traumatic swelling without constriction. These incisions should not cross joints longitudinally. Once decompression has been achieved, contamination should be removed and non-viable tissue excised. Skin is resilient, and only minimal excision is usually necessary, typically around the margin of the wound.
All foreign material should be removed from the wound, but obsessive pursuit of small metallic debris is not worth while. All dead and contaminated tissue should be excised, but determining the extent of the tissue that should be removed is often difficult. Dead muscle is dusky in colour, shows little tendency to bleed, and does not contract to forceps pressure.
Figure 7.
Wound left open with dry, bulky, sterile dressing
Bone fragments denuded of soft tissue attachment should be removed; if left in the wound they will become infected and form osteomyelitic sequestrae. Injured nerves or tendons should be marked (with suture) for later repair.
At the end of the procedure the wound should be washed with copious quantities of saline and then left open. Apply a dry, bulky, sterile dressing.
Some low energy transfer wounds, such as those from most handguns, do not need extensive debridement and excision. These wounds can, in some circumstances, be managed without surgery.
The optimal management of the multiple small fragment wounds often seen as a result of secondary blast injury is debated. The large number of these wounds precludes individual wound excision. There is no cavitation associated with such injury, and, because of the poor aerodynamic qualities of random fragments, the degree of penetration is usually not great. A reasonable approach is to clean all the wounds as thoroughly as possible by irrigation under general anaesthesia and then surgically debride only those major wounds associated with gross, deep contamination and tissue damage.
Figure 8.
Clean wound, ready for delayed primary closure
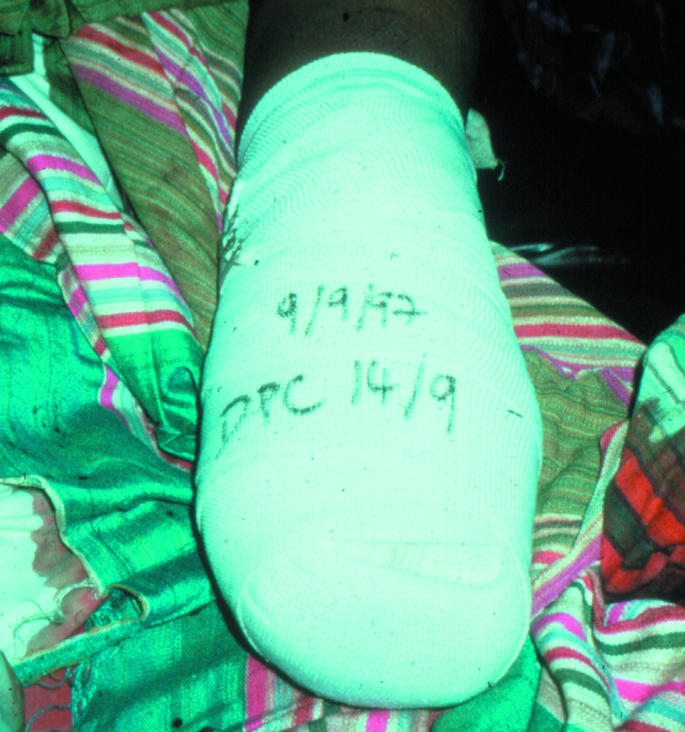
Delayed primary closure
Once wound excision has been done the patient can bereturned to the ward for continued monitoring and analgesia. Dressings should be left in place and removed only when the patient returns to theatre for delayed primary closure. The ICRC recommends an interval of five days, but practice in the developed world now tends towards shorter periods of 48-72 hours. The only indication for return to theatre before this time has elapsed is signs of sepsis or an offensive smelling dressing. The commonest cause of sepsis is inadequate primary surgery.
Figure 9.

Primary myoplastic flap suitable for covering the transected bone of an amputation stump
The dressing should be removed in theatre with the patient under appropriate anaesthesia. If the wound shows no signs of infection, necrosis, or residual contamination it can be closed by suture or a split skin graft. However, multiple debridement may be required: in an ICRC series of amputations, only 45% were suitable for closure at first relook, with 33% of cases needing one further debridement and 22% needing two or more.
Table 3.
Amputation surgery for war wounds
| • Always under tourniquet |
| • Excise all dead and contaminated tissue |
| • Determine best functional level of amputation |
| • Fashion flaps using myoplastic technique |
| For trans-tibial amputation, use medial gastrocnemius flap |
| For trans-femoral amputation, use vastus lateralis or adductor magnus flap |
| • Leave wound open |
| • Delayed primary closure |
If closure is attempted, tension must be avoided. Rehabilitation can then start.
Amputation surgery
Some ballistic injuries, particularly those caused by landmines, will result in traumatic amputation of limbs. In others the limb injury is so severe that surgical amputation is necessary. The decision to amputate should come at the time of wound assessment. Scoring systems for limb injury are only poorly relevant to a ballistic pattern of injury. An insensate or avascular distal limb is a strong indication for amputation; seeking consensus with other surgical staff is helpful.
Skin and bone are relatively resistant to the propagation of blast and fragment, but muscle offers little impediment, and contamination can track along fascial planes. The extent of contamination and devitalisation of tissue is often more extensive than initially apparent.
Military surgeons have traditionally performed guillotine amputations, transecting skin, muscle, and bone all at the same level. Although this is quick and requires little surgical skill, it makes closure difficult, and the final amputation level is often more proximal than necessary. Most humanitarian surgical organisations recommend fashioning definitive flaps at initial surgery, maintaining stump length and facilitating early closure. The use of a myoplastic flap to cover the transected bone is strongly advocated.
Amputation should always be carried out under tourniquet to minimise blood loss. The surgical strategy is as for other war wounds; excise dead and contaminated tissue, determine the best functional level of amputation, and construct flaps to facilitate this. The wound should be left open and dressed with a dry, bulky, sterile dressing until delayed primary closure.
Competing interests: None declared.
The ABC of conflict and disaster is edited by Anthony D Redmond, emeritus professor of emergency medicine, Keele University, North Staffordshire; Peter F Mahoney, honorary senior lecturer, Academic Department of Military Emergency Medicine, Royal Centre for Defence Medicine, Birmingham; James M Ryan, Leonard Cheshire professor, University College London, London, and international professor of surgery, Uniformed Services University of the Health Sciences (USUHS), Bethesda, MD USA; and Cara Macnab, research fellow, Leonard Cheshire Centre of Conflict Recovery, University College London, London. The series will be published as a book in the autumn.
Further reading and resources
- • Coupland RM. War wounds of limbs. Oxford: Butterworth-Heineman, 1993
- • Gray R. War wounds: basic surgical management. Geneva: ICRC publications, 1994
- • Coupland RM. Amputation for war wounds. Geneva: ICRC publications, 1992
- • Mahoney PF, Ryan JM, Brooks A, Schwab CW, eds. Ballistic trauma: a practical guide. London: Springer Verlag, 2004
- • King M, ed. Primary surgery. Vol 2. Trauma. Oxford: Oxford Medical Publications, 1993


