Abstract
The European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC) is a European Respiratory Society (ERS) Clinical Research Collaboration dedicated to improving research and clinical care for people with bronchiectasis. EMBARC has created a European Bronchiectasis Registry, funded by the ERS and by the European Union (EU) Innovative Medicines Initiative Programme.
From the outset, EMBARC had the ambition to be a patient-focussed project. In contrast to many respiratory diseases, however, there are no specific patient charities or European patient organisations for patients with bronchiectasis and no existing infrastructure for patient engagement. This article describes the experience of EMBARC and the European Lung Foundation in establishing a patient advisory group and then engaging this group in European guidelines, an international registry and a series of research studies.
Patient involvement in research, clinical guidelines and educational activities is increasingly advocated and increasingly important. Genuine patient engagement can achieve a number of goals that are critical to the success of an EU project, including focussing activities on patient priorities, allowing patients to direct the clinical and research agenda, and dissemination of guidelines and research findings to patients and the general public. Here, we review lessons learned and provide guidance for future ERS task forces, EU-funded projects or clinical research collaborations that are considering patient involvement.
Educational aims
To understand the different ways in which patients can contribute to clinical guidelines, research projects and educational activities.
To understand the barriers and potential solutions to these barriers from a physician’s perspective, in order to ensure meaningful patient involvement in clinical projects.
To understand the barriers and potential solutions from a patient’s perspective, in order to meaningfully involve patients in clinical projects.
Short abstract
Patient involvement in research and guidelines can greatly enhance the quality and impact of projects http://ow.ly/HGXR30dqSh0
Patients and carers are the key stakeholders in every aspect of medical care; yet, until recently, direct involvement of patients in clinical guidelines, clinical research studies or research consortia was uncommon [1]. Patients have typically been viewed as participants, e.g. subjects in a clinical trial, or involvement has been characterised as “tokenism” [1]. This is changing, as the value of patient involvement is being recognised, as physicians are being provided with the tools and guidance required to achieve meaningful patient engagement, and as research funders increasingly encourage or require patient involvement during the development of research projects [2–5].
The Value+ toolkit defines meaningful patient engagement as giving patients an active role in activities or decisions that will have consequences for the patient community, because of their specific knowledge and relevant experience as patients [6].
Despite an increase in literature regarding patient involvement in projects, one of the major barriers to patient engagement is a lack of understanding from healthcare professionals about how to do it, and a lack of support in terms of funding for patient activities and tools and advice on how to do it [7–9]. From a patient’s perspective, while involvement in clinical projects can be a very positive experience, it is important to consider barriers, such as available time, self-confidence, stigma associated with illness and financial considerations, and to design patient involvement in a way that ensures that patients are adequately supported.
In this article, we describe a successful European Respiratory Society (ERS)/European Union (EU) project focussed on bronchiectasis, in which patients have been closely involved at every stage [10]. The purpose of this article is to highlight the multiple aspects of clinical guidelines and clinical research where patients can make a positive contribution, to highlight the lessons learnt from the European Multicentre Bronchiectasis Audit and Research Collaboration (EMBARC) project in terms of how to support patient engagement, and finally to reflect upon the patients’ experience of these projects, in order to help future patients and professionals to do better.
Patient involvement in EMBARC
EMBARC was one of the first ERS Clinical Research Collaborations awarded in 2013 [10, 11]. The specific objectives of EMBARC defined in its original constitution were: to create a European Bronchiectasis Registry to facilitate research and quality improvement initiatives across different healthcare systems; to build a network of researchers and experts in bronchiectasis to guide future research and clinical priorities; to attract new researchers and clinicians to the field of bronchiectasis; to support and encourage early career researchers in the field of bronchiectasis through involvement in network activities; and to build bronchiectasis research capacity in Europe [10].
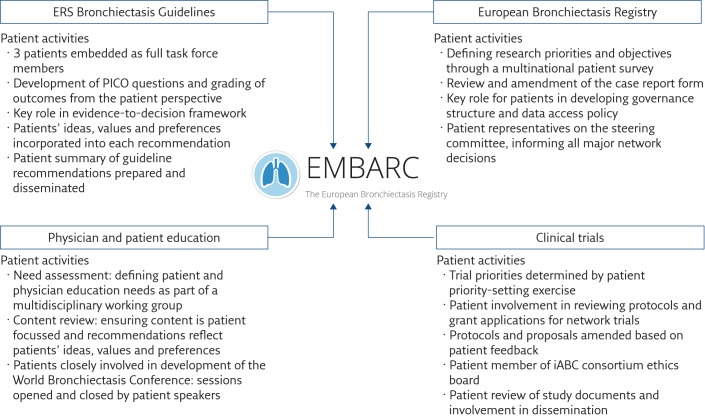
Bronchiectasis is a poorly studied “orphan” condition with limited research and a poorly defined standard of care [12–14]. Patients often have poor quality of life, and may have poor experiences of healthcare due to delayed diagnosis, ineffective treatments, lack of understanding of their condition by the general public and by non-specialist doctors, and a lack of access to quality information [15–18]. Therefore, a decision was made early in the EMBARC project to engage directly with patients to ensure that activities within the project were patient focussed and, where appropriate, patient led. EMBARC has been a multifaceted project with a range of different activities, all of which have involved patients. These are summarised in figure 1 and each is discussed in the following sections.
Figure 1.
Summary of patient involvement in the EMBARC project.
The European bronchiectasis patient advisory group
The formation of the European bronchiectasis patient advisory group was initially challenging, as in common with many rare or neglected conditions there is no formal patient organisation, charity or advocacy organisation for bronchiectasis. Identifying patients that can represent the broader patient community can therefore be difficult [13].
Hence, the proposed activities were dependent on the creation of a representative European patient group, which was facilitated by the European Lung Foundation (ELF). ELF was founded by the ERS in 2000 with the aim of bringing together patients and the public with respiratory professionals to positively influence lung health [19–22]. It has extensive experience of facilitating patient engagement with research and clinical projects, including in EU consortia such as the successful U-BIOPRED (Unbiased Biomarkers for the Prediction of Respiratory Disease Outcomes) project, and has published extensively on the topic [1, 19–25].
Using a combination of existing patient contacts, patients recruited from an online patient survey (discussed in a later section of this article) and patients recommended by European physicians, ELF developed an advisory group of >50 patients. Patients were supported by the patient projects co-ordinator at ELF and kept up to date with activities through regular newsletters.
As projects got underway, the patient advisory group members were asked to volunteer for activities that they would be interested in participating in. Patients were therefore able to choose a level of involvement that suited them, from being deeply involved in working groups to simply remaining up to date on activities and giving input by email.
Patient involvement in an ERS bronchiectasis guidelines task force
Patients, and particularly patients with bronchiectasis, have a strong motivation to ensure that they and other patients receive the best possible care. There is therefore a high level of interest among patients to become involved in guideline task forces. From the physician’s perspective, guideline development is substantially enhanced by patient involvement. ERS guidelines now use the GRADE (Grading of Recommendations Assessment, Development and Evaluation) approach for the development of evidence-based recommendations [26]. GRADE encourages the incorporation of patients’ ideas, values and preferences at every stage of the guideline development process [26, 27].
For the 2017 ERS bronchiectasis guidelines, three patients were invited to participate as full members of the task force. This is, to the best of our knowledge, the first task force in which patients have been included as full voting members of the task force. Patients therefore played a full part in the development of the document, from the initial stages in which the most clinically important questions are determined using the PICO (patient, intervention, comparator, outcome) format, and particularly in rating the outcomes to be used in assessing treatments. In the GRADE approach, all possible outcomes are considered and are rated as critical, important or not/less important, with only critical or important outcomes being used to inform guideline recommendations [26, 27]. Patients are clearly in the strongest position to advise on what outcomes are important to them, and they greatly enhanced this evaluation process.
Patients attended every guideline meeting as full members, participating actively in the discussions and frequently being asked their views on different treatment approaches or proposed recommendations.
Guideline recommendations are formulated using evidence-to-decision frameworks in which evidence from clinical trials/observational studies is pooled and the data are then integrated with additional information, which includes the desirable and undesirable effects of a treatment, the certainty of evidence, resources, equity, acceptability and feasibility of the intervention [28]. Patients played a critical role in informing these assessments, by providing the guideline panel with information about how much or little they valued an intervention, the acceptability of different interventions to them and how they viewed the overall balance between desirable and undesirable effects [28].
Our experience was that the patients’ perspective often differed from those of guideline panellists and that patients made an important contribution in modifying the ultimate guideline recommendations.
Patients were asked to review the final guideline document and, at the time of writing this article, a lay version of the guideline designed for patients and the wider public is being prepared by the patient advisory group in collaboration with ELF.
Patient involvement in the European Bronchiectasis Registry
The formation of the EMBARC registry was a major undertaking, involving over 150 centres in more than 40 countries. As bronchiectasis is a poorly researched disease, there have been limited epidemiological data and we know very little about the natural history [29–31]. The initial development of the registry required the development of a case report form and a governance structure that would allow the registry to succeed over the long term. This, in turn, needed to be focussed on the outputs that we wished to achieve through the research. To inform this, we conducted an online patient survey co-ordinated by ELF. The survey was sent to over 100 European physicians caring for bronchiectasis patients, and the online survey was ultimately completed by more than 1000 patients and carers of those with bronchiectasis, with 711 included in the final analysis [11]. The questions asked in this survey were developed by a small working group composed of three physicians, representatives of ELF and four patients [11].
The result has been published as a research priorities document in the European Respiratory Journal and this “research roadmap” defined by patients and physicians is now used as the basis for the EMBARC strategy and analysis plan [11].
The case report form of the registry was developed with input from patients and directed by the results of the patient survey. The study documents, such as the patient information sheet and consent form, were also reviewed and amended by patients [10].
The governance structure of the registry included patients, and patients have attended each of the registry steering committee meetings. The patient representatives also gave a closing address at the general assembly of the EMBARC project in 2015, and an opening address at the EMBARC general assembly in 2016 (figure 2).
Figure 2.
A group of bronchiectasis patients address the EMBARC annual meeting.
Patients have a stake in ensuring that their data are used to benefit the whole research community and, ultimately, other patients. The patient advisory group therefore played a key role in EMBARC adopting a very open and transparent data access process, which allows any research with a legitimate scientific question to access the data [32].
The EMBARC registry is ongoing and patients continue to play a key role in its governance and development as they have done since its inception.
Patient involvement in bronchiectasis clinical trials and studies
One of the key objectives of the registry is to make it easier for academic researchers, consortia and industry to conduct clinical research studies and clinical trials. Since its inception, the EMBARC project has supported more than 10 such studies, ranging from multinational clinical trials to observational surveys [33–39]. For grant applications, patients have provided input into study design and advice about patient involvement, and have reviewed dissemination plans. Patients have written letters of support to encourage funders to support bronchiectasis-related projects. Patients are now serving on advisory boards and the ethical committees of trial programmes, including the inhaled antibiotics in bronchiectasis and cystic fibrosis (iABC) consortium funded by the EU Innovative Medicines Initiative, of which EMBARC is a member [40]. Patients have had a strong impact on the studies performed. As an example, patient representatives felt strongly that comorbidities were not sufficiently addressed in the work of the registry or in clinical guidelines, feeding back to the working group that often comorbidities associated with bronchiectasis were the factors most strongly influencing their quality of life. EMBARC undertook a linked registry study around comorbidities that confirmed the patients’ impression, leading to a high impact publication in The Lancet Respiratory Medicine [34]. This is a clear example of how patients can drive the research agenda. As these clinical trials continue, patients will be involved in trial conduct and the dissemination of results.
Patient involvement in education initiatives, the ERS Annual Congress and World Bronchiectasis Conference
There is a significant need for physician education in bronchiectasis, as highlighted by the patient priorities survey, in which one of the top patient priorities was that their primary care physician should have greater knowledge and understanding of their condition [11]. Patients have been integral to the development of a physician education platform that is due for launch in 2017. In addition, patients consistently report a lack of high-quality educational material available for them to understand their own condition. Patients have therefore led the development of a patient education website to be launched by ELF in 2017 to provide high-quality peer-reviewed information about bronchiectasis targeted at the general public. These initiatives have been conducted under the same principles as the task force, with multidisciplinary working groups that include patients as equal partners. Patients also participated in the first World Bronchiectasis Conference, held in Hannover, Germany, in 2016. The conference was opened by a lecture by Marta Almagro, a patient with bronchiectasis who gave a powerful, personal presentation about the impact of the disease and the importance of encouraging greater awareness of bronchiectasis (figure 3). Patients have also attended EMBARC meetings at the past three ERS International Congresses.
Figure 3.
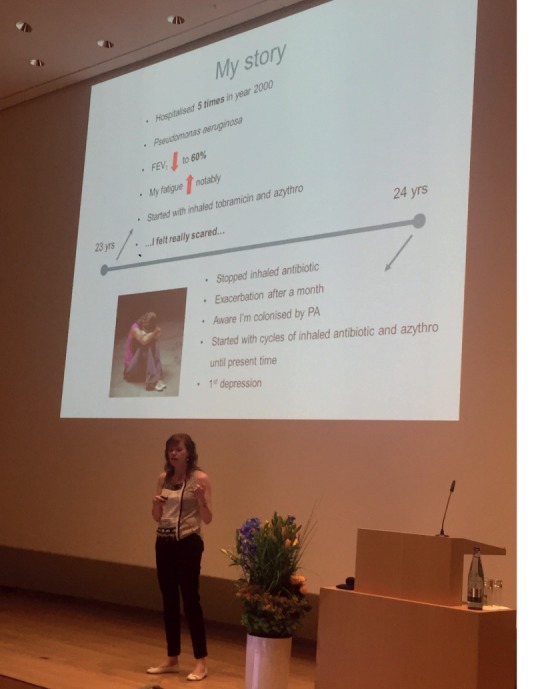
Marta Almagro opens the first World Bronchiectasis Conference.
Experience of patient involvement: the clinician’s perspective
In part as a result of the strong support from patients, the EMBARC project has been a major success. The European Bronchiectasis Registry is now well established with >8000 patients enrolled at the time of writing, and the project has produced a large number of important publications. Although the benefit of patient involvement is clear from the information presented here, the process presented many challenges.
The EMBARC study team had limited prior experience of patient involvement in research projects or guidelines. There was no established pathway or guidelines for how patients should be involved in research or task forces, and as a result the “rules of engagement” had to be generated by EMBARC and ELF on a bespoke basis to suit the project. There was some initial resistance to patient involvement from some quarters, because of concerns that patients may be upset by some aspects of discussion or that the presence of patients may stifle debate. As an example, if a member of a guideline task force is receiving a drug that the guideline task force wants to recommend is ineffective or potentially harmful, how would that patient react, and would this harm their relationship with their existing healthcare professional?
Additional barriers include the need for in-depth scientific discussion, which may not always be accessible for patients or carers, leading to the concern that discussions may be stifled if conversations are constantly being interrupted for lay explanations. Table 1 outlines some of the barriers and concerns and how these were addressed in this project. These can be used as a framework for future projects of this kind, while recognising that barriers may be different depending on the nature of the projects being proposed.
Table 1.
Recommendations for clinicians, written by both physicians and patients, to ensure appropriate patient engagement
| Barriers | Recommendations |
| Representativeness (i.e. are patients involved in the project representative of the overall patient population?) | Involve more than one patient in any project. This has multiple benefits, including increasing the representativeness, but also allowing for peer support and ensuring there is representation if patients become unwell and are unable to attend meetings or participate in activities. If patients are attending as representatives of a large patient group or organisation, ensure that discussions or outcomes are also shared with the wider group so that a larger body of patients has the opportunity to contribute.Ensure patient representatives understand that they are representing other patients and not just giving their personal story.Incorporate broader patient data into data collection, e.g. by performing a literature review for patient perspective articles or performing a patient survey with a sufficient sample size to be considered representative of wider patient opinion. Patient representatives can advise on the most relevant patient-centred search terms of literature reviews and ELF can also provide advice on this. |
| Language | Currently, there is a requirement for participating patients to speak English. This can result in a UK/Ireland bias and so it is important to try to achieve representation of other European countries. Where activities can be multilingual (such as patient surveys), these methods should be used. ELF provides support for multilingual focus groups and surveys. |
| Patient travel and reimbursement | Face-to-face meetings are the most effective way to engage patients. The cost of this is the requirement for patients to travel to meetings, which is expensive and time consuming. It is essential that the project funds patient travel adequately and in an appropriate way and timeline. Where travel is prevented through ill health or other issues, teleconference facilities should be offered to avoid excluding patients’ valuable contributions.The INVOLVE guidelines (www.invo.org.uk) from the National Institute for Health Research (UK) suggest that, wherever possible, patients involved in research projects should receive payment or a fee for participation. However, they note that consideration should be given to whether payments may affect state benefits. |
| Lack of scientific knowledge or background | Patients cannot be expected to be experts in clinical trial design, observational research or guideline methodology. In the ideal scenario, patients would be trained with the knowledge that they require, through schemes such as the European Patient Ambassador Programme (EPAP; www.epaponline.org). If it is not feasible for patients to have such training, we recommend:1)Project chairs meet with patients prior to meetings so that patients can have an explanation of the context of the expected discussion;2)Use of natural breaks in discussion to explain to patients in lay terms what is being discussed and ask patients specific questions where their input is needed;3)Debriefing with patients after meetings to ensure they have understood the discussions.For rare diseases, including rare pulmonary diseases, EURORDIS (Rare Diseases Europe) provides training to empower patient representatives to participate in clinical research and other clinical projects. |
| Perception of “tokenism” | Set specific objectives for patient involvement in projects and communicate these to all stakeholders. The professional participants in a task force or research project should understand what the role of patients in the project is, and patients should understand exactly what is expected of them.Involve patients as equals. We have had a very positive experience of including patients as full equal members of a guideline task force. |
| Patients isolated or ignored in meetings | There is a responsibility on the chairs of meetings to prompt participants to involve the patient representatives, and to prompt patients to provide input where appropriate. Patient participation can be facilitated by making clear the role of patients to both the patients and physicians at the start of the project.Smaller group work, such as subcommittees or working groups, can make it easier for patients to participate as groups are smaller, but there is similarly a responsibility on subgroup participants to ensure patients are involved. |
| Patients lacking confidence to get involved | Welcome and introduce patients at the start of every meeting. Encourage all task force or study team members to introduce themselves; even if all of the professionals are well known to each other, they are not well known to the patients. Chairs should give an introduction explaining the role of the patients and encouraging task force or study members to involve the patients.It is particularly helpful for patients to meet with the chairs or ELF representatives prior to meetings (and particularly the first meeting) so that they know what to expect and get to know some other people in the meeting prior to joining larger group meetings.Research or guideline meetings often also involve social events and it is appropriate to involve patients in social events so that they can get to know panel members in a more relaxed setting and are not excluded. |
| Conflicts of interest and confidentiality | Just like physicians, patients may have conflicts of interest that are relevant to their participation in task forces and research projects.Project chairs should give consideration to how they will manage patients’ conflicts of interest. This may include financial conflicts of interest (patients with business interests related to the healthcare field or having relationships with pharmaceutical companies) or non-financial conflicts of interest. The most frequent non-financial conflict of interest is that the patient may be a patient under the care of a member of the task force. This is not necessarily a problem, but consideration should be given to whether patients may feel coerced to participate, and whether they may feel able to give their honest opinion, which may be at odds with the opinion of their physician.Patient confidentiality should be maintained at all times. Patients may choose to share information about their medical background, but their physician should not disclose information to the panel or panel members without patient consent. |
| Lack of awareness of governance and regulatory aspects around patient involvement | Clinicians may be concerned about involving patients in research in the belief that all work with patients requires ethical or other governance approvals. Note that ethical approval is not required to involve members of the public in designing or conducting research studies, participating as a member of an advisory group or helping to develop study materials or questionnaires. |
| Identifying suitable patients | Consider the knowledge and experiences you need to inform the project. Try to create a “job description” or specification of the kind of patient you wish to involve.Involve patient organisations wherever possible as they provide peer support, training and, in some cases, resources to aid patients. Involving patient organisations also generally means the representatives can be the collective voice of a group rather than simply representing themselves.Consider the commitment required by patients. It is important to remember that patients have jobs, lives and commitments of their own and may not be able to attend all meetings or respond to short deadlines. Give information about the time commitment and project duration up front to let patients make an informed decision about whether to participate. |
Physician attitudes towards patient involvement have clearly changed over the course of the project, with these concerns addressed. Clinicians and allied health professionals have commented how overwhelmingly positive the experience of patient involvement has been, and the genuine level of enthusiasm this has generated is reflected in increasing requests to involve patients in further events, committees and activities. Nevertheless, EMBARC has made plenty of mistakes along the way and it is hoped that the guidance in this document can help to highlight both the good and bad practices we have identified over the past 3 years so that future projects can learn from our experience.
Experience of patient involvement: the patient’s perspective
Patients become involved in research and guideline projects for a variety of reasons, including their own personal experiences of care and a desire to improve treatment for themselves and for others with a similar condition. Making a decision to become involved in a project like EMBARC is a major undertaking and there are a few things that can be done to make it easier for patients to volunteer to become involved [41]. The EMBARC patients’ key recommendations for patient involvement in research are presented in table 2.
Table 2.
EMBARC patients’ key recommendations for patient involvement in research
| Do | Don’t | |
| Involvement |
|
|
| Preparation and training |
|
|
| Meetings |
|
|
| Finance |
|
|
| Publication and dissemination |
|
|
| Communication |
|
|
We recommend that clinicians explain very clearly what they expect from patients, which may be helped by generating a job description for patient representatives. It is important to make clear at the beginning what time commitment is needed and also to let patients know if any training is required or will be provided. We recommend involving patients at an early stage, when they have the opportunity to actively influence the research, rather than later on when most of the major decisions have been made. It is also important to make sure that patients know who to contact with questions or for information.
As a result of an open set of medical professionals, the patients’ input and concerns are fully reflected in all aspects of the EMBARC project. A prime example was in agreeing the final draft of the guidelines, where patient acceptability is one of the criteria. At this stage, the healthcare professionals actively sought the input of the patient representatives. The recommendations in the 2017 ERS bronchiectasis guidelines have all been developed with patients and a lay version of the guidelines will published alongside the main document. Another important impact patients made was to request that all publications arising from EMBARC should be freely available to patients, with the effect that all publications from EMBARC have been open access since 2015.
At the start of the patient involvement, however, meetings were difficult and there was a need for clear guidance on the potential role(s) of the patient (from observer to full participant) and how the meetings could be structured to reflect the presence of patients. To many patients, these meetings present a challenge on five fronts: 1) it is a formal meeting and many patients may not attend formal meetings of any type in their day to day life; 2) the group of medical professionals are already known to each other but not to the patient; 3) the medical members may also be treating the patient away from the meeting; 4) the potential for “deep” scientific and medical discussion with associated jargon; and 5) the need to address topics such as life expectancy calculations, which can be upsetting to patients.
The biggest challenge for a patient is the first meeting. This was also highlighted from the clinicians’ perspective in terms of resistance from the clinicians, which may result from meeting a patient out of the context of a clinic visit, or from the instant access of the patient to a club that the clinicians have invested many years to gain entry into. In most cases it was clear that this was the clinician’s first experience of involving patients in research and clinical projects.
Each patient will be different in their experience of meetings, their subject matter knowledge, how outgoing they are, and their financial circumstance. An underestimated impact of involvement in research projects is the impact that medical data can have on patients. For example, several patients involved in the EMBARC project are chronically infected with Pseudomonas aeruginosa. Across multiple discussions in both research and guideline meetings, it became clear that the physicians regard P. aeruginosa as a poor prognostic sign, a sign of increased mortality and more rapid disease progression requiring more intensive treatment [38, 39, 42]. Hearing this can be very upsetting for a patient who knows that they are infected with P. aeruginosa but who may not have been previously made aware of its health consequences. The “clinical” tone of these discussions was described by one patient as “brutal”. This is not a scenario unique to bronchiectasis, as the reaction would no doubt be similar for a patient with lung cancer on hearing lung cancer 5-year mortality rates, or a patient with sleep apnoea learning about their cardiovascular risks, if they are not warned beforehand that such information will be discussed [43, 44]. It is important to inform patients that aggregated research data show effects across large populations, and do not necessarily have implications for them personally. It is important to emphasise that all patients are different and have different needs for treatment. To give another example, physicians will often discuss that a therapy “has no evidence to support it” or “does not work” when the patients attending the meeting are receiving that therapy. The patient’s natural reaction is to question whether they should be taking the therapy, and whether their doctor may have made a wrong decision in prescribing it. One patient in the bronchiectasis guidelines task force was receiving a therapy that the panel determined should not be used due to an increase in side-effects in clinical trials. After discussion, it was very clear that the patient had benefited from this treatment. It is important to understand that research and guideline projects look at the balance of risks and benefits across a population, and do not determine whether an individual patient will benefit from a treatment. This distinction is not immediately obvious unless clearly explained to patients. Patients told us that they would prefer to have a single point of contact with whom they can discuss issues as they arise, and from whom they can obtain information. This can be a member of the panel, or someone from a patient organisation such as ELF.
The European Lung Foundation perspective
ELF was founded by the ERS to bring together patients and the public with respiratory professionals to positively influence lung health. ELF encourages healthcare professionals to engage with patients and patient organisation representatives to ensure that patient perspectives are at the centre of their project set-up, decision making and outcomes.
Over the last 5 years, ELF’s remit has expanded significantly as its role has become better known within the ERS, resulting in an increasing number of ERS project chairs engaging with ELF for support in facilitating patient input into their activities. This has resulted in a steep learning curve for ELF and, with increasing experience in this area, and building on the facilitation of patient input into over 15 ERS task forces and projects to date, means that we are continually looking to review and refine our approach.
Our experience of working with EMBARC, which has been a very successful collaboration, forms the basis for the challenges and learning points we have identified for this article and which are outlined in table 3. Many of the recommendations and do’s and don’ts outlined in table 2 also give us an opportunity to improve our ways of working to ensure smoother participation and involvement for patients in the future. Some of the challenges identified here have been responded to already and solutions have been implemented.
Table 3 shows the key challenges we faced specifically in working with EMBARC on their multiple projects and we have illustrated the solutions that have already been implemented in response to these, as well as future recommendations.
Table 3.
Challenges and solutions from a European Lung Foundation perspective
| Project area | Specific challenge | Solutions implemented | Future recommendations |
| Engagement with and management of expectations, project chairs and members | ELF to maintain an overview of multiple project actions and deadlines to ensure patient input co-ordinated effectively and with feasible deadlines. | Open and regular communication between EMBARC, ELF and patient representatives. Shared commitment and enthusiasm by all to ensure positive engagement of, and experience for, patients involved in the projects. |
ELF inclusion in development of project action plans at earliest stage possible. |
| Recruitment of a patient advisory group | Larger than usual response to our invitation for patients to get involved in EMBARC projects resulted in >50 members on our bronchiectasis patient advisory group (rather than ∼6–12). | Defined the >50 members as a “patient reference panel” for wider consultation at key points during projects. From this panel, we engaged with those individuals who wanted to be more involved in working groups. | Potential model for future projects. Benefits of having the wider reference panel: 1)There is a core base of people ready and engaged for consultation at key points; 2)Opportunities for easier recruitment for future projects or if representatives have to drop out due to ill health or other commitments; 3)Wider promotion of project outcomes through the core group. |
| Communication and consultation with wider patient advisory group | Ensuring two-way communication between patient representatives attending task force meetings and wider patient advisory panel to ensure that wider views are represented. | Development of “Conflict of Interest and Confidentiality” form for patient representatives and patient advisory group members to complete prior to involvement in task forces and projects. | Provide clearer guidance and mechanisms for patient representatives to easily give feedback and gather views from the wider patient advisory group. |
| Preparation and training for patient representatives involved in task forces | Lack of detailed, written guidance for patient representatives involved in task force meetings. | Developed guidance booklet including case study from patient representative involved in this task force. | Review guidance and training in light of recommendations raised in this article. |
| Ongoing support for patient representatives | Increasing demands on core group of patients as workload increases. | Ongoing communication with patient representatives and project chairs throughout the project to highlight potential pressure points. | Setting realistic role descriptions, expectations and timelines from the beginning and reviewing these throughout the project. |
| Guidance for task force/project chairs | No defined process. | Clarification of our patient input process to aid discussions and planning (supplementary material). Basic guidance for task force chairs developed. |
Involve patient representatives at initial discussion stage to ensure best patient involvement approaches are used. Review current guidance for task force chairs, to expand and include a checklist of key responsibilities. Include recommendations for keeping ELF involved and up to date in project development and timeline. |
| Face-to-face meetings with patient representatives | Value of face-to-face meetings recognised but posed some difficulties for individual patients around potential risks; also some technology difficulties encountered. | Developed risk protocol document in response to this for use with patients attending face-to-face meetings in future. | Ongoing use and review of risk protocol. |
| Evaluation of patient involvement in projects | Lack of embedded evaluation processes. | Added a question to task force annual review reports about their experience of patient involvement to date, to help capture feedback part-way through the project so can tackle any issues raised. Piloted an evaluation survey for patient advisory group members at end of project (aim to widen this out to other projects). Reflection and production of the content for this article. |
Develop ELF evaluation strategy to identify best ways of capturing experiences of patient involvement, in order to promote high-quality engagement in the future. Suggest involvement of patients and healthcare professionals in evaluation stages. Ongoing informal and open communication with patient representatives to encourage the raising of any issues/problems that can be addressed. |
| Ending a project | How to acknowledge patient participation at the end of projects. | Not yet applicable. | Define process for exit strategy for patient representatives when projects end. Current exploration of maintaining patient advisory groups over longer term. |
One of the solutions we have been able to put in place over the life of the task force project has been to refine our patient input process, which is used as the basis for initial discussions with project leaders and chairs to define the appropriate elements of patient involvement to include within each project. We continually review our approach and ways of working to ensure that we can build on feedback received and adapt where necessary to ensure quality patient input.
Conclusions
Patient involvement in the design, conduct, implementation and dissemination of clinical research and clinical guidelines can greatly enhance the quality and impact of such projects. Here we have described the lessons learned, mistakes made and recommendations for the future developed as a result of the extensive public involvement in the EMBARC project. We hope such information will be of use to researchers planning similar projects in future.
Educational questions
- 1. Which of the following statements regarding patient involvement in research projects is not correct?
- a) The Value+ toolkit defines meaningful patient engagement as giving patients an active role in activities or decisions that will have consequences for the patient community, because of their specific knowledge and relevant experience as patients
- b) ELF can connect researchers with patients and patient organisations in order to facilitate patient involvement in research
- c) It is important to involve patients in research projects at an early stage, ideally at the pre-application stage for grant applications or in the development of protocols
- d) It is highly recommended to involve multiple patients or patient organisations in order to have a broad patient view
- e) Patients providing input into clinical trials must participate in and receive training from the European Patient Ambassador Programme (EPAP)
- 2. Which of the following statements regarding dissemination of research findings are correct, where studies are conducted in collaboration with patients?
- a) Scientific reports are generally poorly accessible for patients and so it is advisable to produce lay versions of published studies
- b) It is advisable to make published research papers open access where possible, so that they are accessible to patients and patient groups as well as the wider public
- c) Scientific journals usually produce lay versions or short summaries of their articles, so there is no requirement for authors to do so
- d) Patients are typically not interested in participating in manuscript publications
- e) ELF facilitates patient involvement in research projects but does not publish manuscripts or get involved in the publication process
- 3. Which of the following statements is true regarding patient involvement in ERS task forces and guidelines?
- a) It is mandatory to include patients as part of the task force
- b) It is a requirement of the GRADE methodology used to generate ERS guidelines that the patient perspective is taken into account when forming recommendations
- c) Patients do not have to declare conflicts of interest as members of task force panels
- d) Patients cannot meet the ICMJE (International Committee of Medical Journal Editors) criteria for authorship and should not be included as authors in a task force document/clinical guideline
- e) Patients’ ideas and preferences should take priority over clinical evidence when forming guideline recommendations
Suggested answers
1. e) Patients providing input into clinical trials may benefit from participating in the EPAP programme, but this is not mandatory. If patients have no training in clinical trial methodology it is advisable for the chairs of the research project to meet with participants and explain in detail what is expected of the patients, and provide information to patients regarding the technical aspects of trial design and conduct.
2. a) and b) Lay versions of published articles are highly recommended and patients can assist with developing these. Open access publishing allows patients to access the original published article. Scientific journals generally do not produce lay versions and so this is something that should be produced by authors or patient organisations. Patients should be given the opportunity to be authors if they meet the criteria for authorship. ELF has extensive experience of publishing.
3. b) The GRADE methodology includes patients’ ideas and preferences as a core part of the evaluation of interventions. It is not mandatory to include patients in guidelines task forces, but it is recommended for the majority of task forces. Patients can have conflicts of interest and these should be declared to the panel where patients participate as members of the panel. Patients can meet the criteria for authorship and should be included if they meet these criteria. Patients’ ideas and preferences are important, but will not usually take priority over clinical evidence formed from systematic literature review in making recommendations.
Disclosures
J.D. Chalmers EDU-0095-2017_Chalmers (1.2MB, pdf)
Footnotes
Supplementary material This article has supplementary material available from breathe.ersjournals.com
Conflict of interest P. Powell and J. Boyd are employees of the European Lung Foundation. Further disclosures can be found alongside this article at breathe.ersjournals.com
References
- 1.Supple D, Roberts A, Hudson V, et al. From tokenism to meaningful engagement: best practices in patient involvement in an EU project. Res Involv Engagem 2015; 1: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gamble C, Dudley L, Allam A, et al. Patient and public involvement in the early stages of clinical trial development: a systematic cohort investigation. BMJ Open 2014; 4: e005234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dudley L, Gamble C, Preston J, et al. What difference does patient and public involvement make and what are its pathways to impact? Qualitative study of patients and researchers from a cohort of randomized clinical trials. PLoS One 2015; 10: e0128817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Involve www.involve.org.uk Date last accessed: May 5, 2017.
- 5.Powell P, Williams S, Smyth D. European Lung Foundation: from local to global. Breathe 2016; 12: 236–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Patients’ Forum The Value+ Toolkit. Available from: www.eu-patient.eu/globalassets/projects/valueplus/value-toolkit.pdf Date last accessed: May 5, 2017. Date last updated: August 29, 2012.
- 7.Domecq JP, Prutsky G, Elraiyah T, et al. Patient engagement in research: a systematic review. BMC Health Serv Res 2014; 14: 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brett J, Staniszewska S, Mockford C, et al. Mapping the impact of patient and public involvement on health and social care research: a systematic review. Health Expect 2014; 17: 637–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boote J, Wong R, Booth A. “Talking the talk or walking the walk?” A bibliometric review of the literature on public involvement in health research published between 1995 and 2009. Health Expect 2015; 18: 44–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chalmers JD, Aliberti S, Polverino E, et al. The EMBARC European Bronchiectasis Registry: protocol for an international observational study. ERJ Open Res 2016; 2: 00081-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aliberti S, Masefield S, Polverino E, et al. Research priorities in bronchiectasis: a consensus statement from the EMBARC Clinical Research Collaboration. Eur Respir J 2016; 48: 632–647. [DOI] [PubMed] [Google Scholar]
- 12.Pasteur MC, Bilton D, Hill AT. British Thoracic Society guideline for non-CF bronchiectasis. Thorax 2010; 65: Suppl. 1, i1–i58. [DOI] [PubMed] [Google Scholar]
- 13.Chalmers JD, McDonnell MJ, Rutherford R, et al. The generalizability of bronchiectasis randomized controlled trials: a multicentre cohort study. Respir Med 2016; 112: 51–58. [DOI] [PubMed] [Google Scholar]
- 14.Chalmers JD, Aliberti S, Blasi F. Management of bronchiectasis in adults. Eur Respir J 2015; 45: 1446–1462. [DOI] [PubMed] [Google Scholar]
- 15.Aliberti S, Hill AT, Mantero M, et al. Quality standards for the management of bronchiectasis in Italy: a national audit. Eur Respir J 2016; 48: 244–248. [DOI] [PubMed] [Google Scholar]
- 16.Lonni S, Chalmers JD, Goeminne PC, et al. Etiology of non-cystic fibrosis bronchiectasis in adults and its correlation to disease severity. Ann Am Thorac Soc 2015; 12: 1764–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandal P, Chalmers JD, Graham C, et al. Atorvastatin as a stable treatment in bronchiectasis: a randomised controlled trial. Lancet Respir Med 2014; 2: 455–463. [DOI] [PubMed] [Google Scholar]
- 18.Suarez-Cuartin G, Chalmers JD, Sibila O. Diagnostic challenges of bronchiectasis. Respir Med 2016; 116: 70–77. [DOI] [PubMed] [Google Scholar]
- 19.Fletcher M. European Lung Foundation: past, present and future. Breathe 2013; 9: 161–163. [Google Scholar]
- 20.Smyth D, Powell P, Masefield S. “Patients Included” in the European Respiratory Society International Congress. Breathe 2015; 11: 249–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wedzicha W, Fletcher M, Powell P. Making ERS guidelines relevant and accessible: involving patients and the public. Breathe 2011; 8: 9–11. [Google Scholar]
- 22.Powell P, Spranger O, Hartl S, et al. Listening to the unmet needs of Europeans with COPD. Breathe 2013; 9: 350–356. [Google Scholar]
- 23.Fletcher M, Bassi I. Patient voices at the ERS International Congress 2014: highlighting LAM. Breathe 2014; 10: 283–285. [Google Scholar]
- 24.Fletcher M. Bringing the patient voice to the ERS Annual Congress. Breathe 2011; 8: 91–94. [Google Scholar]
- 25.Fletcher M. Public and patient involvement in action at the ERS Annual Congress 2013. Breathe 2013; 9: 430–433. [Google Scholar]
- 26.Brozek JL, Akl EA, Compalati E, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 3 of 3. The GRADE approach to developing recommendations. Allergy 2011; 66: 588–595. [DOI] [PubMed] [Google Scholar]
- 27.Andrews J, Guyatt G, Oxman AD, et al. GRADE guidelines: 14. Going from evidence to recommendations: the significance and presentation of recommendations. J Clin Epidemiol 2013; 66: 719–725. [DOI] [PubMed] [Google Scholar]
- 28.Dahm P, Oxman AD, Djulbegovic B, et al. Stakeholders apply the GRADE evidence-to-decision framework to facilitate coverage decisions. J Clin Epidemiol 2017; 86: 219–139. [DOI] [PubMed] [Google Scholar]
- 29.Chalmers JD, Elborn JS. Reclaiming the name “bronchiectasis”. Thorax 2015; 70: 399–400. [DOI] [PubMed] [Google Scholar]
- 30.Blasi F, Chalmers JD, Aliberti S. COPD and bronchiectasis: phenotype, endotype or co-morbidity? COPD 2014; 11: 603–604. [DOI] [PubMed] [Google Scholar]
- 31.Quint JK, Millett ER, Joshi M, et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: a population-based cohort study. Eur Respir J 2016; 47: 186–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.EMBARC Data Access and Publications. www.bronchiectasis.eu/dataaccess Date last accessed: May 5, 2017. Date last updated: 2017.
- 33.Chalmers JD, Moffitt KL, Suarez-Cuartin G, et al. Neutrophil elastase activity is associated with exacerbations and lung function decline in bronchiectasis. Am J Respir Crit Care Med 2017; 195: 1384–1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McDonnell MJ, Aliberti S, Goeminne PC, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med 2016; 4: 969–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Soyza A, McDonnell MJ, Goeminne PC, et al. Bronchiectasis rheumatoid overlap syndrome is an independent risk factor for mortality in patients with bronchiectasis: a multicenter cohort study. Chest 2017; 151: 1247–1254. [DOI] [PubMed] [Google Scholar]
- 36.McDonnell MJ, Aliberti S, Goeminne PC, et al. Multidimensional severity assessment in bronchiectasis: an analysis of seven European cohorts. Thorax 2016; 71: 1110–1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aliberti S, Lonni S, Dore S, et al. Clinical phenotypes in adult patients with bronchiectasis. Eur Respir J 2016; 47: 1113–1122. [DOI] [PubMed] [Google Scholar]
- 38.Finch S, McDonnell MJ, Abo-Leyah H, et al. A comprehensive analysis of the impact of Pseudomonas aeruginosa colonization on prognosis in adult bronchiectasis. Ann Am Thorac Soc 2015; 12: 1602–1611. [DOI] [PubMed] [Google Scholar]
- 39.Chalmers JD, Goeminne P, Aliberti S, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med 2014; 189: 576–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kostyanev T, Bonten MJ, O’Brien S, et al. The Innovative Medicines Initiative’s New Drugs for Bad Bugs programme: European public–private partnerships for the development of new strategies to tackle antibiotic resistance. J Antimicrob Chemother 2016; 71: 290–295. [DOI] [PubMed] [Google Scholar]
- 41.Hardavella G, Bjerg A, Saad N, et al. How to optimise patient and public involvement in your research. Breathe 2015; 11: 223–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chalmers JD, McHugh BJ, Doherty C, et al. Mannose-binding lectin deficiency and disease severity in non-cystic fibrosis bronchiectasis: a prospective study. Lancet Respir Med 2013; 1: 224–232. [DOI] [PubMed] [Google Scholar]
- 43.de Batlle J, Turino C, Sánchez-de-la-Torre A, et al. Predictors of obstructive sleep apnoea in patients admitted for acute coronary syndrome. Eur Respir J 2017; 49: 1600550. [DOI] [PubMed] [Google Scholar]
- 44.Mak KS, van Bommel AC, Stowell C, et al. Defining a standard set of patient-centred outcomes for lung cancer. Eur Respir J 2016; 48: 852–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
J.D. Chalmers EDU-0095-2017_Chalmers (1.2MB, pdf)