Abstract
Background and objectives
Delay in the diagnosis of visceral leishmaniasis (VL) particularly in non-endemic areas is associated with higher mortality. In our experience, we found that marked bone marrow eosinopenia was a very frequent accompaniment of VL and might be a useful clue for the diagnosis, which indicates the opportunity for further morphological assessment. The aim of this study was to describe the hematological characteristics including peripheral blood and bone marrow findings of Yemeni adults and children with VL.
Methods
We conducted a descriptive analytic study to evaluate systematically peripheral blood and bone marrow findings of Yemeni adults and children with VL. Peripheral blood and bone marrow aspiration of patients with bone marrow aspirate confirmed VL were examined. Forty-seven patients with the main age (±SD) of 17.34±11.37 years (Range: 1–60) were included in the study. Fifty-one non-VL subjects with splenomegaly and pancytopenia or bicytopenia served as control group.
Results
All patients with VL had anemia, 41 (87%) leukopenia, 42 (89%) neutropenia, 44 (94%) thrombocytopenia, 42 (89%) eosinopenia, 34 (72%) pancytopenia and 13 (28%) had bicytopenia. In bone marrow examination 40 (85%) showed hypercellularity, 44 (94%) eosinopenia, 24 (51%) dyserythropoiesis, 22 (47%) lymphocytosis, 8 (17%) plasmacytosis, 27 (57%) decreased iron stores and 20 (43%) showed decreased sideroblasts. Comparison of VL patients with the control group showed significantly more frequent peripheral blood eosinopenia and lymphopenia and marrow eosinopenia. There was no significant difference between adults and children in any of the hematological features.
Conclusion
Anemia, leukopenia, neutropenia, thrombocytopenia, eosinopenia, pancytopenia and marked bone marrow eosinopenia were the most common findings. The finding of marked bone marrow eosinopenia is a significant clue for the diagnosis of visceral leishmaniasis in patients who present with splenomegaly associated with cytopenias. This finding is particularly valuable in non-endemic areas.
Keywords: Visceral Leishmaniasis, Yemen, Early Diagnosis, Hematological Features, Bone Marrow Eosinopenia
Introduction
The hematological features of visceral leishmaniasis (VL) have evoked particular interest because of their high frequency and severity and because they cause significant mortality and morbidity.1,2,3 There are frequent reports of the hematological manifestations which describe mainly their relative frequencies in different regions of the world.3,4 Common non-specific hematological features of VL include anemia, leukopenia, thrombocytopenia, and pancytopenia.3,5,6 Such hematological features are also frequently encountered in patients with hematological malignancies such as acute leukemia, lymphomas, and myelodysplastic syndrome as well as various infectious diseases.7 There are also frequent reports of VL presenting as an autoimmune disease mimicking autoimmune hepatitis, primary biliary cirrhosis, rheumatoid arthritis and systemic lupus erythematosus.8,9 Higher rates of morbidity and mortality are consequences of the delay in diagnosis.10,11,12 VL is also reported to be one of the most common causes of fever of unknown origin causing troublesome diagnosis in a European low-income country.13 In addition to the non-specificity of clinical and general laboratory features of VL, the confirmatory laboratory tests with the exception of identification of the parasites in Giemsa stained tissue aspirates, are usually interpreted in the light of clinical and epidemiological data which are not helpful in non-endemic areas.14,15 On the other hand, the sensitivity of bone marrow aspirates, which is comparatively a safer procedure compared to splenic aspirates for identification of the parasite, was found to be proportional to the amount of time spent searching for the amastigotes ( 65.5 percent and 95.4 percent at 5 minutes and one hour respectively).16 Finding a collection of hematological features will help to demand a diligent search to confirm the diagnosis particularly in non-endemic areas. Only a few reports have looked at hematological manifestations as helpful clues for the diagnosis, which included mainly bone marrow cytological features.17,18 In Yemen, Leishmania IgG ELISA is rarely available in some centres and experience showed it to be unreliable because of the high frequency of false positive and false negative results when compared to identification of the parasites in Giemsa stained tissue aspirates. Such findings were also addressed by WHO expert group who reported that a significant proportion of people living in endemic areas with no history of VL is positive for antileishmanial antibodies owing to asymptomatic infections.15 The experts also recommend that in areas of low endemicity more accurate diagnostic algorithms are required that would include parasitology in blood and bone marrow. The role of serology in the diagnosis of VL has been reviewed.19,20 PCR for the diagnosis of leishmania is not available in Yemen, and only one report has been recently published in which PCR was used for research purposes with the collaboration of University of Malaya and reported the first Molecular characterization of VL in Yemen.21 Therefore, identification of the parasites in Giemsa stained bone marrow aspirate smears remains the only reliable diagnostic method for the diagnosis of VL in Yemen.3,22 In our experience, we observed that in addition to known hematological features, the presence of marked bone marrow eosinopenia constitutes a crucial clue to the presence of visceral leishmaniasis in challenging cases. Such evidence prompted a careful review of the smears searching for amastigotes, which were identified -although sometimes with a little and scanty distribution- in all suspected cases showing these two features. The aim of this study is to evaluate systematically the hematological characteristics of Yemeni adults and children with VL including objective documentation of the frequency and degree peripheral and bone marrow eosinopenia to find clues that may help to arrive at the diagnosis early. This procedure by avoiding delay in specific treatment will decrease morbidity and mortality. A full epidemiological study of VL in Yemen is not available. The causative organisms are Leishmania donovani complex (anthroponotic VL) and Leishmania infantum complex (zoonotic VL). The pattern of VL in Yemen derives from the few studies published. The disease seems to be endemic in the country, particularly in Hajjah, Taiz and Amran governorates of the Northern part of the country and Lahj and Abyan governorates of the south of the country.3,22
Materials and Methods
The study is a descriptive analytic study conducted in Sana’a, which is the capital city of Yemen, at the hematology unit of Al-Jomhori teaching hospital which is a referral tertiary teaching hospital. The hematology unit deals with all types of hematological diseases including hematological malignancies which are referred from all over the country. The study included 47 patients with VL who were prospectively evaluated and managed at our center between October 2010 and October 2014. Their diagnosis was confirmed by identification of amastigotes in Giemsa stained bone marrow smears. Complete blood count (CBC) was done for each patient using an automated cell counter (Sysmex Automated machine, Sysmex Corporation, Kobe, Japan), The white blood cell count (WBC) differential and red blood cell (RBC) morphology were confirmed manually by a well-trained laboratory hematologist and adjusted accordingly. One peripheral blood Giemsa stained smear and three bone marrow aspiration Giemsa stained smears were examined by the consultant laboratory and clinical hematologist. Informed consent was obtained from the patients or responsible persons and the study was approved by the Ethical Committee of the Faculty of Medicine and Health Sciences of Sana’a University.
The control group included 51 subjects, randomly selected from the records of 207 non-VL patients, 60 years old or younger (considering that the maximum age for patients with VL was 60 years old), who presented with fever, splenomegaly and pancytopenia or bicytopenia during the period of the study between October 2010 and October 2014. Their presenting CBC and WBC differential were taken before any treatment. They were performed by the same machine and in the same way as for all patients including patients with VL. The bone marrow examination was carried out at initial presentation as part of the evaluation of their splenomegaly and cytopenia. Their marrow aspiration Giemsa stained smears were reviewed to determine the eosinophil series percentage and to compare the results with those of patients with VL. They were examined by the same laboratory and clinical hematologist who reviewed the bone marrow smears of patients with VL.
Definitions
Bone marrow eosinopenia: eosinophil series count of less than 0.3% of total marrow myeloid cells calculated as the average number in at least 20 cellular fields examined i.e. at least 20×200= 4000 cells were counted [Normal range of eosinophils on aspirated bone marrow: 0.3–4.0% and the normal mean: 2.2%].23
Dyserythropoiesis
Presence of dysplastic changes of erythropoiesis including megaloblastic features, binuclear and polynuclear normoblasts and other dyserythropoietic features (e.g. internuclear bridges, nuclear budding) with a frequency of > 5 per 100 erythroid cells
Hypercellular marrow
A cellularity > 50% in adults and > 80% in children.
Increased lymphocytes (marrow)
Lymphocytes > 5% of total non-erythroid cells in adults and > 10% in children.
Increased plasma cells (marrow)
Plasma cells > 5% of total non-erythroid cells in both adults and children.
Hemophagocytosis
Presence in the bone marrow of macrophages which phagocytize blood and bone marrow cells including red cells, erythroblasts, other leukocytes and or platelets.
Evaluation of iron stores
Decreased marrow iron stores: less than one iron-positive cell, on the average for each × 40 field or absent iron-positive cells; increased marrow iron stores: more than two iron-positive cell for each × 40 field. Decreased marrow sideroblasts: sideroblasts less than 3% of total erythroblasts in the marrow.24
Statistical analysis
The data were collected, tabulated and compiled in a computer database. SPSS version 21 was used to analyze data. Frequencies and percentages were used to describe categorical data. Unpaired Independent Samples T test was used to evaluate the comparison between adults and children regarding the means of Hb, PCV, MCV, MCH, WBC, platelet, neutrophil, lymphocyte, monocyte and eosinophil counts. Chi squared test was used to compare the degree of abnormal peripheral blood counts and also the peripheral blood and bone marrow morphological data between adults and children. Unpaired Independent Samples T test was used to evaluate the comparison between Patients with VL and control subjects regarding the means of Hb, WBC, platelet, neutrophil, lymphocyte, monocyte, and eosinophil counts. Chi squared test was used to compare the degree of abnormal peripheral blood counts and bone marrow eosinopenia between VL patients and controls.
Results
Forty-seven (32 males and 15 females) patients with the main age (±SD) of 17.34±11.37 years (Range: 1–60) were included in the study. Of these patients, 28 (59.6%) were adults aged 16–60 years with a mean age (±SD) of 24.3 years ±9.2 and 19 (40.4%) patients were children aged 1–15 years with a mean age (±SD) of 7.1 years ±4.7.
Table 1 shows the mean values of the peripheral blood counts of adults and children with VL and table 2 shows the type and degree of abnormal peripheral blood counts.
Table 1.
The mean values of peripheral blood counts of Yemeni adults and children and with visceral leishmaniasis.
| Parameter | All patients* | Children* (no=19) | Adults* (no=28) | P value |
|---|---|---|---|---|
| Hb (g/dl) | 7.49±1.37 | 7.04±1.39 | 7.83±1.30 | 0.057 |
| PCV (%) | 24.47±4.07 | 24.14±4.43 | 24.96±4.06 | 0.572 |
| MCV (fl) | 75.2±6.16 | 71.44±4.95 | 77.95±5.19 | 0.004 |
| MCH (pg) | 23.74±2.31 | 22.07±2.58 | 24.62±1.1.92 | 0.006 |
| Reticulocyte (%) | 1.57±1.13 | 1.75±1.32 | 1.41±0.93 | 0.465 |
| WBC × 106/L | 2097.87±1304.59 | 2194.74±1089.58 | 1833.78±937.4530 | 0.236 |
| Neutrophil × 106/L | 912.02±999.95 | 607.22±1089.58 | 995.61±778.70 | 0.06 |
| Lymphocyte × 106/L | 992.67±773.71 | 1419.06±852.66 | 605.87±261.69 | <0.001 |
| Eosinophil × 106/L | 14.19±22.20 | 13.28±18.34 | 13.74±25.00 | 0.948 |
| Monocyte × 106/L | 168.14±147.45 | 152.78±121.82 | 171.43±164.36 | 0.690 |
| Platelet × 109/L | 68.53±45.34 | 59.32±45.29 | 77.52±43.86 | 0.178 |
Table 2.
Type and degree of abnormal peripheral blood counts in Yemeni adults and children with visceral leishmaniasis.
| Variable | All patients (no=47) | Children (no=19) | Adults (no=28) | p value |
|---|---|---|---|---|
| Eosinopenia (<40 × 106/L) | 42 (89.4%) | 17 (89.5%) | 25 (89.3%) | 0.950 |
| Absolute eosinopenia (0) | 27 (57.4%) | 11 (57.9%) | 16 (57.1%) | 0.680 |
| Hb <10 (g/dl) | 46 (97.9%) | 18 (94.7%) | 28 (100%) | 0.228 |
| Hb <7.0 (g/dl) | 16 (31.9%) | 8 (42%) | 7 (25%) | 0.249 |
| WBC<3.0 × 109/L | 41 (87.2%) | 16 (84.2%) | 25 (89.3%) | 0.368 |
| Pancytopenia | 34 (72.3%) | 14 (73.7%) | 20 (71.4%) | 0.976 |
| Bicytopenia | 13 (27.7%) | 5 (26.3%) | 8 (28.6%) | 0.976 |
| Platelets <100.0 × 109/L | 39(83%) | 18 (94.7%) | 21 (75%) | 0.115 |
| Platelets <150.0 × 109/L | 44 (93.6%) | 18 (94.7%) | 26 (92.9%) | 0.798 |
| Neutrophil < 1.5 × 109/L | 42 (89.4%) | 19(100%) | 23 (82%) | 0.063 |
| Neutrophil < 1.0 × 109/L | 34 (72.3%) | 16 (84.2%) | 18 (64.3%) | 0.194 |
All patients had moderate to severe anemia (Hb range: 4.6–10.4 g/dl) including 16 (32%) patients who had severe anemia; only one patient had Hb > 10 g/dl (10.4 g/dl).
Forty-one (87%) patients had leukopenia, and 42 (89.4%) patients had neutropenia including 34 (72.3%) patients who had significant neutropenia.
Thrombocytopenia was present in 44 (93.6%) patients including 39 (83%) patients who had significant thrombocytopenia. Eosinopenia was present in 42 (89.4%) patients including 27 (57.4%) patients who had absolute eosinopenia.
All patients had either pancytopenia or bicytopenia: 34 (72.3%) and 13 (27.7%) respectively).
The red blood cell morphological characteristics of Yemeni adults and children with visceral leishmaniasis showed that anisocytosis, anisochromia, and microcytic RBCs were the most common red blood cell morphological findings which were present in 30 (63.8%), 25 (53.2%) and 23 (49%) respectively. Ten (21%) patients had poikilocytosis, and five (10%) had tear drop red blood cells.
Table 3 shows the bone marrow morphological characteristics of Yemeni adults and children with visceral leishmaniasis. Regarding bone marrow morphological findings, marked bone marrow eosinopenia was the most common finding which was seen in 44 (93.6%) patients. Forty (85%) patients had hypercellular marrow, and 24 (51%) patients had dyserythropoiesis. Decreased iron stores were present in 27 (57.4%) patients, and 20 (42.6%) had a reduced number of sideroblasts. Only three (6.4 %) patients had increased iron stores. Hemophagocytosis was recognized in two (4.3) patients, and bone marrow plasmacytosis was seen in eight (17%) patients (Figures 1,2,3).
Table 3.
Bone marrow morphological characteristics of Yemeni adults and children with visceral leishmaniasis.
| Variable | All patients (no=47) | Children (no=19) | Adults (no=28) | p value |
|---|---|---|---|---|
| Hypercellular marrow | 40 (85.1%) | 16(84%) | 24(85.7%) | 0.643 |
| Decreased iron stores | 27 (57.4%) | 8(47%) | 19 (67.9%) | 0.335 |
| Increased iron stores | 3 (6.4%) | 1 (5.3%) | 2 (7.1%) | 0.785 |
| Dyserythropoiesis | 24 (51.1%) | 11(57.9%) | 13 (46.4) | 0.369 |
| Decreased sideroblasts | 20 (42.6%) | 8 (42%) | 12 (42.8%) | 0.785 |
| BM eosinopenia | 44 (93.6%) | 19 (100%) | 25 (89.3%) | 0.214 |
| BM lymphocytosis | 22 (46.8%) | 8 (42%) | 14 (50%) | 0.795 |
| Plasmacytosis | 8 (17%) | 3 (15.8%) | 5 (17.9%) | 0.853 |
| hemophagocytosis | 2 (4.3%) | 1 (5.3%) | 1 (3.6%) | 0.778 |
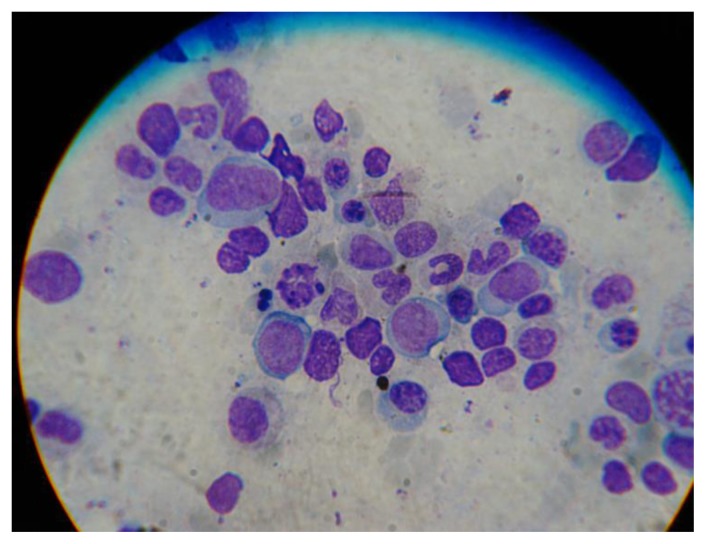
Figure 1.
Bone marrow aspirate smear showing amastigote forms of Leishmania donovani associated with dyserythropoiesis (Giemsa 100×).
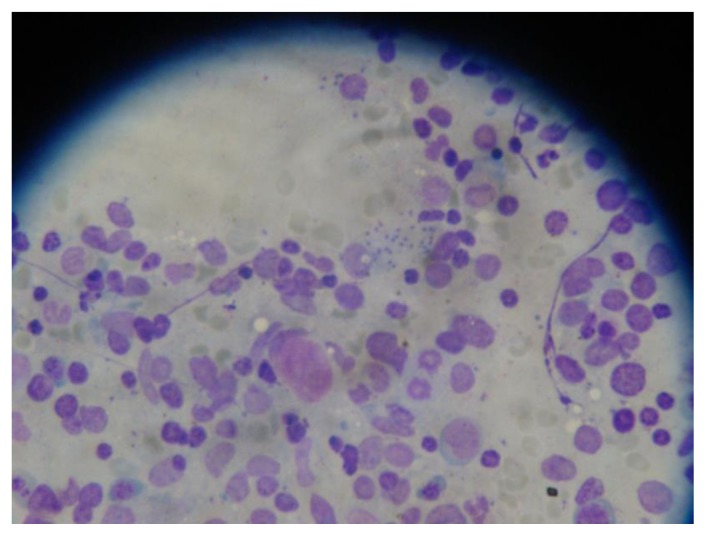
Figure 2.
Bone marrow aspirate smear showing amastigote forms of Leishmania Donovani inside macrophages associated with frequent lymphocytes and dyserythropoiesis (Giemsa 100×).
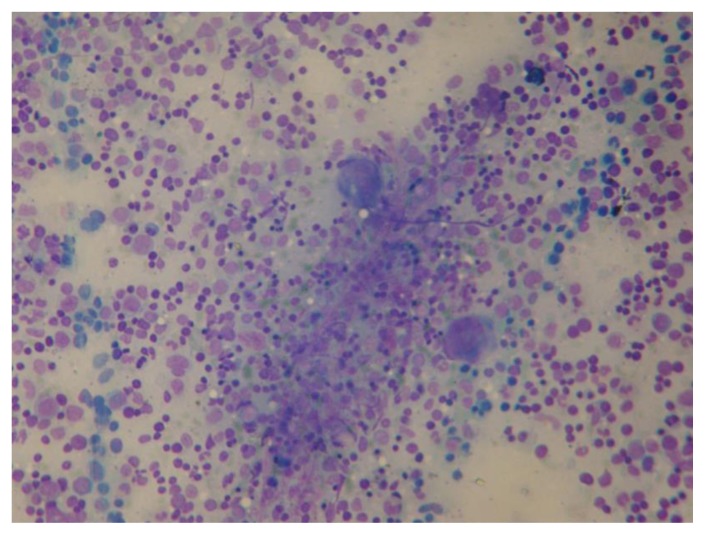
Figure 3.
Bone marrow aspirate smear showing hypercellularity with lymphocytosis and no eosinophils with scattered amastigote forms of Leishmania Donovani (Giemsa 40×).
The control group included 51 subjects (30 males and 21 females) with the main age (±SD) of 20.71±11.92 years (Range: 0.5–60). The mean values of the peripheral blood counts of control subjects was 7.80±1.75 (g/dl) for Hb, 2703.92±826.55 (×106/L) for WBC, 1069.76±626.50 (×106/L) for neutrophils, 1347.76±630.26 (×106/L) for lymphocytes, 88.10±108.84 (×106/L) for eosinophils, 201.06±197.72 (×106/L) for monocytes and 74.65±62.68 (×109/L) for platelets. Comparison of the mean values of peripheral blood counts between patients with VL and control subjects showed no significant difference in any of the above mean values except that patients had significantly lower eosinophil counts (p value 0.000) and lower lymphocyte count (p value 0.014). Table 4 shows comparison of abnormal peripheral blood counts and bone marrow eosinopenia between Yemeni patients with VL and control subjects. Patients had significantly more peripheral blood eosinopenia and lymphopenia and bone marrow eosinopenia compared to control subjects.
Table 4.
Comparison of abnormal peripheral blood counts and bone marrow eosinopenia between Yemeni patients with visceral leishmaniasis and control subjects.
| Variable | patients (no=47) | Control (no=51) | p value |
|---|---|---|---|
| Anemia | 47 | 51 | |
| Eosinopenia (<40 × 106/L) | 42 (89.4%) | 19 (56.9%) | 0.001 |
| WBC<3.0 × 109/L | 41 (87.2%) | 44 (86.3%) | 0.889 |
| Platelets <100.0 × 109/L | 39(83%) | 35 (68.6%) | 0.099 |
| Platelets <150.0 × 109/L | 44 (93.6%) | 46 (90.2%) | 0.825 |
| Neutrophil < 1.5 × 109/L | 42 (89.4%) | 40 (78.4%) | 0.767 |
| Neutrophil < 1.0 × 109/L | 34 (72.3%) | 28 (54.9%) | 0.369 |
| Lymphocyte < 1.0 × 109/L | 25 (53.2%) | 13 (25.5%) | 0.005 |
| Monocyte < 0.2 × 109 | 29 (61.7%) | 33 (64.7%) | 0.758 |
| Bone marrow eosinopenia | 44 (93.6%) | 10 (19.6%) | 0.000 |
Discussion
Our study showed that anemia, leukopenia, neutropenia, thrombocytopenia, eosinopenia, and pancytopenia were the most common peripheral blood findings in patients with VL and that hypercellularity, eosinopenia, dyserythropoiesis, lymphocytosis and decreased marrow iron were the most common bone marrow findings.
Most hematological features including anemia, leukopenia, thrombocytopenia, and pancytopenia are non-specific. Such features are frequent in patients with other infectious diseases, some hematological disorders and some autoimmune collagenous diseases (7,25–28). Diagnosis of VL is straight forward in endemic areas where the disease is suspected and aided by confirmatory laboratory tests including reliable serological tests.14 However, in non-endemic areas, the differential diagnosis includes a broad spectrum of diseases as mentioned above and serological diagnosis is not reliable.15 Finding amastigotes in tissue smears is the most reliable diagnostic test. Splenic aspiration is a risky procedure and is not a usual in non-endemic areas. Bone marrow aspiration remains the safest procedure. However, the sensitivity of such method depends on the time spent examining the smears.16 Paying careful oriented attention and adequate time searching for the parasites increases the sensitivity to around 100%. However, such a time which may take few hours cannot be paid for all patients presenting with the above hematological features because of the high incidence of the diseases presenting with such features. Finding additional clues may limit the number of cases highly suspected of being VL, which need careful, time-consuming study.
The peripheral blood features of our patients which included anemia, thrombocytopenia, leukopenia, bicytopenia, and pancytopenia are not different from those reported from other studies in Asia, Africa, and Mediterranean region or South America.4,29 Hypercellular marrow and dyserythropoiesis were also common in our patient group which is similar to that reported in other studies.30,31 Bone marrow lymphocytosis was also frequent among our patients similar to other studies.6 Our patients also had significant peripheral blood lymphocytopenia. The presence of peripheral blood lymphopenia in association with bone marrow lymphocytosis has been explained by the notion that lymphocytes migrate to the affected lymphoid tissues to build an inflammatory response and that bone marrow lymphocytosis is a compensatory response that provides lymphocytes to organs affected by the parasite.32,33 Only one child and one adult of our patients had bone marrow features of hemophagocytosis. Hemophagocytosis was reported to be a rare occurrence in patients with visceral leishmaniasis causing diagnostic dilemma and unusual presentation.11,34 Our patients showed decreased marrow iron which is consistent with their common finding of microcytic red blood cells. This picture is due to the malnutrition these patients usually have as a consequence of anorexia and is also explained by the fact that the disease affects the poor population predominantly.25,35 Severe anemia, malnutrition and long duration of illness were shown to be associated with an increased risk of death.25,36 These issues should be addressed in evaluating and managing patients with VL. The marked bone marrow eosinopenia associated with marked peripheral blood eosinopenia are the characteristics which were most common in our patients with VL and usually are not reported both together in other simulating illnesses. Bone marrow eosinopenia in VL has not been signaled in humans so far. However, it has been reported in symptomatic canine VL as opposed to asymptomatic canine VL and was found to be correlated with peripheral eosinopenia and it has been regarded together with peripheral blood lymphocytopenia as a biomarker of severe disease.37 Eosinophilic hypoplasia in symptomatic canine VL has been explained by bone marrow dysfunction, which may have contributed to the severe eosinopenia.37,38 On the other hand, Eosinophil infiltration in the lymph-nodes of mice infected by Leishmania major was found to be influenced by sex and parasitic load and that it reflects ineffective inflammation.39 The previous studies in humans on hematological manifestations of VL did not evaluate bone marrow eosinopenia as a feature or as a clue to the diagnosis of the disease. A single study reported three of 18 bone marrow aspirates who had prominent marrow eosinophils.40 However, the authors themselves of the study did not find any report of similar observation in the searched medical literature. We also didn’t find other reports of this finding of marrow eosinophilia. Therefore, secondary causes of eosinophilia could not be excluded in these cases. Furthermore, the percentage of those patients with eosinophilia was too small to regard it a significant finding: 3/18 [16%].40 Our study also showed that there was no significant difference between adults and children regarding peripheral blood and bone marrow eosinopenia or concerning other hematological features.
Conclusions
Based on the above findings we conclude that in the proper clinical setting associated with peripheral blood cytopenias, the finding of marked bone marrow eosinopenia is a critical clue for the diagnosis of symptomatic VL demanding careful, lengthy search for the parasites in bone marrow aspirate smears. This finding is particularly valuable in non-endemic areas.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Pace D. Leishmaniasis. J Infect. 2014;69:S10–18. doi: 10.1016/j.jinf.2014.07.016. https://doi.org/10.1016/j.jinf.2014.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Ready PD. Epidemiolgy of Visceral Leishmaniasis. Clin Epidemiol. 2014;6:147–154. doi: 10.2147/CLEP.S44267. https://doi.org/10.2147/CLEP.S44267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abdul Hamid G, Gobah GA. Clinical and hematological manifestations of visceral leishmaniasis in Yemeni children. Turk J Hematol. 2009;26:25–28. [PubMed] [Google Scholar]
- 4.Sarkari B, Naraki T, Ghatee MA, Abdolahi KS, Davami MH. Visceral Leishmaniasis in Southwestern Iran: A Retrospective Clinico-Hematological Analysis of 380 Consecutive Hospitalized Cases (1999–2014) PLOS ONE. 2016;11(3):e0150406. doi: 10.1371/journal.pone.0150406. https://doi.org/10.1371/journal.pone.0150406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agrawal Y, Sinha AK, Upadhyaya P, Kafle SU, Rijal S, Khanal B. Hematological profile in visceral leishmaniasis. Int J Infect Microbiol. 2013;2(2):39–44. https://doi.org/10.3126/ijim.v2i2.8320. [Google Scholar]
- 6.Varma N, Naseem S. Hematologic Changes in Visceral Leishmaniasis/Kala Azar. Indian J Hematol Blood Transfus. 2010;26:78–78. doi: 10.1007/s12288-010-0027-1. https://doi.org/10.1007/s12288-010-0027-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jain A, Naniwadekar M. An etiological reappraisal of pancytopenia - largest series reported to date from a single tertiary care teaching hospital. BMC Hematol. 2013;13:10. doi: 10.1186/2052-1839-13-10. https://doi.org/10.1186/2052-1839-13-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tunccan OG, Tufan A, Telli G, Akyürek N, Pamukçuoglu M, Yilmaz G, et al. Visceral Leishmaniasis Mimicking Autoimmune Hepatitis, Primary Biliary Cirrhosis, and Systemic Lupus Erythematosus Overlap. Korean J Parasitol. 2012;50(2):133–136. doi: 10.3347/kjp.2012.50.2.133. https://doi.org/10.3347/kjp.2012.50.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cakar M, Cinar M, Yilmaz S, Sayin S, Ozgur G, Pay S. A case of leishmaniasis with a lupus-like presentation. Seminar Arthritis Rheum. 2015;45(1):e3–4. doi: 10.1016/j.semarthrit.2015.04.001. https://doi.org/10.1016/j.semarthrit.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Prasad R, Muthusami S, Pandey N, Tilak V, Shukla J, Mishra OP. Unusual presentations of Visceral leishmaniasis. Indian J Pediatr. 2009;76:843–845. doi: 10.1007/s12098-009-0148-4. https://doi.org/10.1007/s12098-009-0148-4. [DOI] [PubMed] [Google Scholar]
- 11.Celik U, Alabaz D, Alhan E, Bayram I, Celik T. Diagnostic dilemma in an adolescent boy: hemophagocytic syndrome in association with kala azar. Am J Med Sci. 2007;334:139–141. doi: 10.1097/MAJ.0b013e31812e97f4. https://doi.org/10.1097/MAJ.0b013e31812e97f4. [DOI] [PubMed] [Google Scholar]
- 12.Driemeier M, de Oliveira PA, Druzian AF, Lopes Brum GF, Pontes ER, Dorval ME, Paniago AM. Late diagnosis: a factor associated with death from visceral leishmaniasis in elderly patients. Pathog Glob Health. 2015;109(6):283–9. doi: 10.1179/2047773215Y.0000000029. https://doi.org/10.1179/2047773215Y.0000000029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosilkovski M, Dimozva M, Stevanovic M, Cvetkovska VS, Duganovska M. Fever of unknown origin--diagnostic methods in a European developing country. Voinosanit Pregl. 2016;73(6):553–8. doi: 10.2298/vsp140827050b. https://doi.org/10.2298/VSP140827050B. [DOI] [PubMed] [Google Scholar]
- 14.Sakkas H, Gartzonika C, Levidiotou S. Laboratory diagnosis of human visceral leishmaniasis. J Vector Borne Dis. 2016;53(1):8–16. [PubMed] [Google Scholar]
- 15.Report of a meeting of the WHO Expert Committee on the control of Leishmaniasis; Geneve. 22–26 March 2010; [accessed: April, 2, 2017]. Available at: whqlibdoc.who.int. [Google Scholar]
- 16.da Silva MR, Stewart JM, Costa CH. Sensitivity of bone marrow aspirates in the diagnosis of visceral leishmaniasis. AM J Trop Med Hyg. 2005;72(6):811–4. [PubMed] [Google Scholar]
- 17.Bhatia P, Haldar D, Varma N, Marwaha RK, Varma S. A Case Series Highlighting the Relative Frequencies of common/uncommon and Atypical/Unusual Hematological Findings on bone marrow examination in cases of Visceral Leishmaniasis. Mediterr J Hematol Infect Dis. 2011;3:e2011035. doi: 10.4084/MJHID.2011.035. https://doi.org/10.4084/mjhid.2011.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chaufal SS, Pant P, Chachra U, Singh P, Thapliyal N, Rawat V. Role of Haematological Changes in Predicting Occurrence of Leishmaniasis- A Study in Kumaon Region of Uttarakhand. J Clin Diag Res. 2016;10(5):FC39–34. doi: 10.7860/JCDR/2016/15438.7885. https://doi.org/10.7860/JCDR/2016/15438.7885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pagliano P, Ascione T, Di Flumeri G, Boccia G, De Caro F. Visceral leishmaniasis in immunocompromised: diagnostic and therapeutic approach and evaluation of the recently released IDSA guidelines. Infez Med. 2016;24(4):265–271. [PubMed] [Google Scholar]
- 20.Franceschini E, Puzzolante C, Menozzi M, Rossi L, Bedini A, Orlando G, Gennari W, Meacc Mi, Rugna G, Carra E, Codeluppi M, Mussini C. Clinical and Microbiological Characteristics of Visceral Leishmaniasis Outbreak in a Northern Italian Nonendemic Area: A Retrospective Observational Study. BioMed Research International. 2016;2016:7. doi: 10.1155/2016/6481028. Article ID 6481028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahdy MAK, Al-Mekhlafi AM, Abdul-Ghani R, Saif-Ali R, Al-Mekhlafi HM, Al-Eryani SM, Lim YAL, Mahmud R. First Molecular Characterization of Leishmania Species causing Visceral Leishmaniasis among Childeren in Yemen. PLOS ONE. 2016;11(3):e0151265. doi: 10.1371/journal.pone.0151265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-Ghazaly J, Al-Dubai W. The clinical and biochemical characteristics of Yemeni adults and children with visceral leishmaniasis and the differences between them: a prospective cross-sectional study before and after treatment. Trop Doct. 2016;46(4):224–231. doi: 10.1177/0049475515622862. https://doi.org/10.1177/0049475515622862. [DOI] [PubMed] [Google Scholar]
- 23.Bates I, Burthern J. Bone marrow biopsy. In: Bain B, Bates I, Laffan M, Lewis SM, editors. Dacie and Lewis Practical Haematology. 11th edition. Churchill Livingstone Elsevier; 2012. p. 130. [Google Scholar]
- 24.Ryan DH. Examination of the marrow. In: Kaushansky K, Lichtman M, Beutler E, Kipps TJ, Seligsohn U, Prchal JT, editors. Williams Hematology. 8th edition. McGraw Hill Medical; 2011. p. 33. [Google Scholar]
- 25.Collin S, Davidson R, Ritmeijer K, Keus K, Melaku Y, Kipngetich S, Davies C. Conflict and kala-azar: determinants of adverse outcomes of kala-azar among patients in southern Sudan. Clin Infect Dis. 2004;38(5):612–19. doi: 10.1086/381203. https://doi.org/10.1086/381203. [DOI] [PubMed] [Google Scholar]
- 26.Kopterides P, Halikias S, Tsavaris N. Visceral leishmaniasis masquerading as myelodysplasia. Am J Hematol. 2003;74:198–199. doi: 10.1002/ajh.10408. https://doi.org/10.1002/ajh.10408. [DOI] [PubMed] [Google Scholar]
- 27.Arlet JB, Capron L, Pouchot J. Visceral leishmaniasis mimicking systemic lupus erythematosus. J Clin Rheumatol. 2010;16:203–204. doi: 10.1097/RHU.0b013e3181dfd26f. https://doi.org/10.1097/RHU.0b013e3181dfd26f. [DOI] [PubMed] [Google Scholar]
- 28.Pagliano P, Costantini S, Gradoni L, Faella FS, Spasiano A, Mascarella G, Prossomariti L, Fusco U, Ricchi P. Case report: Distinguishing visceral leishmaniasis from intolerance to pegylated interferon-a in a thalassemic splenectomized patient treated for chronic hepatitis C. American Journal of Tropical Medicine and Hygiene. 2008;79(1):9–11. [PubMed] [Google Scholar]
- 29.Chakrabarti S, Sarkar S, Goswami BK, Sarkar N, Das S. Clinico-hematological profile of visceral leishmaniasis among immunocompetent patients. Southeast Asian J Trop Med Public Health. 2013;44(2):143–9. [PubMed] [Google Scholar]
- 30.Bain BJ. Dyserythropoiesis in visceral leishmaniasis. American J Hematol. 2010;85(10):781. doi: 10.1002/ajh.21787. https://doi.org/10.1002/ajh.21787. [DOI] [PubMed] [Google Scholar]
- 31.Temiz F, Gurbuz BB, Leblebisatan G, Ozkan A, Canoz PY, Harmanogullari S, Gezer H, Tumogor G, Turgut M. An association of leishmaniasis and dyserythropoiesis in children. Indian J Hematol Blood Transfus. 2014;30(1):19–21. doi: 10.1007/s12288-012-0189-0. https://doi.org/10.1007/s12288-012-0189-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bourdoiseau G, Bonnefont C, Magnol JP, Saint-Andre I, Chabanne L. Lymphocyte subset abnormalities in canine leishmaniasis. Vet ImmunolImmunopathol. 1997;1997;56:345–351. doi: 10.1016/s0165-2427(96)05768-6. https://doi.org/10.1016/S0165-2427(96)05768-6. [DOI] [PubMed] [Google Scholar]
- 33.Reis AB, Teixeira-Carvalho A, Giunchetti RC, Guerra LL, Carvalho MG, et al. Phenotypic features of circulating leucocytes as immunological markers for clinical status and bone marrow parasite density in dogs naturally infected by Leishmania chagasi. Clin Exp Immunol. 2006;146:303–311. doi: 10.1111/j.1365-2249.2006.03206.x. https://doi.org/10.1111/j.1365-2249.2006.03206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scalzone M, Ruggiero A, Mastsngelo S, Trombatore G, Ridola V, Maurii P, Riccardi R. Hemophagocytic lymphohistiocytosis and visceral leishmaniasis in children: case report and systematic review of literature. J Infect Dev Ctries. 2016;10(1):103–8. doi: 10.3855/jidc.6385. https://doi.org/10.3855/jidc.6385. [DOI] [PubMed] [Google Scholar]
- 35.Jeronimo SMB, de Queiroz Sousa A, Pearson RD. Leishmaniasis. In: Guerrant RL, Walker DH, Weller PF, editors. Tropical infectious diseases: principles, pathogens and practice. Churchill Livingstone Elsevier; Edinburgh, Scotland: 2006. pp. 1095–1113. [Google Scholar]
- 36.Houweling TA, Karim-Kos HE, Kulik Mc, Stolk WA, Haagsama JA, Lenk EJ, Richardus JH, de Vlas SJ. Socioeconomic Inequalities in Neglected Tropical Diseases: A Systematic Review. J Clin Exp Hepatol. 2016;6(2):146–8. doi: 10.1371/journal.pntd.0004546. https://doi.org/10.1371/journal.pntd.0004546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nicolato RC, Abreu RT, Roatt BM, Aguiar-Soares RDO, Reis LES, Carvalho MG, Carneiro CM, Giunchetti RC, et al. Clinical Forms of Canine Visceral Leishmaniasis in Naturally Leishmania infantum–Infected Dogs and Related Myelogram and Hemogram Changes. PLOS ONE. 2013;8(12):e82947. doi: 10.1371/journal.pone.0082947. https://doi.org/10.1371/journal.pone.0082947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tryphonas L, Zawidzka Z, Bernard MA, Janzen EA. Visceral leishmaniasis in a dog: clinical, hematological and pathological observations. Can J Comp Med. 1997;41:1–12. [PMC free article] [PubMed] [Google Scholar]
- 39.Salpnickova M, Volkova V, Cepickova M, Kobets T, Sima M, Svobodova M, et al. Gene-specific sex effects on eosinophil infiltration in leishmaniasis. Biolgy of Sex Differences. 2016;7:59. doi: 10.1186/s13293-016-0117-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dhingra KK, Gupta P, Saroha V, Setia N, Khurana N, Singh T. Morphological findings in bone marrow biopsy and aspirate smears of visceral Kala Azar: A review. Indian J Pathol Microbiol. 2010;53(1):96–100. doi: 10.4103/0377-4929.59193. https://doi.org/10.4103/0377-4929.59193. [DOI] [PubMed] [Google Scholar]