Abstract
Background
The number of children visiting Emergency Departments (EDs) is increasing in Lithuania; therefore, the aim of this study was to determine the factors influencing the parental decision to bring their child to the ED for a minor illness that could be managed in a primary healthcare setting, and to compare parents’ and medical professionals’ attitudes toward a child’s health status and need for urgent care.
Material/Methods
A prospective observational study was performed at the tertiary-level teaching Children’s Hospital in Vilnius. A total of 381 patients’ parents were interviewed using an original questionnaire based on Andersen’s behavioral model of healthcare utilization; in addition, the medical records of patients were reviewed to identify factors that might have an impact on parental decisions to bring their child to the ED for a minor health problem. The study participants were enrolled from October 1, 2013 to August 31, 2014. The urgency of medical care needed to be provided to the patients was evaluated by a tertiary-level triage system.
Results
Based on the assessment of the triage nurses, the need for emergency care to patients was distributed as follows: 298 patients (78.2%) needed non-urgent care and 83 patients (21.8%) needed urgent care. More than one-third (38.8%) of the parents reported that they came to the ED due to their child’s urgent care need and worsened child’s health; however, the opinion of ED professionals indicated only a fifth of patients required urgent care. Parents who brought their children to the ED without physician referral were five times more likely to visit the ED during evening hours and on weekends (OR=5.416; 95% CI, 3.259–8.99; p<0.001). The decision to come to the ED without visiting a primary care physician was made more often by parents with a higher income (OR=2.153; 95% CI, 1.167–3.97) and those who came due to children having rash (OR=4.303; 95% CI, 1.089–16.995) or fever (OR=3.463; 95% CI, 1.01–11.876). Older parents were 2.07 (95% CI, 1.1224–3.506) times more likely to evaluate their child’s health unfavorably than younger parents.
Conclusions
We identified predisposing, enabling, and need factors that influenced the parents’ decision to bring their child to the ED for minor health problems that could be managed by a primary care physician. Parents assessed their child’s condition more critically and thought that their child required urgent medical aid more frequently than healthcare professionals.
MeSH Keywords: Behavior and Behavior Mechanisms; Emergency Service, Hospital; Health Services Misuse; Hospitals, Pediatric; Parents; Primary Health Care
Background
Hospital Emergency Departments (EDs) are part of the emergency healthcare system, connecting out-of-hospital services and in-patient services provided at the hospital. Primary healthcare services are provided at EDs during nonworking hours of primary healthcare centers.
In recent years, the flow of patients to hospital EDs has increased due to health condition issues that could be solved by a family physician or a pharmacist without using in-patient hospital healthcare resources. The number of unnecessary, primary healthcare-related visits to hospital EDs has increased [1–3]. Parents bring their children to EDs due to minor illnesses and non-urgent health conditions. Generally, children arrive at the EDs due to fever, pain, trauma, respiratory problems, and digestive system problems.
The unnecessary use of EDs worsens the overall accessibility and quality of emergency services, increases healthcare costs, and reduces continuity of healthcare services [4,5]. The overcrowding of EDs is related to the increased rates of hospitalization and patients’ dissatisfaction with such ED services [6–9]. Problems related to accessibility of primary healthcare services are of utmost importance in the overcrowding of EDs [10].
The number of children visiting hospital EDs is increasing in Lithuania; therefore, the aim of this study was to determine the factors influencing the parental decision to bring their child to the ED for a minor illness that could be managed in a primary healthcare setting, and to compare parents’ and medical professionals’ attitudes toward a child’s health status and the need for urgent care.
Material and Methods
A prospective observational study was performed at the tertiary-level teaching Children’s Hospital in Vilnius. A total of 381 parents or legal representatives of children who were brought to the Pediatric Emergency Department of the Children’s Hospital and provided with out-patient care for a minor illness, were interviewed using an original questionnaire; medical records of patients were reviewed in order to identify factors that had an impact on the parental decision to come to the hospital ED for a minor illness. Minor illnesses were defined as conditions that “require little or no medical intervention” [11] and can be appropriately managed in a primary care setting.
The study participants were enrolled from October 1, 2013 to August 31, 2014. Parents were eligible to participate if their child was less than 18 years of age and was assigned a nurse triage category “yellow” (urgent) or “green” (non-urgent), and they were Lithuanian-speaking. The parents of trauma and surgery patients and those who were assigned a nurse triage category “red” (emergent) were excluded from the study.
The factors that influenced the parental decision to contact the ED of Children’s Hospital for minor illness were identified with the help of the theoretical Andersen’s behavioral model of healthcare utilization, which is widely used in studies analyzing healthcare consumption and availability. The patient is a central figure in this model, influenced by three groups of factors: predisposing, enabling, and need factors [12–15].
A questionnaire consisting of two parts was used: part A had 10 questions and part B had 20 questions. Part A of the questionnaire assessed the factors that affect the parental decision to come to the ED of Children’s Hospital. In this part of the questionnaire, parents had to indicate their answers using a Likert scale by circling the number best revealing their opinion from 1 (strongly disagree) to 5 (strongly agree). Part B of the questionnaire comprised 20 general questions about the respondents’ demographic and social characteristics, child’s health, and primary healthcare services.
The study instrument was tested for its validity and reliability. Factorial analysis was applied to examine eligibility of questionnaire variables. The Kaiser-Meyer-Olkin index (KMO) for A1–A10 questions was 0.79. The Cronbach alpha coefficient was used to test internal consistency reliability of the questionnaire scales. The internal consistency of the scale was good (α=0.72).
Patients’ health records were reviewed and the following variables were assessed: patient’s age and gender, arrival time (during working hours, after working hours, or at night), triage category, patient’s condition (easy, average, severe, extremely severe), length of stay in the ED, clinical diagnosis, arrival nature (with or without referral), medical services, diagnostic and therapeutic actions. Parents’ health literacy was evaluated by comparing parents’ and medical staff’s opinion on the: severity of child’s condition, emergency level, main symptoms, and need for tests and treatment.
Informed consent was obtained from each participant. The study was approved by the Vilnius Regional Biomedical Research Ethics Committee.
The results were summarized by applying descriptive statistics, correlation analysis, logistic regression analysis, and factorial analysis. The level of statistical significance was set at p<0.05.
Results
Of all the 381 patients included in the study, 50.4% were boys and 49.6% were girls. The mean age of the patients was 3.6 years (range, 1 month to 17 years). The demographic, social, and economic characteristics of the selected participants (patients and parents) are shown in Table 1. The selected variables were compared by the nature of arrival (arrived without or with healthcare professional’s referral) (Table 1).
Table 1.
The demographic, social, and economic characteristics of patients and parents (n=381).
| Indicator | Without referral, total number 248 n (%) | With referral, total number 133 n (%) | Total number 381 n (%) | χ2, p |
|---|---|---|---|---|
| Parental education |
χ2=10.735 df=2 p=0.005 (p<0.01) |
|||
| Secondary | 19 (7.7) | 19 (14.4) | 38 (10) | |
| College degree | 53 (21.4) | 41 (31.1) | 94 (24.7) | |
| University degree | 176 (71) | 72 (54.5) | 248 (65.3) | |
| Parental age |
χ2=4.944 p=0.176 (p>0.05) |
|||
| Less than 35 years | 169 (68.1) | 95 (72) | 264 (69.4) | |
| More than 35 years | 79 (31.8) | 37 (28) | 116 (30.5) | |
| Monthly income of a family (n=287) |
χ2=13.888 df=2 p=0.001 (p<0.01) |
|||
| Less than 580 Eur | 24 (13.4) | 27 (25.0) | 51 (17.8) | |
| 580–1 160 Eur | 92 (51.4) | 63 (58.3) | 155 (54.0) | |
| More than 1 161 Eur | 63 (35.3) | 18 (16.7) | 81 (28.3) | |
| Time to go to primary health care institution |
χ2=1.190 df=2 p=0.552 (p>0.05) |
|||
| Less than 15 min. | 125 (50.2) | 74 (56.1) | 199 (52.2) | |
| 15–30 min. | 103 (41.4) | 48 (36.4) | 151 (39.6) | |
| More than 30 min. | 21 (8.4) | 10 (7.6) | 31 (8.1) | |
| Time to go to children’s hospital |
χ2=14.945 df=2 p=0.002 (p<0.01) |
|||
| Less than 15 min. | 76 (30.6) | 24 (18.2) | 100 (26.3) | |
| 15–30 min. | 128 (51.6) | 66 (50.0) | 194 (51.1) | |
| More than 30 min. | 44 (17.7) | 38 (28.8) | 86 (22.6) |
χ2=5.494 df=3 p=0.240 (p>0.05) |
| Child’s age, years | ||||
| <1 | 42 (16.9) | 32 (24.1) | 74 (19.4) | |
| 1–2 | 89 (35.9) | 43 (32.3) | 132 (34.6) | |
| 3–7 | 97 (39.1) | 42 (31.6) | 139 (36.5) | |
| >8 | 21 (8.5) | 15 (11.3) | 36 (9.4) | |
| Child’s gender |
χ2=0.911 p=0.498 (p>0.05) |
|||
| Girl | 122 (49.2) | 67 (50.4) | 189 (50.4) | |
| Boy | 126 (50.8) | 66 (49.6) | 192 (49.6) |
χ2 – chi square; df – degrees of freedom; P – significance level.
Factors that influenced parental decision to go to the Children’s Hospital ED
During the working hours of the primary healthcare center (workdays from 7 AM to 7 PM), parents brought their children to the ED with physician’s or ambulance staff’s referral more often than during non-working hours. Parents who brought their children without referral were five times more likely to visit the ED in the evening hours and weekends (OR=5.416; 95% CI, 3.259–8.99; p<0.001).
Fifty-six patients (14.7%) were brought to the ED by ambulance. An ambulance brought patients more frequently during evening hours and working days (p<0.05). Children less than three years of age were brought by ambulance more often compared with their older counterparts (p<0.05).
Our study showed that more educated parents brought their children by themselves significantly more often. The decision to arrive independently, without visiting a primary care physician, was taken more often by parents with a higher income (OR=2.153; 95% CI, 1.167–3.97; p=0.014). Parents brought their 3–7-year-old children significantly more often (OR=2.571; 95% CI, 1.545–12.139; p<0.001), whereas infants were more often referred by physicians and ambulance professionals (p<0.05).
Location of living place (residence) was a significant social factor determining the use of services. Since the majority of those who came to the ED lived in the city of Vilnius, we studied whether they lived closer to their primary healthcare facility or to the Children’s Hospital. More than half (52.2%) of the children who presented to the hospital ED lived 15 minutes away from their primary healthcare facility, whereas only 26.3% of the patients needed the same time to reach the ED. The time to reach a primary healthcare institution and the time to reach the Children’s Hospital ED correlated significantly (r=0.212, p<0.001). However, more patients who arrived without referral lived closer to the hospital (p<0.01), and vice versa, children who lived further away from the ED were referred to the ED by a physician more frequently.
A total of 160 children (42.1%) had not visited the hospital ED during the last 12 months; 173 (45.5%) visited it one or two times, and 47 (12.4%) visited it three or more times. Parents who brought their children to the hospital themselves were significantly more likely to visit the ED.
Child’s overall health was rated as very good by 106 parents (27.9%); as good by 201 parents (52.9%); and as moderate or poor, by 73 parents (19.2%). Parents who had children less than three years of age rated their child’s health as very good significantly more often (p<0.001) compared to those who had children older than three years (38.5% and 15.4%, respectively). Twenty-two parents (10.7%) with children younger than three years and 51 parents (29.1%) with children older than three years indicated their child’s health as being moderate or poor (p<0.001).
We compared parents’ opinions about their child’s health depending on the parent’s age: 84.5% of the parents younger than 35 years old rated their child’s health as good or very good, while among those parents aged more than 35 years, fewer (72.4%) gave such an assessment (p<0.05). Based on multivariate logistic regression analysis, parents belonging to the older age group were 2.07 times as likely to evaluate their child’s health unfavorably (95% CI, 1.1224–3.506).
We also looked at parental education and found that the evaluation of their child’s health did not differ significantly (χ2=5.554, df=4, p=0.235). However, child’s health was rated as very good by significantly more parents when the child lived with both parents (χ2=8.083, df=2, p=0.018).
Parents with higher family incomes rated their child’s health as very good significantly more often than those with low incomes (χ2=7.145, df=4, p<0.05).
The evaluation of child’s health and the frequency of visits to the hospital ED correlated significantly (r=0.2, p=0.002). Child’s health was rated as very good significantly more often by parents of a child who did not visit the ED in the last 12 months or visited the ED one to two times compared with parents who had children who visited the ED more than three times (n=56, 35.0% and n=47, 27.2% versus n=3, 6.4%, respectively; p<0.01).
The distribution of the mean scores of parental responses is presented in Table 2.
Table 2.
Distribution of the mean scores of parental responses (n=381).
| Factors that could have led to the parents’ decision to come to the ED | Mean (SD) |
|---|---|
| 1. My child’s health has never been as bad as now | 3.02 (1.26) |
| 2. We arrived because of the necessity of tests to determine the causes of my child’s disease | 4.35 (1.0) |
| 3. I am aware about similar symptoms to another child who was very ill | 3.14 (1.34) |
| 4. I know that I acted correctly, but I still want to check whether or not | 4.01 (1.07) |
| 5. I have to take special care of my child when he or she gets sick or gets trauma, because he/she has poorer health than his/her peers | 2.61 (1.5) |
| 6. The hospital ED only can provide my child with required aid | 3.87 (1.16) |
| 7. The person whom I trust advised me to bring my child to the hospital ED | 3.49 (1.53) |
| 8. I learned important information through the media, which led me to apply to the ED for my child’s health check-up | 2.5 (1.37) |
| 9. Medicines and medical aid, which my child got at home, did not help | 3.5 (1.28) |
| 10. The hospital ED is the best place where I can take my child to | 4.33 (0.92) |
| Total | 3.38 (0.67) |
Comparison of parents’ and medical professionals’ attitudes toward child’s condition and need for medical interventions
The urgency of medical aid provided to the patients was evaluated by a tertiary-level triage system utilized at the Children’s Hospital. Based on the assessment of the triage nurses working in the ED of Children’s Hospital, the need for emergency care for patients was distributed as follows: 298 patients (78.2%) needed non-urgent and 83 patients (21.8%) needed urgent care.
More than one-third (38.8%) of the parents reported that they arrived at the ED due to urgent care need and especially worsened child’s health; however, based on the opinion of professionals, only a fifth of patients required urgent care.
In the questionnaire, the parents had to name a child’s health disorder (worrying symptoms), which encouraged them to come to the ED, and the child’s condition on arrival to the ED (need factors). Parents’ answers and evaluation by ED physicians were compared. The evaluation of child’s condition revealed that 73 respondents (19.3%) stated that they could not assess their child’s condition; the assessment of the remaining respondents were distributed as follows: easy, 18 (4.7%); average, 168 (44.1%); and severe/extremely severe, 122 (32.0%). Whereas, a total of 58 (15.2%) ED physicians assessed child’s condition as satisfactory and 323 (88.3%) as average. According to the physicians’ opinion, there were no patients in the group with a severe/extremely severe condition.
Non-parametric Kendall correlation analysis showed that the triage color and the assessment of severity of the child’s disease correlated significantly (r=0.2, p<0.001). Of the 168 parents who rated their child’s condition as average on arrival to the ED, a significantly greater proportion of these patients needed non-urgent care (triage category “green”) than urgent care (triage category “yellow”) (n=140, 58.8% and n=28, 40.0%, respectively). On the contrary, of the 122 parents who reported their child’s condition as severe/extremely severe on arrival to the ED, a significantly lower percentage of the patients needed non-urgent care than urgent care (n=81, 34.0% and n=41, 58.6%, respectively) (Figure 1).
Figure 1.
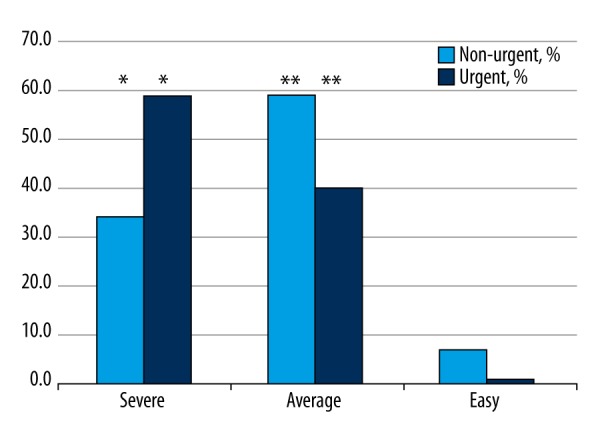
Percentage distribution of child’s health assessment (in parents’ opinion) by the triage category (χ2=14.758, df=2, p=0.001, *,** p<0.05).
Of the 148 parents who indicated that they arrived at the ED due to especially worsened child’s health; only 27 (18.2%) children required emergency aid. Despite emergency aid required by only a small percentage of patients, the condition of 119 children (80.4%) was assessed by ED physicians as being of average severity.
Acute upper respiratory tract infections (n=117), fever (n=84), gastrointestinal infections and functional disorders (n=78), skin and mucous membrane pathology (n=50), and lower respiratory tract diseases (n=30) were the most common diagnoses made by physicians. Younger children were brought to the ED due to fever and breathing difficulties more often than older children (p<0.05).
Parents who had children suffering from skin and mucous membranes diseases (diseases occurring with rashes) (OR=4.303; 95% CI, 1.089–16.995) and fever (OR=3.463; 95% CI, 1.01–11.876) were more likely to bring their children to the ED without a referral than parents of children with other diseases.
A total of 310 children (81.4%) underwent at least one test. At least one medication was prescribed to 316 children (83.0%), and 65 children (17.0%) were not given any treatment in the ED.
Discussion
Using Andersen’s behavioral model of healthcare utilization, we identified the predisposing, enabling, and need factors that influenced the parental decision to bring the child to the Children’s Hospital ED for minor health problems that could be managed in a primary healthcare setting. We found only a few studies that evaluated the demographic and social characteristics of the parents making a decision for their children [4,16,17].
Predisposing factors
Predisposing factors are factors that existed before the onset of the disease, such as demographic and social characteristics attributed to parents and parental attitudes and beliefs about their child’s health and the healthcare system. The following significant factors that influenced parental decision to arrive at the ED without referral were identified: child’s age (parents brought their three- to seven -year-old children without referral significantly more often); parental education (parents with higher education brought their children without referral significantly more often); family income (parents with better income brought their children without referral more often); and distance to the ED (patients who brought their children without referral lived closer to the hospital). Younger parents and parents with a higher income considered their child’s health as very good significantly more often compared to parents with a low income. ED services were used more often by parents arriving without referral and those who rated their child’s health as average or bad.
Low parental health literacy is known to be a predisposing factor for the increased use of ED services, especially when the child’s condition does not require emergency aid. Parents having lower health literacy bring their children to the ED three times more frequently for non-urgent care than those with a sufficient level of health literacy [18,19]. Parents having lower health literacy have difficulties interpreting information about medications, their dosage, and the use of aids, which leads to unnecessary consumption of specialized healthcare services for chronically ill children [20,21].
In our study, we found that the health of the majority of children who presented to the ED was assessed by their parents as very good or good, and only a fifth of respondents rated his/her child’s condition as average or bad. Differences in the assessment of a child’s health were observed based on demographic and social factors. We found that younger parents and parents with a higher income assessed their child’s health as very good significantly more often compared to older parents and parents who had a lower income. Chambers et al. in 2011 also reported that parents who thought their child’s health to be worse used healthcare services provided at the ED more often [22].
Enabling factors
This study highlighted the following factors enabling the utilization of services based on Andersen’s model, and having an influence on the parents’ decision to come to the ED: insufficient accessibility of primary healthcare services in the case of acute disease of a child (less than one-third of the children were consulted by a family physician before arriving at the ED); lack of information (parents were insufficiently informed regarding where primary healthcare services for their child should be provided when their family physician was not available (non-working hours); parents’ opinion about the ED (parents thought that the ED of the hospital was the best place to take a child in cases of acute disease).
Berry et al. in 2008 found that parents expected that their child’s health problem would be solved more quickly at the ED, trusted the qualifications of the professionals at the hospital more, and thought the possibilities of examinations offered a better possible assessment [4]. One study carried out in the United States showed that 62% of parents who come to the ED considered it the most convenient place for their child to receive healthcare services [23].
The majority of the children who came to the ED of Children’s Hospital did not have a referring consultation with a family physician. Long waiting time and limited access to a family physician on the same day of the hospital visit has been shown to increase the number of visits to the EDs due to health problems attributed to the competence of family physician [4,24,25]. Previous studies have reported that parents identified bad accessibility to primary healthcare services and inconvenient working hours as reasons why they decided to come to the hospital ED [4,10,24,26].
Low spatial density of primary healthcare institutions and long distance to primary healthcare institutions from place of residence are strongly related to unnecessary use of ED services [27]. Unnecessary and frequent use of ED services is related to good geographic accessibility – patients living closer to the hospital tend to use the services of the ED more often [28–30]. Similar results were obtained also in our study.
Need factors
Andersen’s model describes the factors that stimulate the utilization of healthcare services based on patients’ needs. Factors predetermined by subjective needs include parent’s self-assessment of their child’s health condition and identification of worrying symptoms. Objective healthcare needs are based on physicians’ opinions regarding urgency of care and severity of the condition, as well as diagnostic and treatment measures required [13,15]. The results of our study showed that parents were mostly influenced by the following factors predetermined by need: child’s condition (parents assessed their child’s condition more critically than healthcare professional assessments); urgency of medical aid (parents thought more often that their child needed urgent medical aid as compared to the ED professionals); diagnosis (parents tended to bring their children to the ED more often by themselves if their child had skin and mucous membrane diseases and fever); possibilities of immediate examination (at least one test was done for 81.4% of the children); and administration of necessary treatment (at least one medication was prescribed to 83.0% of the children).
Some studies have shown that parents most often assess their children’s condition more critically than healthcare professionals [29,31]. This was also found in our study where one-third of the parents assessed their child’s condition as severe and extremely severe despite this category of patient being excluded from the study. The analysis of our study results revealed that healthcare service consumers, namely children’s parents in our study, possess insufficient knowledge about the necessity for urgent care for their children and basic first aid after noticing common symptoms in a child such as fever, sickness, diarrhea, or cold symptoms [32]. Measures enabling parents to distinguish when a child requires emergency aid at the ED and when it is possible to provide aid at home or in a family physician’s practice are necessary [21,31,33]. Parental age as well as education and socioeconomic status are prognostic factors for healthcare service consumption due to a child’s diseases [34].
Our results showed that a decision to come to the ED depended on the parental opinion about their child’s health, the severity of their child’s condition, the urgency of medical aid, and the symptoms of the child’s disease raising concern for the parents. In general, parents’ opinion was different from that of the ED staff member opinion, except for identification of the main disease symptoms. Literature describes the differences between the opinions of parents, primary healthcare physicians, and the ED staff members in the assessment of a child’s health, severity of a child’s condition, and urgency of medical aid in cases of “minor” diseases not requiring emergency aid [35–37].
Interventions increasing parents’ health literacy may reduce the utilization of ED services for non-emergency medical aid. In the literature, measures such as introduction of additional fees paid by patients, changes in responsibility of institutions providing primary healthcare services, and application of methodological recommendations are suggested to reduce the overuse of ED services; however, the greatest effect in reduction of the utilization of the ED services may be achieved through parent training [19,38].
Limitations
There are several limitations to this study. First, the study recruited study participants from one pediatric ED providing care to children of Vilnius city and its district; therefore, the study sample may not be representative. Another limitation was that it was not possible for us to monitor changes in patient’s health. Moreover, we did not assess whether the study participants had any chronic diseases that could influence parents’ answers about their child’s health at arrival at the ED.
Recommendations
In the future, efforts should be focused on increasing the accessibility to primary healthcare services for children and ensuring that pediatric patients receive consultation by their primary care physician on the day they seek medical help. Moreover, the provision of primary healthcare services after working hours and on weekends and improvement in parental health literacy need to be addressed.
Conclusions
By applying Andersen’s behavioral model of healthcare utilization, we identified predisposing, enabling, and need factors that influenced the parental decision to bring their child to the Children’s Hospital ED for minor health problems that could be managed by a primary care physician. Parents and the ED staff judged the severity of child’s condition differently.
Footnotes
Source of support: Departmental sources
Competing interests
The authors declare that they have no competing interests.
References
- 1.Akenroye AT, Thurm CW, Neuman MI, et al. Prevalence and predictors of return visits to pediatric Emergency departments. J Hosp Med. 2014;9(12):779–87. doi: 10.1002/jhm.2273. [DOI] [PubMed] [Google Scholar]
- 2.Easter JS, Bachur R. Physicians’ assessment of pediatric returns to the Emergency Department. J Emerg Med. 2013;44(3):682–88. doi: 10.1016/j.jemermed.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Cho CS, Shapiro DJ, Cabana MD, et al. A national depiction of children with return visits to the Emergency Department within 72 hours, 2001–2007. Pediatr Emerg Care. 2012;28(7):606–10. doi: 10.1097/PEC.0b013e31825cf7cf. [DOI] [PubMed] [Google Scholar]
- 4.Berry A, Brousseau D, Brotanek JM, et al. Why do parents bring children to the Emergency Department for nonurgent conditions? A qualitative study. Ambul Pediatr. 2008;8(6):360–67. doi: 10.1016/j.ambp.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Ben-Isaac E1, Schrager SM, Keefer M, Chen AY. National profile of nonemergent pediatric Emergency Department visits. Pediatrics. 2010;125(3):454–59. doi: 10.1542/peds.2009-0544. [DOI] [PubMed] [Google Scholar]
- 6.Carter EJ, Pouch SM, Larson EL. The relationship between Emergency Department crowding and patient outcomes: A systematic review. J Nurs Scholarsh. 2014;46(2):106–15. doi: 10.1111/jnu.12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun BC, Hsia RY, Weiss RE, et al. Effect of Emergency Department crowding on outcomes of admitted patients. Ann Emerg Med. 2013;61(6):605–11.e6. doi: 10.1016/j.annemergmed.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsia RY, Asch SM, Weiss RE, et al. Is Emergency Department crowding associated with increased “bounceback” admissions? Med Care. 2013;51(11):1008–14. doi: 10.1097/MLR.0b013e3182a98310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tekwani KL, Kerem Y, Mistry CD, et al. Emergency Department crowding is associated with reduced satisfaction scores in patients discharged from the Emergency Department. West J Emerg Med. 2013;14(1):11–15. doi: 10.5811/westjem.2011.11.11456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hummel K, Mohler MJ, Clemens CJ, Duncan B. Why parents use the Emergency Department during evening hours for nonemergent pediatric care. Clin Pediatr (Phila) 2014;53(11):1055–61. doi: 10.1177/0009922814540988. [DOI] [PubMed] [Google Scholar]
- 11.The Royal Pharmaceutical Society of Great Britain. Better Management of Minor Ailments Using the Pharmacist. 2003. [accessed on 29 December 2016]. Available at http://faculty.ksu.edu.sa/hisham/Documents/RPSGB_Files_/1/bettmanminail.pdf.
- 12.Fasoli DR, Glickman ME, Eisen SV. Predisposing characteristics, enabling resources and need as predictors of utilization and clinical outcomes for veterans receiving mental health services. Med Care. 2010;48(4):288–95. doi: 10.1097/mlr.0b013e3181cafbe3. [DOI] [PubMed] [Google Scholar]
- 13.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of health services Use: A systematic review of studies from 1998–2011. Psychosoc Med. 2012;9 doi: 10.3205/psm000089. Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heider D, Matschinger H, Müller H, et al. Health care costs in the elderly in Germany: An analysis applying Andersen’s behavioral model of health care utilization. BMC Health Serv Res. 2014;14:71. doi: 10.1186/1472-6963-14-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 16.Hendry SJ, Beattie TF, Heaney D. Minor illness and injury: Factors influencing attendance at a paediatric accident and Emergency Department. Arch Dis Child. 2005;90(6):629–33. doi: 10.1136/adc.2004.049502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moon TD, Laurens MB, Weimer SM, Levy JA. Nonemergent emergency room utilization for an inner-city pediatric population. Pediatr Emerg Care. 2005;21(6):363–66. doi: 10.1097/01.pec.0000166725.76685.4a. [DOI] [PubMed] [Google Scholar]
- 18.Stanley R, Zimmerman J, Hashikawa C, Clark SJ. Appropriateness of children’s nonurgent visits to selected Michigan Emergency Departments. Pediatr Emerg Care. 2007;23(8):532–36. doi: 10.1097/PEC.0b013e318128f84a. [DOI] [PubMed] [Google Scholar]
- 19.Morrison AK, Myrvik MP, Brousseau DC, et al. The relationship between parent health literacy and pediatric Emergency Department utilization: A systematic review. Acad Pediatr. 2013;13(5):421–29. doi: 10.1016/j.acap.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herman A, Young KD, Espitia D, Fu N, Farshidi A. Impact of a health literacy intervention on pediatric Emergency Department use. Pediatr Emerg Care. 2009;25(7):434–38. doi: 10.1097/PEC.0b013e3181ab78c7. [DOI] [PubMed] [Google Scholar]
- 21.Herman A, Jackson P. Empowering low-income parents with skills to reduce excess pediatric emergency room and clinic visits through a tailored low literacy training intervention. J Health Commun. 2010;15(8):895–910. doi: 10.1080/10810730.2010.522228. [DOI] [PubMed] [Google Scholar]
- 22.Chambers PL, Mahabee-Gittens EM, Leonard AC. Vulnerable child syndrome, parental perception of child vulnerability, and Emergency Department usage. Pediatr Emerg Care. 2011;27(11):1009–13. doi: 10.1097/PEC.0b013e318235bb4f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alessandrini EA, Lavelle JM, Grenfell S, et al. Return visits to a pediatric Emergency Department. Pediatr Emerg Care. 2004;20(3):166–71. doi: 10.1097/01.pec.0000117924.65522.a1. [DOI] [PubMed] [Google Scholar]
- 24.Brousseau DC, Bergholte J, Gorelick MH. The effect of prior interactions with a primary care provider on nonurgent pediatric Emergency Department use. Arch Pediatr Adolesc Med. 2004;158(1):78–82. doi: 10.1001/archpedi.158.1.78. [DOI] [PubMed] [Google Scholar]
- 25.Brousseau DC, Hoffmann RG, Nattinger AB, et al. Quality of primary care and subsequent pediatric Emergency Department utilization. Pediatrics. 2007;119(6):1131–38. doi: 10.1542/peds.2006-3518. [DOI] [PubMed] [Google Scholar]
- 26.Stockwell MS, Findley SE, Irigoyen M, et al. Change in parental reasons for use of an urban pediatric Emergency Department in the past decade. Pediatr Emerg Care. 2010;26(3):181–85. doi: 10.1097/PEC.0b013e3181d1dfc7. [DOI] [PubMed] [Google Scholar]
- 27.Mathison DJ, Chamberlain JM, Cowan NM, et al. Primary care spatial density and nonurgent Emergency Department utilization: A new methodology for evaluating access to care. Acad Pediatr. 2013;13(3):278–85. doi: 10.1016/j.acap.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 28.Afilalo J, Marinovich A, Afilalo M, et al. Nonurgent Emergency Department patient characteristics and barriers to primary care. Acad Emerg Med. 2004;11(12):1302–10. doi: 10.1197/j.aem.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 29.Farchi S, Polo A, Franco F, et al. Primary paediatric care models and non-urgent Emergency Department utilization: An area-based cohort study. BMC Fam Pract. 2010;11:32. doi: 10.1186/1471-2296-11-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grafstein E, Wilson D, Stenstrom R, et al. A regional survey to determine factors influencing patient choices in selecting a particular Emergency Department for care. Acad Emerg Med. 2013;20(1):63–70. doi: 10.1111/acem.12063. [DOI] [PubMed] [Google Scholar]
- 31.Williams A, O’Rourke P, Keogh S. Making choices: Why parents present to the Emergency Department for non-urgent care. Arch Dis Child. 2009;94(10):817–20. doi: 10.1136/adc.2008.149823. [DOI] [PubMed] [Google Scholar]
- 32.Kubicek K, Liu D, Beaudin C, et al. A profile of nonurgent Emergency Department use in an urban pediatric hospital. Pediatr Emerg Care. 2012;28(10):977–84. doi: 10.1097/PEC.0b013e31826c9aab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doobinin KA, Heidt-Davis PE, Gross TK, Isaacman DJ, et al. Nonurgent pediatric Emergency Department visits: Care-seeking behavior and parental knowledge of insurance. Pediatr Emerg Care. 2003;19(1):10–14. doi: 10.1097/00006565-200302000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Ogunlesi TA, Olanrewaju DM. Socio-demographic factors and appropriate health care-seeking behavior for childhood illnesses. J Trop Pediatr. 2010;56(6):379–85. doi: 10.1093/tropej/fmq009. [DOI] [PubMed] [Google Scholar]
- 35.Salami O, Salvador J, Vega R. Reasons for nonurgent pediatric Emergency Department visits: Perceptions of health care providers and caregivers. Pediatr Emerg Care. 2012;28(1):43–46. doi: 10.1097/PEC.0b013e31823f2412. [DOI] [PubMed] [Google Scholar]
- 36.Fieldston ES, Alpern ER, Nadel FM, et al. A qualitative assessment of reasons for nonurgent visits to the Emergency Department: Parent and health professional opinions. Pediatr Emerg Care. 2012;28(3):220–25. doi: 10.1097/PEC.0b013e318248b431. [DOI] [PubMed] [Google Scholar]
- 37.Sturm JJ, Hirsh DA, Lee EK, et al. Practice characteristics that influence nonurgent pediatric Emergency Department utilization. Acad Pediatr. 2010;10(1):70–74. doi: 10.1016/j.acap.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 38.Morgan SR, et al. Non-Emergency Department interventions to reduce ED utilization: A systematic review. Acad Emerg Med. 2013;20(10):969–85. doi: 10.1111/acem.12219. [DOI] [PMC free article] [PubMed] [Google Scholar]


