Abstract
Many people newly diagnosed with HIV are lost to follow-up before timely initiation of antiretroviral therapy (ART). A randomised controlled trial (RCT), WelTel Kenya1, demonstrated the effectiveness of the WelTel text messaging intervention to improve clinical outcomes among patients initiating ART. In preparation for WelTel Retain, an RCT that will evaluate the effect of the intervention to retain patients in care immediately following HIV diagnosis, we conducted an informative qualitative study with people living with HIV (n = 15) and healthcare providers (HCP) (n = 5) in October 2012. Study objectives included exploring the experiences of people living with HIV who have attempted to engage in HIV care, the use of cell phones in everyday life, and perceptions of communicating via text message with HCP. Participants were recruited through convenience sampling. Semi-structured, qualitative interviews were conducted and recorded, transcribed verbatim and analysed using NVivo software. Analysis was guided by the Theory of Reasoned Action and the Technology Acceptance Model. Results indicate that while individuals have many motivators for engaging in care after diagnosis, structural and individual barriers including poverty, depression and fear of stigma prevent them from doing so. All participants had access to a mobile phone, and most were comfortable communicating through text messages, or were willing to learn. Both people living with HIV and HCP felt that increased communication via the text messaging intervention has the potential to enable early identification of problems, leading to timely problem solving that may improve retention and engagement in care during the first year after diagnosis.
Keywords: engagement in care, HIV, mobile health, sub-Saharan Africa
Introduction
Patient engagement in care and treatment adherence is critical to achieving the full benefits of antiretroviral therapy (ART) among people living with HIV or AIDS (PLWHA). Engaging PLWHA at all points along the cascade of care is central to transforming the management of the disease from a fatal condition to a chronic one (Gardner et al. 2011). Early engagement has pronounced implications for effective disease management, including the treatment and prevention of co-morbidities, CD4 monitoring and the timely initiation of ART (Smith et al. 2013). Improved management can significantly reduce future health system and patient costs, and can decrease further transmission of HIV. Retaining individuals who have initiated ART in care is challenging, however, with a recent review estimating that 20% of patients in resource-limited settings are lost to follow-up within 12 months of initiating therapy (Fox and Rosen 2010). For ART-ineligible patients, a study in Kenya estimated clinic retention at 12 months at 63% (Kohler et al. 2011).
Interventions to increase retention in care are emerging. Evidence of their efficacy is weak or limited, however, due to methodological issues including inadequate study design and small sample sizes (Scanlon and Vreeman 2013). Patient-focused interventions shown to have a positive effect on loss to follow-up include financing transportation costs in Uganda (Emenyonu et al. 2010), and the introduction of free co-trimoxazole to ART-ineligible patients in Kenya (Kohler et al. 2011). Other studies have examined health service delivery (Jaffar et al. 2009, Sanne et al. 2010, Selke et al. 2010), including investigating the cost effectiveness of interventions that prevent loss to follow-up (Losina et al. 2009). Barriers related to engaging in care are both structural, such as healthcare delivery, poverty, lack of infrastructure and lack of education (Coetzee et al. 2011); and individual, such as depression, abusive relationship, mistrust of clinics and healthcare providers (HCPs) (Smith et al. 2013, Smillie et al. 2014).
An intervention that addresses both structural and individual barriers may hold the most potential for increasing engagement (McNairy and El-Sadr 2012). Mobile health (mHealth) is an emerging area of disease management that has the potential to improve patient adherence to prolonged treatment regimens and support care (Lester et al. 2006, Wei et al. 2011). The WelTelKenya1 study demonstrated that a text-messaging intervention is effective in improving adherence to medication and viral load suppression in HIV-infected individuals who had initiated ART (Lester et al. 2010). It is not yet known, however, if mHealth interventions offer an effective approach to improve retention starting before ART initiation, in the first year following HIV diagnosis. In preparation for a randomised controlled trial (RCT) to determine the effect of the WelTel intervention on retention in care in the first 12 months after diagnosis (van der Kop et al. 2013), we conducted a qualitative study with PLWHA and HCPs at the study site to inform implementation.
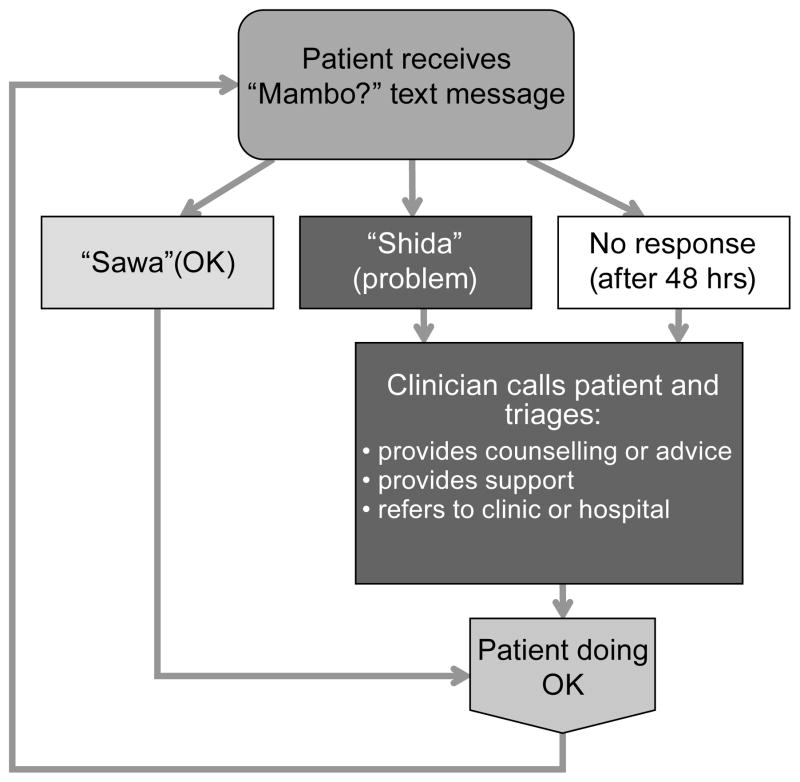
The WelTel intervention involves a weekly text message via short messaging service (SMS) to check in on how patients are doing and provide them the opportunity to identify whether assistance is required (Figure 1). For example, on Monday mornings, an automated text message from a central computer platform at the clinic will be sent to intervention arm participants asking ‘Mambo?’ (Kiswahili for ‘How are you?’). Participants will be instructed to indicate within 48 hours of receiving the message either that they are well (e.g., ‘OK’ or ‘Sawa’) or that they have a problem (e.g., ‘Problem’ or ‘Shida’). A nurse experienced in HIV care will follow up all participants who identify a problem. The nurse will call those who do not respond after 48 hours to enquire as to their status. The purpose of this informative qualitative research was to gain an understanding of: 1) the perceptions and experiences of PLWHA who have attempted to engage in HIV care; and 2) the use of cell phones in everyday life, including perceptions of communicating via text message with HCPs. In the context of this study, engagement in care is defined as returning to care for treatment following diagnosis.
Figure 1.
The WelTel intervention
Methods
Study setting
This study took place at the Kibera Community Health Centre (KCHC), an African Medical and Research Foundation (AMREF) clinic in Nairobi, Kenya, serving over 4 000 HIV infected individuals. The health centre is a comprehensive care clinic, and there are no direct costs to patients for HIV/AIDS care and treatment.
The clinic is located in the heart of Kibera, one of the largest informal settlements in Africa, with an ethnically diverse population of approximately 170 000 people (KNBS 2010). The population the clinic serves lacks or has minimal access to services such as education, water, sanitation and other public services. Transport infrastructure is minimal. HIV prevalence among adults is estimated at 13% (Dalal et al. 2013).
Participants
In October 2012, a total of 5 HCPs and 15 client participants were recruited through convenience sampling (Table 1). Eligibility criterion for healthcare professionals was employment at KCHC. PLWHA were eligible if they were KCHC clients, ≥18 years old and HIV-positive. The eligibility criterion for client participants was positive HIV status. Allsparticipants provided written informed consent to participate in the study. Ethical approval was granted by the AMREF Ethics and Scientific Review Committee. To protect participant anonymity, all names are pseudonyms
Table 1.
Patient demographics [n (%)]
| Gender | Female: 11 (73%) |
| Male: 4 (27%) | |
| Age | Median: 29 years |
| Range: 23–46 years | |
| Marital Status | Married: 9 (60%) |
| Widow: 1 (7%) | |
| Single: 2 (13%) | |
| Separated/divorced: 3 (20%) | |
| Children | Yes: 15 (100%) |
| Education level | Never been: 1 (8%) |
| Primary school: 8 (53%) | |
| Secondary school: 4(26%) | |
| University / Other: 2 (13%) | |
| Living in Kibera | Yes: 10 (67%) |
| No: 5 (33%) | |
| Employment | Employed: 1 (7%) |
| Self-employed: 4 (26%) | |
| Casual labour: 8 (53%) | |
| Unemployed: 1 (7%) | |
| Other: 1 (7%) |
Data collection
Semi-structured interviews using an interview guide were conducted to ensure common themes, and topics were explored across interviews. Questions were open-ended to obtain participants’ perspectives about their experiences. Interviews were conducted in English, with a translator fluent in Kiswahili and English present to assist. The interviews lasted from 20–60 minutes, were recorded, translated into English by a bilingual translator (when necessary), and transcribed verbatim. Interview topics included barriers and facilitators to attending the clinic and adhering to medication, availability of emotional support, use of cell phones in everyday life, and the acceptability of using text messaging to communicate about issues related to HIV care.
Data analysis
Interview data were analysed using thematic analysis. Interview transcripts were read multiple times by two researchers who coded for important concepts, events and experiences. Once a consistent coding framework was established, transcripts were coded using NVivo 9 (QSR International Pty Ltd, Doncaster, Australia) software. To increase reliability, 20% of the transcripts were double coded. Data were selected and reviewed for important themes related to: 1) individual behaviours and attitudes towards HIV care; 2) the use of cell phones in everyday life; and 3) preferences for the proposed mHealth intervention.
Guiding analytic theory
The collection and analysis of data was guided by the Theory of Reasoned Action (TRA) and the Technology Acceptance Model (TAM) (Davis et al. 1989). The TRA posits that a person’s behaviour can be determined by considering three factors: 1) the subjective norms associated with the behaviour, defined as whether or not people important to the individual believe they should perform the behaviour or not; 2) the individual’s attitude towards the behaviour; and 3) an individual’s intention to engage in a behaviour. This theory guided analysis of results related to participants’ discussion of engaging in HIV care.
The TRA was adapted by Davis et al. (1989) for the realm of user acceptance of information systems, resulting in the TAM. Davis et al. (1989) identified two distinct attitudes that could predict the adoption of a new information system: perceived ease of use and usefulness. Usefulness is defined as “the degree to which a person believes that using a particular system would enhance his or her job performance” and ease of use as, “the degree to which an individual believes that using a particular system would be free of physical and mental effort” (Davis et al. 1989: 320). We adapted job performance to engagement in care. For further use of TRA and TAM in relation to the WelTel intervention, see Smillie et al. (2014).
Results
Perceptions and experiences of engaging in HIV care
Experiences returning to care
Client participants were asked about their experiences returning to a clinic after receiving a diagnosis, and what facilitated or prevented them from doing so. Two main issues arose when participants described their experience returning for care: First, returning to receive care was directly influenced by the manner in which client participants were treated by staff — being treated with respect and kindness was a determining factor in returning for follow-up care. Compared to other clinics where patients felt rushed and did not feel that the staff had a caring attitude, client participants described the KCHC clinic as offering quality service with respectful interactions between patients and reception staff, nurses and doctors: ‘The services are good… immediately we entered yesterday, a nurse came and she talked to us politely and she introduced us to another nurse. Went quick and they managed to convince us to take a test because my wife was pregnant. [We] agreed but we had not planned for that …The counsellor there talked to us well, everything just went on smooth’ (Patrick, age 35).
The HCPs echoed the importance of the client/provider relationship, describing the importance of treating clients with respect and dignity by using patients’ first names, listening, being patient and allowing people to discuss their fears. Many HCP and client participants noted the importance and value of the counselling sessions (patients who are diagnosed receive up to four counselling sessions), and that this was a motivation to return: ‘It is because the one who counselled me said that if I came back and we work together, then I would have a chance to live. So it is not the end of life. What he said motivated me to come back’ (Sarah, age 28).
Secondly, client participants return to care for the practical reason of obtaining free treatment. Having access to free medication and receiving prompt service when prescriptions were needed were both highlighted as important. HCPs added that PLWHA return to the clinic to learn their test results and to receive counselling. Other reasons noted by HCPs include coming for a second opinion or because they had become severely ill. The clinic offers co-trimoxazole to those who are ART ineligible, and many HCPs believe that this may improve retention in pre-ART care as patients will return to pick up their drugs. One client participant described being offered co-trimoxazole: ‘I was positive, they [KCHC] immediately produced the Septrin and told me don’t worry this will help you not to get the other diseases. So, there are other clinics that you go and get tested, you are told you are positive then “go home”. Nothing else, they just tell you, you are positive… So [KCHC] are nice because they keep on encouraging you… Whenever you are sick they told you are not supposed to pay anything, so you come you have free treatment here so they are nice and l like them’ (Rachel, age 33). A few HCPs also explained, however, that despite their attempts to educate and counsel clients, some on co-trimoxazole will see their CD4 counts increase and will conclude that they no longer require medication so will not return to the clinic.
Current facilitators to retaining individuals in care
Client participants were asked about any reminder methods they used to attend appointments and/or take medication. Most participants had a strategy, including recording appointments in a calendar or diary, setting reminders on their mobile phone, using a timer to remind them to take their medication, and asking someone to remind them. Some participants said they would not forget because they, ‘just keep it all in my head’ (Sharon, age 38). Finally, client participants described how family members and friends, who were also HIV-positive offered support to accept their diagnosis, attend appointments and take medications: ‘But why God, I cried for two weeks, but my, my husband comforted me, very much with a lot of love and care. So nowadays I am very okay, I know that there is still life’ (Rachel, age 33). A few participants felt they had no one to confide in, and were totally alone: ‘so far am just alone because [I] am the breadwinner of everybody, the family… At home, they expect to get something from me, my parents they expect to get something from me, my children need school fees’ (David, age 42).
Barriers to retention in care
While retention at the KCHC clinic was described by the HCPs as fairly good, instances of missed appointments still occurred. The most prevalent comments by HCPs concerned stigma — clients may want to attend a different clinic for fear that they will run into someone they know: ‘One of the main barriers that we encounter is the issue of stigmatization. Most of the patients tend to want to keep things to themselves, some of them even move out of where they live they go to another place or for example if a health care worker knows where they stay, they will decide to go to another place so that they are not found. For others disclosure is an issue because [for example] a mother has brought the child and the mother does not want the child to know’ (Joseph, HCP).
When clients default on treatment and miss appointments, a HCP will visit them at their home. When the client first enrols in the clinic, they are asked where they live, both the address and nearby landmarks. One HCP explained that by asking so many questions, it makes it difficult for the client to lie about where they live. Tracking patients is not only time consuming, but also difficult as people are prone to moving if they think a HCP will come to their village and disclose their HIV status. To mitigate this, HCPs try and visit everyone in the area so as not to identify those who are HIV-positive. If patients do not answer their phones when a HCP calls using the clinic phone, the clinicians will sometimes use their personal phones with better success.
Lack of regular and local employment was cited by client participants as a major barrier to attending appointments. Most client participants work on a temporary or on-call basis or have to relocate for work, making regular clinic attendance difficult. ‘[Work] can make me … miss my appointment. Because if you get absent today, tomorrow, someone will not keep you, they will just tell you go out’ (David, age 42). Other reasons included being too sick to travel and not wanting to leave their children. HCPs also noted travel and affordable transport as barriers to care. To reduce the number of clinic appointments, KCHC has recently started CD4 testing at the same appointment that patients test positive for HIV, thus eliminating the extra step of having to return to the clinic at a later date. HCPs will also try to connect patients with facilities that are close to home to make accessing care easier. Language barriers were also listed as an occasional barrier to care: ‘most of the patients at least can understand Swahili, some even English, in case we find some who can’t understand, especially Swahili, then we have to get one health care worker who can speak their language’ (John, HCP). Finally, HCPs spoke of instilling the need for behaviour change in terms of adherence to medications, condom use and restricting alcohol and drug intake is challenging.
Client participant cell phone use and perceptions of the WelTel intervention
Access to and use of mobile phones was common by all client participants. The participants in this study were accustomed to using mobile phones, with all client participants having access to a mobile phone (15/15), either their own or shared. Just under half of those asked already knew how to use text messaging (6/12). Most client participants (9/15) expressed interest in communicating with their HCP team through text messaging and believed that the WelTel intervention would be convenient and helpful in managing their care. ‘Texting the health concerns will help. It is good. I think when you are texting matters relating to health, that is when you can speak about everything that you are having. I don’t have any concerns, you are free. You can be more free when you text’ (Joshua, age 35). Of particular interest was receiving more timely responses from clinicians regarding information on diet and medications, and the fact that they would not need to come to the clinic to have questions answered.
A few client participants expressed concerns around compromised privacy, including the possibility of someone looking through their phone: ‘if someone else reads the message and they find out about my status’ (Joan, age 31). Other issues included the phone running out of battery due to limited access to electricity and missing a message from the HCP.
HCPs perceptions of the WelTel intervention
HCPs believed there were many potential benefits of the mHealth intervention. All believed that increased contact with patients would be undoubtedly positive. HCPs would have a better understanding of an individual’s issues if they were in contact on a more regularly, would be able to deal with issues including questions on side effects in a more timely manner, and would be better prepared for appointments: ‘I think it will help because as much as we think we have dealt with all our clients issues, there might be an aspect to that [which has] not been touched even when they were coming. So if we use this kind of a method actually l believe we will be able to understand our clients better’ (Mercy, HCP). One HCP had concerns that the programme would increase their workload. However, most did not feel this would be an issue, particularly as the messages are sent out automatically. A few believed that the programme may decrease their workload as they would be able to deal with minor issues outside of appointments, and may not have to travel to client’s homes for follow-up visits with clients who had missed their participants. They also discussed the potential benefits to the patients. HCPs also posited that clients may receive an increase in psychosocial support that may lead to increased trust, a benefit that was discussed repeatedly. Being able to communicate through text messaging may reduce fears of HCPs showing up at their house, particularly for those who have not disclosed their status: ‘Some don’t like to be followed up because of the issue that the neighbours will know I am positive. They do not want people around them to know. And I must say that using the phone would reduce that, as it is just a text message’ (Joseph HCP). Finally, text messages may serve as an effective reminder for appointments.
HCPs had a few concerns regarding the intervention, including their ability to interpret a client’s message. They stressed that whoever reads and responds to messages must know the client’s history and have a background in HIV care. The main concern discussed by all HCPs was around disclosure: ‘confidentiality, especially if the phones are shared’ (James, HCP). Many of their clients were illiterate, so they would not be able to respond to a text, and some could not speak Kiswahili (particularly the elderly). As many of the clinic clients have low incomes, buying food is a priority over their mobile phone: ‘at the end of the day you will need to feed your family. So health care is not a priority, survival is the priority’ (Lisa, HCP). Phones are often stolen or lost, so keeping track of numbers would be difficult.
Discussion
According to the Technology Acceptance Model, perceived ease of use and perceived usefulness of a system are the two predominant indicators of system adoption. The participants in this study were accustomed to using mobile phones. For many of these participants, adopting the WelTel intervention will not require the acquisition of new skills, and for those who do not know how to text, the desire to learn is promising. As the cost of text messaging in Kenya is low and all clients have experience using mobile phones, the integration of the intervention will likely require little effort, although this may be more challenging for those who share a phone, do not have funds for credit or are illiterate. The HCPs expressed few concerns around integrating the intervention into their care, as the initial texts would be sent from an automated platform. They stressed, however, the importance of someone with a background in HIV care responding to the messages received. Most client participants and all HCP participants believed the WelTel intervention has the potential to be useful in increasing communication between the two groups, and listed potential benefits as having access to more timely information and improved communication. A few concerns related to the WelTel intervention were identified by both HCP and client participants, including shared access to phones and the implications for privacy and disclosure, issues also identified elsewhere (Crankshaw et al. 2010). Both HCP and client participant responses suggest that the intervention may be both easy to use and useful to the management of care, indicating that adoption by this group is likely.
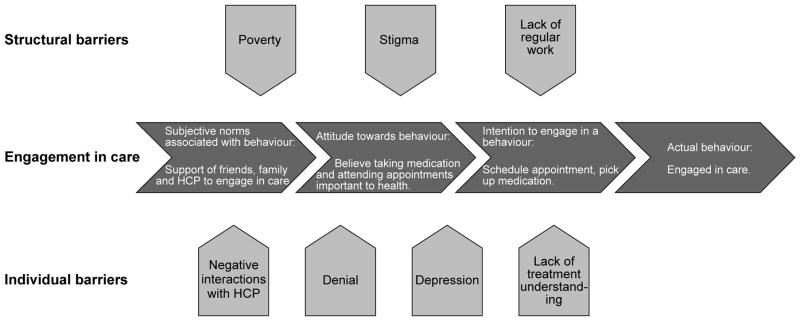
Analysis of responses to questions related to HIV care was guided by the Theory of Reasoned Action. Results indicate that most client participants believed that taking medication and attending appointments was important to their health (attitudes towards behaviour) and that most who had disclosed their status had the support of close family and/or friends to engage in HIV care (subjective norms associated with the behaviour). Participants also intended to engage in care by seeking out and attending a clinic that offered them care in a respectful and timely manner, and described personal motivations for seeking care, including a desire to look after their children, providing for their family and not wanting to die (intention to engage in behaviour). Most of these participants believe that engaging in HIV care is an important behaviour to adopt.
Despite these intentions, participants identified several barriers at both the individual and structural level that may impede their ability to engage in care (Figure 2). Incomplete engagement is not simply the result of an individual decision to neglect care, but a combination of structural factors and individual circumstances that make accessing available care challenging. Both HCP and client participants described individual barriers, including feeling depressed after diagnoses, denial of status, having negative interactions with HCPs, and a lack of understanding of treatment. Similar issues have been reported elsewhere (Bhatia et al. 2011, Konkle-Parker et al. 2011, Nachega et al. 2012, Bogart et al. 2013). Structural barriers to care identified by both groups included lack of regular and local work, poverty and public stigma, an issue heightened by the fact that Kibera is an informal settlement not recognised by the government. Poverty as a reason for non-retention has been reported in South Africa (Maskew et al. 2007) and in Kenya (Ochieng-Ooko et al. 2010). The impact of stigma on retention in care has been reported by HCPs elsewhere (Coetzee et al. 2011, Bogart et al. 2013), and a large qualitative study in Nigeria, Tanzania and Uganda found that patients reported social relationships as central to overcoming barriers to care as a result of social expectations (Ware et al. 2009). Interestingly, transport and distance to the clinic were not listed as barriers to care, an issue that has been reported in other resource-limited settings such as Uganda (Emenyonu et al. 2010), Malawi (Yu et al. 2007) and South Africa (Rabkin et al. 2010).
Figure 2.
Theory of Reasoned Action guided analysis of participants’ responses to questions regarding engagement in HIV care
At the individual client level, the WelTel intervention may provide a useful and accessible link to health services. Improved communication and support may allow some people to better manage their care during the first year after diagnosis, whether their needs are psychosocial (such as the need for counselling to cope with their diagnosis), medical (such as adhering to medications and managing side effects), or informational (such as being informed of the purpose of specific medications and tests). Furthermore, this link may help to foster the development of a trusting relationship between HCPs and clients, a factor highlighted in this study and shown elsewhere to increase long-term engagement (Mallinson et al. 2007). As the provision of HIV care follows the path of other chronic diseases and becomes increasingly decentralised, supporting the development of self-management skills is a key component of this transformation (Swendeman et al. 2009, van Olmen et al. 2012). For many in Kenya, however, access to free treatment, medical care and follow-up care continues to be a challenge. The WelTel intervention has the potential to support clients during the first year after diagnosis by providing a convenient link to HCPs who can assist them in developing these skills.
While the WelTel intervention will not eliminate structural barriers, it may assist with making the delivery of some health services more efficient and convenient. Previous HIV programmes have raised concerns about the extent to which they draw resources away from national health-care systems (El-Sadr and Hoos 2008). A cost-effectiveness component of the WelTel Retain trial will bring about a better understanding of the costs associated with operating WelTel. As with other chronic diseases such as diabetes, hypertension and asthma, the ability of HCPs to detect and manage complications in clients early on is central to effective disease management (van Olmen et al. 2012). For HCPs, more frequent communication may lead to a better understanding of issues their clients are experiencing in a timelier manner, thus allowing for faster follow-up if needed. Facilitating communication via text messaging may also reduce the number of unnecessary appointments, thus eliminating costs and travel time. Finally, if individuals can be contacted via text messaging, HCPs will not have to physically search for them in their communities, an issue that was highlighted as not only time consuming but also as creating anxiety for those clients who feared disclosure.
The enormity of public stigma and blame associated with an HIV diagnosis highlights a major distinction between HIV and other chronic diseases — PLWHA are often regarded as responsible for their status, an issue that sufferers of other chronic diseases may not contend with (van Olmen et al. 2012). As antiretroviral drugs become increasingly available in many sub-Saharan African countries and the number of people who engage in HIV treatment and care increases, public understanding and perception of the disease may also change (Castro and Farmer 2005). Retaining individuals in care is central to this transformation. While the WelTel intervention will not change public attitudes towards PLWHA, it does have the potential to support individuals in their ability to engage in care during the first year after diagnosis and beyond. Individuals who can participate in daily activities at work, school and the home will be the means through which stereotypes and misconceptions are challenged.
Limitations
This small-scale informative study must be considered in the context of its limitations. With only 20 participants, the results are not intended to be generalisable. As client participants were selected through convenience sampling, they do not necessarily offer a range of perspectives and experiences from different groups, but are instead a snapshot of clients attending the KCHC clinic in October 2012. Courtesy bias may also have been a possibility as information was collected from clients in the clinic where they received care; however they were advised during their interview that anything they shared would not be disclosed to clinic staff.
Conclusion
Understanding the facilitators and barriers that individuals experience when attempting to engage in HIV care is central to developing an effective intervention. While the patient participants involved in this study indicate that they believe engaging in care is an important behaviour to adopt, and the study clinic has developed several approaches to assist in retaining individuals in care, missed appointments and loss to follow-up still occur. Lack of retention in care is the result of both individual circumstances, such as depression, lack of understanding of treatment, negative interactions with HCP and denial, and structural barriers, such as poverty, absence of regular work and public stigma. While no intervention can target and overcome all of these barriers, one that assists in improving communication and support may provide patients and HCPs an effective link. As mobile phone use is already well established with both patients and HCPs in this area, the WelTel intervention has the potential to support patients in their efforts to engage in care.
Acknowledgments
We thank the patients and the staff at the African Medical and Research Foundation and the Kibera Community Health Centre, and the Swahili interviewer/translator Elizabeth Mwenda.
This research was supported by the National Institute of Mental Health of the National Institutes of Health under grant number R01MH097558-01. The funding source had no role in the design of the study, its execution, analyses, interpretation of data or decision to submit results. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The authors — Kirsten Smillie, MA, is the mHealth Coordinator at the British Columbia Centre for Disease Control, Vancouver, Canada. Her research interests include mobile health, health services and the interplay of culture and health.
Natasha van Borek, BA, MScPPH, works at McMaster University. Her research interests include HIV prevention, community based research with vulnerable populations and evaluation of population health interventions.
Mia van der Kop, MSc is an epidemiologist at the University of British Columbia in Vancouver and a doctoral student at the Karolinska Institutet, Sweden. Her research interests include global health, mobile health, research methodology and statistics.
Abigael Lukhwaro, MA, is a counsellor working with HIV/AIDS patients to prepare them for treatment initiation and offer health education and support.
Neville Li, MA, worked at the British Columbia Centre for Disease Control (BCCDC) in Vancouver, Canada. His research interests are in health and healthcare policies, ethnicity and health, and qualitative methodologies.
Sarah Karanja, MA, is a Research Officer at AMREF Health Africa.
Anik Patel, BScPharm, MHA, is a PhD candidate at the University of British Columbia. He is a practising pharmacist and his research interests are in the economic and clinical impact of innovative technology in health care.
David I Ojakaa, PhD, is an independent research consultant in Kenya.
Richard T Lester is an infectious diseases physician and Director of the Neglected Global Diseases Initiative at the University of British Columbia and co-founder of the WelTel International mHealth Society. His interests are use of emerging health technologies, clinical medicine, and health system strengthening, particularly in remote and resource limited settings.
References
- Bhatia R, Hartman C, Kallen MA, Graham J, Giordano TP. Persons newly diagnosed with HIV infection are at high risk for depression and poor linkage to care: results from the Steps Study. AIDS Behaviour. 2011;15:1161–1170. doi: 10.1007/s10461-010-9778-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogart LM, Chetty S, Giddy J, Sypek A, Sticklor L, Walensky RP, Losina E, Katz JN, Bassett IV. Barriers to care among people living with HIV in South Africa: contrasts between patient and healthcare provider perspectives. AIDS Care. 2013;25:843–53. doi: 10.1080/09540121.2012.729808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro A, Farmer P. Understanding and addressing AIDS-related stigma: from anthropological theory to clinical practice in Haiti. American Journal of Public Health. 2005;95:53–59. doi: 10.2105/AJPH.2003.028563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coetzee B, Kagee A, Vermeulen N. Structural barriers to adherence to antiretroviral therapy in a resource-constrained setting: the perspectives of health care providers. AIDS Care. 2011;23:146–151. doi: 10.1080/09540121.2010.498874. [DOI] [PubMed] [Google Scholar]
- Crankshaw TCI, Giddy J, Nicholas PK, Eichbaum Q, Butler LM. Exploring the patterns of use and the feasibility of using cellular phones for clinic appointment reminders and adherence messages in an antiretroviral treatment clinic, Durban, South Africa. AIDS Patient Care and STDS. 2010;24:729–734. doi: 10.1089/apc.2010.0146. [DOI] [PubMed] [Google Scholar]
- Dalal W, Feikin DR, Amolloh M, Ransom R, Burke H, Lugalia F, Ouma A, Laserson KF, Mermin J, Breiman RF, Bunnell R. Home-based HIV testing and counseling in rural and urban Kenyan communities. Journal of Acquired Immune Deficiency Syndromes. 2013;62:e47–54. doi: 10.1097/QAI.0b013e318276bea0. [DOI] [PubMed] [Google Scholar]
- Davis FD, BP, Warshaw PR. User acceptance of computer technology: A comparison of two theoretical models. Management Science. 1989;35:892–1003. [Google Scholar]
- El-Sadr WM, Hoos D. The President’s Emergency Plan for AIDS Relief — is the emergency over? New England Journal of Medicine. 2008;359:553–555. doi: 10.1056/NEJMp0803762. [DOI] [PubMed] [Google Scholar]
- Emenyonu N, Muyindike W, Habyarimana J, Pops-Eleches C, Thirumurthy H, Ragland K, Bangsberg DR. Cash transfers to cover clinic transportation costs improve adherence and retention in care in a HIV treatment program in rural Uganda. Proceedings of the 17th Conference on Retroviruses and Opportunistic Infections; 16–19 February 2010; San Francisco, California. 2010. [Google Scholar]
- Fox MP, Rosen S. Patient retention in antiretroviral therapy programs up to three years on treatment in sub-Saharan Africa, 2007–2009: systematic review. Tropical Medicine and International Health. 2010;15(S1):1–15. doi: 10.1111/j.1365-3156.2010.02508.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clinical Infectious Diseases. 2011;52:793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffar S, Amuron B, Foster S, Birungi J, Levin J, Namara G, Nabiryo C, Ndembi N, Kyomuhangi R, Opio A, Bunnell R, Tappero JW, Mermin J, Coutinho A, Grosskurth H. Rates of virological failure in patients treated in a home-based versus a facility-based HIV-care model in Jinja, southeast Uganda: a cluster-randomised equivalence trial. Lancet. 2009;374:2080–2089. doi: 10.1016/S0140-6736(09)61674-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KNBS (Kenya National Bureau of Statistics) Kenya Population and Housing Census 2009. Nairobi: Government Printer; 2010. [Google Scholar]
- Kohler PK, Chung MH, McGrath CJ, Benki-Nugent SF, Thiga JW, John-Stewart GC. Implementation of free cotrimoxazole prophylaxis improves clinic retention among antiretroviral therapy-ineligible clients in Kenya. AIDS. 2011;25:1657–1661. doi: 10.1097/QAD.0b013e32834957fd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konkle-Parker DJ, Amico KR, Henderson HM. Barriers and facilitators to engagement in HIV clinical care in the Deep South: results from semi-structured patient interviews. Journal of the Association of Nurses in AIDS Care. 2011;22:90–99. doi: 10.1016/j.jana.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester RT, Gelmon L, Plummer FA. Cell phones: tightening the communication gap in resource-limited antiretroviral programmes? AIDS. 2006;20:2242–2244. doi: 10.1097/QAD.0b013e3280108508. [DOI] [PubMed] [Google Scholar]
- Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, Jack W, Habyarimana J, Sadatsafavi M, Najafzadeh M, Marra CA, Estambale B, Ngugi E, Ball TB, Thabane L, Gelmon LJ, Kimani J, Ackers M, Plummer FA. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376:1838–1845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- Losina E, Toure H, Uhler LM, Anglaret X, Paltiel AD, Balestre E, Walensky RP, Messou E, Weinstein MC, Dabis F, Freedberg KA. Cost-effectiveness of preventing loss to follow-up in HIV treatment programs: a Côte d’Ivoire appraisal. PLoS Medicine. 2009;6:e1000173. doi: 10.1371/journal.pmed.1000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallinson RK, Rajabiun S, Coleman S. The provider role in client engagement in HIV care. AIDS Patient Care and STDS. 2007;21:S77–84. doi: 10.1089/apc.2007.9984. [DOI] [PubMed] [Google Scholar]
- Maskew M, Macphail P, Menezes C, Rubel D. Lost to follow up: contributing factors and challenges in South African patients on antiretroviral therapy. South African Medical Journal. 2007;97:853–857. [PubMed] [Google Scholar]
- McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. AIDS. 2012;26:1735–1738. doi: 10.1097/QAD.0b013e328355d67b. [DOI] [PubMed] [Google Scholar]
- Nachega JB, Morroni C, Zuniga JM, Schechter M, Rockstroh J, Solomon S, Sherer R. HIV treatment adherence, patient health literacy, and health care provider-patient communication: Results from the 2010 AIDS Treatment for Life International Survey. Journal of the International Association of Physicians in AIDS Care (Chicago) 2012;11:128–133. doi: 10.1177/1545109712437244. [DOI] [PubMed] [Google Scholar]
- Ochieng-Ooko V, Ochieng D, Sidle JE, Holdsworth M, Wools-Kaloustian K, Siika AM, Yiannoutsos CT, Owiti M, Kimaiyo S, Braitstein P. Influence of gender on loss to follow-up in a large HIV treatment programme in western Kenya. Bulletin of the World Health Organization. 2010;88:681–688. doi: 10.2471/BLT.09.064329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabkin M, Austin J, Nash D, et al. High patient retention rates in a multinational HIV/AIDS treatment program: The Columbia University Mother-to-Child-Plus Experience. Proceedings of the 17th Conference on Retroviruses and Opportunistic Infections; 16–19 February 2010; San Francisco, California. 2010. [Google Scholar]
- Sanne I, Orrell C, Fox MP, Conradie F, Ive P, Zeinecker J, Cornell M, Heiberg C, Ingram C, Panchia R, Rassool M, Gonin R, Stevens W, Truter H, Dehlinger M, van der Horst C, Mcintyre J, Wood R. Nurse versus doctor management of HIV-infected patients receiving antiretroviral therapy (CIPRA-SA): a randomised non-inferiority trial. Lancet. 2010;376:33–40. doi: 10.1016/S0140-6736(10)60894-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scanlon ML, Vreeman RC. Current strategies for improving access and adherence to antiretroviral therapies in resource-limited settings. HIV AIDS (Auckland) 2013;5:1–17. doi: 10.2147/HIV.S28912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selke HM, Kimaiyo S, Sidle JE, Vedanthan R, Tierney WM, Shen C, Denski CD, Katschke AR, Wools-Kaloustian K. Task-shifting of antiretroviral delivery from health care workers to persons living with HIV/AIDS: clinical outcomes of a community-based program in Kenya. Journal of Acquired Immune Deficiency Syndromes. 2010;55:483–490. doi: 10.1097/QAI.0b013e3181eb5edb. [DOI] [PubMed] [Google Scholar]
- Smillie K, van Borek N, Abaki J, Pick N, Maan EJ, Friesen K, Graham R, Levine S, van der Kop ML, Lester RT, Murray M. A qualitative study investigating the use of a mobile phone short message service designed to improve HIV adherence and retention in care in Canada (WelTel BC1) Journal of the Association of Nurses in AIDS Care. 2014;25:614–625. doi: 10.1016/j.jana.2014.01.008. [DOI] [PubMed] [Google Scholar]
- Smith LR, Amico KR, Shuper PA, Christie S, Fisher WA, Cornman DH, Doshi M, Macdonald S, Pillay S, Fisher JD For The Sa Options T. Information, motivation, and behavioral skills for early pre-ART engagement in HIV care among patients entering clinical care in KwaZulu-Natal, South Africa. AIDS Care. 2013;25:1685–1690. doi: 10.1080/09540121.2013.775398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendeman D, Ingram BL, Rotheram-Borus MJ. Common elements in self-management of HIV and other chronic illnesses: an integrative framework. AIDS Care. 2009;21:1321–1334. doi: 10.1080/09540120902803158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Kop ML, Ojakaa DI, Patel A, Thabane L, Kinagwi K, Ekstrom AM, Smillie K, Karanja S, Awiti P, Mills E, Marra C, Kyomuhangi LB, Lester RT. The effect of weekly short message service communication on patient retention in care in the first year after HIV diagnosis: study protocol for a randomised controlled trial (WelTel Retain) BMJ Open. 2013:3. doi: 10.1136/bmjopen-2013-003155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Olmen J, Schellevis F, Van Damme W, Kegels G, Rasschaert F. Management of chronic diseases in sub-Saharan Africa: Cross-fertilisation between HIV/AIDS and diabetes care. Journal of Tropical Medicine. 2012:349312. doi: 10.1155/2720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware NC, Idoko J, Kaaya S, Biraro IA, Wyatt MA, Agbaji O, Chalamilla G, Bangsberg DR. Explaining adherence success in sub-Saharan Africa: an ethnographic study. PLoS Medicine. 2009;6:e11. doi: 10.1371/journal.pmed.1000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J, Hollin I, Kachnowski S. A review of the use of mobile phone text messaging in clinical and healthy behaviour interventions. Journal of Telemedicine and Telecare. 2011;17:41–48. doi: 10.1258/jtt.2010.100322. [DOI] [PubMed] [Google Scholar]
- Yu JK, Chen SC, Wang KY, Chang CS, Makombe SD, Schouten EJ, Harries AD. True outcomes for patients on antiretroviral therapy who are “lost to follow-up” in Malawi. Bulletin of the World Health Organization. 2007;85:550–554. doi: 10.2471/BLT.06.037739. [DOI] [PMC free article] [PubMed] [Google Scholar]