Abstract
Background
To be consistent with the United Nations’ sustainable development goals on gender equality, mobile health (mHealth) programmes should aim to use communications technology to promote the empowerment of women. We conducted a pre-trial analysis of data from the WelTel Retain study on retention in HIV care to assess gender-based differences in phone access, phone sharing and concerns about receiving text messages from a healthcare provider.
Methods
Between April 2013–June 2015, HIV-positive adults were screened for trial participation at two clinics in urban slums in Nairobi, Kenya. Proportions of men and women excluded from the trial due to phone-related criteria were compared using a chi-square test. Gender-based differences in phone sharing patterns and concerns among trial participants were similarly compared.
Results
Of 1068 individuals screened, there was no difference in the proportion of men (n = 39/378, 10.3%) and women (n = 71/690, 10.3%) excluded because of phone-related criteria (p-value = 0.989). Among those who shared their phone, women (n = 52/108, 48.1%) were more likely than men (n = 6/60, 10.0%) to share with other non-household and household members (p <0.001). Few participants had concerns about receiving text messages from their healthcare provider; those with concerns were all women (n = 6/700).
Discussion
In this study, men and women were equally able to participate in a trial of an mHealth intervention. Equitable access in these urban slums may indicate the ‘gender digital divide’ is narrowing in some settings; however, gender-specific phone sharing patterns and concerns regarding privacy must be fully considered in the development and scale-up of mHealth programmes.
Keywords: Telehealth, telemedicine, HIV/AIDS, sub-Saharan Africa, gender
Introduction
Background and rationale
Sub-Saharan Africa is the world’s fastest growing mobile phone market, forecasted to grow from 635 million mobile subscriptions at the end of 2014 to 930 million by the end of 2019.1 Access to mobile communications technology has had profound social, political and economic repercussions for hundreds of millions of people in places that previously lacked landline infrastructure. Kenya has been at the forefront of this mobile phone revolution, with one of the highest rates of mobile phone penetration in Africa and a global leadership role in mobile banking. Mobile phones are also transforming health care. Mobile health (mHealth), the delivery of healthcare via mobile communication devices,2 is expected to be one of the largest growth sectors in healthcare over the next six years.3
Most mHealth research and implementation in resource-limited settings has focussed on text-messaging interventions in the context of human immunodeficiency virus (HIV) care.4 In sub-Saharan Africa, HIV disproportionately affects women, whose situation may be compounded by gender-related barriers in access to HIV care, including economic vulnerability and inequality, restricted mobility, child-care responsibilities and fear of violence.5 Women in resource-limited settings also have differential access to technology, known as the ‘gender digital divide’.6 Women in sub-Saharan Africa are 13% less likely to own a mobile phone and have differential patterns of mobile phone use compared to men,7 such as mobile Internet use.8 Despite the explosive growth of mHealth and the well-known ‘gender gap’ in mobile phone ownership and use, few studies have examined gender as it relates to mHealth.9 To be consistent with the United Nations’ new sustainable development goals on gender equality, mHealth programmes should aim to enhance the use of communications technology to promote the empowerment of women.10 Collection of gender-disaggregated data is critical to determine equity in access and barriers to uptake of mHealth interventions and ensure that women are not further marginalised from care. In this study, we examined baseline data from an ongoing trial of a text-messaging intervention to improve retention in early HIV care.11 Our objectives were to determine whether disparities in mobile phone access affected the ability to participate in an mHealth trial, and whether there were gender-based differences in shared phone use and participants’ concerns about text-messaging with their healthcare provider.
Methods
Study design
This cross-sectional study used baseline data collected for a randomised controlled trial evaluating the effectiveness of a text-messaging intervention to improve retention in early HIV care (WelTel Retain).11 Adults testing positive for HIV at two comprehensive care clinics in Nairobi, Kenya were assessed for trial eligibility, including mobile phone access.
Study setting and participants
Between April 2013–June 2015, participants were recruited from the Kibera Community Health Centre (KCHC), an Amref Health Africa clinic located in an informal urban settlement with limited access to services including education, water and sanitation. At this comprehensive care clinic, there are no direct patient costs for HIV/acquired immune deficiency syndrome (AIDS) care and treatment. In March 2014, recruitment began at a second comprehensive care clinic, the Baba Dogo Health Centre, operated by Partners for Health and Development in Africa (University of Manitoba and the University of Nairobi). The Baba Dogo Health Centre is located in an informal settlement in Nairobi’s Eastlands area.
Patients were eligible to participate in the study if they were 18 years old or older, HIV-positive, had access to a mobile phone (including shared access), and could communicate by text-messaging or have somebody text-message on their behalf. Patients previously assessed for antiretroviral (ART) eligibility, with prior ART exposure or on ART were excluded. Women known to be pregnant at the time of enrolment were also excluded because of their differing incentive to remain in contact with the clinic, compared with a non-pregnant population. Full details of the WelTel Retain study protocol have been published previously.11
The WelTel intervention
The WelTel intervention is based on a model of patient-healthcare provider mobile phone communication used in the original WelTel Kenya1 trial.12,13 Participants randomised to the intervention arm are registered to receive the WelTel mHealth intervention for 12 months, where every Monday morning, customised computer software sends the text message ‘Mambo?’ (KiSwahili for ‘How are you?’) to patients to inquire about their status. Patients are instructed to respond within 48 h either that they were doing well (‘Sawa’) or had a problem (‘Shida’). The clinician then calls participants to provide assistance to those who indicate a problem or fail to respond.
Outcomes
Exclusions based on phone-related criteria
Screened participants were considered excluded from participating in the trial because of criteria relating to phone use and access if they: (a) did not own or have regular access to a cell phone; or (b) could not operate a phone using simple text messaging or have someone who could text message on their behalf.
Shared phone use
If participants owned a cell phone, they were asked who, if anyone, shared access to their phone. If participants did not own a phone, but had regular access to a phone, they were asked whose phone they had regular access to, and whether that individual knew their HIV status.
Concerns about receiving text messages from a healthcare provider
Participants were asked whether they would have any concerns about receiving text messages from a healthcare provider, and if so, to specify their concerns.
Data sources and measurement
At the time of study enrolment, research nurses collected data on participants’ gender. Gender was defined as ‘female’ or ‘male’ and based on self-report. Data on how many patients were excluded from participating in the trial because of mobile phone-related criteria were collected using a screening tool. Additional study data were collected using an interviewer-administered questionnaire.
Sample size
A total of 1068 patients were screened for participation in the WelTel Retain trial and contributed to this analysis. The 700 participants eligible for the trial contributed additional data on phone sharing and concerns regarding receiving text messages from a healthcare provider.
Ethics
The original study protocol was approved by the University of British Columbia Clinical Ethics Review Board and Amref Health Africa’s Ethics and Scientific Review Committee.
Statistical analyses
We conducted descriptive analyses of the study population, including reasons for trial exclusion, phone ownership and access, and participants’ concerns. A chi-squared test was used to determine whether the proportion of males and females excluded from trial on the basis of phone-related criteria differed, and to examine gender-based differences in the additional outcomes. In cases where the total value of the table was less than 40 and an expected value was less than five, a Fisher’s exact test was used. All p-values are two-sided. Analyses were performed using Stata version 12 (Statacorp, College Station, Texas, USA).
Results
Study population
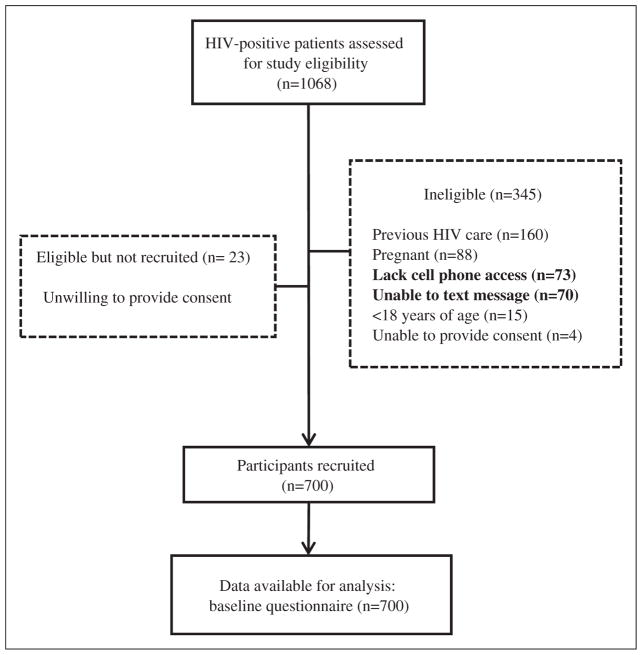
Between April 2013–June 2015, 1068 individuals were screened for trial participation (Figure 1); 690 (64.6%) of whom were female. The median age of those screened was 31 years (interquartile range 26–39 years). Less than 3% of those screened who were eligible for the trial declined participating, and there was no statistically significant difference in the proportions of men (n = 10/378; 2.6%) and women (n = 13/690; 1.9%) who declined participation (p = 0.412). Of the 700 participants who enrolled in the trial, 59.9% (419/700) were female. Table 1 provides baseline demographic and clinical information disaggregated by gender for the trial participants.
Figure 1.
Flow of participants. HIV: human immunodeficiency virus.
Table 1.
Demographic and clinical characteristics of participants enrolled in the WelTel Retain trial, by gender. Values are numbers (%).
| Variable | Female (n = 419) | Male (n = 281) |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 31.23 (8.97) | 37.44 (9.71) |
| <30 | 207 (49.4) | 64 (22.8) |
| 30–39 | 146 (34.8) | 118 (42.0) |
| 40–49 | 49 (11.7) | 60 (21.4) |
| ≥50 | 17 (4.1) | 39 (13.9) |
| Marital status | ||
| Single | 88 (21.0) | 22 (7.8) |
| Married | 174 (41.5) | 225 (80.1) |
| Divorced/separated/widowed | 157 (37.5) | 34 (12.1) |
| Average monthly household income (US$) | ||
| <100 | 76 (18.1) | 46 (16.4) |
| 100–200 | 22 (5.3) | 63 (22.4) |
| >200 | 8 (1.9) | 41 (14.6) |
| Unwilling to disclose | 13 (3.1) | 12 (4.3) |
| Uncertain | 129 (30.8) | 88 (31.3) |
| Missing | 171 (40.8) | 31 (11.0) |
| Educational level | ||
| No formal education | 18 (4.3) | 3 (1.1) |
| Primary school | 275 (65.6) | 158 (56.2) |
| Secondary school | 110 (26.3) | 99 (35.2) |
| Tertiary school | 16 (3.8) | 21 (7.5) |
| Clinic | ||
| Kibera | 304 (72.6) | 197 (70.1) |
| Baba Dogo | 115 (27.4) | 84 (29.9) |
| CD4 | ||
| Median (IQR) (cells/μl) | 322 (159–488) | 267 (139–445) |
IQR: interquartile range; SD: standard deviation.
Gender and mobile phone-based inclusion criteria
Overall, 90% (n = 958/1068) of potential participants screened had access to a mobile phone and text-messaging capability. The proportions of potential participants who did not fulfil mobile phone-related eligibility criteria are shown in Table 2. Men and women were equally likely to be excluded from participating in the trial because they did not meet the study’s phone-related criteria (39/378 (10.3%) of men and 71/690 (10.3%) of women; p-value = 0.989).
Table 2.
Exclusions from the trial according to phone-related criteria, by gender. Values are numbers (%).
| Female (n = 690) | Male (n = 378) | p-Value | |
|---|---|---|---|
| Phone access | 645 (93.5) | 350 (92.6) | 0.583 |
| No phone access | 45 (6.5) | 28 (7.4) | |
| Text-message capability | 644 (93.3) | 354 (93.7) | 0.841 |
| No text-message capability | 46 (6.7) | 24 (6.3) | |
| Overall | |||
| Met phone-related criteria | 619 (89.7) | 339 (89.7) | 0.989 |
| Did not meet phone-related criteria | 71 (10.3) | 39 (10.3) | |
Gender-based comparison of phone sharing
Of participants enrolled in the trial, 94.7% (n = 663/700) owned a mobile phone. Mobile phone ownership was not markedly different between men and women: 94.0% (n = 394/419) of women owned a mobile phone compared to 95.7% (269/281) of men (p-value = 0.326). Among those who owned a phone, men and women were similarly likely to share access to their phone with someone else (Table 3); however, the people with whom they shared access to their phone varied. Men most frequently shared access to their phone with their partner (56/60; 93.3%), but few shared their phone with other household or non-household members. Women also frequently shared their phone with their partner (65/108; 60.2%); however, a greater proportion of women versus men shared their phone with other household and non-household members.
Table 3.
Gender differences in phone ownership, phone sharing and additional phone-related outcomes.
| Female (n = 419) | Male (n = 281) | p-Value | |
|---|---|---|---|
| Land line ownership | 4 (1.0) | 4 (1.4) | 0.567 |
| Mobile phone ownership | 394 (94.0) | 269 (95.7) | 0.326 |
| Communicated with a HCP in the pasta | 23 (5.5) | 15 (5.3) | 0.957 |
| Prefer to communicate with HCP via | |||
| Text-message | 64 (15.3) | 43 (15.3) | 0.209 |
| Voice call | 116 (27.8) | 62 (22.1) | |
| Either text message or voice call | 237 (56.8) | 176 (62.6) | |
| Share one’s phone with others | 108 (27.4) | 60 (22.3) | 0.138 |
| Partner | 65 (60.2) | 56 (93.3) | <0.001 |
| Another household member | 40 (37.0) | 6 (10.0) | <0.001 |
| Non-household member | 12 (11.1) | 0 (0.0) | 0.007 |
| Do not own – have regular access | 25 (6.0) | 12 (4.3) | 0.326 |
| Partnera | 12 (48.0) | 6 (50.0) | 0.477 |
| Another household member | 8 (32.0) | 2 (16.7) | |
| Non-household member | 4 (16.0) | 4 (33.3) | |
| Missing | 1 (4.0) | 0 (0.0) | |
| Phone owner knows participant’s statusa | 19 (72.0) | 9 (75.0) | 1.000 |
| Concerned about receiving text messages from their HCP | 6 (1.4%) | 0 (0.0%) | 0.044 |
HCP: healthcare provider.
Missing data: 1 male and 1 female.
Of the small proportion of men and women who did not own a cell phone, but had regular access to a cell phone, men and women most frequently reported regular access to their partner’s phone (n = 12/25 women and n = 6/12 men regularly accessed their partner’s phone; Table 3). There were no significant differences between men and women as to whose phone they regularly had access to, and whether they had disclosed their HIV status to that person.
Communication via mobile phone with a healthcare provider
Of the participants enrolled in the trial, few had previously communicated with their healthcare provider by cell phone (n = 38/700; 5.4%), and most did not express a preference between receiving voice calls or text messages. There were no gender differences in either of these outcomes. Most participants did not have any concerns about receiving text messages from their healthcare provider. Only six participants (6/700; 0.9%), all women, responded that they had concerns (Table 3). Half of these concerns related to fear of HIV status disclosure (n = 3); one stated a preference for voice calls over text-messaging; one was concerned she would not know which healthcare provider had sent the message; and the other was concerned about receiving ‘bad news’ via text message.
Discussion
Key results
The gender gap in mobile phone ownership is narrowing in Kenya (7%); however, it has been found to be much higher among poorer households (16%).7 Therefore, we had expected that the ‘gender digital divide’ would translate into gender differences in the ability to enrol in a trial of a mobile health intervention that required phone ownership or access. Instead, we found that 90% of those screened met phone-related inclusion criteria, and there was no difference in the proportion of men and women excluded based on these criteria. Our results are especially surprising given the urban slum setting, in which greater economic and educational gender disparities persist.14 Even in the informal economy prevalent in slum settings, women are disproportionately concentrated in lower income segments, creating a gender gap in income and other work-related benefits.15 Equally high levels of phone access and the ability to text-message among both genders is promising for mHealth programmes in the scale-up phase, and others who seek to improve the delivery of HIV healthcare services through mobile communication. Increasing urbanisation, with the slum growth rate exceeding the overall urban rate,16 together with the greater health challenges faced by slum residents, makes finding additional opportunities to enhance health care in these settings of particular importance.
Less than 3% of those who were eligible to participate in the trial declined to give consent, and there was no difference in the proportions of male and female enrolment, indicating that, overall, people had few concerns regarding participating in an mHealth trial. While few of those enrolled in the trial had concerns regarding receiving text messages from their healthcare provider, those with concerns were all women. The WelTel mHealth intervention the participants were to receive did not contain language relating to HIV; however, concerns over the fear of HIV status disclosure must be seriously considered, and strategies to protect participant confidentiality are of paramount importance. This is especially pertinent given that the quarter of participants who were using someone else’s phone to potentially receive the service had not yet disclosed their HIV status to that person. With proper consideration, allowing those to participate who do not own a phone, but have shared phone access, can effectively increase the reach of mHealth interventions. Mitigating gender-specific concerns should be considered in light of differing phone sharing patterns between men and women. While men and women were equally likely to share access to their phone with another person, women were more likely to share their phone with other household and non-household members than were men, potentially leading to a differential risk of privacy breach. Implementers involved in the scale-up of evidence-based mHealth interventions should consider the implications of gender-specific phone-sharing behaviour when rolling out their programme.
Limitations of the study
While the results of our study indicate that the ‘gender digital divide’ might be closing, at least at the two clinics involved in this study, our results might not be generalisable to other settings. The barriers to health services access and phone access may be similar, and women attending the clinics may differ from women who were not able to reach the clinic. Furthermore, Kenya is one of the sub-Saharan countries with the highest mobile penetration rate: the gender digital divide may be more pronounced in other sub-Saharan African countries with lower mobile phone ownership, or in rural settings. Nevertheless, there are limited gender-disaggregated data from the region, most of which indicate gender disparities in access and use. Therefore, our results provide an important indication that things may be changing, particularly given that they arose from a very low-income context. A second limitation is the descriptive nature of the study. To delve deeper into gender-specific phone-sharing behaviour and concerns about receiving text messages as part of HIV care, a qualitative investigation is required. A greater understanding of these issues may allow implementers the opportunity to address the ‘gender gap’ more thoroughly when planning mHealth programmes for HIV care.
Comparison with other studies
Gender-disaggregated data on phone ownership and use from resource-limited settings is scarce. Of the policy papers17,18 and research studies published,19 males were more likely to own a mobile phone than females. The Wesolowski et al. study in Kenya indicated that women were also more likely to share somebody else’s phone, which is consistent with the decreased need for phone sharing as ownership increases.20 Programme implementers ought to bear in mind the risk that mHealth may exacerbate gender inequalities, as was the case in a pilot study aimed to increase HIV knowledge in Uganda,21 in which men were twice as likely to respond as women, or in the Congo, where the target population of a family planning service was women, yet over 80% of callers were men.22 Although the authors of the Congolese study were unsure as to why men were the primary users of the service, they believed it was because men were more likely to own a cell phone and have greater exposure to mass media.22 Although we do not yet have gender-specific data on the use of the intervention in this specific trial, it is promising that in this very low-income environment, men and women were equally able to meet the phone-related criteria to enable them to participate. Previous studies of the WelTel intervention in a population of HIV-positive individuals initiating ART showed that women were as likely to engage in the intervention as men, with similar response rates to the messages and requests for additional clinician contact.23
Conclusions
At two clinics in low-income informal settlements in Nairobi, Kenya, men and women were equally able to participate in a trial of an mHealth intervention that required phone access. Equitable access in these slum settings is promising in light of the United Nations’ new sustainable development goals on gender equality that stipulate that mHealth programmes should aim to enhance the use of communications technology to promote the empowerment of women. While opportunities to improve health care delivery through the use of mobile phones may be expanding, gender-specific phone sharing patterns and concerns regarding privacy must be fully considered in the development and scale-up of mHealth interventions.
Acknowledgments
The authors would like to thank Patrick Nagide, Richard Gichuki and Sarah Karanja for their dedicated work on the study; and all of the clinical staff, research team members, and patients who participated in the study. They are grateful to Joshua Kimani and Partners for Health and Development in Africa for supporting the study at the Baba Dogo Clinic. They also thank Shaina Pennington for her careful editing of the manuscript and Jamie Fujioka for her assistance with background research and manuscript preparation.
Funding
The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: research reported in this publication was supported by the National Institute of Mental Health of the National Institutes of Health under grant number R01MH097558. The funding source had no role in the design of the study and did not have any role during its execution, analyses, interpretation of data, or decision to submit results. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported by the CIHR Canadian HIV Trials Network (grant number CTN 284). MVDK is supported by a Canadian Institutes of Health Research Doctoral Foreign Study Award (grant number 290960).
Footnotes
Declaration of conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: This study uses a technology platform (WelTel) that has been developed by a non-profit organization and a private company. The primary investigator of this study, RTL, has financial as well as professional interests in both organizations. The other authors declare that there is no conflict of interest.
References
- 1.Ericsson. [accessed 7 March 2016];Sub-Saharan Africa: Ericsson mobility report appendix. 2014 http://www.ericsson.com/res/docs/2014/emr-june2014-regional-appendices-ssa.pdf.
- 2.Torgan C. [accessed 7 March 2016];The mHealth Summit: Local & global converge. 2009 http://www.caroltorgan.com/mhealth-summit/
- 3.Grand View Research. [accessed 7 March 2016];mHealth Market Analysis and Segment Forecasts to 2020. 2014 http://www.grandviewresearch.com/industry-analysis/mhealth-market/segmentation.
- 4.Déglise C, Suggs LS, Odermatt P. SMS for disease control in developing countries: a systematic review of mobile health applications. J Telemed Telecare. 2012;18:273–281. doi: 10.1258/jtt.2012.110810. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. [accessed 29 March 2016];Gender inequalities and HIV. 2016 http://apps.who.int/gender/hiv_aids/en/
- 6.Kularski C, Moller S. The digital divide as a continuation of traditional systems of inequality. Sociology. 2012;5151:1–23. [Google Scholar]
- 7.GSMA Development Fund. [accessed 8 March 2016];Bridging the gender gap: Mobile access and usage in low- and middle-income countries. 2015 http://www.gsma.com/connectedwomen/wp-content/uploads/2015/02/GSM0001_02252015_GSMAReport_FINAL-WEB-spreads.pdf.
- 8.iHub Research & Research Solutions Africa. [accessed 7 March 2016];Mobile phone usage at the Kenyan base of the pyramid. 2012 https://blogs.worldbank.org/ic4d/files/ic4d/mobile_phone_usage_kenyan_base_pyramid.pdf.
- 9.Kanter R, Ramirez-Zea M, Martinez H. Gender differences in participation in a mHealth intervention to promote lifestyle changes in Latin America (380.8) FASEB J. 2014;28:380.8. [Google Scholar]
- 10.United Nations. [accessed 7 March 2016];Sustainable development goals. 2016 http://www.un.org/sustainabledevelopment/gender-equality/
- 11.van der Kop ML, Ojakaa DI, Patel A, et al. The effect of weekly short message service communication on patient retention in care in the first year after HIV diagnosis: Study protocol for a randomised controlled trial (WelTel Retain) BMJ Open. 2013;3:e003155. doi: 10.1136/bmjopen-2013-003155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lester RT, Ritvo P, Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. Lancet. 2010;376:1838–1845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 13.Lester RT, Mills EJ, Kariri A, et al. The HAART cell phone adherence trial (WelTel Kenya1): A randomized controlled trial protocol. Trials. 2009;10:87. doi: 10.1186/1745-6215-10-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chant S. Cities through a ‘gender lens’: A golden ‘urban age’ for women in the global South. Environ Urban. 2013;25:9–29. [Google Scholar]
- 15.Chant S, Datu K. Women in cities: Prosperity or poverty? A need for multi-dimensional and multi-spatial analysis. In: Coles A, Gray L, Momsen J, editors. The city in urban poverty. London: Palgrave Macmillan UK; 2015. pp. 39–63. [Google Scholar]
- 16.UN Human Settlements Programme. The state of African cities 2010: Governance, inequalities and urban land markets. Nairobi: UN-HABITAT; 2010. [Google Scholar]
- 17.Milek Gillwald A, Stork C. [accessed 7 March 2016];Gender assessment of ICT access and usage in Africa. Volume One 2010 Policy Paper 5. 2010 http://idl-bnc.idrc.ca/dspace/bitstream/10625/44152/1/130564.pdf.
- 18.Cherie Blair Foundation for Women. [accessed 7 March 2016];Women and mobile: A global opportunity. www.cherieblairfoundation.org/women-and-mobile-a-global-opportunity/
- 19.Zurovac D, Otieno G, Kigen S, et al. Ownership and use of mobile phones among health workers, caregivers of sick children and adult patients in Kenya: Cross-sectional national survey. Glob Health. 2013;9:20. doi: 10.1186/1744-8603-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wesolowski A, Eagle N, Noor AM, et al. Heterogeneous mobile phone ownership and usage patterns in Kenya. PLoS One. 2012;7:e35319. doi: 10.1371/journal.pone.0035319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chib A, Wilkin H, Ling LX, et al. You have an important message! Evaluating the effectiveness of a text message HIV/AIDS campaign in Northwest Uganda. J Health Commun. 2012;17:146–157. doi: 10.1080/10810730.2011.649104. [DOI] [PubMed] [Google Scholar]
- 22.Corker J. ‘Ligne Verte’ toll-free hotline: Using cell phones to increase access to family planning information in the Democratic Republic of Congo. Cases Public Health Commun Mark. 2010;4:23–37. [Google Scholar]
- 23.Van der Kop ML, Karanja S, Thabane L, et al. In-depth analysis of patient-clinician cell phone communication during the WelTel Kenya1 antiretroviral adherence trial. PLoS One. 2012;7:e46033. doi: 10.1371/journal.pone.0046033. [DOI] [PMC free article] [PubMed] [Google Scholar]