Abstract
Cigarette smoking increases the risk of developing several systemic conditions including cancer, cardiovascular and pulmonary diseases. Cigarette smoking is also detrimental to oral health as it increases the incidence and severity of oral cancer, periodontal diseases, and periimplantitis, as well as impacting negatively dental patients’ response to therapy. Therefore, consideration of smoking behavior and recommendation of smoking cessation are important parts of dental treatment planning. However, cigarettes are no longer the most popular form of tobacco use among adolescents in the United States and globally. In recent years, tobacco smoking using a waterpipe (“hookah”, “shisha”) and use of electronic cigarettes (ECIGs) has increased significantly. Thus, dental clinicians likely will treat more patients who are waterpipe and/or ECIG users. Yet, the literature on the health effects of waterpipe and ECIGs use is sparse. Both waterpipe and ECIGs deliver the dependence-producing drug nicotine. Waterpipe tobacco smoking has been associated with periodontitis, dry socket, premalignant lesions and oral and esophageal cancer. The health effects of long-term ECIG use are unknown. The purpose of this review is to inform healthcare professionals about waterpipe and ECIGs, highlight emerging evidence on the biological effects of these increasingly popular tobacco products, and introduce perspectives for dental patient management and future research.
Keywords: Electronic Cigarettes, Waterpipe, periodontal disease, oral cancer, smoking
1. Introduction
Tobacco cigarette smoking causes a variety of adverse health effects including cancer and cardiovascular and pulmonary disease (1). Cigarette, bidi, pipe, and cigar smoking, as well as smokeless tobacco use is associated with increased risk for malignant and premalignant lesions of the oral cavity, periodontal diseases, tooth loss and dental implant failures (2, 3).
Periodontal diseases have been the most widely studied oral condition in relation to cigarette smoking. Detrimental effects of smoking on periodontal tissues, clinical consequences, and possible biological mechanisms that render smokers more susceptible to periodontitis have been reviewed (4). Cross-sectional and longitudinal studies show that smokers exhibit a higher prevalence, greater severity, and faster progression of periodontal disease than never or former smokers. Cigarette smoking also has a negative influence on non-surgical and surgical periodontal therapy including regenerative and plastic surgeries (4, 5). While heavy cigarette smokers exhibit more severe forms of the disease and unfavorable treatment outcomes, quitting cigarette smoking decreases the progression of periodontal destruction and leads to better clinical results (6). Cigarette smoking has also been associated with peri-implantitis, peri-implant bone loss and implant failure (7). Hence, cigarette smoking clearly creates a major risk for periodontal and likely for peri-implant diseases and cigarette smoking behavior and implementation of smoking cessation programs constitute an important part of treatment planning to prevent and manage these diseases.
The adverse health effects of smoking likely are due to the toxicant content of tobacco cigarette smoke. In addition to the dependence-producing, stimulant drug nicotine, cigarette smoke contains hundreds of other toxicants many of which are carcinogenic (8). There is a wide array of combustible tobacco products on the world market and extensive literature investigating the deleterious health effects of tobacco cigarette smoking and smokeless tobacco (1). Less well-known are the health effects of two other tobacco products that are beginning to rival or even eclipse the popularity of cigarette smoking nationally and globally, particularly among youth: waterpipe (hookah, narghile, shisha) and electronic cigarettes (“vape pens”, “personal vaporizers”). Current evidence suggests that waterpipe tobacco smoke contains many toxicants and is associated with adverse health effects (9). Health effects of electronic cigarettes (ECIGS) are less well known, and many factors influence ECIG emissions, such as the electrical power of the device, the constituents of the liquid that the device aerosolizes, and the experience of the user. Further, because these devices are unregulated in many countries, the device characteristics and liquid constituents can change frequently.
While the clinical and laboratory data are too limited to assess comprehensively the effect of waterpipe or ECIG use on oral and systemic health, their use may increase susceptibility for tobacco product-related disorders in the oral cavity. Based on current trends, dental care providers likely will treat more patients who are exposed to these products. The purpose of this review is to inform dental healthcare professionals about waterpipe and ECIGs, highlight emerging evidence on the biological effects of these increasingly popular tobacco products, and introduce perspectives for dental patient management and future research.
2a. Waterpipe Definition and Global Prevalence Rates
A waterpipe consists of a head, body, water bowl, and a hose with mouthpiece (Figure 1). Flavored tobacco (strawberry, watermelon/melon, apple/double apple, mint) was introduced to the market in the 1990s and proved to be very appealing with over 90% of users reporting a flavor preference (10). The combination of the water-cooled and flavored smoke with the incorrect perception of decreased toxicant content relative to cigarette smoke has contributed to a dramatic increase in prevalence of waterpipe tobacco smoking (WTS) (10, 11).
Figure 1. Waterpipe photograph and scheme.
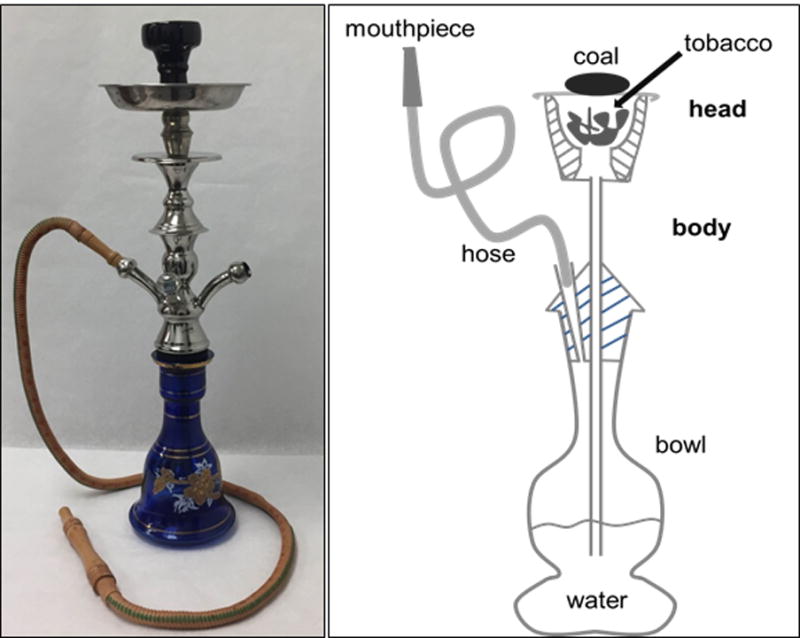
Generally, the waterpipe head is fired-clay, the body is metal, the bowl is glass or plexiglass, and the hose is plastic or leather. The user inhales from the mouthpiece, causing a pressure drop in the bowl. As a result, air is drawn over the charcoal and through the head, heating the tobacco and producing a charcoal and tobacco smoke mixture that is drawn through the body, into the bowl and through the water, into the hose and is subsequently inhaled by the user.
WTS prevalence is increasing within the U.S. and globally, particularly among adolescents, young adults and women (12–16). For example, national data from the U.S. indicate that WTS among 12th graders rose from 17% in 2010 to 19.8% in 2015 (15). WTS prevalence also is on the rise around the world. In the eastern Mediterranean region WTS has long surpassed cigarette use among adolescents (11, 17). The prevalence of at least weekly waterpipe use in the U.K. among high school students was 7.6%, double that of the prevalence of cigarette use (18). One of the highest prevalence rates was observed in Lebanon where nearly 38% of boys aged 13–15 reported WTS in the past 30 days (19). Many factors likely are leading to these increases in WTS among youth, including an incorrect belief of decreased harm of WTS and possibly unregulated sales to minors (20).
Even with healthcare provider and patient awareness, reducing WTS prevalence may prove difficult because this form of tobacco use supports dependence. As with tobacco cigarettes, this dependence is likely due to the self-administration of nicotine (21, 22). Nicotine delivery of WTS and tobacco cigarette use involve similar peak plasma nicotine concentrations but, due to the longer use episode associated with WTS, participants received 1.7 times the nicotine from a single waterpipe use episode as compared to a single cigarette (23), though use over longer periods may lead to less nicotine delivery via waterpipe as compared to cigarette (24). Waterpipe users exhibit typical signs of dependence: difficulty quitting, abstinence symptoms, and, the more often they use a waterpipe, the more ‘hooked’ they report feeling (25). A waterpipe dependence measure has been validated (26) and higher scores are associated with adverse health outcomes (27). WTS-induced dependence constitutes a threat to individual and public health.
2b. WTS Toxicant Emissions and User Toxicant Exposure
The aerosol that emerges from the waterpipe mouthpiece which is inhaled by the user is a combination of charcoal smoke and tobacco smoke exposing users to many of the same disease-causing toxicants and carcinogens as the smoke generated by tobacco cigarettes such as nicotine, carbon monoxide (CO), polyaromatic hydrocarbons, volatile aldehydes, and tobacco-specific nitrosamines (24, 28, 29, 30). During a single 30–60 minute WTS episode, waterpipe tobacco smokers can inhale over 40 liters of smoke as compared to 1 liter or less for a single cigarette (22, 23, 31). Therefore, the amount of toxicants generated during a single waterpipe smoking session is much more than those in the smoke generated from a single cigarette (31, 32). For example, during a waterpipe session 242–2350 mg of tar and 5.7–367 mg of CO is produced compared to 1–27 mg of tar and 14–23 mg of CO from a single cigarette (33). During a waterpipe smoking session, the CO exposure can be so great that some users experience acute CO intoxication that requires medical attention (33–39). In fact, higher CO levels in cafes serving waterpipe also raise the concern for second hand exposure (40).
Together, the evidence suggests that WTS exposes users and possibly non-users who are in the same environment to numerous toxicants and likely causes a threat for adverse health problems.
2c. Effect of WTS on Oral and Systemic Health: clinical studies
WTS is associated with many of the similar systemic conditions as cigarette smoking including cancer, respiratory and cardiovascular problems, and adverse pregnancy outcomes (Table 1) (41–52).
Table 1.
Clinical Studies on the effects of waterpipe smoking
| Health Outcomes of WP | Publication | Sample Size (n) |
|---|---|---|
| Lung Cancer (correlational studies) | Aoun et al 201341 | 50 |
| Gupta et al 200142 | 265 | |
| Respiratory tract disorders due to passive exposure | Tamim et al 200343 | 625 |
| Vascular Changes | Alomari et al 201445 | 53 |
| Layoun et al 201446 | 132 | |
| Alomari et al 201550 | 53 | |
| Pulmonary Abnormalities | Strulovici-Barel Y et al 201651 | 40 |
| Malignant and premalignant lesions in the oral cavity | Al-Amad et al 201461 | 102 |
| Dangi et al 201262 | 761 | |
| Low birth-weight infants | Mirahmadizadeh et al 200847 | 2,808 |
| Nuwayhid, et al 199848 | 913 | |
| Tamim et al 200849 | 8,593 | |
| Periodontal disease | Javed et al 201656 | 200 |
| Bibars et al 201553 | 190 | |
| Natto et al 200457 | 244 | |
| Natto et al 200558 | 262 | |
| Natto et al 200559 | 262 | |
| Baljoon et al 200560 | 355 | |
| Khemiss et al 201663 | 120 | |
| Dry Socket | Al-Belasy et al 200452 | 300 |
| CO intoxication/Poisoning | Ashurst et al 201237 | 1 (case report) |
| Lim et al 200938 | 1 (case report | |
| Ozkan et al 201339 | 1 (case report | |
| La Fauci et al 201236 | 1 (case report) | |
| von Rappard et al 201435 | 4 (case report) | |
| Increased inflammation and candida | Seifi et al 201468 | 120 |
| El-Setouhy et al 200870 | 206 | |
| Genotoxic effects | Al-Amrah et al 201473 | 20 |
| Alsatari et al 201271 | 68 | |
| Khabour et al 201172 | 68 |
Oral cavity is one of the first sites exposed to the constituents of waterpipe smoke. Similar to the negative biological effects of conventional cigarettes on the oral mucosa, WTS is also associated with several conditions within the oral cavity including impaired inflammatory responses, susceptibility to candida infections, periodontal diseases, dry socket, premalignant lesions, and oral cavity cancer (Table 1) (4, 53–62). Although the number of studies is still limited, WTS has been consistently associated with increased prevalence of periodontal disease as measured by increased periodontal pocket depth, loss of clinical attachment, and vertical bone defects compared to non-smokers (57–63). While periodontal disease severity tends to increase in waterpipe smokers, similar to cigarette smoking, WTS also results in decreased gingival bleeding (57). This finding implies that impaired immune and inflammatory responses which have been associated with the disease pathology in cigarette smokers likely play a role in WTS associated adverse effects on the periodontium as well. In two studies waterpipe smokers exhibited higher dental plaque scores compared to nonsmokers (57, 63). One study found no difference in toothbrush between cigarettes smokers and waterpipe smokers (63) while another reported less frequent dental visits reported by waterpipe smokers (57). One of the limitation of the studies was that the specific microbial composition between groups (waterpipe smokers versus nonsmokers) was not determined. Therefore, future studies are warranted to assess how WTS affects immune and inflammatory parameters and oral microbiome to elucidate fully its biological effects within the oral cavity.
2d. Effect of WTS on cellular/biological pathways: in vivo and in vitro studies
The cellular and molecular mechanism by which WTS causes deleterious effects has not been elucidated. To date, the studies demonstrated that exposure to waterpipe smoke produces negative cognitive effects, inflammation, cytotoxicity, and genotoxicity (Table 2) (64–75).
Table 2.
Preclinical Studies on the effects of waterpipe smoking
| Health Outcomes of WP | Publication | Study Type | Species |
|---|---|---|---|
| Pregnancy complications (low birth-weight and neonatal death) | Khabour et al 201675 | In vivo | Rats |
| Cardiovascular disease | Rammah et al 201367 | In vitro | Human aortic endothelial cells |
| Adverse/impaired memory effects | Alzoubi et al 201564 | In vivo | Rats |
| Reduced cell proliferation | Shihadeh et al 201469 | In vitro | Human alveolar cells |
| Inflammation in lung | Khabour et al 2015 b65 | In vivo | Mice |
| Khabour et al 201266 | In vivo | Mice |
In vivo, following 4 weeks (1hr/day; 5days/week) of waterpipe smoke exposure, rats demonstrated short and long term memory impairment which correlated with changes in oxidative stress biomarkers in the hippocampal tissues (64). In another study, waterpipe smoke exposure increased inflammatory markers in rodent lung tissue including matrix metalloproteinases (MMP-1, -9, and -12) and pro-inflammatory cytokines, TNF and IL-6, as well as total white blood cell count, neutrophil, macrophage, and lymphocyte numbers (65, 66). In vitro studies demonstrated that waterpipe smoke exposure causes genotoxic effects (DNA damage) in lymphocytes (71, 72), buccal cells (70, 73), and leukocytes (73). For example, genotoxicity in lymphocytes was compared in 18 human non-smokers, 18 cigarette smokers (>30 cigarettes/day), and 50 waterpipe smokers using the sister chromatic exchange (SCEs) assay. Lymphocytes from both the cigarette and waterpipe smokers demonstrated significantly higher increases in the frequencies of SCEs as compared to healthy participants (72). Further, the frequency of SCEs were significantly higher in waterpipe smokers compared to those smoking cigarettes implying that WTS might be more genotoxic than cigarette smoking.
Considering the known toxicants in waterpipe smoke and the reported biological consequences thus far, WTS likely has similar effects on human health as tobacco smoking. While exact molecular mechanisms by which waterpipe causes adverse health problems in oral tissues and systemically have yet to be identified, health care providers need to be aware of possible risks.
3a. ECIG Definition and Global Prevalence Rates
ECIGs are an evolving class of products that use an electrical heating element that aerosolizes a liquid that usually contains a mixture of propylene glycol (PG) and/or vegetable glycerin (VG), flavorants, and, oftentimes, nicotine (74). The aerosol constituents that reach the user largely are determined by device type, power (voltage and resistance), and liquid contents (76). The first ECIGs introduced into the U.S. market were disposable, constrained to one electrical power level, and used a cartridge that had been pre-filled with the liquid to be aerosolized; the cartridges usually could not be refilled and the batteries could not be recharged. Sometimes these products are referred to as “cigalikes” because they are the size and shape of a tobacco cigarette. While these “cigalike” products remain on the market, ECIGs have evolved to include products with adjustable voltage settings, refillable cartridges or “tanks”, and no longer resemble combustible cigarettes (Figure 2). These latter products can be refilled with liquid in over 7000 flavors (77) with variable ingredients, including nicotine concentrations ranging from 0 to at least 36 mg/ml (78). Because the nicotine present in many ECIG liquids is derived from the tobacco plant, the U.S. Food and Drug Administration (FDA) regulates them under the Family Smoking Prevention and Tobacco Control Act (79). Around the world, different countries have adopted various policy options that include prohibiting ECIGs or regulating them as tobacco products, medicinal products, or consumer products, among other categories (80). The discussion continues as to the regulatory policy options for ECIG regulation, in part because regulation may help address the rapid increase in ECIG use among youth.
Figure 2. Examples of electronic cigarettes.
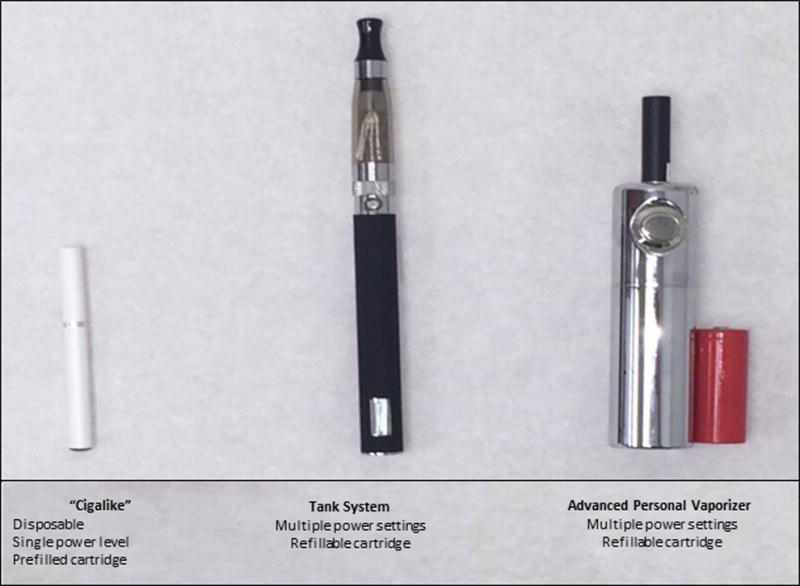
Cigalikes are ECIGs that visually resemble traditional tobacco cigarettes. They often have a single low power setting, and can be disposable, and often contain a prefilled cartridge. An open system ECIG has a single power setting, but usually a refillable cartridge and is not disposable. The advanced personal vaporizer has multiple power settings that can be altered by the user and has a refillable cartridge.
In the U.S. (81) and globally (82), ECIG use is increasing annually in all age groups, including adolescents (14, 15, 83). National youth tobacco surveys demonstrated a 3-fold increase in last 30-day use of ECIGs from 2011 to 2013 (participants in grades 6–12) (83), and higher use of ECIGs than tobacco cigarettes in 12th graders in 2014 (15). Among middle schoolers, in 2014, ECIGs were the most commonly used tobacco product with a past 30 day use prevalence of 3.9% (14). In a more recent survey, ECIG use in high school students (16%;2,390,000) and middle school students (5.3%;620,000) was the highest compared to the prevalence of other tobacco products including traditional tobacco cigarettes, cigars, waterpipe, smokeless tobacco, pipe tobacco, and bidis (84). The increased use of ECIGs in youth coupled with the unknown long term health effects of ECIGs is worrisome (85). Though not conclusive, some research suggests that early use of these products may lead to initiation of combustible tobacco products, such as cigarettes and hookah in adulthood (86, 87). And while adolescents use ECIGs for a variety of reasons such as experimentation (88), some adult ECIG users cite tobacco cigarette cessation as the reason (89, 90). However, the efficacy of ECIGs as a cessation aid is still uncertain (91–95, 96). A recent study reported that ECIG use not only failed to decrease tobacco use, but also decreased the likelihood of smoking cessation (97). Findings and conclusions are further complicated by the immense variety of ECIG devices, e-liquid composition, flavors, and nicotine content. More long term and well conducted studies are needed to understand the effects of ECIG use on cigarette smoking cessation. Unfortunately, while ECIG use clearly is increasing among U.S. youth and adults, the effects of long term ECIG use remain unknown.
3b. ECIG Toxicant Emissions and User Toxicant Exposure
The constituents of ECIG aerosol emissions are determined by device type, user experience and behavior, power, liquid contents, and materials that make up the heating element and device liquid reservoir (98–100). While some “cigalike” products deliver negligible amounts of nicotine to users (101,102), others deliver nicotine approximately in the same timeframe as a tobacco cigarette (100, 103), or even meet or perhaps exceed the nicotine delivery profile of a tobacco cigarette (98, 104). Nicotine emissions are influenced by puff topography and device voltage. For example, holding all other factors constant, doubling the puff duration can lead to approximately triple the amount of nicotine emitted by a device, while increasing the voltage from 3.3 to 5.2 V can lead to approximately a quadrupling of nicotine emitted (99). These results may help explain why devices that are more powerful electrically are now available.
ECIG use exposes users to much more than nicotine. Aerosol constituents can include glycols, aldehydes, metals, and volatile organic compounds (105), glyoxal and methyl glyoxal (106), and formaldehyde (107). Some constituents may be present in the liquid before aerosolization, while others may be formed during heating of the liquid (74). Flavorants can be a major source of aerosol toxicants. Each flavor has a unique chemical profile and thus, likely, a unique toxicant emissions profile. Importantly, many flavorants added to ECIG liquid are generally recognized as safe when ingested orally but have an unknown safety profile when heated, aerosolized, and inhaled. For example, diacetyl, a compound used in microwavable popcorn, has been identified in some ECIG liquids (103, 108). While this flavorant is safe to ingest orally, inhalation of it causes bronchiolitis obliterans, an irreversible pulmonary disorder that is otherwise known as ‘popcorn lung (108). One toxicant that perhaps deserves special mention is formaldehyde. There is little doubt that at least some ECIG device/liquid combinations are capable of generating formaldehyde (76, 103) though there is controversy as to the extent to which this formaldehyde is likely to be inhaled by the user (103, 109). Considering ECIGs are a rapidly evolving product and remain unregulated in many countries, a comprehensive understanding of ECIG toxicant emissions is required.
3c. Effect of ECIG on oral and systemic health: clinical studies
A few clinical studies (Table 3) have examined the health effects of exposure to ECIG aerosols using outcome measures such as blood flow (110), lung function and respiratory influences (111–115). A recent study investigated ECIG use as a cessation aid and reported that mucociliary clearance improved more in participants who quit smoking without any cessation aid compared to those who used ECIG (116). Data on health effects of ECIGs is sparse and is limited to specific device/liquid combinations that continue to evolve even as research is being conducted. While more studies are clearly needed, the absence of standardization of products and testing protocols suggest continued uncertainty regarding how long-term, daily use of these products will influence users.
Table 3.
Clinical Studies on the effects of ECIG use
| Health Outcomes of ECIG | Publication | Sample Size (n) | ECIG Device/Battery Voltage | Nicotine Concentration/Flavors |
|---|---|---|---|---|
| No effect on lung function and similar effect on serum cotinine levels as tobacco smokers | Flouris et al 2013111 | 30 | Giant, Nobacco G.P., Greece/not stated | 11 mg/ml/Nobacco USA Mix, Nobacco G.P., Greece |
| Negative effects on sinonasal symptoms and mucociliarly clearance | Kumral et al 2016116 | 98 | Multiple/variable | 11–12 mg/ml/variable flavors |
| Caused no changes in arterial stiffness | Szołtysek-Bołdys et al 2014113 | 15 | Ego-3 ECIGs (Volish Ltd, Poland)/3.4V | 24 mg/ml/not stated |
| Induces inhibition of cough reflex sensitivity | Dicpinigaitis et al 2016114 | 30 | Blu; Lorrilard Techinologies/not stated | 20–24 mg/ml/classic tobacco flavor |
| Increased blood flow in the buccal mucosa | Reuther et al 2016110 | 10 | Not stated | 0 or 16 mg/ml/not stated |
| Respiratory symptoms | Wang et al 2016112 | 45,128 | Not stated | Not stated |
| Cho and Paik 2016115 | 35,904 | Not stated | Not stated |
3d. Effect of ECIG on cellular/biological pathways: in vivo and in vitro studies
Long-term outcome studies investigating the biological effect of ECIG use are unavailable. A variety of studies have examined the effects of ECIG aerosols on various cell preparations and in vivo animal models and reported conflicting results. The variations in the results are likely due to the use of different device/liquids combinations and/or different methods to form the aerosols which may impact the ECIG emissions (Table 4) (117–124).
Table 4.
Preclinical Studies on the effects of ECIG use
| Health outcomes of ECIG | Publication | Study Type | Species | ECIG Device/Battery Voltage | Nicotine Concentration/Flavors |
|---|---|---|---|---|---|
| Cytotoxic effects | Romagna et al 2013117 | In vitro | Mouse | 510 T, Omega Vape, Manchester, UK/3.7 V | 0.8%/multiple |
| Increased inflammatory and oxidative stress response | Lerner et al 2015119 | In vitro and in vivo | Human and Mouse lung epithelial cells | eGo and Blu/not stated | 0, 6, 11,12, 16,18, 24 mg/ml/multiple |
| Cytotoxic effects on cardiomyoblasts | Farsalinos et al 2013123 | In vitro | Human | eGo, Joyetech, and Lavatube/3.7 or 4.7V | 0, 6, 8, 9, 11, 12,18, 24 mg/ml/multiple |
| Adverse effects on cardiac development | Palpant et al 2015120 | In vitro and in vivo | Human and Zebrafish embryos | Not stated | 16 mg/per cartridge/South Beach Smoke, Tobacco Classic, Full Flavored |
| Impaired phagocytosis and antimicrobial response against viruses and bacteria | Sussan et al 2015121 | In vivo | Mice | NJOY/not stated | 1.8%/menthol bold and traditional bold |
| Cytotoxic and genotoxic effects | Yu et al 2016122 | In vitro | Human epithelial cells and Head and Neck Squamous Carcinoma cell lines | V2 and VaporFi/not stated | 0% and 1.2% nicotine/Classic Tobacco and Red American Tobacco |
| Cytotoxic effects | Scheffler et al 2015125 | In vitro | Human bronchial epithelial cells | Reevo Mini-S/3.3V | 0 and 24 mg/ml/Tennessee Cured |
| Decreased cell proliferation but not cell death; inflammation | Husari et al 2016129 | In vivo and in vitro | Human and Mouse | V4L CoolCart/4.2V | 18 mg/ml/strawberry |
| Induces proteostasis/autophagy impairment leading to oxidative stress, apoptosis, and senescence | Shivalingappa et al 2015126 | In vivo and in vitro | Human bronchial epitheial cell line (Beas-2B) and mouse model | Kanger EVOD (Kangertech)/not stated | 25mg/ml/not stated |
| Cytotoxicity to airway cells, impaired immune response, increased inflammation and microbial virulence | Hwang et al 2016127 | In vitro and in vivo | Human epithelial cells and mouse model | multiple/not stated | 0, 6, 14, 18, 24, and 50 mg/ml/Treasury, none, Highlander Grog, California Blues |
| Withdrawal symptoms, cognitive deficit and anxiety-like behavior | Ponzoni et al 2015124 | In vivo | Mice | Not stated | 5.6 mg/session/not stated |
| Loss of lung endothelial barrier function and increased inflammation and oxidative stress response | Schweitzer et al 2015128 | In vitro and in vivo | Human lung microvascular endothelial cells and Mouse model | iClear 16/not stated | 0, 1–25 mM nicotine/Vanilla Dream, Kentucky Prime |
| Cytotoxicity in oral epithelial cells | Ji et al, 2016130 | In vitro | Human oral keratinocytes | multiple/not stated | 0 and 24 mg/ml/tobacco and menthol |
| Altered cellular morphology, increased apoptosis and L-lactate dehydrogenase (LDH) activity | Rouabhia et al 2016131 | In vitro | Human oral keratinocytes | EMOW/4.2V | 12 mg/ml/Smooth Canadian Tobacco |
| E-cigs with flavorings cause increased oxidative/carbonyl stress, inflammatory responses and DNA damage with histone deacetylase 2 (HDAC2) reduction. | Sundar et al 2016132 | In vitro | Human oral keratinocytes/periodontal ligament fibroblasts/fibroblasts and 3D | BLU®/not stated | 0 and13–16 mg/ml/Magnificent Menthol and Classic tobacco |
Reported adverse effects of ECIG aerosols in various cell types include decreased cell viability, increased rates of apoptosis, increased DNA strand breaks, changes in cell morphology and elevated inflammatory mediator production (117–123, 125–132). Flavors may exacerbate some of these negative effects (132). A recent study reported increased airway inflammation and impaired immune responses to viruses leading to increased morbidity and mortality following ECIG aerosol exposure in an in vivo murine model (121). The same study also reported impaired bacterial phagocytosis in the alveolar macrophages (121). In addition, some studies have examined the effect of un-aerosolized ECIG liquids in several in vitro cell cultures (133–135). However, as ECIG users are exposed to the products of aerosolized ECIG liquids, the results of studies utilizing un-aerosolized liquids need to be interpreted carefully.
In summary, though the data on short and long term effects of ECIG aerosol are sparse and inconclusive, the accumulating evidence supports the notion that chronic and long term exposure to ECIG aerosols may impact health negatively. Further research is warranted to determine the effects of ECIG aerosol exposure to oral and systemic health.
SUMMARY AND IMPLICATIONS FOR HEALTH CARE.
Underlying biological mechanisms of exacerbated severity and progression of periodontitis in cigarette smokers have been reviewed previously (3). Briefly, smoking may deregulate immune responses leading to heightened or suppressed inflammation in mucosal surfaces, impaired immunity to pathogens, and modulate microvasculature affecting healing and resolution of inflammation. Understanding the mechanisms of actions of cigarette smoke and its products in the host responses and oral microbiota is essential to develop more effective therapeutic and preventive strategies.
Use prevalence of waterpipe and ECIGs has recently increased around the world in part because there is a general belief that they are less harmful than conventional cigarettes. Waterpipe smoke, in particular, contains some of the same toxicants, including carcinogens, as cigarette smoke. Although studies are limited, emerging evidence reveals that WTS can cause similar deleterious biological effects as conventional cigarettes. In addition, some tobacco cigarette smokers have begun ECIG use as a smoking cessation aid. However, the extent to which ECIGs can help with cessation is unclear (91, 96,136). In fact, recently it was suggested that adolescents who try ECIGs are more likely to initiate use of cigarettes, cigars, and WPS than their peers who have not (85, 137).
The increased global prevalence of WTS and ECIG use warrants more research to elucidate their biological effects and impacts on therapeutic clinical outcomes in different parts of the body including oral cavity. Research efforts will require well designed epidemiological and clinical studies as well as development of in vivo and ex vivo methods that can model the effect of these new products on oral mucosa. Currently, health care professionals should not disregard the use of these products in patient care. Dental care professionals should become familiar with waterpipe, ECIGs, and other novel tobacco products, document their use in health records, communicate health effects to their patients, and be prepared to provide counseling for tobacco product use cessation.
Acknowledgments
The manuscript was supported by the National Institute of Dental and Craniofacial Research grant DE025037 (SES) and also by the National Institute on Drug Abuse of the National Institutes of Health under Award Number P50DA036105 and the Center for Tobacco Products of the U.S. Food and Drug Administration. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
Footnotes
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- 1.U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. http://www.surgeongeneral.gov/library/reports/50-years-of-progress/index.html#fullreport. [Google Scholar]
- 2.Chrcanovic BR, Albrektsson T, Wennerberg A. Smoking and dental implants: A systematic review and meta-analysis. J Dent. 2015;43:487–498. doi: 10.1016/j.jdent.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 3.Lee J, Taneja V, Vassallo R. Cigarette smoking and inflammation: cellular and molecular mechanisms. J Dent Res. 2012;91:142–149. doi: 10.1177/0022034511421200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nociti FH, Jr, Casati MZ, Duarte PM. Current perspective of the impact of smoking on the progression and treatment of periodontitis. Periodontol 2000. 2015;67:187–210. doi: 10.1111/prd.12063. [DOI] [PubMed] [Google Scholar]
- 5.Kotsakis GA, Javed F, Hinrichs JE, Karoussis IK, Romanos GE. Impact of cigarette smoking on clinical outcomes of periodontal flap surgical procedures: a systematic review and meta-analysis. J Periodontol. 2015;86:254–263. doi: 10.1902/jop.2014.140452. [DOI] [PubMed] [Google Scholar]
- 6.Fiorini T, Musskopf ML, Oppermann RV, Susin C. Is there a positive effect of smoking cessation on periodontal health? A systematic review. J Periodontol. 2014;85:83–91. doi: 10.1902/jop.2013.130047. [DOI] [PubMed] [Google Scholar]
- 7.Mombelli A, Muller N, Cionca N. The epidemiology of peri-implantitis. Clin Oral Implants Res. 2012;23(Suppl 6):67–76. doi: 10.1111/j.1600-0501.2012.02541.x. [DOI] [PubMed] [Google Scholar]
- 8.Smith CJ, Perfetti TA, Garg R, Hansch C. IARC carcinogens reported in cigarette mainstream smoke and their calculated log P values. Food Chem Toxicol. 2003;41:807–817. doi: 10.1016/s0278-6915(03)00021-8. [DOI] [PubMed] [Google Scholar]
- 9.World Health Organization (Tobacco Free Initiative): Advisory Note. Waterpipe Tobacco Smoking: Health Effects, Research Needs and Recommended Actions by Regulators. (2nd) http://www.who.int/tobacco/publications/prod_regulation/waterpipesecondedition/en/
- 10.Smith-Simone S, Maziak W, Ward KD, Eissenberg T. Waterpipe tobacco smoking: knowledge, attitudes, beliefs, and behavior in two U.S. samples. Nicotine Tob Res. 2008;10:393–398. doi: 10.1080/14622200701825023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maziak W, Ward KD, Afifi Soweid RA, Eissenberg T. Tobacco smoking using a waterpipe: a re-emerging strain in a global epidemic. Tob Control. 2004;13:327–333. doi: 10.1136/tc.2004.008169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cobb C, Ward KD, Maziak W, Shihadeh AL, Eissenberg T. Waterpipe tobacco smoking: an emerging health crisis in the United States. Am J Health Behav. 2010;34:275–285. doi: 10.5993/ajhb.34.3.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maziak W. The global epidemic of waterpipe smoking. Addict Behav. 2011;36:1–5. doi: 10.1016/j.addbeh.2010.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arrazola RA, Singh T, Corey CG, et al. Tobacco use among middle and high school students – United States, 2011–2014. MMWR Morb Mortal Wkly Rep. 2015;64:381–385. [PMC free article] [PubMed] [Google Scholar]
- 15.Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring the Future national survey results on drug use: 1975–2014: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. p. 52. [Google Scholar]
- 16.Haddad L, El-Shahawy O, Ghadban R, Barnett TE, Johnson E. Waterpipe Smoking and Regulation in the United States: A Comprehensive Review of the Literature. Int J Environ Res Public Health. 2015;12:6115–6135. doi: 10.3390/ijerph120606115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Awa F, Warren CW, Jones NR. Changes in tobacco use among 13–15-year-olds between 1999 and 2007: findings from the Eastern Mediterranean Region. East Mediterr Health J. 2010;16:266–273. [PubMed] [Google Scholar]
- 18.Jawad M, Wilson A, Lee JT, Jawad S, Hamilton FL, Millett C. Prevalence and predictors of water pipe and cigarette smoking among secondary school students in London. Nicotine Tob Res. 2013;15:2069–2075. doi: 10.1093/ntr/ntt103. [DOI] [PubMed] [Google Scholar]
- 19.Maziak W, Taleb ZB, Bahelah R, et al. The global epidemiology of waterpipe smoking. Tob Control. 2015;24(Suppl 1):i3–i12. doi: 10.1136/tobaccocontrol-2014-051903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Akl EA, Jawad M, Lam WY, Co CN, Obeid R, Irani J. Motives, beliefs and attitudes towards waterpipe tobacco smoking: a systematic review. Harm Reduct J. 2013;10:12. doi: 10.1186/1477-7517-10-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.St Helen G, Benowitz NL, Dains KM, Havel C, Peng M, Jacob P., 3rd Nicotine and carcinogen exposure after water pipe smoking in hookah bars. Cancer Epidemiol Biomarkers Prev. 2014;23:1055–1066. doi: 10.1158/1055-9965.EPI-13-0939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maziak W, Rastam S, Shihadeh AL, et al. Nicotine exposure in daily waterpipe smokers and its relation to puff topography. Addict Behav. 2011;36:397–399. doi: 10.1016/j.addbeh.2010.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eissenberg T, Shihadeh A. Waterpipe tobacco and cigarette smoking: direct comparison of toxicant exposure. Am J Prev Med. 2009;37:518–523. doi: 10.1016/j.amepre.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jacob P, 3rd, Abu Raddaha AH, Dempsey D, et al. Comparison of nicotine and carcinogen exposure with water pipe and cigarette smoking. Cancer Epidemiol Biomarkers Prev. 2013;22:765–772. doi: 10.1158/1055-9965.EPI-12-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aboaziza E, Eissenberg T. Waterpipe tobacco smoking: what is the evidence that it supports nicotine/tobacco dependence? Tob Control. 2015;24(Suppl 1):i44–i53. doi: 10.1136/tobaccocontrol-2014-051910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Primack BA, Khabour OF, Alzoubi KH, et al. The LWDS-10J: reliability and validity of the Lebanon Waterpipe Dependence Scale among university students in Jordan. Nicotine Tob Res. 2014;16:915–922. doi: 10.1093/ntr/ntu002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Salameh P, Waked M, Khoury F, et al. Waterpipe smoking and dependence are associated with chronic bronchitis: a case-control study in Lebanon. East Mediterr Health J. 2012;18:996–1004. doi: 10.26719/2012.18.10.996. [DOI] [PubMed] [Google Scholar]
- 28.Monzer B, Sepetdjian E, Saliba N, Shihadeh A. Charcoal emissions as a source of CO and carcinogenic PAH in mainstream narghile waterpipe smoke. Food Chem Toxicol. 2008;46:2991–2995. doi: 10.1016/j.fct.2008.05.031. [DOI] [PubMed] [Google Scholar]
- 29.Sepetdjian E, Shihadeh A, Saliba NA. Measurement of 16 polycyclic aromatic hydrocarbons in narghile waterpipe tobacco smoke. Food Chem Toxicol. 2008;46:1582–1590. doi: 10.1016/j.fct.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 30.Shihadeh AL, Eissenberg TE. Significance of smoking machine toxicant yields to blood-level exposure in water pipe tobacco smokers. Cancer Epidemiol Biomarkers Prev. 2011;20:2457–2460. doi: 10.1158/1055-9965.EPI-11-0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Primack BA, Carroll MV, Weiss PM, et al. Systematic Review and Meta-Analysis of Inhaled Toxicants from Waterpipe and Cigarette Smoking. Public Health Rep. 2016;131:76–85. doi: 10.1177/003335491613100114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shihadeh A, Schubert J, Klaiany J, El Sabban M, Luch A, Saliba NA. Toxicant content, physical properties and biological activity of waterpipe tobacco smoke and its tobacco-free alternatives. Tob Control. 2015;24(Suppl 1):i22–i30. doi: 10.1136/tobaccocontrol-2014-051907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang LW, He EY, Ghosh D, et al. Severe carbon monoxide poisoning from waterpipe smoking: a public health concern. Med J Aust. 2015;202:446–447. doi: 10.5694/mja14.01264. [DOI] [PubMed] [Google Scholar]
- 34.El-Zaatari ZM, Chami HA, Zaatari GS. Health effects associated with waterpipe smoking. Tob Control. 2015;24(Suppl 1):i31–i43. doi: 10.1136/tobaccocontrol-2014-051908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.von Rappard J, Schonenberger M, Barlocher L. Carbon monoxide poisoning following use of a water pipe/hookah. Dtsch Arztebl Int. 2014;111:674–679. doi: 10.3238/arztebl.2014.0674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.La Fauci G, Weiser G, Steiner IP, Shavit I. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. CJEM. 2012;14:57–59. doi: 10.2310/8000.2011.110431. [DOI] [PubMed] [Google Scholar]
- 37.Ashurst JV, Urquhart M, Cook MD. Carbon monoxide poisoning secondary to hookah smoking. J Am Osteopath Assoc. 2012;112:686–688. [PubMed] [Google Scholar]
- 38.Lim BL, Lim GH, Seow E. Case of carbon monoxide poisoning after smoking shisha. Int J Emerg Med. 2009;2:121–122. doi: 10.1007/s12245-009-0097-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ozkan S, Ozturk T, Ozmen Y, Durukan P. Syncope Associated with Carbon Monoxide Poisoning due to Narghile Smoking. Case Rep Emerg Med. 2013;2013:796857. doi: 10.1155/2013/796857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cobb CO, Vansickel AR, Blank MD, Jentink K, Travers MJ, Eissenberg T. Indoor air quality in Virginia waterpipe cafes. Tob Control. 2013;22:338–343. doi: 10.1136/tobaccocontrol-2011-050350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aoun J, Saleh N, Waked M, Salame J, Salameh P. Lung cancer correlates in Lebanese adults: a pilot case–control study. J Epidemiol Glob Health. 2013;3:235–244. doi: 10.1016/j.jegh.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gupta D, Boffetta P, Gaborieau V, Jindal SK. Risk factors of lung cancer in Chandigarh, India. Indian J Med Res. 2001;113:142–150. [PubMed] [Google Scholar]
- 43.Tamim H, Musharrafieh U, El Roueiheb Z, Yunis K, Almawi WY. Exposure of children to environmental tobacco smoke (ETS) and its association with respiratory ailments. J Asthma. 2003;40:571–576. doi: 10.1081/jas-120019029. [DOI] [PubMed] [Google Scholar]
- 44.Haddad L, Kelly DL, Weglicki LS, Barnett TE, Ferrell AV, Ghadban R. A Systematic Review of Effects of Waterpipe Smoking on Cardiovascular and Respiratory Health Outcomes. Tob Use Insights. 2016;9:13–28. doi: 10.4137/TUI.S39873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alomari MA, Khabour OF, Alzoubi KH, Shqair DM, Eissenberg T. Central and peripheral cardiovascular changes immediately after waterpipe smoking. Inhal Toxicol. 2014;26:579–587. doi: 10.3109/08958378.2014.936572. [DOI] [PubMed] [Google Scholar]
- 46.Layoun N, Saleh N, Barbour B, et al. Waterpipe effects on pulmonary function and cardiovascular indices: a comparison to cigarette smoking in real life situation. Inhal Toxicol. 2014;26:620–627. doi: 10.3109/08958378.2014.945106. [DOI] [PubMed] [Google Scholar]
- 47.Mirahmadizadeh A, Nakhaee N. Prevalence of waterpipe smoking among rural pregnant women in Southern Iran. Med Princ Pract. 2008;17:435–439. doi: 10.1159/000151563. [DOI] [PubMed] [Google Scholar]
- 48.Nuwayhid IA, Yamout B, Azar G, Kambris MA. Narghile (hubble-bubble) smoking, low birth weight, and other pregnancy outcomes. Am J Epidemiol. 1998;148:375–383. doi: 10.1093/oxfordjournals.aje.a009656. [DOI] [PubMed] [Google Scholar]
- 49.Tamim H, Yunis KA, Chemaitelly H, Alameh M, Nassar AH, National Collaborative Perinatal Neonatal Network Beirut L Effect of narghile and cigarette smoking on newborn birthweight. BJOG. 2008;115:91–97. doi: 10.1111/j.1471-0528.2007.01568.x. [DOI] [PubMed] [Google Scholar]
- 50.Alomari MA, Khabour OF, Alzoubi KH, Shqair DM, Stoner L. Acute vascular effects of waterpipe smoking: Importance of physical activity and fitness status. Atherosclerosis. 2015;240:472–476. doi: 10.1016/j.atherosclerosis.2015.02.047. [DOI] [PubMed] [Google Scholar]
- 51.Strulovici-Barel Y, Shaykhiev R, Salit J, et al. Pulmonary Abnormalities in Young, Light-Use Waterpipe (Hookah) Smokers. Am J Respir Crit Care Med. 2016;194:587–595. doi: 10.1164/rccm.201512-2470OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Al-Belasy FA. The relationship of “shisha” (water pipe) smoking to postextraction dry socket. J Oral Maxillofac Surg. 2004;62:10–14. doi: 10.1016/j.joms.2002.11.001. [DOI] [PubMed] [Google Scholar]
- 53.Bibars AR, Obeidat SR, Khader Y, Mahasneh AM, Khabour OF. The Effect of Waterpipe Smoking on Periodontal Health. Oral Health Prev Dent. 2015;13:253–259. doi: 10.3290/j.ohpd.a32671. [DOI] [PubMed] [Google Scholar]
- 54.Warnakulasuriya S. Waterpipe smoking, oral cancer and other oral health effects. Evid Based Dent. 2011;12:44–45. doi: 10.1038/sj.ebd.6400790. [DOI] [PubMed] [Google Scholar]
- 55.Munshi T, Heckman CJ, Darlow S. Association between tobacco waterpipe smoking and head and neck conditions: A systematic review. J Am Dent Assoc. 2015;146:760–766. doi: 10.1016/j.adaj.2015.04.014. [DOI] [PubMed] [Google Scholar]
- 56.Javed F, Al-Kheraif AA, Rahman I, et al. Comparison of Clinical and Radiographic Periodontal Status Between Habitual Water-Pipe Smokers and Cigarette Smokers. J Periodontol. 2016;87:142–147. doi: 10.1902/jop.2015.150235. [DOI] [PubMed] [Google Scholar]
- 57.Natto S, Baljoon M, Abanmy A, Bergstrom J. Tobacco smoking and gingival health in a Saudi Arabian population. Oral Health Prev Dent. 2004;2:351–357. [PubMed] [Google Scholar]
- 58.Natto S, Baljoon M, Bergstrom J. Tobacco smoking and periodontal bone height in a Saudi Arabian population. J Clin Periodontol. 2005;32:1000–1006. doi: 10.1111/j.1600-051X.2005.00813.x. [DOI] [PubMed] [Google Scholar]
- 59.Natto S, Baljoon M, Bergstrom J. Tobacco smoking and periodontal health in a Saudi Arabian population. J Periodontol. 2005;76:1919–1926. doi: 10.1902/jop.2005.76.11.1919. [DOI] [PubMed] [Google Scholar]
- 60.Baljoon M, Natto S, Abanmy A, Bergstrom J. Smoking and vertical bone defects in a Saudi Arabian population. Oral Health Prev Dent. 2005;3:173–182. [PubMed] [Google Scholar]
- 61.Al-Amad SH, Awad MA, Nimri O. Oral cancer in young Jordanians: potential association with frequency of narghile smoking. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:560–565. doi: 10.1016/j.oooo.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 62.Dangi J, Kinnunen TH, Zavras AI. Challenges in global improvement of oral cancer outcomes: findings from rural Northern India. Tob Induc Dis. 2012;10:5. doi: 10.1186/1617-9625-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khemiss M, Ben Khelifa M, Ben Rejeb M, Ben Saad H. Periodontal bone height of exclusive narghile smokers compared with exclusive cigarette smokers. Libyan J Med. 2016;11:31689. doi: 10.3402/ljm.v11.31689. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Alzoubi KH, Khabour OF, Alharahshah EA, Alhashimi FH, Shihadeh A, Eissenberg T. The Effect of Waterpipe Tobacco Smoke Exposure on Learning and Memory Functions in the Rat Model. J Mol Neurosci. 2015;57:249–256. doi: 10.1007/s12031-015-0613-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khabour OF, Alzoubi KH, Abu Thiab TM, Al-Husein BA, Eissenberg T, Shihadeh AL. Changes in the expression and protein level of matrix metalloproteinases after exposure to waterpipe tobacco smoke. Inhal Toxicol. 2015;27:689–693. doi: 10.3109/08958378.2015.1085471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Khabour OF, Alzoubi KH, Bani-Ahmad M, Dodin A, Eissenberg T, Shihadeh A. Acute exposure to waterpipe tobacco smoke induces changes in the oxidative and inflammatory markers in mouse lung. Inhal Toxicol. 2012;24:667–675. doi: 10.3109/08958378.2012.710918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rammah M, Dandachi F, Salman R, Shihadeh A, El-Sabban M. In vitro effects of waterpipe smoke condensate on endothelial cell function: a potential risk factor for vascular disease. Toxicol Lett. 2013;219:133–142. doi: 10.1016/j.toxlet.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Seifi S, Feizi F, Mehdizadeh M, Khafri S, Ahmadi B. Evaluation of cytological alterations of oral mucosa in smokers and waterpipe users. Cell J. 2014;15:302–309. [PMC free article] [PubMed] [Google Scholar]
- 69.Shihadeh A, Eissenberg T, Rammah M, Salman R, Jaroudi E, El-Sabban M. Comparison of tobacco-containing and tobacco-free waterpipe products: effects on human alveolar cells. Nicotine Tob Res. 2014;16:496–499. doi: 10.1093/ntr/ntt193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.El-Setouhy M, Loffredo CA, Radwan G, et al. Genotoxic effects of waterpipe smoking on the buccal mucosa cells. Mutat Res. 2008;655:36–40. doi: 10.1016/j.mrgentox.2008.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Alsatari ES, Azab M, Khabour OF, Alzoubi KH, Sadiq MF. Assessment of DNA damage using chromosomal aberrations assay in lymphocytes of waterpipe smokers. Int J Occup Med Environ Health. 2012;25:218–224. doi: 10.2478/S13382-012-0027-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Khabour OF, Alsatari ES, Azab M, Alzoubi KH, Sadiq MF. Assessment of genotoxicity of waterpipe and cigarette smoking in lymphocytes using the sister-chromatid exchange assay: a comparative study. Environ Mol Mutagen. 2011;52:224–228. doi: 10.1002/em.20601. [DOI] [PubMed] [Google Scholar]
- 73.Al-Amrah HJ, Aboznada OA, Alam MZ, ElAssouli MZ, Mujallid MI, ElAssouli SM. Genotoxicity of waterpipe smoke in buccal cells and peripheral blood leukocytes as determined by comet assay. Inhal Toxicol. 2014;26:891–896. doi: 10.3109/08958378.2014.970787. [DOI] [PubMed] [Google Scholar]
- 74.Breland A, Soule E, Lopez A, Ramoa C, El-Hellani A, Eissenberg T. Electronic cigarettes: what are they and what do they do? Ann N Y Acad Sci. 2016 doi: 10.1111/nyas.12977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Khabour OF, Alzoubi KH, Al-Sheyab N, Shihadeh A, Eissenberg T. Investigating the Effects of Exposure to Waterpipe Smoke on Pregnancy Outcomes Using an Animal Model. Nicotine Tob Res. 2016;18:585–589. doi: 10.1093/ntr/ntv275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Talih S, Balhas Z, Salman R, Karaoghlanian N, Shihadeh A. “Direct Dripping”: A High-Temperature, High-Formaldehyde Emission Electronic Cigarette Use Method. Nicotine Tob Res. 2016;18:453–459. doi: 10.1093/ntr/ntv080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhu SH, Sun JY, Bonnevie E, et al. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23(Suppl 3):iii3–9. doi: 10.1136/tobaccocontrol-2014-051670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Etter JF. A longitudinal study of cotinine in long-term daily users of e-cigarettes. Drug Alcohol Depend. 2016;160:218–221. doi: 10.1016/j.drugalcdep.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 79.U.S. Department of Health and Human Services. Food and Drug Administration. Deeming Tobacco Products To Be Subject to the Federal Food, Drug, and Cosmetic Act, as Amended by the Family Smoking Prevention and Tobacco Control Act 2014. Docket No. FDA-2014-N-0189. [Google Scholar]
- 80.Institute for Global Tobacco Control. Country Laws Regulating E-cigarettes: A Policy Scan. Baltimore, MD: Johns Hopkins Bloomberg School of Public Health; http://globaltobaccocontrol.org/e-cigarette/country-laws-regulating-e-cigarettes. [Google Scholar]
- 81.McMillen RC, Gottlieb MA, Shaefer RM, Winickoff JP, Klein JD. Trends in Electronic Cigarette Use Among U.S. Adults: Use is Increasing in Both Smokers and Nonsmokers. Nicotine Tob Res. 2015;17:1195–1202. doi: 10.1093/ntr/ntu213. [DOI] [PubMed] [Google Scholar]
- 82.Gravely S, Fong GT, Cummings KM, et al. Correction: Gravely, S., et al. Awareness, Trial, and Current Use of Electronic Cigarettes in 10 Countries: Findings from the ITC Project. Int J Environ Res Public Health. 2014;11:11691–11704. doi: 10.3390/ijerph111111691. [DOI] [PMC free article] [PubMed] [Google Scholar]; Int J Environ Res Public Health. 2015;12:4631–4637. [Google Scholar]
- 83.Bunnell RE, Agaku IT, Arrazola RA, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013. Nicotine Tob Res. 2015;17:228–235. doi: 10.1093/ntr/ntu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Singh T, Arrazola RA, Corey CG, et al. Tobacco Use Among Middle and High School Students–United States, 2011–2015. MMWR Morb Mortal Wkly Rep. 2016;65:361–367. doi: 10.15585/mmwr.mm6514a1. [DOI] [PubMed] [Google Scholar]
- 85.Rennie LJ, Bazillier-Bruneau C, Rouesse J. Harm Reduction or Harm Introduction? Prevalence and Correlates of E-Cigarette Use Among French Adolescents. J Adolesc Health. 2016;58:440–445. doi: 10.1016/j.jadohealth.2015.12.013. [DOI] [PubMed] [Google Scholar]
- 86.U.S. Department of Health and Human Services. E-Cigarette Use Among Youth and Young Adults A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. https://e-cigarettes.surgeongeneral.gov/documents/2016_SGR_Full_Report_non-508.pdf. [Google Scholar]
- 87.Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to Traditional Cigarette Smoking After Electronic Cigarette Use Among US Adolescents and Young Adults. JAMA Pediatr. 2015;169:1018–23. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Barrington-Trimis JL, Urman R, Berhane K, Unger JB, Cruz TB, Pentz MA, Samet JM, Leventhal AM, McConnell R. E-Cigarettes and Future Cigarette Use. Pediatrics. 2016:138. doi: 10.1542/peds.2016-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Li J, Newcombe R, Walton D. The prevalence, correlates and reasons for using electronic cigarettes among New Zealand adults. Addict Behav. 2015;45:245–251. doi: 10.1016/j.addbeh.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 90.Grana RA, Popova L, Ling PM. A longitudinal analysis of electronic cigarette use and smoking cessation. JAMA Intern Med. 2014;174:812–813. doi: 10.1001/jamainternmed.2014.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382:1629–1637. doi: 10.1016/S0140-6736(13)61842-5. [DOI] [PubMed] [Google Scholar]
- 92.McRobbie H, Bullen C, Hartmann-Boyce J, Hajek P. Electronic cigarettes for smoking cessation and reduction. Cochrane Database Syst Rev. 2014:CD010216. doi: 10.1002/14651858.CD010216.pub2. [DOI] [PubMed] [Google Scholar]
- 93.Tseng TY, Ostroff JS, Campo A, et al. A Randomized Trial Comparing the Effect of Nicotine Versus Placebo Electronic Cigarettes on Smoking Reduction Among Young Adult Smokers. Nicotine Tob Res. 2016;18:1937–1943. doi: 10.1093/ntr/ntw017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kalkhoran S, Glantz SA. E-cigarettes and smoking cessation in real-world and clinical settings: a systematic review and meta-analysis. Lancet Respir Med. 2016;4:116–128. doi: 10.1016/S2213-2600(15)00521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Malas M, van der Tempel J, Schwartz R, et al. Electronic Cigarettes for Smoking Cessation: A Systematic Review. Nicotine Tob Res. 2016;18:1926–1936. doi: 10.1093/ntr/ntw119. [DOI] [PubMed] [Google Scholar]
- 96.McQueen N, Partington EJ, Harrington KF, Rosenthal EL, Carroll WR, Schmalbach CE. Smoking Cessation and Electronic Cigarette Use among Head and Neck Cancer Patients. Otolaryngol Head Neck Surg. 2016;154:73–79. doi: 10.1177/0194599815613279. [DOI] [PubMed] [Google Scholar]
- 97.Ramoa CP, Hiler MM, Spindle TR, et al. Electronic cigarette nicotine delivery can exceed that of combustible cigarettes: a preliminary report. Tob Control. 2016;25:e6–9. doi: 10.1136/tobaccocontrol-2015-052447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Talih S, Balhas Z, Eissenberg T, et al. Effects of user puff topography, device voltage, and liquid nicotine concentration on electronic cigarette nicotine yield: measurements and model predictions. Nicotine Tob Res. 2015;17:150–157. doi: 10.1093/ntr/ntu174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vansickel AR, Eissenberg T. Electronic cigarettes: effective nicotine delivery after acute administration. Nicotine Tob Res. 2013;15:267–270. doi: 10.1093/ntr/ntr316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev. 2016 Sep 14;9:CD010216. doi: 10.1002/14651858.CD010216.pub3. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Eissenberg T. Electronic nicotine delivery devices: ineffective nicotine delivery and craving suppression after acute administration. Tob Control. 2010;19:87–88. doi: 10.1136/tc.2009.033498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Yan XS, D’Ruiz C. Effects of using electronic cigarettes on nicotine delivery and cardiovascular function in comparison with regular cigarettes. Regul Toxicol Pharmacol. 2015;71:24–34. doi: 10.1016/j.yrtph.2014.11.004. [DOI] [PubMed] [Google Scholar]
- 103.Farsalinos KE, Kistler KA, Gillman G, Voudris V. Evaluation of electronic cigarette liquids and aerosol for the presence of selected inhalation toxins. Nicotine Tob Res. 2015;17:168–174. doi: 10.1093/ntr/ntu176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dawkins LE, Kimber CF, Doig M, Feyerabend C, Corcoran O. Self-titration by experienced e-cigarette users: blood nicotine delivery and subjective effects. Psychopharmacology (Berl) 2016;233:2933–2941. doi: 10.1007/s00213-016-4338-2. [DOI] [PubMed] [Google Scholar]
- 105.Cheng T. Chemical evaluation of electronic cigarettes. Tob Control. 2014;23(Suppl 2):ii11–17. doi: 10.1136/tobaccocontrol-2013-051482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Uchiyama S, Ohta K, Inaba Y, Kunugita N. Determination of carbonyl compounds generated from the E-cigarette using coupled silica cartridges impregnated with hydroquinone and 2,4-dinitrophenylhydrazine, followed by high-performance liquid chromatography. Anal Sci. 2013;29:1219–1222. doi: 10.2116/analsci.29.1219. [DOI] [PubMed] [Google Scholar]
- 107.Jensen RP, Luo W, Pankow JF, Strongin RM, Peyton DH. Hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372:392–394. doi: 10.1056/NEJMc1413069. [DOI] [PubMed] [Google Scholar]
- 108.Allen JG, Flanigan SS, LeBlanc M, et al. Flavoring Chemicals in E-Cigarettes: Diacetyl, 2,3-Pentanedione, and Acetoin in a Sample of 51 Products, Including Fruit-, Candy-, and Cocktail-Flavored E-Cigarettes. Environ Health Perspect. 2016;124:733–739. doi: 10.1289/ehp.1510185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Pankow JF, Strongin RM, Peyton DH. More on hidden formaldehyde in e-cigarette aerosols. N Engl J Med. 2015;372:1576–1577. doi: 10.1056/NEJMc1502242. [DOI] [PubMed] [Google Scholar]
- 110.Reuther WJ, Hale B, Matharu J, Blythe JN, Brennan PA. Do you mind if I vape? Immediate effects of electronic cigarettes on perfusion in buccal mucosal tissue–a pilot study. Br J Oral Maxillofac Surg. 2016;54:338–341. doi: 10.1016/j.bjoms.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 111.Flouris AD, Chorti MS, Poulianiti KP, et al. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhal Toxicol. 2013;25:91–101. doi: 10.3109/08958378.2012.758197. [DOI] [PubMed] [Google Scholar]
- 112.Wang MP, Ho SY, Leung LT, Lam TH. Electronic Cigarette Use and Respiratory Symptoms in Chinese Adolescents in Hong Kong. JAMA Pediatr. 2016;170:89–91. doi: 10.1001/jamapediatrics.2015.3024. [DOI] [PubMed] [Google Scholar]
- 113.Szoltysek-Boldys I, Sobczak A, Zielinska-Danch W, Barton A, Koszowski B, Kosmider L. Influence of inhaled nicotine source on arterial stiffness. Przegl Lek. 2014;71:572–575. [PubMed] [Google Scholar]
- 114.Dicpinigaitis PV, Lee Chang A, Dicpinigaitis AJ, Negassa A. Effect of Electronic Cigarette Use on the Urge-to-Cough Sensation. Nicotine Tob Res. 2016;18:1763–1765. doi: 10.1093/ntr/ntw021. [DOI] [PubMed] [Google Scholar]
- 115.Cho JH, Paik SY. Association between Electronic Cigarette Use and Asthma among High School Students in South Korea. PLoS One. 2016;11:e0151022. doi: 10.1371/journal.pone.0151022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kumral TL, Salturk Z, Yildirim G, et al. How does electronic cigarette smoking affect sinonasal symptoms and nasal mucociliary clearance? B-ENT. 2016;12:17–21. [PubMed] [Google Scholar]
- 117.Romagna G, Allifranchini E, Bocchietto E, Todeschi S, Esposito M, Farsalinos KE. Cytotoxicity evaluation of electronic cigarette vapor extract on cultured mammalian fibroblasts (ClearStream-LIFE): comparison with tobacco cigarette smoke extract. Inhal Toxicol. 2013;25:354–361. doi: 10.3109/08958378.2013.793439. [DOI] [PubMed] [Google Scholar]
- 118.Salturk Z, Cakir C, Sunnetci G, et al. Effects of Electronic Nicotine Delivery System on Larynx: Experimental Study. J Voice. 2015;29:560–563. doi: 10.1016/j.jvoice.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 119.Lerner CA, Sundar IK, Yao H, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One. 2015;10:e0116732. doi: 10.1371/journal.pone.0116732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Palpant NJ, Hofsteen P, Pabon L, Reinecke H, Murry CE. Cardiac development in zebrafish and human embryonic stem cells is inhibited by exposure to tobacco cigarettes and e-cigarettes. PLoS One. 2015;10:e0126259. doi: 10.1371/journal.pone.0126259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sussan TE, Gajghate S, Thimmulappa RK, et al. Exposure to electronic cigarettes impairs pulmonary anti-bacterial and anti-viral defenses in a mouse model. PLoS One. 2015;10:e0116861. doi: 10.1371/journal.pone.0116861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yu V, Rahimy M, Korrapati A, et al. Electronic cigarettes induce DNA strand breaks and cell death independently of nicotine in cell lines. Oral Oncol. 2016;52:58–65. doi: 10.1016/j.oraloncology.2015.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Farsalinos KE, Romagna G, Allifranchini E, et al. Comparison of the cytotoxic potential of cigarette smoke and electronic cigarette vapour extract on cultured myocardial cells. Int J Environ Res Public Health. 2013;10:5146–5162. doi: 10.3390/ijerph10105146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ponzoni L, Moretti M, Sala M, et al. Different physiological and behavioural effects of e-cigarette vapour and cigarette smoke in mice. Eur Neuropsychopharmacol. 2015;25:1775–1786. doi: 10.1016/j.euroneuro.2015.06.010. [DOI] [PubMed] [Google Scholar]
- 125.Scheffler S, Dieken H, Krischenowski O, Forster C, Branscheid D, Aufderheide M. Evaluation of E-cigarette liquid vapor and mainstream cigarette smoke after direct exposure of primary human bronchial epithelial cells. Int J Environ Res Public Health. 2015;12:3915–3925. doi: 10.3390/ijerph120403915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Shivalingappa PC, Hole R, Westphal CV, Vij N. Airway Exposure to E-Cigarette Vapors Impairs Autophagy and Induces Aggresome Formation. Antioxid Redox Signal. 2015 doi: 10.1089/ars.2015.6367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Hwang JH, Lyes M, Sladewski K, et al. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J Mol Med (Berl) 2016;94:667–679. doi: 10.1007/s00109-016-1378-3. [DOI] [PubMed] [Google Scholar]
- 128.Schweitzer KS, Chen SX, Law S, et al. Endothelial disruptive proinflammatory effects of nicotine and e-cigarette vapor exposures. Am J Physiol Lung Cell Mol Physiol. 2015;309:L175–187. doi: 10.1152/ajplung.00411.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Husari A, Shihadeh A, Talih S, Hashem Y, El Sabban M, Zaatari G. Acute Exposure to Electronic and Combustible Cigarette Aerosols: Effects in an Animal Model and in Human Alveolar Cells. Nicotine Tob Res. 2016;18:613–619. doi: 10.1093/ntr/ntv169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ji EH, Sun B, Zhao T, Shu S, Chang CH, Messadi D, Xia T, Zhu Y, Hu S. Characterization of Electronic Cigarette Aerosol and Its Induction of Oxidative Stress Response in Oral Keratinocytes. PLoS One. 2016;11:e0154447. doi: 10.1371/journal.pone.0154447. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rouabhia M, Park HJ, Semlali A, Zakrzewski A, Chmielewski W, Chakir J. E-Cigarette Vapor Induces an Apoptotic Response in Human Gingival Epithelial Cells Through the Caspase-3 Pathway. J Cell Physiol. 2016 doi: 10.1002/jcp.25677. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 132.Sundar IK, Javed F, Romanos GE, Rahman I. E-cigarettes and flavorings induce inflammatory and pro-senescence responses in oral epithelial cells and periodontal fibroblasts. Oncotarget. 2016 Oct 24; doi: 10.18632/oncotarget.12857. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Willershausen I, Wolf T, Weyer V, Sader R, Ghanaati S, Willershausen B. Influence of E-smoking liquids on human periodontal ligament fibroblasts. Head Face Med. 2014;10:39. doi: 10.1186/1746-160X-10-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sancilio S, Gallorini M, Cataldi A, di Giacomo V. Cytotoxicity and apoptosis induction by e-cigarette fluids in human gingival fibroblasts. Clin Oral Investig. 2016;20:477–483. doi: 10.1007/s00784-015-1537-x. [DOI] [PubMed] [Google Scholar]
- 135.Wu Q, Jiang D, Minor M, Chu HW. Electronic cigarette liquid increases inflammation and virus infection in primary human airway epithelial cells. PLoS One. 2014;9:e108342. doi: 10.1371/journal.pone.0108342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Al-Delaimy WK, Myers MG, Leas EC, Strong DR, Hofstetter CR. E-cigarette use in the past and quitting behavior in the future: a population-based study. Am J Public Health. 2015;105:1213–1219. doi: 10.2105/AJPH.2014.302482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, Williams RJ. Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tob Control. 2016 doi: 10.1136/tobaccocontrol-2015-052705. [DOI] [PMC free article] [PubMed] [Google Scholar]


