To the Editor
Electronic health record (EHR) implementation may affect time allocation during patient visits.1 Clinicians may use EHRs in silence, risking lower patient satisfaction,2 or by multitasking while talking with patients. Concurrent multitasking (performing ≥2 tasks simultaneously) is associated with increased error risk and time to complete tasks.3 We studied time allocation and transitions into and out of silent EHR use in clinics after EHR implementation.
Methods
This observational study (2013–2015) included five primary and specialty safety net clinics transitioning from basic to fully-functional EHR. Eligible English-/Spanish-speaking adults with chronic conditions were enrolled and interviewed in a pre-EHR implementation study (N=47).4 Eligible clinicians (N=39) included physicians and nurse practitioners. Research assistants video-recorded visits 3–16 months (median 9) after EHR implementation. After visits, patients rated recent quality of care (poor to excellent).
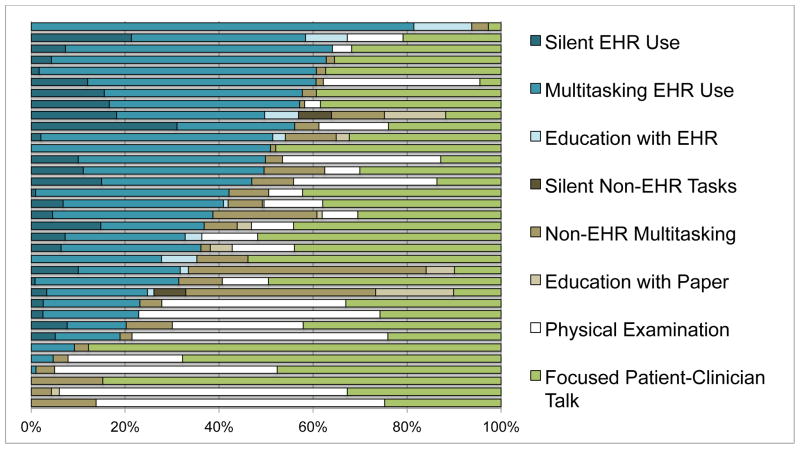
Two researchers coded visits using mutually exclusive categories (Figure): multitasking EHR use (while clinician or patient spoke); silent EHR use (≥3 second silence); non-EHR multitasking; silent non-EHR tasks; education with EHR; education with paper; physical examination; and focused patient-clinician talk. For each category, we calculated total proportion of visit time and sample medians (interquartile ranges).
Figure. Time allocation in a study of electronic health record use in primary and specialty care (n=35 encounters)*.
*Multitasking EHR use: clinicians used EHR while clinicians or patients spoke; Silent EHR use: clinicians used EHR in silences > 3 seconds; Non-EHR multitasking: clinicians completed non-EHR tasks while clinicians or patients spoke; Silent non-EHR tasks: clinicians completed non-EHR tasks in silences > 3 seconds; Education with EHR: clinicians used EHRs to counsel patients; Education with paper: clinicians used paper to counsel patients; Physical examination: clinicians examined patients; Focused patient-clinician talk: clinicians and patients spoke with no clinician tasks.
We qualitatively coded EHR tasks conducted silently and communication transitioning into and out of silent EHR use. We compared patients rating care as “excellent” after visits above and below median multitasking EHR use, using generalized estimating equations regression.
Results
Among 35 visits between 25 patients and 25 clinicians, 17% were in Spanish and 40% of relationships were >5 years (Table). Median visit length was 20.6 minutes.
Table.
Patient, clinician, and encounter characteristics in a study of electronic health record use in safety net primary and specialty care
| Characteristic | Value |
|---|---|
|
| |
| Patients (n=25) | |
| Mean age, y (SD) | 56.8 (11.0) |
| Women, n (%) | 11 (44.0) |
| Hispanic, n (%) | 12 (48.0) |
| Asian, n (%) | 6 (24.0) |
| White, n (%) | 4 (16.0) |
| African-American, n (%) | 2 (8.0) |
| Multiethnic, n (%) | 1 (4.0) |
| Primary Language Spanish, n (%) | 10 (40.0) |
| Limited English proficiency, n (%)* | 6 (24.0) |
| ≤ 8th grade education, n (%) | 2 (8.0) |
| Some high school or graduate/GED, n (%) | 7 (28.0) |
| Some college or college graduate, n (%) | 16 (64.0) |
| Limited health literacy, n (%)† | 5 (20.0) |
| Income ≤ $20,000/year, n (%) | 23 (92.0) |
|
| |
| Clinicians (n=25) | |
| Mean age, y (SD) | 44.9 (11.9) |
| Women, n (%) | 14 (66.7) |
| Primary care clinic, n (%) | 14 (56.0) |
| Diabetes clinic, n (%) | 5 (20.0) |
| Cardiology clinic, n (%) | 3 (12.0) |
| Rheumatology clinic, n (%) | 3 (12.0) |
| Physician, n (%) | 21 (84.0) |
| Nurse practitioner or physician assistant, n (%) | 4 (16.0) |
| Years since professional degree, mean (SD) | 15.7 (11.3) |
|
| |
| Encounters (n=35) | |
| Relationship length years at baseline, n (%) | |
| < 1 year | 2 (5.7) |
| 1–5 years | 19 (54.3) |
| >5 years | 14 (40.0) |
| Language during encounter, n (%) | |
| English | 29 (82.9) |
| Spanish | 5 (14.3) |
| Spanish interpreter | 1 (2.9) |
| Electronic health record (EHR) use during visit, n (%) | |
| Multitasking EHR and Silent EHR Use | 26 (74.2) |
| Multitasking EHR only | 6 (17.1) |
| No EHR use | 3 (8.6) |
| Visit length in minutes, median (IQR) | 20.6 (16.7 – 32.2) |
| Proportion (%) of visit time during encounters, median (IQR) | |
| Multitasking EHR use | 30.5 (20.4 – 41.2) |
| Silent EHR use | 4.6 (0.0 – 11.1) |
| Patient education using EHR | 0.0 (0.0 – 1.0) |
| Multitasking non-EHR tasks | 4.3 (2.0 – 10.8) |
| Silent non-EHR tasks | 0.0 (0.0 – 0.0) |
| Patient education using paper | 0.0 (0.0 – 0.4) |
| Physical examination | 9.0 (0.0 – 30.5) |
| Focused patient-clinician talk | 33.1 (0.24 – 44.2) |
Spanish-speaking patients who reported English proficiency less than “very well.”
Somewhat, a little bit, or not at all confident “filling out medical forms by yourself”
The Table shows visit time proportions. Multitasking EHR use comprised 30.5% of visit time, silent EHR 4.6%, multitasking non-EHR tasks 4.3%, and focused patient-clinician talk 33.1%. The Figure shows that multitasking time exceeded silent EHR use.
Patients rated care “excellent” after 66.7% of low multitasking EHR use visits and 76.5% of high multitasking EHR visits (p=0.65).
Silent EHR use (n=193 instances) occurred while clinicians viewed (39.4%) or entered (24.4%) information, prescribed (13.5%), reconciled medications (8.3%), arranged appointments (5.2%), ordered tests or referrals (5.2%), and sought or typed patient education (3.1%). The median silent EHR use lasted 16.2 seconds, shortest for viewing information (4.6) and longest for patient education (34.0).
Qualitative analysis revealed:
Clinicians demonstrated various transitions into silent EHR use. Sometimes clinicians signaled a need to focus (“Give me a minute, I want to review in the computer what we’ve done before.”). Other times, clinicians shifted into silence without warning (“There aren’t specific treatments...but they’re going to...uh...uh...uh...”).
Patients often broke silent EHR use with small talk (“So, how is your family?”), or by introducing concerns (“Oh yea, what did the x-ray show about my shoulder?”).
Discussion
Clinicians mostly multitasked with EHRs. Transitions to silent EHR use could be ambiguous. Patients sometimes broke EHR silences for social and medical reasons.
Multitasking increases risk for errors,3 in EHR tasks and communication (e.g., missing patient concerns). Risks are affected by cognitive complexity of the information, EHR usability, documentation support and teamwork, and clinician-patient dynamics.3, 5 Certain EHR (e.g., prescribing high-risk medications) and communication tasks (e.g., depression assessment) may require focus.
Safety net patients could benefit from silence, since clinician talk typically dominates visits and imposes literacy burdens.6 However, clinicians must attend to emerging patient concerns and decide whether to address those concerns, defer them to complete EHR tasks safely, or attempt to complete both, despite multitasking risks.3
Limitations include sample size, single setting, timeframe after implementation, and lack of clinical outcomes. Study strengths are inclusion of a diverse provider and patient population.
Studies should explore strategies for negotiating multitasking and silent EHR use, engaging patients “actively” during silent EHR use, and ensuring clinicians detect emerging patient concerns.
Acknowledgments
Author Contributions: Dr. Ratanawongsa had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Ratanawongsa, Lyles, Koenig, Barton, Matta, Yu, Schillinger
Acquisition, analysis, or interpretation of data: Ratanawongsa, Lyles, Koenig, Barton, Matta, Yu, Schillinger
Drafting of the manuscript: Ratanawongsa, Matta, Schillinger
Critical revision of the manuscript for important intellectual content: Ratanawongsa, Lyles, Koenig, Barton, Matta, Yu, Schillinger
Statistical analysis: Ratanawongsa
Obtained funding: Ratanawongsa, Barton, Schillinger
Administrative, technical, or material support: Matta, Yu
Study supervision: Ratanawongsa, Schillinger
Conflict of Interest Disclosures: No disclosures were reported.
Funding/Support: Research reported in this publication was supported by AHRQ Grants 1K08HS022561, P30HS023558, and K99HS022408; National Institute of Arthritis and Musculoskeletal and Skin Diseases 1K23AR064372; and the National Center for Advancing Translational Sciences of the NIH under Award Number KL2TR000143. Dr. Schillinger is supported by the Health Delivery Systems Center for Diabetes Translational Research (CDTR) funded through NIDDK grant 1P30-DK092924. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of AHRQ or the NIH. Drs. Ratanawongsa and Barton were fellows supported by the Pfizer Medical Academic Partnership Fellowship in Health Literacy.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of AHRQ or the NIH.
Footnotes
Presentations: Preliminary data from this manuscript was presented at The Patient, the Practioner, and the Computer Conference, Providence, RI, March 18, 2017, and the Annual Meeting of the Society of General Internal Medicine, Washington, DC, April 20, 2017.
References
- 1.Sinsky C, Colligan L, Li L, et al. Allocation of Physician Time in Ambulatory Practice: A Time and Motion Study in 4 Specialties. Ann Intern Med. 2016;165(11):753–760. doi: 10.7326/M16-0961. Medline:27595430. [DOI] [PubMed] [Google Scholar]
- 2.Alkureishi MA, Lee WW, Lyons M, et al. Impact of Electronic Medical Record Use on the Patient-Doctor Relationship and Communication: A Systematic Review. J Gen Intern Med. 2016;31(5):548–560. doi: 10.1007/s11606-015-3582-1. Medline:26786877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Douglas HE, Raban MZ, Walter SR, Westbrook JI. Improving our understanding of multitasking in healthcare: Drawing together the cognitive psychology and healthcare literature. Appl Ergon. 2017;59(Pt A):45–55. doi: 10.1016/j.apergo.2016.08.021. [DOI] [PubMed] [Google Scholar]
- 4.Ratanawongsa N, Barton JL, Lyles CR, et al. Association Between Clinician Computer Use and Communication With Patients in Safety-Net Clinics. JAMA Intern Med. 2016;176(1):125–128. doi: 10.1001/jamainternmed.2015.6186. Medline:26619393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin SA, Sinsky CA. The map is not the territory: medical records and 21st century practice. Lancet. 2016 doi: 10.1016/S0140-6736(16)00338-X. [DOI] [PubMed] [Google Scholar]
- 6.Nouri SS, Rudd RE. Health literacy in the “oral exchange”: an important element of patient-provider communication. Patient Educ Couns. 2015;98(5):565–571. doi: 10.1016/j.pec.2014.12.002. Medline:25620074. [DOI] [PubMed] [Google Scholar]