To the Editor
Introduction
Asthma is the most common chronic disease in children, (1) with many modifiable risk factors impacting asthma morbidity, including adherence to medications. Despite research demonstrating the importance of adherence to asthma medication regimens, poor and variable adherence persists,(2) with patients receiving 30–70% of prescribed doses of inhaled corticosteroids.(3) Non-adherence may be especially prevalent in minorities and those of lower socioeconomic status, which may contribute to higher morbidity in these groups.(4)
High stress levels among asthmatic children and/or their caregivers may predict higher asthma morbidity, which has been demonstrated in inner-city children.(5) To our knowledge, the interaction between stress and adherence on asthma morbidity has not been examined. The aim of this study was to examine the impact of adherence and stress on asthma morbidity in a school inner-city population and to examine the interaction of stress and adherence on asthma outcomes.
Methods
The School Inner City Asthma Study (SICAS) was a prospective, school-based study, which evaluated the role of classroom/home exposures on asthma morbidity in school-aged students.(6) Institutional Review Board approval, subject assent, and caregiver consent were obtained prior to starting the study.
A survey including socio-demographic information and asthma symptoms was administered to caregivers. Children taking a daily controller medication were included in this analysis. Caregiver-reported adherence was measured at baseline with an un-validated 11-item survey that included questions related to adherence to asthma medications over the previous three months. A ‘non-adherence score’ was calculated with one point given for each positive response on the questionnaire. Caregiver psychosocial stress was assessed at baseline using the Perceived Stress Scale-4 (PSS-4), a validated 4-item questionnaire measuring how one’s life situations are perceived as stressful.(7) Using the PSS-4, caregiver stress was defined categorically as normal (within 1 standard deviation (SD) of mean), high (> 1-SD above mean), or very high (>2-SD above mean). A mean score of 4.49 and SD of 2.96 were used based on a previous validated report.(7)
The primary outcome of interest was asthma morbidity. Maximum symptom days were defined as the largest value among the following in the last 2 weeks: (1) number of days with asthma symptoms, (2) number of nights awakening due to asthma, or (3) number of days slowing down/discontinuing activities because of asthma. Additional outcomes were based on the participant’s symptoms in the last 4 weeks: dyspnea, night-time symptoms, decreased daytime activity, and rescue medication use. Poor asthma control was defined as shortness of breath greater than twice weekly, night-time awakenings due to asthma at least once, limitation in activity whereby the child’s asthma kept him/her from getting things done some, most, or all of the time, or use of rescue asthma medication ≥ twice weekly in the past 4 weeks.
Binomial family generalized estimating equations (GEEs) with a logit link, exchangeable correlation structure, robust variance estimates, and clustered at the participant level were used for all outcomes. An overdispersion parameter was used for maximum symptom days, as it was considered the sum of 14 binomial “successes” in a two-week period.
To investigate the role of stress in modifying the adherence-morbidity relationship, we first tested the interaction effect of adherence and stress level. If the interaction effect was p≥0.10, then the interaction effect was removed and the main effect of adherence was reported. We included potential confounders in all models if their association with adherence was p<0.10. Alpha was set at 0.05 for all other tests.
Results
A total of 194 children were included in the analysis (Table E1). Fifty-five percent of caregivers in the study population reported at least one issue with adherence (Table I). Nearly 25% of caregivers reported stopping a child’s prescription before it was complete because they felt their child was better. Other common barriers to adherence included difficulty following a child’s asthma medication schedule or concerns that the medicine is addictive or has harmful side effects.
Table I.
Caregiver Adherence Questionnaire – Frequency of Positive Responses
| Question | ‘Yes’ response (%) |
|---|---|
| 1. Many families have problems getting the medicines their child needs because the pharmacy does not have the medicine or it is hard to get to the pharmacy. In the past 3 months, have you had to skip some of your child’s medicine because of problems like these? | 9.3% |
| 2. Some families have problems getting their child’s asthma medicines because they do not have insurance and the medicines cost too much. In the past 3 months, have you had any problems trying to get your child his/her asthma medicine because of cost issues like these? | 5.7% |
| 3. In the past 3 months, have you ever run out of medicines for your child’s asthma and not had any when he/she had an asthma attack? | 11.3% |
| 4. Sometimes families have trouble giving asthma medicines because the child refuses to take the medicine. Sometimes it’s because the child is too busy playing or the medicine tastes bad or makes him/her feel funny. Have you had to skip a dose of medicine because of this problem? | 6.7% |
| 5. Asthma medication schedules can be hard to follow. When there are many medicines to keep track of, the schedule can be confusing. Do you feel that your child’s medication schedule is hard to follow? | 15.5% |
| 6. Some families do not give their child all the asthma medicine prescribed by the doctor because they feel that he/she could become addicted or that too much medicine is bad. Other times, it may be that the child or the adults in the home do not like the side effects. In the past 3 months, have you ever cut back on your child’s asthma medications because of these worries? | 15.5% |
| 7. There are times when people think the child is all better before finishing the prescription. Did you stop using the medicine because your child felt better? | 24.7% |
| 8. Some families feel that the asthma medications do not really work, Are there times you stopped giving your child the asthma medicines because you felt this way? | 4.1% |
| 9. Sometimes family or friends recommend using remedies such as teas, rubs, and herbs for asthma. Did you use these instead of your child’s regular asthma medication? | 3.6% |
| 10. Many people have problems making and keeping doctor’s appointments for their child’s asthma. Sometimes appointments are hard to get or people have to wait a long time. Sometimes it is hard to get to the office or they are not open at good times. In the past 3 months, have you missed any appointments or chosen not to make one because of these problems? | 7.7% |
| 11. Many people have problems making or keeping appointments because they cannot afford the cost of the appointment or because of problems with insurance. In the past 3 months, have you missed any appointments or chosen not to make one because of money or insurance problems? | 4.1% |
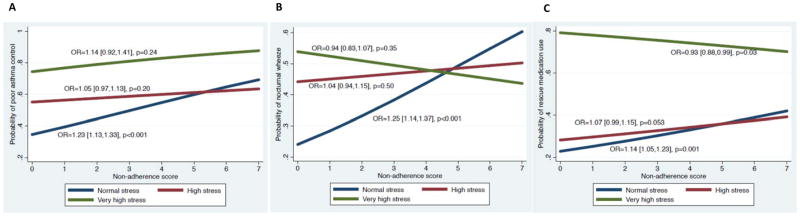
There was no association between stress and non-adherence (p=0.24). The association between a diagnosis of food allergy and non-adherence score was significant at p<0.10 and was therefore included in all subsequent models (p=0.08). There was a significant interaction effect between stress and non-adherence when predicting poor asthma control, nocturnal wheezing, and rescue medication use. At higher stress levels, the effect of poor adherence was less predictive of worse asthma morbidity (Figure 1).
Figure 1.
For the remaining outcomes there was no interaction between stress and adherence. When adjusting for stress and food allergy, the independent effect of worse adherence was associated with worse asthma morbidity for the following outcomes: increased maximum symptom days (odds ratio (OR) =1.18[1.05,1.33], p=0.005), dyspnea (OR=1.20[1.03,1.41], p=0.02), and poor asthma control (OR=1.33[1.14,1.56], p<0.001. When adjusting for adherence, the independent effects of stress were: those with very high caregiver stress had higher odds of reporting increased maximum symptom days and dyspnea compared to those with normal stress. Those with high and very high stress had higher odds of poor asthma control compared to those with normal stress (Table II).
Table II.
Relationship Between Stress and Asthma Morbidity*
| Odds Ratio** | 95% CI | P-value | ||
|---|---|---|---|---|
| Increased maximum symptoms days | High stress | OR= 0.91 | [0.65, 1.27] | P=0.578 |
| Very high stress | OR=2.79 | [1.59, 4.89] | P<0.001 | |
| Limited Activity | High stress | OR=1.44 | [0.79, 2.64]s | P=0.232 |
| Very high stress | OR=1.95 | [0.41, 9.3] | P=0.404 | |
| Dyspnea | High stress | OR= 0.95 | [0.54, 1.68] | P=0.87 |
| Very high stress | OR=5.62 | [2.61, 12.09] | P<0.001 | |
| Poor parent-reported asthma control | High stress | OR= 1.75 | [1.08, 2.85] | P=0.023 |
| Very high stress | OR=4.67 | [1.88, 11.63] | P=0.001 |
Adjusting for non-adherence and food allergy
Normal stress is the reference group
Discussion
In this school-based population of inner-city asthmatic children, higher non-adherence scores were associated with worse asthma morbidity, and those with very high caregiver stress had higher odds of asthma morbidity than those with normal stress. An unexpected finding in this study was that caregiver stress modified the relationship between adherence and asthma morbidity. Poor adherence had less influence on asthma morbidity on those children with high and very high caregiver stress levels, but was very important in those with normal caregiver stress levels. We suspect that adherence affects those with normal stress levels but not high stress levels, as those with high stress are already at higher risk for asthma morbidity. In our study, the effect of poor adherence at higher stress levels was negligible, as stress already conferred very high risk of asthma morbidity.
Further research is needed to understand how baseline caregiver stress level affects adherence in an at-risk population. This study adds support to the growing body of literature which highlights the importance of targeting factors associated with asthma morbidity, including medication adherence and caregiver stress, particularly in an inner-city population.
Sincerely,
Meredith. A. Dilley, MD, 1, 2
Carter R. Petty, MA 1
William. J. Sheehan, MD, 1, 2
Jonathan M. Gaffin, MD, MMSc 1, 2
Marissa Hauptman, MD, MPH 1, 2
Wanda Phipatanakul, MD, MS 1,2
1Boston Children’s Hospital, Boston, MA; 2 Harvard Medical School, Boston, MA
Supplementary Material
Acknowledgments
Financial Support: M.D. is funded by NIH grant T32HD0757270. W.S. is funded by K23AI104780. J.G. is funded by NIH K23AI106945. W.P. is funded by NIH grant K24AI106822. C.P. is supported by NIH grant U01 AI 110397.
Abbreviations
- SICAS
School Inner City Asthma Study
- PSS-4
4-item perceived stress scale
- SD
standard deviation
- OR
Odds Ratio
Footnotes
CLINICAL TRIAL REGISTRATION: NCT01756391
Conflict of Interest: None
References
- 1.Friedman B, Berdahl T, Simpson LA, et al. Annual report on health care for children and youth in the United States: focus on trends in hospital use and quality. Acad Pediatr. 2011;11:263–79. doi: 10.1016/j.acap.2011.04.002. [DOI] [PubMed] [Google Scholar]
- 2.Bender BG. Nonadherence to Asthma Treatment: Getting Unstuck. J Allergy Clin Immunol Pract. 2016;4:849–51. doi: 10.1016/j.jaip.2016.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Cochrane MG, Bala MV, Downs KE, Mauskopf J, Ben-Joseph RH. Inhaled corticosteroids for asthma therapy: patient compliance, devices, and inhalation technique. Chest. 2000;117:542–50. doi: 10.1378/chest.117.2.542. [DOI] [PubMed] [Google Scholar]
- 4.Smith LA, Bokhour B, Hohman KH, et al. Modifiable risk factors for suboptimal control and controller medication underuse among children with asthma. Pediatrics. 2008;122:760–9. doi: 10.1542/peds.2007-2750. [DOI] [PubMed] [Google Scholar]
- 5.Wade S, Weil C, Holden G, et al. Psychosocial characteristics of inner-city children with asthma: a description of the NCICAS psychosocial protocol. National Cooperative Inner-City Asthma Study. Pediatr Pulmonol. 1997;24:263–76. doi: 10.1002/(sici)1099-0496(199710)24:4<263::aid-ppul5>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 6.Phipatanakul W, Bailey A, Hoffman EB, et al. The school inner-city asthma study: design, methods, and lessons learned. J Asthma. 2011;48:1007–14. doi: 10.3109/02770903.2011.624235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cohen S, Williamson GM, editors. The Social Psychology of Health. Newbury Park, CA: Sage Publications; 1988. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.