ABSTRACT
The study objective was to examine precision in wound measurement using a recently Food and Drug Administration-approved Scout (WoundVision, LLC, Indianapolis, Indiana) device to measure wound length (L) and width (W). Wound perimeter and a ruler measurement of L and W were also made. Images of 40 actual patient wounds were measured using the Scout device. All 3 techniques (length, width, perimeter) demonstrated acceptable within and between reader precision; however, the best precision was in wound perimeter measurement.
KEYWORDS: wound measurement, measurement precision, measurement accuracy, wound image measurement
INTRODUCTION
Currently, the accepted standard for wound measurement is to use a hand ruler to measure wound size.1 Although there are several variations on the ruler method, a common practice is outlined by the National Pressure Ulcer Advisory Panel (NPUAP) on its website and in the NPUAP Pressure Ulcer Scale for Healing (PUSH) Tool version 3.0. The PUSH Tool is designed to document data on a complete pressure ulcer assessment, which is then tabulated for a total score. Clinicians can use the PUSH Tool to document healing or wound deterioration over time. The website and PUSH Tool instruct clinicians to measure the longest length of the wound head to toe and then the longest width of the wound, taking the width measurements perpendicular to the length measurement.1–3 This technique resulted in the least overestimation of wound area in a study by Langemo et al.4
The manual ruler method is quick and noninvasive, but the area measurements are almost always inaccurate as the length × width (L × W) technique assumes a square or rectangular wound shape. The deviation from the true area is dependent on multiple factors, including wound bed size and shape, which are easily distorted by body position. Studies have shown wound area calculations using the L × W ruler method can overestimate area by 44%,5 especially for wounds with irregular edges.4 Although highly inaccurate, the ruler method yields fairly reproducible results from measurement to measurement. Therefore, measurement of wound size over time provides a fairly reliable measure of change in wound status.6,7
Other devices on the market for measuring wound size include tracing wound edges directly on acetate and using digital photographs.6–8 Measuring wounds from digital photographs, although more complex to use bedside, has been shown to provide more accurate wound measurements than the ruler method.4
This study measured 40 patient wounds to demonstrate the performance of an instrument new to the market, called the Scout device, on actual wounds in the intended clinical population.
BACKGROUND INFORMATION
The Food and Drug Administration–approved Scout device (WoundVision, LLC, Indianapolis, Indiana), previously known as the Wound Measurement and Monitoring System, has 2 main components: the Scout ImageCapture and the Scout ImageReview software. The ImageCapture is a combination digital camera and long-wave infrared camera. The digital camera is indicated for the use of capturing visual images of a part of the body or 2 body surfaces. The long-wave infrared camera is indicated for the use of capturing thermal images. The ImageReview software allows for measurement of the diameter, surface area, and perimeter of wound images and the thermal intensity variation data of a part of the body or 2 body surfaces.
Intended for qualified healthcare personnel who are trained in its use, the Scout is a noncontact, noninvasive, nonradiating device. The Scout is considered safe to use (for both patient and user) for capturing both visual and thermal images.
This study was institutional review board-approved and was conducted in compliance with the protocol, good clinical practices, and all applicable regulatory requirements. All investigational staff members were trained on the protocol and the proper use of the Scout ImageReview. There was no anticipated benefit to the study subjects who participated in this study. However, the images collected may lead to the improved care in the future.
Design
A prospective design was used to retrospectively analyze collected images of actual patient wounds from 40 patient subjects from both an inpatient and an outpatient setting.
Study Objectives
The study objectives were to (1) compare the L × W ruler method and wound area calculation to the Scout L × W method and the perimeter trace method of visual wound area measurement and (2) to establish within and between reader agreement of the Scout L × W, Scout trace area, and Scout trace perimeter (measurements of trace area and perimeter).
Methods
Following institutional review board approval, 40 actual patient wounds were imaged at an inpatient and an outpatient clinical site in Indiana to represent feasibility of the Scout in both inpatient and outpatient clinical settings. The 40 patient wounds were of various etiologies, representing those commonly seen on an inpatient and outpatient basis (eg, venous, neuropathic, arterial, and pressure ulcers). This study used both experts in clinical wound care (n = 3) and nonexpert readers (n = 2). The 5 study readers included a physician, a registered nurse, a licensed practical nurse, and 2 readers familiar with the device but not experts in clinical wound assessment. The expert readers were clinicians trained in wound care and in the appropriate use of the Scout system. Previous study data of the researchers, as well as other peer-reviewed literature,9 suggest that variation in qualitative wound characteristics (wound edge) exists not only between readers of different experience levels and training, but also between readers of similar specialized training and experience.
Multiple clinicians measuring wounds in a clinical setting with a ruler multiple times was a patient safety concern from the standpoint of potential wound bed contamination, as well as patient comfort. Therefore, only the Scout device measurements had replicate measurements completed. During the conduct of this study, 5 readers made 3 replicate measures for each of the Scout measurements, Scout L × W, and Trace, for each image. Therefore, 3 replicate measurements are available for each reader for the Scout L × W area, Scout trace area, and Scout trace perimeter.
Scout Measurements
The readers were trained on the operation of the Scout prior to completing these measurements. Then, each reader completed the Scout L × W and External Wound Trace for each image 3 times.
The Scout L × W is designed to emulate the reference standard ruler technique by taking the greatest length head to toe by greatest width at a 90-degree angle to length. The head orientation was indicated at the time of image capture. When measuring the image, the reader placed the cursor at the head or toe wound edge and drew to the opposing wound edge. The width of the wound was then drawn. The readers were able to use the compass feature of Scout ImageReview to ensure alignment with head orientation relative to each wound.
The External Wound Trace utilizes software to allow the user to visually trace the wound edge. The software then calculates trace area and trace perimeter. Both the Scout L × W and External Wound Trace were completed on the same image.
Wounds were selected from the library of images that met the study criteria. Individual written consent was provided for each wound from each adult 18 years or older. Wounds were excluded if the edges were obscured in any way, if the image was blurred, and if images were not at 18-inch distance or not at 90 degrees perpendicular to the external wound. All 40 wounds selected were evaluated for performance on the study device.
To control for carryover, the 40 wound images were randomized. Each reader measured the L × W area, trace area, and trace perimeter for the first set of 40 wound images 1 time. They were then provided with a second set of randomized 40 wound images, where they performed the second set of measurements. This process was repeated for the third set of measurements. A separate randomization was completed for each of the 3 replicates. The same randomization was used for each of the 5 readers.
End Points
The primary end points for this study were (1) length measure of the wound using the Scout ImageReview software, (2) width measure of the wound using the Scout ImageReview software, (3) calculated square area of the wound using L × W measure of the Scout ImageReview software, (4) surface area of the wound using the External Wound Trace feature, and (5) perimeter of the wound using the External Wound Trace feature.
Data Analysis
Data were handled according to the WoundVision, LLC data management procedures. Descriptive statistics included the mean, median, maximum, and minimum for the Scout L × W area and perimeter trace area. Measurements of precision included intrareader and interreader reliability (repeatability), as well as total variability. The CV% was calculated as the SD divided by the mean times 100 for within and between readers for each individual wound for the repeatability (reliability) measure. An analysis of variance was completed using a random-effects model with reader and wound in the model as random factors for each measurement method. In addition, the model was rerun including the interaction term as a random factor. The within- and between-reader precision was recalculated separately for the 2 groups of readers, the 3 clinical experts, and the 2 nonexperts. SAS software (SAS Institute, Cary, North Carolina) was utilized for statistical analysis.
RESULTS
Objective 1 could not be completed because repeat measurements with the standard of care ruler were impractical. All of the results in this section address objective 2.
Data from all 40 wound images for each of the 5 readers, with measurements (Scout L × W area and Scout trace area) for each end point completed 3 times per 40 wounds were utilized in analyses. Descriptive statistics are as follows: the average area for the Scout L × W calculation was 20.07 (SD, 1.51) cm2 (95% confidence interval, 19.23-20.91 cm2), and the Scout trace area was 16.28 (SD, 1.17) cm2 (95% confidence interval, 19.23-20.91 cm2).
Within-Reader Accuracy
The within-reader precision was calculated for each individual wound and averaged across the 5 readers for each of the Scout measurement methodologies (Figure 1). The average CV% across all 40 wounds was less than 10% for each of the measurement methodologies, with the CV% lowest for the Scout trace perimeter. This suggests that regardless of the measurement used a reader can perform multiple measurements of the same wound with acceptable variation.
Figure 1.
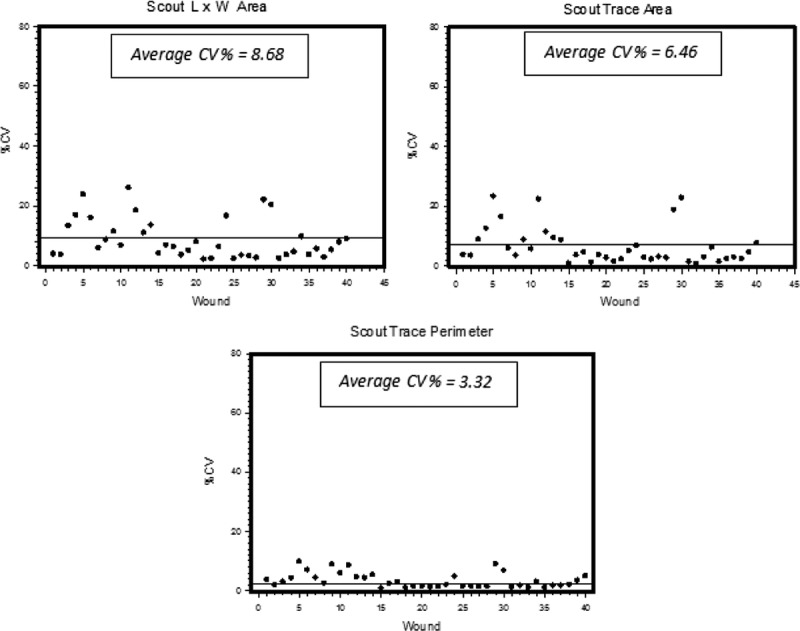
INTENDED USE POPULATION: WITHIN READER CV%: 5 REVIEWERS
The CV% for each of the 40 wound images for each of the Scout measurement methodologies. Each dot is the within reader CV% for each wound. The line is the average CV% across all 40 wounds for each methodology. Scout L x W area average CV% = 8.68; Scout trace area average CV% = 6.46, and Scout trace perimeter average CV% = 3.32.
Interrater Reliability
The between-reader precision for each individual wound for each of the Scout measurement methodologies was on average less than 20% CV. Similar to both the within-reader precision and that from a previous study,10 the average CV% is smallest for the perimeter measurements (Figure 2).
Figure 2.
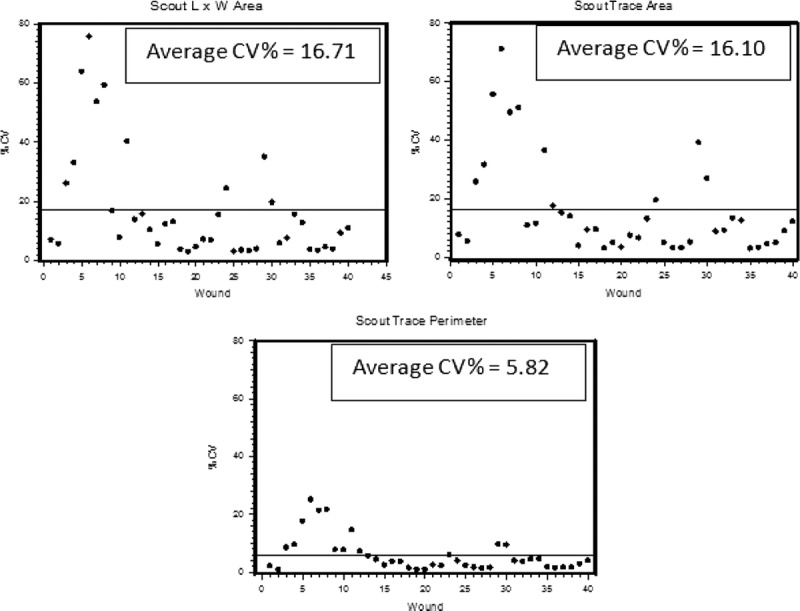
INTENDED USE STUDY BETWEEN READER CV% 5 READERS’ AVERAGE
Between-reader CV% for each of the Scout measurements. Each dot is the within reader CV% for each wound. The line is the average CV% across all 40 wounds for each methodology. Scout L × W area average CV% = 16.71; Scout trace area average CV% = 16.10, and Scout trace perimeter average CV% = 5.82.
Data from a previous study10 and other literature4 suggest that when measuring shapes of known size with a defined edge the between-reader agreement shows acceptable variation regardless of measurement technique. The results of this study using actual wounds suggest that regardless of the measurement used, readers differ in how they define the wound’s border.4,11 The source of this variation may lie within the subjective perception of qualitative wound characteristics.9 Therefore, from the previous study measuring shapes of known size,10 in this study measuring actual wounds, as well as the literature, it can be concluded that the differences that exist between readers in wound measurement are not necessarily due to the measurement technique, but rather the judgment of the reader performing the measurement.11
Analysis by Reader Type
This study used both experts in clinical wound care (n = 3) and nonexpert readers (n = 2). The within- and between-reader precision for each of the reader types yields similar results (Figure 3). These results support that the Scout device can be utilized by a variety of individuals in the clinical setting yielding similar results.
Figure 3.
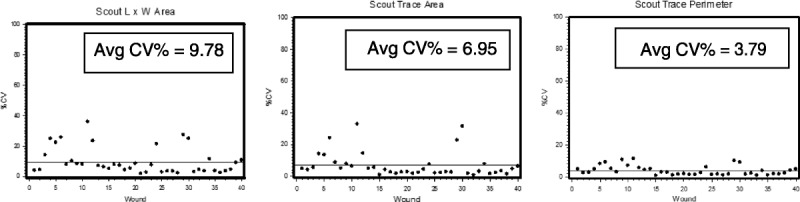
WITHIN-READER CV% CLINICIAN AVERAGE
The within-reader CV% for each of the 40 wound images for each of the Scout measurement methodologies. Each dot is the within-reader CV% for each wound. The line is the average CV% across all 40 wounds for each methodology. Scout L x W area average CV% = 9.78; Scout trace area average CV% = 6.95, and Scout trace perimeter average CV% = 3.79. The 3 readers in this analysis are all clinicians with expertise in wound care.
SUMMARY
Study data suggest that a single reader can measure the same wound multiple times yielding similar results. And as expected, multiple readers do not measure the same wound as well as a single reader. The variation that exists between readers in wound measurement is not necessarily due to the measurement technique but rather the judgment of the reader in determining the wound edges performing the measurement.4,11
The within- and between-reader precision is similar for the Scout trace area (within 6.46 CV% and between 16.10 CV%) and the Scout L × W (within 8.68 CV% and between 16.71 CV%). Perimeter measurement is more precise than both traced area and Scout L × W (within 3.32 CV% and between 5.82 CV%). For all measurements, the within-reader precision is better than the between-reader. For the Scout L × W area, within-reader precision was 8.68 CV% and between 16.71 CV%. For the traced area, within-reader precision was 6.46 CV% and between 16.10 CV%; and for the perimeter, the within-reader precision was 3.32 CV% and between 5.82 CV%.
On analysis of variance when the interaction term was included, there was a significant interaction between wound and reader. However, the wound data are not normally distributed and the within- and between-reader precision is not similar across all wound shapes; therefore, the results of the analysis of variance are not valid.
CONCLUSIONS
The within-reader precision was acceptable (CV% <10) for all 3 measurements (Scout trace perimeter 3.32 CV%, Scout trace area 6.46 CV%, Scout L × W area 8.68 CV%). Although the between-reader variability was larger than the within-reader variability, it still averaged less than 20% for all measurements (perimeter 5.82 CV%, traced surface area 16.10 CV%, and Scout L × W area 16.71 CV%), making it an acceptable technique. This finding suggests that the differences in subjective perception of qualitative wound characteristics, particularly wound edge, can influence wound assessment agreement, consistent with previous literature.9 The within-reader results using actual wounds in this study are consistent with a previous study on simulated wounds (CV% 3.32–6.68 vs CV% 2.33–5.39, respectively),10 demonstrating reliable results from the Scout device in the clinical setting for repeat measurements by the same reader.
Using actual wounds in this study, the between-reader results were greater than those on simulated wounds (CV% 5.82–16.71 vs CV% 2.75–6.47, respectively) in a previous study.10 The study of Langemo et al10 used metal objects, obviously enabling a cleaner determination of wound shape or wound edge compared with actual wounds (Table). This finding is consistent with previous research demonstrating that between-reader differences exist less unrelated to measurement technique and more related to the reader judgment of wound edge.4,11
Table.
BETWEEN AND WITHIN COMPARISONS FOR 3 TECHNIQUES ON WOUND SHAPES VERSUS ACTUAL WOUND IMAGES
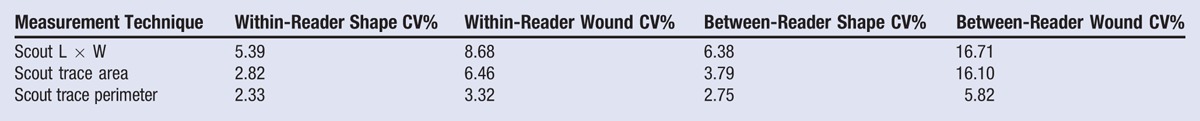
The Scout device provides accurate and reliable measurements of actual wounds.10 It is most accurate in measuring wound perimeter, even between readers. The current standard of measuring wounds is the L × W area calculation, which is known to have large variability, in fact up to 44%.4,5,12 The Scout device can be used by individuals with varied backgrounds and provides similar results when clinical experts and nonclinicians utilize the device.
The Scout device is able to accurately measure wound perimeter, which is a reliable measurement of wound area (Table). As wounds heal from the bottom up followed by the edges inward, it is a good measure of serial reporting for indications of healing.13 The device is noncontact; therefore, patient comfort is a nonissue. The Scout device showed 3% variability in the wound shape study,10 whereas it was only 5% in actual wounds in this current study. The Scout device is reliable in measuring small as well as large wounds.
Techniques for wound measurement that are most desirable are those that are accurate, safe for patients, and easy to learn and use clinically. The technique must also be valid and reliable and sensitive enough to document change over time for clinical as well as research purposes.4,14 The noncontact, Food and Drug Administration–approved Scout device meets all these requirements. Although the Scout device is more expensive than a paper ruler, it is far more accurate in documenting progress toward improvement or deterioration of a wound.
REFERENCES
- 1.National Pressure Ulcer Advisory Panel. PUSH Tool Version 3.0 (9/15/98). http://www.npuap.org/resources/educational-and-clinical-resources/push-tool/push-tool. Last accessed January 14, 2015.
- 2.National Quality Forum. National Voluntary Consensus Standards for Developing a Framework for Measuring Quality for Prevention and Management of Pressure Ulcers. Washington, DC: National Quality Forum, 2011. http://www.qualityforum.org/Publications/2011/12/National_Voluntary_Consensus_Standards_for_Developing_a_Framework_for_Measuring_Quality_for_Prevention_and_Management_of_Pressure_Ulcers.aspx. [Google Scholar]
- 3. Reger S, Langemo D, Taler G. NPUAP best practice recommendation on pressure ulcer measurement. NPUAP 2008. http://www.npuap.org/wp-content/uploads/2012/05/Fall07.pdf. [Google Scholar]
- 4. Langemo D, Melland H, Hanson D, Olson B, Hunter S, Henly S. Two-dimensional wound measurement: comparison of 4 techniques. Adv Wound Care 1998; 11: 337- 43. [PubMed] [Google Scholar]
- 5. Keast DH, Bowering CK, Evans AW, Mackean GL, Burrows C, D’Souza L. MEASURE: A proposed assessment framework for developing best practice recommendations for wound assessment. Wound Repair Regen 2004; 12: S1– 17. [DOI] [PubMed] [Google Scholar]
- 6. Gethin G. The importance of continuous wound measuring. Wounds UK 2006; 2 (2): 60- 8. [Google Scholar]
- 7. Chang A, Dearman B, Greenwood J. A comparison of wound measurement techniques: Visitrak versus photography. ePlasty 2011; 11: e18. [PMC free article] [PubMed] [Google Scholar]
- 8. Thawer H, Houghton P, Woodbury G, Keast D, Campbell K. A comparison of computer-assisted and manual wound size measurement. Ostomy Wound Manage 2002; 48 (10): 46- 53. [PubMed] [Google Scholar]
- 9. Terris D, Woo C, Jarczok MN, Ho CH. Comparison of in-person and digital photograph assessment of stage III and IV pressure ulcers among veterans with spinal cord injuries. J Rehab Res Dev 2011; 48: 215- 44. [DOI] [PubMed] [Google Scholar]
- 10. Langemo D, Spahn JG, Snodgrass L. Accuracy and reproducibility of the wound shape measuring and monitoring system. Adv Skin Wound Care 2015. In press. [DOI] [PubMed] [Google Scholar]
- 11. Nemeth M, Sprigle S, Gajjala A. Clinical usability of a wound measurement device. Shepherd Center, Georgia Institute of Technology, Atlanta, GA: www.woundzoom.com/docs/Clinical_Usability.pdf. Last accessed January 5, 2014. [Google Scholar]
- 12. Griffin JW, Tolley EA, Tooms RE, Reyes RA, Clifft JK. A comparison of photographic and transparency-based methods for measuring wound surface area. Phys Ther 1993; 73: 117- 22. [DOI] [PubMed] [Google Scholar]
- 13. Gilman T. Wound Outcomes: The Utility of surface measures. Int J Low Extrem Wounds 2004; 3: 125- 32. [DOI] [PubMed] [Google Scholar]
- 14. Ferrell BA, Artinian BM, Sessing D. The Sessing Scale for assessment of pressure ulcer healing. J Am Geriatr Soc 1995; 43: 37- 40. [DOI] [PubMed] [Google Scholar]


