Abstract
Fusobacterium nucleatum (Fn) is an important tumour-associated bacterium in colorectal cancer (CRC). The antioxidant protein alkyl hydroperoxide reductase subunit C (AhpC) can induce strong antibacterial immune response during various pathogen infections. Our study aimed to evaluate the efficacy of Fn-AhpC as a candidate vaccine. In this work, by western blot analysis, we showed that Fn-AhpC recombinant protein could be recognized specifically by antibodies present in the sera of CRC patients; using the mouse Fn-infection model, we observed that systemic prophylactic immunization with AhpC/alum conferred significant protection against infection in 77.3% of mice. In addition, we measured the anti-AhpC antibody level in the sera of CRC patients and found that there was no obvious increase of anti-AhpC antibodies in the early-stage CRC group. Furthermore, we treated Fn with the sera from both immunized mice and CRC patients and found that sera with high anti-AhpC antibodies titre could inhibit Fn growth. In conclusion, our findings support the use of AhpC as a potential vaccine candidate against inhabitation or infection of Fn in the intestinal tract, which could provide a practical strategy for the prevention of CRC associated with Fn infection.
Introduction
The gram-negative anaerobe Fusobacterium nucleatum (Fn) is an important tumour-associated bacterium that promotes colorectal tumour growth and inhibits T cell-mediated immune responses against colorectal tumours1, 2. A number of studies have identified the increased carriage of Fn in tumour tissues and faecal samples of colorectal cancer (CRC) patients3, 4 and demonstrated an association of Fn overabundance with shorter survival rates of CRC patients5. Faecal Fn infection has been identified as an important diagnostic marker for CRC6, 7. Previously, Fn was considered a key aetiological agent in human periodontal disease8–10 that plays important roles in different infectious processes, including juvenile idiopathic arthritis, rheumatoid arthritis and Alzheimer’s disease11–13. Recently, accumulating evidence has shown a high correlation between Fn infection and gastrointestinal tumours, and novel strategies on cancer prevention and treatment by targeting Fn have been proposed2, 14.
Previous studies have shown that Fn induced a significant humoural immune response in chronic oral infection12, 15. In a recent study, we showed that Fn infection elicited high-level serum antibody to Fn in CRC patients16. Using the sera from CRC patients to probe the bacteria protein extract, we identified a strong reactive antigen, alkyl hydroperoxide reductase subunit C (AhpC), which triggers the anti-Fn immune response16. The AhpC protein is a member of the highly conserved family of peroxiredoxins that catalyse the reduction of hydroperoxides for protection against oxygen radical damage17. AhpC is present in most bacterial species, which is particularly important for the role of protecting cells against organic peroxides in obligate anaerobes by eliminating hydroperoxides. AhpC has been identified as a potent immunoantigen that induces strong T cell-mediated responses in patients with acute melioidosis18. Recently, the antioxidant protein AhpC was considered a potential vaccine candidate against various bacterial infections, including Helicobacter pylori, Bacillus anthracis, Streptococcus zooepidemicus, Salmonella typhimurium and Burkholderia pseudomallei 18–22.
In the present study, we developed a recombinant AhpC vaccine and examined the protective efficacy against Fn overload in the murine intestinal tract. We further evaluated the prevalence of serum antibodies to Fn-AhpC in CRC patients and investigated the role of anti-Fn-AhpC antibodies against Fn in vitro.
Results
Identification of AhpC as vaccine candidate antigen for F. nucleatum
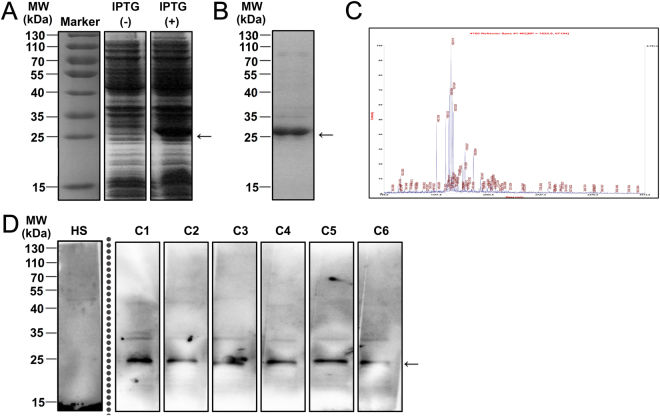
To identify anti-Fn vaccine candidates, we measured the pooled sera from 6 Fn-positive CRC patients using western blotting to probe the bacterial protein, as previously described16. We observed that AhpC protein induced a much stronger immune response than FomA protein, although a lower level of AhpC was presented in the total protein of Fn compared to FomA16. Next, we constructed a prokaryotic expression plasmid pET28a-AhpC to prepare recombinant Fn-AhpC protein. The overexpressed AhpC-His fusion proteins were detected at approximately 25 kDa (Fig. 1A). After IPTG induction, the soluble AhpC was purified using a Ni-NTA agarose column and was validated using a MALDI-TOF/TOF analyser (Fig. 1B,C). The purified Fn-AhpC reacted strongly with the pooled sera from CRC patients, whereas no immunoreactivity was detected in the sera from healthy subjects, indicating the antibodies present in the sera of CRC patients specifically recognized the Fn-AhpC proteins (Fig. 1D).
Figure 1.
Preparation of recombinant F. nucleatum-AhpC and identification of its immunogenic role in CRC patients. (A) Expression of recombinant Fn-AhpC after IPTG induction. The PCR amplified AhpC-DNA was inserted into pET28a vector before transformed into E. Coli BL21 strain. The expression of recombinant AhpC in the absence (−) or presence (+) of 0.5 mM IPTG was detected using 12% SDS-PAGE and Coomassie brilliant blue staining. (B) Purification of recombinant AhpC. The recombinant AhpC with a His tag was purified using a Ni-NTA column. (C) Identification of recombinant AhpC. The recombinant AhpC proteins were extracted from the gels stained with Coomassie brilliant blue R250, and subsequently digested with trypsin. The resulting peptides were further analysed using a MALDI-TOF/TOF analyser. (D) Antigens reactive with anti-AhpC-IgA were determined using western blotting. Recombinant AhpC were incubated with a reference dilution of pooled serum from 6 healthy subjects or separated serum from 6 Fn-positive CRC individuals as primary antibody. Notably, Fig. 1A,B and D were cropped from a single image on the dashed or solid lines to be better presented in the article’s context. The complete figures for Fig. 1A,B and D are provided in Supplementary Fig. 1A, Supplementary Fig. 1B and Supplementary Fig. 2, respectively.
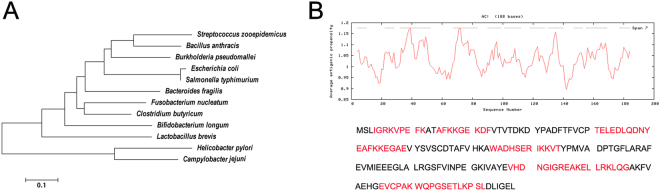
Furthermore, we constructed a phylogenetic tree based on the alignment of AhpC amino acid sequences, and the results showed an evolutionary relationship between Fn and other species (Fig. 2A). BLASTP analysis revealed that Fn-AhpC exhibited a low level of sequence identity with the human AhpC protein (31%). In addition, Fn-AhpC showed low identity with H. pylori (34.6%) and Campylobacter jejuni (37.2%), and moderate identity with S. zooepidemicus (56%), B. anthracis (59%), S. typhimurium (59%) and B. pseudomallei (61.7%). Antigenic peptide prediction suggested that Fn-AhpC possessed multiple cell antigenic determinants, indicating that Fn-AhpC had the capacity to induce an intense immune response (Fig. 2B).
Figure 2.
Phylogenetic tree analysis and antigenic determinants prediction for AhpC of F. nucleatum. (A) Phylogenetic tree of AhpC amino acid sequences. The amino acid sequences of AhpC present in protein database of GenBank were analysed using MEGA version 5.1 (www.megasoftware.net). The numbers at each branch represent the bootstrap values obtained with 1000 replicates. (B) The improved self-optimized software (DNAStar Protean system) was used to predict the antigenic plot for Fn-AhpC protein. Average antigenic propensity for this protein is 1.0330.
Interestingly, although Fn-AhpC also shared moderate amino acid identity with intestinal commensal bacteria, such as Lactobacillus brevis (53%), Bifidobacterium longum (58%), Escherichia coli (59%), Bacteroides fragilis (61%), and Clostridium butyricum (68%) (Fig. 2A), the potential antigenic determinants in AhpC differed among these microorganisms (Supplementary Table 1), suggesting that the AhpC protein of F. nucleatum induces few immune cross-reactions with these commensal bacteria (Fig. 2B). However, further studies are required to empirically demonstrate this finding. The results also showed that Fn-AhpC is a potential candidate antigen to develop the vaccine or diagnostic reagent against Fn.
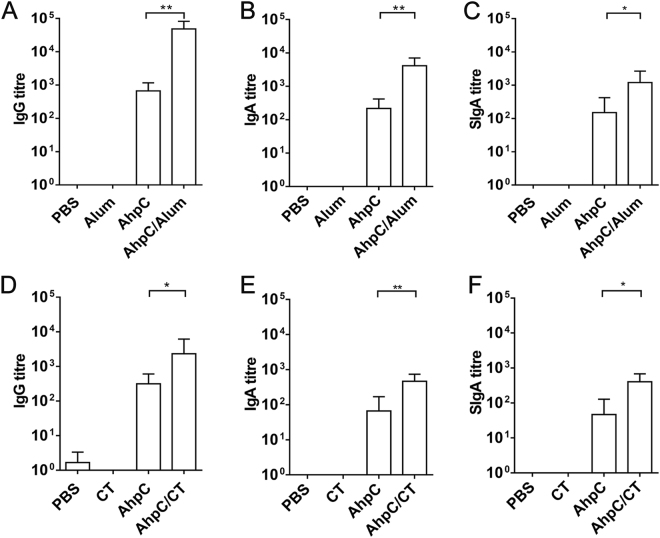
Protective efficacy of AhpC antigen against F. nucleatum challenge
To investigate whether Fn-AhpC could induce strong systemic or mucosal responses, the mice were treated with recombinant Fn-AhpC (100 μg) with or without adjuvant/cholera toxin by intraperitoneal (i.p.) injection or intragastric (i.g.) administration, respectively (Table 1). Mice treated similarly with either adjuvant or PBS alone served as control groups. As shown in Fig. 3A–F, all mice immunized with Fn-AhpC elicited specific anti-Fn-AhpC antibodies, while mice solely immunized with PBS or adjuvant rarely showed any induction of an immune response. In addition, immunization with AhpC/alum by i.p. injection enhanced a stronger immune response to AhpC antigen and showed significantly higher serum IgG, IgA and intestinal mucus SIgA antibodies compared to those immunized with AhpC alone (Fig. 3A–C). Consistently, we detected higher titres of serum IgG, IgA and SIgA antibodies in mucosal immunization with AhpC/cholera toxin compared to immunization with AhpC alone (Fig. 3D–F). Notably, the titres of serum antibodies in the i.p. injection groups were markedly higher than those in the i.g. administration groups, indicating that mucosal immunization with Fn-AhpC elicited lower levels of antibodies compared with systemic immunization.
Table 1.
Study time frames for the systemic and mucosal immunization studies.
| Route | Immunization (week) | Challenge (week) | Adjuvant | n | |
|---|---|---|---|---|---|
| Systemic | Intraperitoneal injection (i.p.) | 1, 3, 5 | ×3 doses (5) | Alum | 10 |
| Mucosal | Intragastric (i.g.) | 1, 3, 5 | ×3 doses (5) | Cholera toxin | 10 |
Figure 3.
Quantitative antibody response to F. nucleatum-AhpC immunization. Mice were immunized by intraperitoneal injection (systemic immunization) (A,B,C) or by intragastric administration (mucosal immunization) (D,E,F) with PBS, adjuvant, Fn-AhpC or Fn-AhpC combined with alum or cholera toxin (CT). One week after final vaccination, anti-AhpC IgG and IgA titres in sera/intestinal mucus were determined using ELISA. *P < 0.05, **P < 0.01.
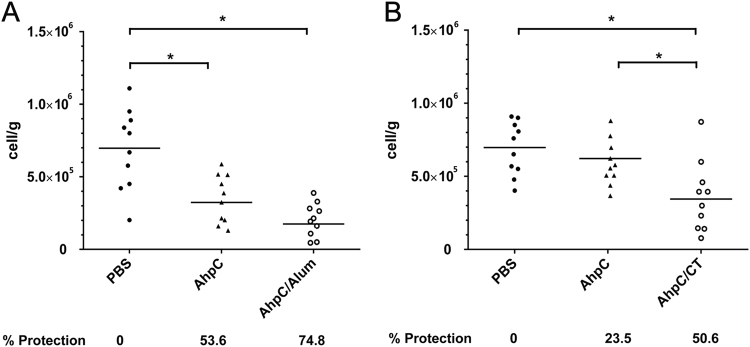
Furthermore, the mice were challenged with live Fn by daily oral gavage, and the protective efficacy was determined according to the load levels of Fn within mice intestine tissues using qPCR. The results showed that 74.8% of mice immunized by i.p. injection with AhpC/alum obtained significant protection from infection with Fn, whereas only 53.6% of mice immunized with AhpC alone obtained protection against Fn infection (Fig. 4A). However, immunization by i.g. administration showed a lower efficacy in protecting from infection compared to immunization by i.p. injection. Approximately 50.6% of immunized animals were protected from infection after challenge with Fn in the AhpC/cholera toxin group, while only 23.5% of immunized animals were protected in the AhpC group (Fig. 4B). This finding indicated that i.p. injection elicited a more efficacious effect in inhibiting the intestinal colonization of Fn compared with the i.g. administration of AhpC/cholera toxin. These results demonstrated that systemic immunization with Fn-AhpC conferred stronger protection than mucosal immunization. The systemic immunization of Fn-AhpC/alum exhibited the most significant reduction in bacterial load, suggesting that the Fn-AhpC vaccine might have the potential to decrease Fn colonization in the digestive tract.
Figure 4.
Induction of significant protection against F. nucleatum by immunization with F. nucleatum-AhpC vaccine. Mice were immunized by intraperitoneal injection (A) or intragastric administration (B) with PBS, AhpC or AhpC combined with alum or cholera toxin (CT). One week after the final vaccination, the mice were challenged with F. nucleatum and colonization quantified using qPCR assay. *P < 0.05, **P < 0.01.
Serological survey of antibodies against F. nucleatum-AhpC in CRC patients
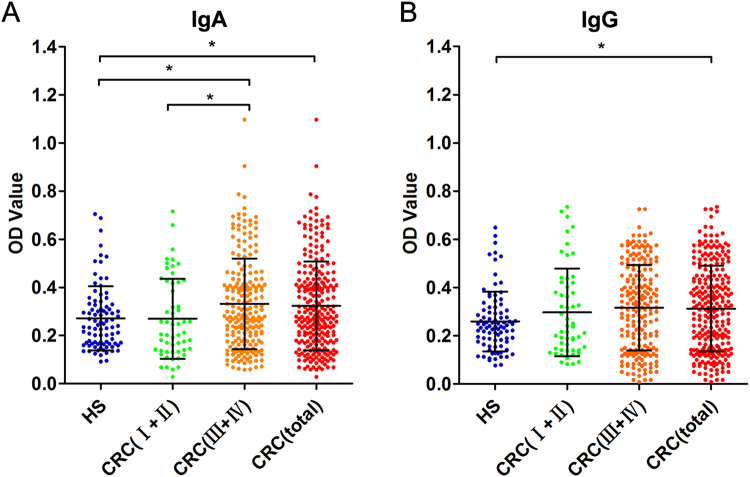
To further analyse the anti-Fn-AhpC antibody levels in CRC patients, sera samples from CRC patients (n = 258) and healthy subjects (n = 92) were detected using indirect ELISA. The purified Fn-AhpC was coated as an antigen, while the diluted sera of patients and controls served as primary antibodies. The average absorbance for anti-Fn-AhpC IgA in the CRC group exhibited a significantly higher level than observed in healthy subjects (P = 0.018, P < 0.05) (Fig. 5A). The serum IgA levels of anti-Fn-AhpC in patients with late-stage CRC (stage III-IV, n = 203) were remarkably higher than those in healthy subjects (P = 0.007, P < 0.05) and in early-stage CRC patients (P = 0.026, P < 0.05). There was no significant difference between early-stage CRC patients (stage I-II, n = 55) and healthy subjects. However, a significantly higher level of anti-AhpC IgG was detected in all CRC groups compared to the healthy group (P = 0.001, P < 0.05). No significant difference was observed between early-stage and advanced CRC groups (Fig. 5B).
Figure 5.
Comparison of serum levels of anti-F. nucleatum-AhpC from CRC patients and healthy subjects. Healthy subjects (HS, n = 92), stage I-II of CRC (n = 55), stage III-IV of CRC (n = 203), the total of CRC patients (n = 258) were individually assayed. Symbols indicate individual OD value; horizontal lines indicate the mean values ± SD. Differences between the four groups were analysed using the Kruskal-Wallis test. *P < 0.05. (A) anti-Fn-AhpC-IgA. (B) anti-Fn-AhpC-IgG.
The associations between levels of anti-Fn-AhpC and clinicopathological parameters are presented in Supplementary Table 2. Neither anti-Fn-AhpC IgA nor IgG showed an obvious correlation with age, gender, tumour volume, histological differentiation, T classification, N classification, metastasis and tumour marker CEA or CA19–9. However, a significant association between the presence of anti-Fn-AhpC IgA and clinical stage (P = 0.026) was observed. Pearson’s correlation coefficient and linear regression analysis were applied to analyse the correlation between the levels of antibodies to Fn whole-cell and AhpC antigen. The levels of IgA antibody to AhpC were positively correlated with IgA antibody to Fn whole-cell (R = 0.149, P = 0.002), but the levels of anti-AhpC-IgG were not correlated with IgG to Fn whole-cell. (Supplementary Fig. 3). These results showed that the elevated antibody levels to Fn-AhpC only presented in late-stage CRC groups, suggesting that patients with early-stage CRC might lack the anti-Fn-AhpC antibody against Fn-AhpC.
Antibodies of AhpC inhibited growth of F. nucleatum in vitro
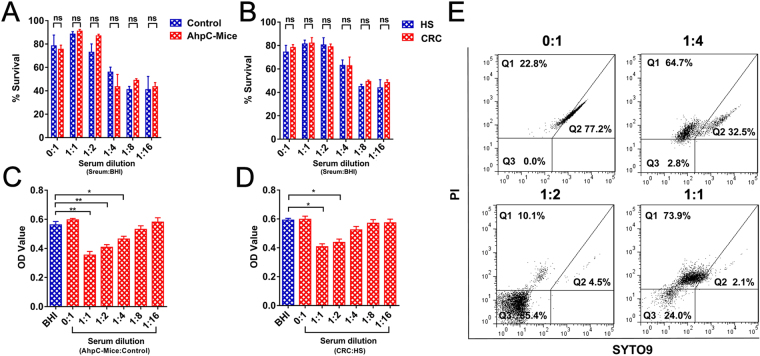
To investigate the bactericidal effect of anti-AhpC antibodies, Fn was incubated with pooled serum from mice immunized with AhpC at 37 °C for 30 min, and the serum from unimmunized mice was used as a control. The pooled serum was diluted 1:1 to 1:16, and there was no significant difference in survival between incubation with serum from immunized and unimmunized mice (Fig. 6A). However, media containing higher serum concentrations (>25%) improved the survival rate of Fn compared to media without serum. A similar result was observed for the Fn bacteria incubated with serum from healthy subjects compared to CRC patients with high titres of anti-AhpC antibodies (Fig. 6B).
Figure 6.
Serum with high titre antibodies to AhpC inhibited Fn growth in vitro. Survival of F. nucleatum strains was measured by bactericidal assays in serum of AhpC immunized and unimmunized mice (A) or CRC patients and healthy subjects (B). Inhibition of F. nucleatum strains was measured using antibacterial assays in the serum of AhpC immunized and unimmunized mice (C) or CRC patients and healthy subjects (D). Flow cytometric analysis of the stained Fn (E). Gates indicate the position and concentration of intact cells on the plots. Q1: dead cells, Q2: live cells; Q3: injured cells and debris. *P < 0.05, **P < 0.01, ns: no significant.
Additionally, serum from immunized mice or CRC patients was two-fold serial diluted with serum from unimmunized mice or healthy individuals, respectively. Subsequently, Fn was cultured with 25% of the above pooled serum from mice for 48 h. The results showed that Fn cultured with immunized serum significantly inhibited Fn growth in a titre-dependent manner, while Fn cultured with serum from unimmunized mice did not show any growth inhibition (Fig. 6C). Furthermore, Fn was cultured in 25% pooled serum from CRC patients and healthy individuals for 48 h. These results showed that Fn growth was significantly inhibited when treated with sera from CRC patients with a high titre of anti-AhpC IgG and IgA, while Fn growth in sera from healthy subjects was not inhibited (Fig. 6D). The viability of Fn bacteria was further detected by flow cytometric analysis. The percentage of live Fn sharply decreased when treated with low anti-AhpC titre serum (1:4 dilution) (77% vs. 32.5%), and almost no bacteria survived (2.1%) when treated with high titre serum (1:1 dilution) (Fig. 6E). These results showed that antibodies to AhpC could inhibit Fn growth as an antibody-based AhpC inhibitor rather than playing a bactericidal role.
Discussion
Emerging studies have demonstrated that Fn infection could drive strong immune responses12, 13, 15, 23, 24. Mice immunized with ultraviolet-inactivated Fn effectively minimized the progression of chronic halitosis associated with abscesses25. However, the whole-cell vaccine approach, including inactivated pathogens or live attenuated mutants, remains infeasible, reflecting the carcinogenicity of Fn. Thus, the development of safe subunit vaccines is a promising strategy to eliminate or eradicate Fn infection.
In the present study, we detected two candidate antigens, FomA and AhpC. Vaccination targeting FomA has previously been explored against bacterial biofilm formation and was found to be associated with pathogenicities, such as periodontal infection and halitosis26, 27. Oral administration of recombinant FomA-expressing Lactobacillus acidophilus was demonstrated to reduce the risk of periodontal infection28. Although FomA conferred a protective effect against bacterial co-aggregation with Porphyromonas gingivalis, recent studies have identified a mechanism involving the overabundance of Fn in tumourigenesis and metastasis26, 27. Thus, it is important to develop a new target as tumour vaccine to reduce the Fn load.
Oxidative stress is associated with malignant transformation29. In several intracellular bacterial pathogens, the antioxidant protein AhpC is unregulated as part of the response to host stress. H. pylori-AhpC has been demonstrated as a prognostic or diagnostic marker to monitor different stages of tissue damage from H. pylori-infected gastrointestinal diseases30, 31. In addition, AhpC is required for intestinal colonization and for the survival of Helicobacter cinaedi under oxidative stress32. Similarly, as an abundant and versatile antioxidant enzyme, Fn-AhpC is involved in protection against hydrogen peroxide damage and may be important for Fn survival. Theoretically, for obligate anaerobic bacteria, which are extremely sensitive to oxidative stress, the AhpC antibody could block the protective role against hydrogen peroxide damage, suggesting that AhpC may serve as a potential target for the development of vaccines against the survival of Fn.
Furthermore, as a potential vaccine against H. pylori-infection, H. pylori-AhpC stimulates strong adaptive immunity by decreasing the bacterial load in the stomach22. Mycobacterium tuberculosis-AhpC elicits a strong humoural immune response and stimulates T cells33. The AhpC protein was considered a virulence factor important for the survival of mycobacteria within macrophages. S. typhimurium-AhpC is induced during macrophage interactions, and both cell-mediated and humoural responses to AhpC were developed during the course of infection through T helper cell activation34, 35. Subsequently, we identified that Fn-AhpC was strongly immunogenic for mice model and seropositive human donors. We observed that Fn contained an AhpC homologue that showed extremely low sequence identity with human AhpC (31%) and moderate identity (50~70%) with the intestinal bacterium, although highly conserved homologues of AhpC are widespread throughout bacteria. The results of the sequence analysis suggested that antibody for Fn-AhpC could be specific, reflecting low cross-reactivity with the host or commensal bacteria. Consistent with this result, western blot assay showed that antibodies against AhpC were specific for the serum from CRC patients with Fn infections.
In general, an alternative approach to induce cellular immunity by subunit vaccination involves formulations containing adjuvants capable of promoting this type of response. IgG is the most prevalent serum antibody is used as the most common correlate of protection, and SIgA, secreted by the gut mucosa, is an important contributor to gut barrier function36. In the present study, systemic prophylactic immunization with AhpC/alum exhibited higher IgG levels and conferred protection against infection in 77.3% of mice, while mucosal immunization with AhpC/cholera toxin conferred partial protection against infection in 50.6% of mice and elicited low levels of serum IgG but higher SIgA compared with systemic immunization. These results showed that both serum IgG levels and intestinal mucus SIgA in AhpC vaccines could play important roles in reducing the Fn load.
Recent studies have reported that Fn-DNA is enriched in early-stage CRC37. Consistently, in a previous study, we showed an increase of the total antibody levels of Fn in early CRC patients16, indicating that although Fn induced both humoural and cellular immune responses in early-stage tumours, the host was incapable of eradicating the pathogen Fn. The serological survey in the present study also showed elevated anti-AhpC levels in only a few patients with late-stage of CRC, suggesting that Fn overload in CRC patients likely reflect a lack of protective antibodies, such as the anti-AhpC antibody.
Previous studies have shown that antibodies can inhibit bacterial and fungal infections directly and prior to attachment38. Mycograb is an antibody against fungal heat-shock protein 90 (HSP90), which directly inhibits the growth of Candida in vitro 39. HSP90 is essential for cell viability and can protect cells against oxidative stress. Interestingly, the extracellular Hsp90 proteins are secreted via a non-classical exosomal protein secretory pathway40. In addition, as an antibody fragment without Fc component, Mycograb plays an inhibitory role via the complement-independent pathway. The similar antioxidant function of HSP90 with AhpC implies a similar antibacterial mechanism by which anti-AhpC antibody may act as an antibody-based AhpC inhibitor.
In summary, we have shown that immunization with recombinant Fn-AhpC protein is able to induce strong humoural immunity and can suppress Fn loads in the mouse intestinal tract. The serological survey further showed a lack of anti-AhpC antibodies in early-stage CRC patients. Importantly, we found that serum with a high titre of anti-AhpC antibodies was able to inhibit Fn growth in vitro. These results demonstrated that AhpC constitutes a potential target for immune responses during Fn infection and represents a promising candidate for Fn vaccine. Future studies will address multivalent subunit vaccination using combinations of several virulence proteins to eradicate intracellular infections, thus enhancing the protective effects of AhpC vaccination.
Materials and Methods
Bacterial strain and culture conditions
Fn ATCC 25586 was purchased from the Institute of Microbiology of Chinese Academy of Sciences. The organisms were anaerobically grown at 37 °C for 48 h in brain heart infusion (BHI, Oxoid, Hampshire, UK) broth prior to harvesting.
Patients, blood samples and ethical approval
Serum samples from 258 patients with primary CRC and from 92 healthy subjects were selected prior to surgery from an archive of blood samples at the Cancer Center of Sun Yat-sen University (SYSU), as previously described16. Ethics approval was granted by the Ethics Committee of SYSU Cancer Center (No. GZR2012–123). All experiments were performed in accordance with the approved guidelines and related regulations. Written informed consent was required for all patients involved in the present study.
Phylogenetic analyses and antigenic determinants prediction of AhpC
Phylogenetic tree based on the sequence alignment of AhpC coding regions was constructed using the Neighbour-Joining (N-J) method in the MEGA 5.1 software41 with 1,000 bootstrap replicates. The hydrophilicity, surface probability and antigenic index plots of AhpC protein were predicted according to the methods of Jameson-Wolf, Emini and Hopp-Woods using the DNAStar protein analysis system Lasergene 14.1 (Madison, WI, USA). The dominant B cell epitopes of the AhpC proteins were selected through comprehensive analysis.
Construction and purification of recombinant AhpC
The Fn-AhpC gene was PCR amplified using the following primer pair: 5′-CAG TAC GCA TAT GTC ATT AAT AGG AAG-3′ and: 5′-AGC GGA TCC TTA TAA TTC TCC AAT TAA ATC-3′, incorporating a NdeI and a BamHI restriction site, respectively. The PCR products were double digested to generate sticky ends and ligated into a digested pET28a expression vector (Novagen, Inc., Madison, WI, USA). The vector construct was transformed into E. coli DH5α. The amplified pET28a construct was purified from the cultured cells and transformed into E. coli BL21. Subsequently, isopropyl-β-D-thiogalactoside (IPTG, 0.5 mM) was added to the culture for 16 h at 25 °C to induce the expression of AhpC, and the fusion protein from the supernatant of the IPTG-induced bacterium lysate was purified using a standard Ni-NTA agarose column purification protocol (Sangon Biotech, China).
Recombinant AhpC identification by MALDI-TOF/TOF MS
The purified recombinant AhpC was extracted from gels stained with Coomassie brilliant blue R250 and digested with trypsin (Promega, USA) using the Mass Standards Kit for the 4700 Proteomics Analyser (Applied Biosystems); subsequently the tryptic protein hydrolysates were analysed using 4800 Plus MALDI TOF/TOFTM Analyser (Applied Biosystems, USA). Protein identification was repeated at least twice using bands from two different gels. The peptide mass fingerprint (PMF) was obtained using Mascot 2.2 software to search Swiss-Prot and NCBI nr protein databases.
Antibody detection using western blotting
Bacterial total protein or recombinant Fn-AhpC was separated using 10% SDS-PAGE and subsequently transferred onto PVDF membranes. After blocking with 5% non-fat dry milk in PBST, the membrane strips were incubated with pooled serum from 6 healthy subjects or separated serum from 6 Fn-positive CRC individuals as primary antibody (1:3000 dilution) at 4 °C overnight. Subsequently, the PVDF membrane strip was incubated with horseradish peroxidase (HRP) labelled anti-Mouse-IgA (1:8000) for 2 h. The bands were detected using Pierce ECL Plus Substrate (Thermo Scientific, USA) according to the manufacturer’s instructions.
Animal used and ethical approval
Specific pathogen-free and age-matched 4- to 8-week-old female BALB/c mice were purchased from Sun Yat-Sen University (Guangzhou, China). All animal procedures were authorized by the Sun Yat-Sen University Animal Experimentation Ethics Committee and performed in accordance with the approved guidelines (Ethics number: IACUC- DD-16-0301).
Immunization with AhpC and assessment of protective efficacy
Mice were immunized according to the schedule shown in Table 1. In the initial systemic immunization study, mice were immunized intraperitoneally with PBS, alum, AhpC (100 μg) or AhpC (100 μg) combined with alum (1:1, Imject Pierce, USA) at two weeks apart. In the mucosal study, the mice were immunized once a week with 3 orogastric doses containing PBS, cholera toxin (CT, 10 μg, Sigma-Aldrich), AhpC (100 μg) or AhpC (100 μg) combined with cholera toxin. At one week after the final immunization (week 6), the mice were challenged with Fn (1 × 108 CFU/ml, 100 μl) by oral gavage daily for a week.
The load levels of Fn within mice intestines tissues were quantified by qPCR using SYBR Green PCR MasterMix (Applied Biosystems, USA). The following primers were used in the qPCR: Fn forward: 5′-ATA CCG GGA ATA AAG ACA-3′ and reverse: 5′-TAC AAC CCA ATC CAT AAG T-3′. Universal 16 S rDNA forward: 5′-CGC TAG TAA TCG TGG ATC AGA ATG-3′ and reverse: 5′-TGT GAC GGG CGG TGT GTA-3′16, 42. The copy numbers of Fn DNA and 16S rRNA were determined after serially diluting the standards (108~101 copies of plasmid DNA containing the respective amplicon). Subsequently, quantifications of Fn were normalized to the 16S rRNA copies as following: Fn copies = Fn(target) copies × (108/16S rRNA copies of total). Bacterial quantity was expressed as bacteria per gram of colon (approximately one copy per cell)43. The rate of protection was calculated using the following the formula: protection rate (%) = (infection percentage in the control group − infection percentage in the immunized group)/infection percentage in the control group × 100%44.
Evaluation of serum antibody responses by ELISA
ELISA plates were coated with purified AhpC (0.5 μg/ml; 100 μl/well) overnight at 4 °C. Serum samples from CRC patients were diluted at 1:50. Sera extracted from immunized mice for 6 weeks were diluted from 1:100 to 1:12800. Intestinal mucus samples were collected from a 10 cm portion of the small intestine and diluted at 1:10 and at 1:4 serial dilutions. Subsequently, the samples were added in duplicates for 1 h at 37 °C, and the plates were washed three times with PBST. Next, 100 μl of goat anti-mouse IgG or IgA conjugated with HRP (1:8000, EarthOx, USA) was incubated at 37 °C for 30 min. Next, the plates were washed and the substrate (tetramethylbenzidine) solution was added, and subsequently, the reaction was terminated using 2 M H2SO4 and read at an OD of 450 nm using an ELISA spectrophotometer (Bio-Rad, USA).
Serum bactericidal assays
Serum bactericidal assays were performed according to the method described by Lewis LA et al.45. Briefly, approximately 1 × 105 CFU of Fn bacteria were incubated with the pooled serum (two-fold serial diluted in BHI) from immunized/unimmunized mice or serum from CRC patients/healthy subjects, respectively. After incubation at 37 °C for 30 min (t30) anaerobically, live bacteria with serial dilutions were counted using the standard plate count method. Survival ratio was calculated as the number of viable colonies at t30 relative to t0.
Serum antibacterial assays
The pooled serum from immunized mice was serially diluted from 1:1 to 1:64 in serum from unimmunized mice. Similarly, the pooled serum from CRC patients was serially diluted from 1:1 to 1:64 in serum from healthy subjects. 1 × 105 CFU of Fn bacteria were subsequently cultured with 25% pooled serum in BHI broth at 37 °C for 48 h anaerobically. The minimum inhibitory concentration (MIC) of the immunized mouse serum or CRC patient serum was determined according to the standard broth microdilution method. The lowest concentration that completely inhibited microbial growth, as determined by optical density measurements at 600 nm, was considered the MIC. All reactions were performed in triplicate. The viability of Fn bacteria was monitored using the LIVE/DEAD BacLight Bacterial Viability Kit (Thermo, USA) and detected using flow cytometry (Merck Darmstadt, Germany). All protocols were performed according to the manufacturer’s instructions. Viable bacteria were labelled with SYTO 9, whereas dead bacteria were labelled with propidium iodide (PI).
Statistical analysis
All statistical analyses were performed using the SPSS 16.0 statistical software package (SPSS Inc., Chicago, IL). The relationships between the anti-AhpC antibodies and the clinicopathological features were analysed using the Mann-Whitney U test. Comparisons of Fn colonization numbers and the specific anti-AhpC antibodies for the different groups of immunized mice were assessed using a two-tailed Student’s t test. The results of the antibody and F. nucleatum load levels were expressed as the means ± standard deviation (SD). The correlation between the levels of antibodies to F. nucleatum bacteria and AhpC antigen in the serum of CRC patients was analysed using Pearson’s correlation coefficient and linear regression. The statistical limit for significance was P < 0.05.
Electronic supplementary material
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81372573; No. 81673005).
Author Contributions
S.-H.G., H.-F.W., Z.-G.N., Y.-D.W., Q.-Y.Z. and G.Z. contributed to the conception, designed the study, performed research and collected data. S.-H.G., H.-F.W. and G.Z. analysed data, wrote and revised the paper. All authors read and approved the final manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Song-He Guo and Hai-Fang Wang contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-11127-x
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yu YN, et al. Berberine may rescue Fusobacterium nucleatum-induced colorectal tumorigenesis by modulating the tumor microenvironment. Oncotarget. 2015;6:32013–32026. doi: 10.18632/oncotarget.5166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kostic AD, et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe. 2013;14:207–215. doi: 10.1016/j.chom.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flanagan L, et al. Fusobacterium nucleatum associates with stages of colorectal neoplasia development, colorectal cancer and disease outcome. Eur J Clin Microbiol. 2014;33:1381–1390. doi: 10.1007/s10096-014-2081-3. [DOI] [PubMed] [Google Scholar]
- 4.Wu N, et al. Dysbiosis signature of fecal microbiota in colorectal cancer patients. Microb Ecol. 2013;66:462–470. doi: 10.1007/s00248-013-0245-9. [DOI] [PubMed] [Google Scholar]
- 5.Mima K, et al. Fusobacterium nucleatum in colorectal carcinoma tissue and patient prognosis. Gut. 2015;65:1973–1980. doi: 10.1136/gutjnl-2015-310101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong SH, et al. Quantitation of faecal Fusobacterium improves faecal immunochemical test in detecting advanced colorectal neoplasia. Gut. 2016;0:1–8. doi: 10.1136/gutjnl-2016-312766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liang Q, et al. 303 Fecal Bacteria Act as Novel Biomarkers for Non-Invasive Diagnosis of Colorectal Cancer. Gastroenterology. 2016;150 doi: 10.1016/S0016-5085(16)30349-3. [DOI] [Google Scholar]
- 8.Signat B, Roques C, Poulet P, Duffaut D. Fusobacterium nucleatum in periodontal health and disease. Curr Issues Mol Biol. 2011;13:25–36. [PubMed] [Google Scholar]
- 9.Paster BJ, Olsen I, Aas JA, Dewhirst FE. The breadth of bacterial diversity in the human periodontal pocket and other oral sites. Periodontol 2000. 2006;42:80–87. doi: 10.1111/j.1600-0757.2006.00174.x. [DOI] [PubMed] [Google Scholar]
- 10.Bao K, Belibasakis GN, Selevsek N, Grossmann J, Bostanci N. Proteomic profiling of host-biofilm interactions in an oral infection model resembling the periodontal pocket. Sci Rep. 2015;5 doi: 10.1038/srep15999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lange L, et al. Symptoms of periodontitis and antibody responses to Porphyromonas gingivalis in juvenile idiopathic arthritis. Pediatr Rheumatol. 2016;14 doi: 10.1186/s12969-016-0068-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mikuls TR, et al. Periodontitis and Porphyromonas gingivalis in patients with rheumatoid arthritis. Arthritis Rheumatol. 2014;66:1090–1100. doi: 10.1002/art.38348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sparks Stein P, et al. Serum antibodies to periodontal pathogens are a risk factor for Alzheimer’s disease. Alzheimers Dement. 2012;8:196–203. doi: 10.1016/j.jalz.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamamura K, et al. Human microbiome Fusobacterium nucleatum in esophageal cancer tissue is associated with prognosis. Clin Cancer Res. 2016;22:5574–5581. doi: 10.1158/1078-0432.CCR-16-1786. [DOI] [PubMed] [Google Scholar]
- 15.Velsko IM, et al. Fusobacterium nucleatum Alters Atherosclerosis Risk Factors and Enhances Inflammatory Markers with an Atheroprotective Immune Response in ApoE(null) Mice. PloS one. 2015;10 doi: 10.1371/journal.pone.0129795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang HF, et al. Evaluation of antibody level against Fusobacterium nucleatum in the serological diagnosis of colorectal cancer. Sci Rep. 2016;6 doi: 10.1038/srep33440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu J, Holmgren A. The thioredoxin antioxidant system. Free Radic Biol Med. 2014;66:75–87. doi: 10.1016/j.freeradbiomed.2013.07.036. [DOI] [PubMed] [Google Scholar]
- 18.Reynolds C, et al. T Cell Immunity to the Alkyl Hydroperoxide Reductase of Burkholderia pseudomallei: A Correlate of Disease Outcome in Acute Melioidosis. J Immunol. 2015;194:4814–4824. doi: 10.4049/jimmunol.1402862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim YH, et al. Immunoproteomically identified GBAA_0345, alkyl hydroperoxide reductase subunit C is a potential target for multivalent anthrax vaccine. Proteomics. 2014;14:93–104. doi: 10.1002/pmic.201200495. [DOI] [PubMed] [Google Scholar]
- 20.Velineni S, Timoney JF. Identification of novel immunoreactive proteins of Streptococcus zooepidemicus with potential as vaccine components. Vaccine. 2013;31:4129–4135. doi: 10.1016/j.vaccine.2013.06.100. [DOI] [PubMed] [Google Scholar]
- 21.Taylor PD, Inchley CJ, Gallagher MP. The Salmonella typhimurium AhpC polypeptide is not essential for virulence in BALB/c mice but is recognized as an antigen during infection. Infect Immun. 1998;66:3208–3217. doi: 10.1128/iai.66.7.3208-3217.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Riordan AA, et al. Alkyl hydroperoxide reductase: a candidate Helicobacter pylori vaccine. Vaccine. 2012;30:3876–3884. doi: 10.1016/j.vaccine.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 23.Polak D, Wilensky A, Shapira L, Weiss EI, Houri-Haddad Y. Vaccination of mice with Porphyromonas gingivalis or Fusobacterium nucleatum modulates the inflammatory response, but fails to prevent experimental periodontitis. J Clin Periodontol. 2010;37:812–817. doi: 10.1111/j.1600-051X.2010.01598.x. [DOI] [PubMed] [Google Scholar]
- 24.Dye BA, et al. Serum antibodies to periodontal bacteria as diagnostic markers of periodontitis. J Periodontol. 2009;80:634–647. doi: 10.1902/jop.2009.080474. [DOI] [PubMed] [Google Scholar]
- 25.Liu PF, Haake SK, Gallo RL, Huang CM. A novel vaccine targeting Fusobacterium nucleatum against abscesses and halitosis. Vaccine. 2009;27:1589–1595. doi: 10.1016/j.vaccine.2008.12.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nakagaki H, et al. Fusobacterium nucleatum envelope protein FomA is immunogenic and binds to the salivary statherin-derived peptide. Infect Immun. 2010;78:1185–1192. doi: 10.1128/IAI.01224-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu PF, et al. Vaccination targeting surface FomA of Fusobacterium nucleatum against bacterial co-aggregation: Implication for treatment of periodontal infection and halitosis. Vaccine. 2010;28:3496–3505. doi: 10.1016/j.vaccine.2010.02.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma L, Ding Q, Feng X, Li F. The protective effect of recombinant FomA-expressing Lactobacillus acidophilus against periodontal infection. Inflammation. 2013;36:1160–1170. doi: 10.1007/s10753-013-9651-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khansari N, Shakiba Y, Mahmoudi M. Chronic inflammation and oxidative stress as a major cause of age-related diseases and cancer. Recent Pat Inflamm Allergy Drug Discov. 2009;3:73–80. doi: 10.2174/187221309787158371. [DOI] [PubMed] [Google Scholar]
- 30.Huang CH, et al. Alkylhydroperoxide reductase of Helicobacter pylori as a biomarker for gastric patients with different pathological manifestations. Biochimie. 2011;93:1115–1123. doi: 10.1016/j.biochi.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 31.Pourakbari B, et al. Evaluation of a new antigen for diagnosis of Helicobacter pylori infection in stool of adult and children. Helicobacter. 2011;16:42–46. doi: 10.1111/j.1523-5378.2010.00813.x. [DOI] [PubMed] [Google Scholar]
- 32.Charoenlap N, et al. Alkyl hydroperoxide reductase is required for Helicobacter cinaedi intestinal colonization and survival under oxidative stress in BALB/c and BALB/c interleukin-10-/- mice. Infect Immun. 2012;80:921–928. doi: 10.1128/IAI.05477-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gupta A, et al. Mycobacterium tuberculosis: immune evasion, latency and reactivation. Immunobiology. 2012;217:363–374. doi: 10.1016/j.imbio.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 34.Hoiseth SK, Stocker BA. Aromatic-dependent Salmonella typhimurium are non-virulent and effective as live vaccines. Nature. 1981;291:238–239. doi: 10.1038/291238a0. [DOI] [PubMed] [Google Scholar]
- 35.Maybeno M, et al. Polyfunctional CD4+ T cell responses to immunodominant epitopes correlate with disease activity of virulent Salmonella. PloS one. 2012;7 doi: 10.1371/journal.pone.0043481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mantis NJ, Rol N, Corthesy B. Secretory IgA’s complex roles in immunity and mucosal homeostasis in the gut. Mucosal Immunol. 2011;4:603–611. doi: 10.1038/mi.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yu J, et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut. 2017;66:70–78. doi: 10.1136/gutjnl-2015-309800. [DOI] [PubMed] [Google Scholar]
- 38.Forthal DN. Functions of Antibodies. Microbiol Spectr. 2014;2:1–17. doi: 10.1128/microbiolspec.AID-0019-2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matthews RC, et al. Preclinical assessment of the efficacy of mycograb, a human recombinant antibody against fungal HSP90. Antimicrob Agents Chemother. 2003;47:2208–2216. doi: 10.1128/AAC.47.7.2208-2216.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li W, Sahu D, Tsen F. Secreted heat shock protein-90 (Hsp90) in wound healing and cancer. Biochim Biophys Acta. 2012;1823:730–741. doi: 10.1016/j.bbamcr.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tamura K, et al. MEGA5: molecular evolutionary genetics analysis using maximum likelihood, evolutionary distance, and maximum parsimony methods. Mol Biol Evol. 2011;28:2731–2739. doi: 10.1093/molbev/msr121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Trombone AP, et al. Periodontitis and arthritis interaction in mice involves a shared hyper-inflammatory genotype and functional immunological interferences. Genes Immun. 2010;11:479–89. doi: 10.1038/gene.2010.13. [DOI] [PubMed] [Google Scholar]
- 43.van Minnen LP, et al. Modification of intestinal flora with multispecies probiotics reduces bacterial translocation and improves clinical course in a rat model of acute pancreatitis. Surgery. 2007;141:470–80. doi: 10.1016/j.surg.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 44.Wu C, et al. Protection against Helicobacter pylori infection in mongolian gerbil by intragastric or intramuscular administration of H. pylori multicomponent vaccine. Helicobacter. 2008;13:191–199. doi: 10.1111/j.1523-5378.2008.00609.x. [DOI] [PubMed] [Google Scholar]
- 45.Vu DM, Wong TT, Granoff DM. Cooperative serum bactericidal activity between human antibodies to meningococcal factor H binding protein and neisserial heparin binding antigen. Vaccine. 2011;29:1968–1973. doi: 10.1016/j.vaccine.2010.12.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.