Abstract
Objective To assess the effects of psychosocial and psychological interventions compared with usual antepartum, intrapartum, or postpartum care on the risk of postnatal depression.
Data sources Medline, Embase, CINAHL, Cochrane central register of controlled trials, Cochrane pregnancy and childbirth group trials register, Cochrane depression, anxiety, and neurosis trials register, secondary references and review articles, and experts in the field.
Study selection All published and unpublished randomised controlled trials of preventive psychosocial or psychological interventions in which the primary or secondary aim was a reduction in the risk of postnatal depression. All trials recruited pregnant women or new mothers less than six weeks postpartum. Eligible studies were abstracted, assessed for methodological quality, and pooled with relative risk for categorical data and weighted mean difference for continuous data.
Results Fifteen trials with 7697 women were included. Although there was no overall statistically significant effect on the prevention of postnatal depression in the meta-analysis of all types of interventions (15 trials, n = 7697; relative risk 0.81, 95% confidence interval 0.65 to 1.02), these results suggest a potential reduction in postnatal depression. The only intervention to have a clear preventive effect was intensive postpartum support provided by a health professional (0.68, 0.55 to 0.84). Identifying women “at risk” assisted in the prevention of postnatal depression (0.67, 0.51 to 0.89). Interventions with only a postnatal component were more beneficial (0.76, 0.58 to 0.98) than interventions that incorporated an antenatal component. In addition, individually based interventions were more effective (0.76, 0.59 to 1.00) than group based interventions (1.03, 0.65 to 1.63).
Conclusions Diverse psychosocial or psychological interventions do not significantly reduce the number of women who develop postnatal depression. The most promising intervention is the provision of intensive, professionally based postpartum support.
Introduction
Postnatal depression is a major health issue for many women from diverse cultures.1,2 Although longitudinal and epidemiological studies have yielded varying prevalence rates, a meta-analysis of 59 studies reported a prevalence of 13%,3 with most cases starting in the first three months postpartum.4 This morbidity has well documented health consequences for the mother, child, and family. Women who have postnatal depression are significantly more likely to experience future episodes of depression,5 and infants and children are particularly vulnerable because of impaired maternal-infant interactions and negative perceptions of infant behaviour.
The cause of postnatal depression remains unclear,6 with extensive research suggesting many contributory factors. Epidemiological studies and meta-analyses of predictive studies, however, have consistently identified the importance of psychosocial and psychological risk factors3,6,7—such as life stress,3,7-9 marital conflict,3,7-10 maternal self esteem,7,11 and lack of social support.3,7,9,11-15 A comprehensive review suggested that in women with postnatal depression, psychosocial and psychological treatment may be suitable.16 As such, it is theoretically possible that these interventions may also prevent postnatal depression, as many of the known risk factors are present during pregnancy and the immediate postpartum period. There have been two critical reviews of preventive trials17,18 and one systematic review that examined diverse interventions to reduce “probable depression” in the postnatal period.19 However, no systematic review has examined the overall preventive effect of psychosocial and psychological interventions or determined which characteristics are most beneficial.
I assessed the effects of such interventions compared with usual antepartum, intrapartum, or postpartum care on the risk of postnatal depression. This systematic review is based on a full review published in the Cochrane Library.20
Methods
Searches
I searched the Cochrane pregnancy and childbirth group trials register. This database contains trials identified from quarterly searches of the Cochrane central register of controlled trials, monthly searches of Medline and hand searches of 30 journals and the proceedings of major conferences. In addition, the Cochrane depression, anxiety, and neurosis trials register, Medline (1966-2004), Embase (1980-2004), and CINAHL (1982-2004) were all independently searched. Secondary references and review articles were scanned and experts in the field were contacted. Trials published in all languages were considered.
Selection
Published and unpublished studies were eligible if they were randomised controlled trials; were methodologically strong based on a validity assessment; evaluated a psychosocial or psychological intervention in which the primary or secondary aim was a reduced risk of postnatal depression; and included pregnant women and new mothers less than six weeks postpartum. I excluded studies if they incorporated a quasi-randomised design; recruited women identified with symptoms of depression, or solely evaluated an educational intervention. For this review, a psychosocial or psychological intervention incorporated various non-pharmaceutical strategies that were delivered antenatally or within the first month postpartum, or both, by a health professional or layperson.
Assessment of validity
The methodological quality of each trial was assessed according to the recommendations of the Cochrane Collaboration and examined the generation of allocation sequence; allocation concealment; blinding of outcome assessors; completeness of follow-up data; and intention to treat analysis. Two reviewers independently assigned a quality rating to each trial; results were compared and differences discussed until agreement was obtained.
Abstraction of data
Two reviewers independently extracted data and included study design; participants (number and characteristics); intervention type, mode, onset, duration, and provider; outcomes measured; and results. Wherever necessary, unpublished or missing data were requested from the trial's corresponding author and data were double entered into Review Manager version 4.2.3 (Cochrane Collaboration software).
Quantitative data synthesis
While the primary meta-analysis was based on the occurrence of postnatal depression (however measured by trialists), several depression rating scales or cut-off points were incorporated. To address the potential measurement differences, I made direct comparisons using a fixed effect model between trials using the same rating scale and cut off. Meta-analyses were performed using relative risks as the measure of effect size for binary outcomes and weighted mean differences for continuous outcome measures, both with 95% confidence intervals.
Heterogeneity was investigated by calculating I2 statistics,21 and if this indicated a high level among the trials included in an analysis (I2 > 50%), a random effects meta-analysis was used. Where I found high levels of heterogeneity I used sensitivity analyses, excluding the trials most susceptible to bias based on the following quality assessment: those with unclear allocation concealment, high levels of losses or exclusions after randomisation, or uncertain on no blinding of outcome assessment. A priori subgroup analyses estimated the effect of intervention type (for example, psychosocial and psychological), intervention mode (for example, individual v group based), intervention onset (for example, antenatal and postnatal v postnatal only), and sample selection criteria (for example, targeting women with specific risk factors v a general population).
Results
The search identified 155 studies, of which 99 were excluded as non-experimental. Of the 56 trials retrieved for a more detailed evaluation, 15 studies were of treatment interventions for postnatal depression. The 41 remaining potentially appropriate trials were examined for inclusion/exclusion criteria and methodological quality. I excluded 26 trials because of a quasi-experimental design (n = 4),22-25 poor methodological quality (n = 3),26-28 not a psychosocial or psychological intervention (n = 12),29-40 the prevention of postnatal depression was not the primary or secondary objective (n = 5),41-45 and the intervention was for the treatment of antenatal depression (n = 2)46,47 (table 1).
Table 1.
Characteristics of excluded studies
| Study | Reason for exclusion |
|---|---|
| Buist26 | Methodologically weak pilot trial (n=44) with unclear randomisation method. Significant group differences in baseline characteristics. No usable outcome data; published data were mean scores without SD |
| Chabrol22 | Not randomised controlled trial. Odd v even number group assignment. Data not analysed with intention to treat |
| Elliott23 | Not randomised controlled trial. Group allocation based on delivery date. Potential selection bias with significant differences between participating and non-participating eligible women. Data presented with median instead of mean results |
| Gordon24 | Not randomised controlled trial. Inexplicit non-random group allocation. Primary outcome was “emotional upset” with subjective measure. Characteristics of participants lacking and 46% of mothers lost to follow-up |
| Gordon41 | Postnatal depression not the primary or secondary outcome. Poor measure of postnatal depression that included single item question and subscore on mental health index of SF-36. In addition, 30% women excluded after randomisation |
| Harris29 | Intervention not psychosocial or psychological; examined effect of thyroxine to prevent postnatal depression among thyroid-antibody-positive women |
| Harrison-Hohner30 | Intervention not psychosocial or psychological; examined effect of prenatal calcium supplementation. Postnatal depression was not primary or secondary outcome |
| Hayes31 | Intervention not psychosocial or psychological; included single educational session about postnatal depression, provided antenatally by midwife |
| Heh32 | Intervention not psychosocial or psychological; included only information related to postnatal depression |
| Hodnett42 | Postnatal depression not primary or secondary outcome |
| Lawrie34 | Intervention not psychosocial or psychological; examined effect of norethisterone enanthate (progesterone therapy) |
| Lieu43 | Premature assessment of postnatal depression (two weeks after delivery), which was neither primary or secondary outcome |
| Llorente33 | Intervention not psychosocial or psychological; examined effect of docosahexaenoic acid supplementation |
| Marks27 | Methodologically weak for “prevention” trial. About 25% of participants were currently suffering from depression at recruitment and 49% had depressive episode sometime during perinatal period |
| Okano35 | Intervention not psychosocial or psychological; study examined educational session retrospectively involving two non-randomised groups of women who sought psychiatric care postnatally |
| Rees36 | Intervention not psychosocial or psychological; examined effect of relaxation with guided imagery |
| Saisto44 | Postnatal depression not primary or secondary outcome; statistical results related to Postnatal depression not reported |
| Serwint25 | Not randomised controlled trial. Group allocation based on two week period |
| Shields45 | Study reports on element of larger trial where primary and secondary outcome was not postnatal depression. One item on Edinburgh scale (self harm) excluded, rendering clinical interpretability of outcome data questionable |
| Sichel37 | Intervention not psychosocial or psychological; examined effect of oestrogen therapy |
| Spinelli46 | Intervention targeting treatment of antenatal depression not prevention of postnatal depression |
| Spinelli47 | Intervention targeting treatment of antenatal depression not prevention of postnatal depression |
| Webster38 | Intervention not psychosocial or psychological; included antenatal identification as high risk, educational booklet and discussion about risk of developing postnatal depression, and letter to woman's referring general practitioner and local child health nurse alerting them of woman's risk |
| Wolman28 | Methodologically weak trial. Researchers significantly changed study protocol before trial completion. Inability to assess selection bias. Trial had 21% loss to follow-up and poor measure of postnatal depression (Pitt depression inventory) used for main portion of trial |
| Wisner39 | Intervention was not psychosocial or psychological; examined effect of antidepressant medication |
| Wisner40 | Intervention was not psychosocial or psychological; examined effect of antidepressant medication |
Study characteristics
The 15 trials in the meta-analysis incorporated 7697 women and were published between 1995 and 2003 (table 2). Most trials were conducted in Australia and the United Kingdom; two trials were conducted in the United States48,49 and one in China.50 Seven trials targeted women believed to be at additional risk of postnatal depression,48-54 while the eight others enrolled women from the general population.
Table 2.
Characteristics of included studies
| Study | Methods (all RCTs) | Participants | Interventions | Outcome | Notes |
|---|---|---|---|---|---|
| Armstrong51 | Randomisation performed with computer generated random numbers table and completed by clerical staff not involved in eligibility assessment. Power analysis performed and outcome assessor blinded to group allocation. Nurses providing intervention blinded to six weeks postpartum (within usual care parameters). Attrition rate 12% at 16 weeks | 181 mothers (90 in intervention; 91 in control) who gave birth in one urban hospital in Queensland, Australia. Families were included where child, for environmental reasons, was at increased risk for poor health and developmental outcomes | Intervention: weekly nursing home visits for first 6 weeks, fortnightly until 12 weeks, then monthly until 24 weeks. Mothers also encouraged to access existing community services Control: standard care, included encouragement to access existing community services, offer of home visits by nurse (usually limited to one visit), and no limit on number of centre visits (by appointment only) | EPDS > 12 at 6 and 16 weeks postpartum | Only 63% of mothers completed screening questionnaire before trial |
| Brugha52 | Randomisation performed with computer based stratification process with minimisation on three prognostic factors (level of support, screening, and ethnic group). Power analysis performed and outcome assessors blinded to group allocation. Attrition rate 9% at 12 weeks | 209 pregnant women (103 in intervention; 106 in control) who attended antenatal clinics in UK hospital between 12 and 20 weeks' gestation identified by screening to be at increased risk of postnatal depression | Intervention: Preparing for Parenthood—six structured two hour weekly antenatal classes (preceded by initial introductory meeting with participant and her partner) and one reunion class at eight weeks postpartum. Classes provided by trained nurse and occupational therapist and based on established psychological models for tackling depression together with emerging models for enhancing social support | EPDS > 10 at 12 weeks postpartum | Only 45% of participants in intervention group attended enough sessions to “likely receive benefit” |
| Gamble54 | Randomisation performed with consecutively numbered, sealed, opaque envelopes. Power analysis conducted and outcome assessor blinded to group allocation. Attrition rate 0% at 12 weeks | 103 mothers (50 in intervention; 53 in control) assessed for labour trauma risk in immediate postpartum period in hospital in Brisbane, Australia | Intervention: one midwife-led debriefing session before hospital discharge and another at 6-8 weeks postpartum. Control: standard care with no debriefing session | EPDS > 12 at 12 weeks postpartum | |
| Gorman48 | Randomisation performed with random numbers table and blocking strategy based on presence or absence of current or past history of depression. Outcome data collected via interview and mailed questionnaires. Attrition rate 18% at 24 weeks | 45 pregnant women (24 in intervention; 21 in control) at risk of postnatal depression attending various obstetric clinics in Iowa City and St Louis, US | Intervention: five individual sessions based on interpersonal psychotherapy, beginning in late pregnancy and ending at about four weeks after birth | EPDS > 12 and SCID at 4 and 24 weeks postpartum | |
| Gunn59 | Randomisation performed via telephone through centrally controlled randomisation centre. Power analysis conducted and outcome data collected via mailed questionnaires. Attrition rate 34% at 24 weeks | 683 healthy mothers (Nos in each group not stated) who gave birth in one rural and one metropolitan hospital in Victoria, Australia. Women excluded if they were patients of general practitioners who were trial reference group, attended teenage clinic, or delivered by emergency caesarean section | All participants received letter and appointment date to see general practitioner for checkup: intervention group for 1 week after hospital discharge and control group for 6 weeks postpartum | EPDS > 12 at 12 and 24 weeks | |
| Lavender61 | Randomisation performed with computer generated numbers and consecutively numbered, sealed opaque envelops. Power analysis conducted and outcome data collected via mailed questionnaire. Attrition rate 5% at three weeks | 114 primiparous mothers (60 in intervention; 60 in control) in UK teaching hospital. Inclusion criteria: singleton pregnancy, cephalic presentation, spontaneous labour at term, normal vaginal delivery. | Intervention: one debriefing session lasting 30-120 minutes before hospital discharge, provided by midwife with no formal training Control: standard care with no debriefing session | HADS > 10 at 3 weeks postpartum | Atypical population, 60% were single mothers |
| MacArthur56 | Cluster design—randomisation performed with customised, computer program in independent clinical trials unit. 17 practices randomised to intervention and 19 were to control. Power analysis conducted and outcome data collected via mailed questionnaires. Attrition rate 27% at 16 weeks | 2064 UK mothers (1087 in intervention; 977 in control). Excluded mothers expected to move out of general practice area | Intervention: flexible, individualised, extended home visits by midwife to 28 days postpartum that included screening with symptoms checklist and EPDS; referral to general practitioner as necessary' and 10-12 week discharge visit Control: standard care, included seven midwifery home visits to 10-14 days postpartum (may extend to 28 days) and care by health visitors thereafter. General practitioners completed routine home visits and final check up at 6-8 weeks postpartum | EPDS > 12 at 16 weeks postpartum | |
| Morrell57 | Randomisation performed with random numbers table and consecutively numbered, sealed opaque envelopes. Power analysis conducted and outcome data collected via mailed questionnaires. Attrition rate 21% at 24 weeks | 623 UK mothers (311 in intervention; 312 in control). Exclusion criteria: insufficient English to complete questionnaires and infant in special care unit for >48 hours | Intervention: postnatal care at home by community midwives plus up to 10 home visits in first month postpartum lasting up to 3 hours provided by community postnatal support worker Control: postnatal care at home by community midwives | EPDS >12 at 6 and 24 weeks postpartum | |
| Priest62 | Randomisation performed within strata of parity and mode of delivery. Each woman selected envelope from group of at least six sealed, opaque envelopes containing random allocation. Power analysis conducted and outcome data collected via mailed questionnaires. Attrition rate 19% at 52 weeks | 1745 Australian mothers (875 in intervention; 870 in control). Exclusion criteria: insufficient English to complete questionnaires, being under psychological care at time of delivery, mother aged <18 years, and infant needing neonatal intensive care | Intervention: single, standardised debriefing session provided in hospital immediately after randomisation of next day; duration ranged from 15 minutes to 1 hour and all research midwives received training in critical incident stress debrieting Control: standard postpartum care | EPDS >12 at 8, 24, and 52 weeks postpartum | |
| Reid55 | 2×2 factorial design, randomisation performed with computer generated scheme with randomised permuted blocks, stratified by centre. Power analysis conducted and outcome data collected via mailed questionnaires. Attrition rate 29% at 24 weeks | 1004 UK mothers (503 in intervention; 501 in control). All primiparous women attending antenatal clinics in two participating hospitals. Women whose infant subsequently died or was admitted to the special care unit for >2 weeks were excluded | Two postpartum interventions incorporating four groups: control, mailed self help materials, invitation to support group, and self help materials plus invitation to support group. Data analysed by pooling four groups as self help v no self help and support group v no support group. Support groups run on weekly basis for two hours, facilitated by trained midwives | EPDS >11 at 12 and 24 weeks postpartum | For this review, only support group v no support group comparisons were included. Only 18% of participants in intervention group attended support group session |
| Small60 | Randomisation performed via telephone with computer generated randomisation schedule for each midwife. Power analysis conducted and outcome data collected via mailed questionnaire. Attrition rate 12% at 24 weeks | 1041 mothers (520 in intervention; 521 in control) who had operative delivery in large maternity teaching hospital in Melbourne, Australia | Intervention: midwife-led debriefing session before discharge to provide women with opportunity to discuss their labour, birth, and events and experiences after delivery Control: standard care, included brief visit from midwife on discharge to give pamphlet on sources of assistance | EPDS >12 at 24 weeks postpartum | |
| Stamp53 | Randomisation performed with consecutively numbered, sealed opaque envelopes with stratification by parity. Power analysis conducted and outcome data collected via mailed questionnaire. Attrition rate 13% at 24 weeks | 144 pregnant women (73 in intervention; 71 in control) screened for risk of postnatal depression during antenatal clinic visits in Adelaide, Australia. Inclusion criteria: English-speaking, singleton fetus, and <24 weeks' gestation | Intervention: routine antenatal care plus two antenatal and one postnatal midwife-led group sessions Control: routine antenatal and postnatal care, which included class at six weeks postpartum that incorporated video on postnatal depression | EPDS >12 at 6, 12, and 24 weeks postpartum | High number of women screened “vulnerable” and only 31% of participants in intervention group attended all three sessions |
| Tam50 | Randomisation performed with random numbers table and consecutively numbered, sealed, opaque envelopes. Power analysis conducted and outcome data collected via interview and mailed questionnaires. Attrition rate 21% at 6 weeks | 560 Chinese mothers in hospital (280 in each group) with at least one suboptimal outcome in perinatal period ranging from antenatal complications requiring admission, elective caesarean section, labour induction, postpartum haemorrhage, infant admission to special care unit, etc | Intervention: routine postpartum care plus 1-4 sessions of “educational counselling” by research nurse before hospital discharge that included information related to adverse event and counselling to assist mother to “come to terms with her losses and find solutions to specific difficulties” (median total time 35 minutes). Twenty four women also received one session with physician | HADS >4 at 6 weeks postpartum | Health professionals not blinded to group allocation |
| Waldenstrom58 | Randomisation performed via telephone with consecutively numbered, sealed, opaque envelopes. Power analysis conducted and outcome data collected via mailed questionnaires. Attrition rate 7% at 8 weeks | 1000 pregnant low risk mothers (495 in intervention; 505 in control) attending antenatal clinic in Melbourne, Australia. Inclusion criteria: >25 weeks' gestation, English-speaking, and low medical risk | Intervention: team midwifery care provided antenatally and postnatally in hospital with focus on continuity Control: standard antenatal and postnatal care by physicians and midwives with no focus on continuity | EPDS >12 at 8 weeks postpartum | Demographic differences found between responders and non-responders |
| Zlotnick49 | Unclear randomisation process. Outcome data collected via interview. Attrition rate 6% at 12 weeks | 37 pregnant women (17 in intervention; 18 in control) on public assistance who had at least one risk factor for postnatal depression and were attending prenatal clinic at general hospital in northeast US | Intervention: Survival Skills for New Moms, which involved four 60 minute group sessions over four weeks based on principles of interpersonal psychotherapy Control: standard antenatal care | SCID at 12 weeks postpartum | 50% of eligible women declined to participate; 77% of participants were single women |
RCT=randomised controlled trial; EPDS=Edinburgh postnatal depression scale; HADS=hospital anxiety depression scale; SCID=structured clinical interview for DSM-IV.
Types of interventions
The studies were subgrouped into categories to examine specific types of psychosocial interventions—such as antenatal and postnatal classes,52,53,55 professional51,56 and lay57 home visits, continuity of care,58 and early postpartum follow-up (for example, postpartum care initiated earlier than usual practice)59—and psychological interventions, such as debriefing50,54,60-62 and interpersonal psychotherapy.48,49 The interventions were provided by various professionals, including physicians,59 nurses,50-52 midwives,53-56,58,60-62 and other healthcare providers.48,52 In one trial, the intervention was provided by lay women recruited from the community.57 In most studies, the control group was reported to have received usual antenatal/postnatal care, which varied both between and within countries.
Definition of postnatal depression
In all trials but one,49 postnatal depression was defined as a score above a specified cut-off point on a self reported measure. Most studies (10 out of 15) used an Edinburgh postnatal depression scale score > 12 to indicate postnatal depression. Two additional trials used the Edinburgh postnatal depression scale but incorporated a different cut off score; one study used a 10/11 cut off52 while another selected a 11/12 cut off.55 Several studies also reported mean scores using this measure.48,51,55-57,59,60 The Edinburgh postnatal depression scale does not diagnose postnatal depression (as this can be accomplished only through a psychiatric clinical interview) but rather it is the most commonly used instrument to assess postpartum depressive symptoms.7 Two trials used the self reported hospital anxiety depression scale,50,61 and two studies used a semistructured diagnostic interview (structured clinical interview for DSM-IV).48,49 The timing of the outcome assessment varied considerably between studies, ranging from three61 to 24,48,53,55,57,59,60,62 weeks postpartum; one trial also included a 52 week assessment.62
Methodological quality
Randomisation was often with consecutively numbered, sealed, opaque envelopes.50,53,54,57,58,61,62 Four trials used various forms of computer based randomisation.51,52,55,56 Two trials incorporated a central computerised randomisation service accessed by telephone,59,60 and one trial used a block randomisation procedure using a random numbers table48; one trial was cluster randomised.56 Allocation concealment was unclear in one trial.49 All but two trials48,49 completed a power analysis, and data were analysed with an intention to treat approach. Outcome data were collected by assessors blinded to group allocation48,51,52 or mailed questionnaires; one study did not identify the outcome assessor.49 Five trials had a follow-up attrition rate > 20% at final study assessment.50,55,56,57,59 Follow-up in all these trials included mailed questionnaires. Based on susceptibility to bias (for example, unclear allocation concealment, high levels of exclusions or attrition after randomisation, or unblinded outcome assessment), I excluded six trials as appropriate during the sensitivity analysis for outcomes with high levels of heterogeneity (I2 > 50%).49,50,55-57,59
Quantitative data synthesis
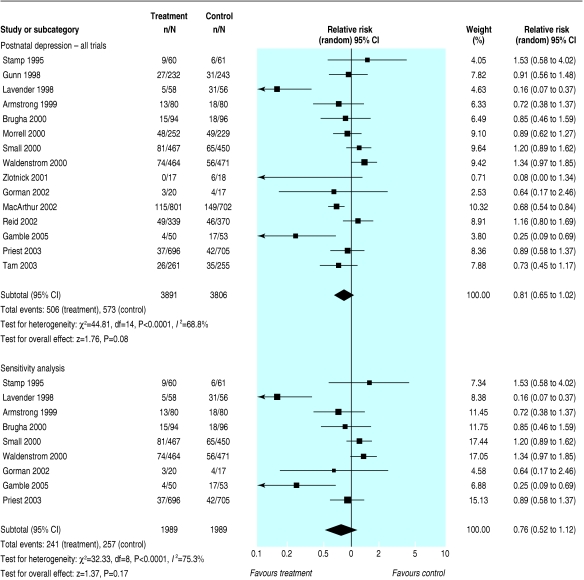
Postnatal depression at last assessment
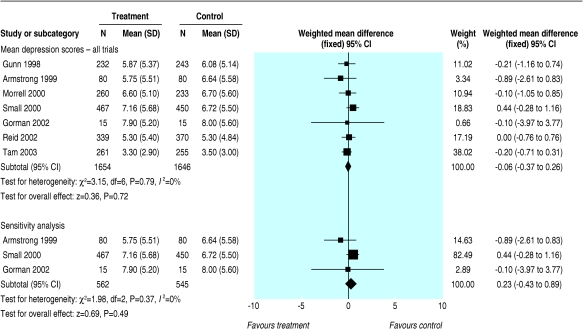
Variously defined—My main outcome measure was postnatal depression at the last study assessment. Although there was no statistically significant beneficial effect on the prevention of postnatal depression in the meta-analysis of all types of interventions (15 trials, n = 7697; relative risk 0.81, 95% confidence interval 0.65 to 1.02) (fig 1), these results suggest a potential 19% reduction in postnatal depression. There was significant heterogeneity among these trials (I2 = 68.8%). The removal of trials at risk of bias, however, resulted in no substantial change to the conclusion. I found a similar non-significant effect when I calculated a weighted mean difference (WMD) among the trials that provided a mean score on the Edinburgh postnatal depression scale (seven trials, n = 3300; WMD -0.06, -0.37 to 0.26) (fig 2).
Fig 1.
Postnatal depression at final assessment (variously defined) among studies evaluating interventions versus normal care in the prevention of postnatal depression
Fig 2.
Mean depression scores at final assessment among studies evaluating interventions versus normal care in the prevention of postnatal depression
Edinburgh postnatal depression score >12—To examine potential measurement differences, I used a random effects model to directly compare trials that used the Edinburgh postnatal depression scale with the recommended 12/13 cut-off score63 and found no preventive effect (10 trials, n = 6126; 0.91, 0.73 to 1.15).
Postnatal depression at 8, 16, and 24 weeks
Variously defined—To assess the short and longer term effects of the preventive interventions, I categorised assessments of postnatal depression at 0-8 weeks postpartum (short term effect); 9-16 weeks (intermediate effect); and 17-24 weeks (longer term effect). Results showed a short term reduction in the development of postnatal depression (eight trials, n = 4091; 0.65, 0.43 to 1.00). The effect weakened at the intermediate period (eight trials, n = 3326; 0.80, 0.56 to 1.12) and disappeared after 16 weeks (seven trials, n = 4314; 1.02, 0.87 to 1.19).
Edinburgh postnatal depression scale score >12—When I included only those trials that used an Edinburgh postnatal depression scale score > 12 as the outcome measure, there were no statistically significant short term (six trials, n = 3452; 0.90, 0.65 to 1.25), intermediate (five trials, n = 2369; 0.72, 0.49 to 1.06), or longer term (six trials, n = 3598; 1.00, 0.84 to 1.19) effects.
Subgroup analyses
Type of intervention—I found no preventive effect with antenatal and postnatal classes (two trials, n = 311; 1.02, 0.61 to 1.72), lay home visits (one trial, n = 481; 0.89, 0.62 to 1.27), and early post-partum follow-up (one trial, n = 475; 0.91, 0.56 to 1.48). I did, however, find a positive trend related to continuity of care (one trial, n = 935; 1.34, 0.97 to 1.85) and a clear beneficial effect with home visits provided by a health professional (two trials, n = 1663; 0.68, 0.55 to 0.84). Among psychological interventions, there was no preventive effect in relation to interpersonal psychotherapy (two trials, n = 72; 0.31, 0.04 to 2.52) but a positive trend in relation to debriefing in hospital (five trials, n = 3051; 0.57, 0.31 to 1.04).
Mode of intervention—Analysis of 11 trials evaluating individually based interventions showed a benefit in preventing postnatal depression at the last study assessment (n = 6642; 0.76, 0.59 to 1.00). When I excluded trials susceptible to bias, the direction of the effect remained the same but the confidence interval widened (seven trials, n = 3667; 0.68, 0.43 to 1.09). Of the four trials that evaluated group based interventions, there was no apparent reduction in depressive symptoms at last study assessment (n = 1055; 1.03, 0.65 to 1.63).
Onset of intervention—Studies in which the intervention began antenatally and continued postnatally failed to reduce the likelihood of women developing postnatal depression (four trials, n = 1283; 1.21, 0.93 to 1.59). However, there was a preventive effect in those trials evaluating a postnatal only intervention (10 trials, n = 6379; 0.76, 0.58 to 0.98).
Effect of sample selected—Trials that selected participants considered to be “at risk” had more success in preventing postnatal depression (seven trials, n = 1162; 0.67, 0.51 to 0.89) than those that enrolled women from the general population (eight trials, n = 6535; 0.87, 0.66 to 1.16).
Discussion
This systematic review of the prevention of postnatal depression shows that there is no clear evidence to recommend the implementation of antenatal and postnatal classes, early postpartum follow-up, continuity of care models, psychological debriefing in hospital, and interpersonal psychotherapy. There is emerging evidence, however, to support the importance of additional professional support provided postnatally. Although one well designed trial suggested that intensive home visits by nurses with at risk mothers was protective during the first six weeks postpartum,51 the benefit was not maintained to 16 weeks. It is noteworthy that the 16 week assessment coincided with a decrease from weekly to monthly visits. Results from a cluster randomised controlled trial showed that flexible, individualised postpartum care by midwives that incorporated assessment tools also had a preventive effect.56 Due to the cluster randomisation process, however, this trial may have been overweighted in the meta-analyses. The effectiveness of postpartum support provided by laypeople remains uncertain.57
The trials can be further classified into different categories depending on the target population: universal interventions are offered to all women, selective interventions are offered to women at increased risk of developing postnatal depression, and indicated interventions are offered to women who have been identified as depressed or probably depressed.64 Though I did not include any trial that evaluated an indicated intervention, the results of a subgroup analysis to examine the effects of universal and selective interventions showed that identifying mothers with risk factors assisted in the prevention of postnatal depression. Currently there is no consistency in the identification of such women, and a review of 16 antenatal screening tools suggests that there is no measure with acceptable predictive validity to accurately identify women who will later develop postnatal depression.65 This may partially explain why interventions with only a postnatal component seem to be more beneficial than interventions that also incorporate an antenatal component. Although I did not examine interaction effects between the five a priori subgroups, the estimates were independent and the sample sizes were large.66
The included trials were of good methodological quality. The reporting of the trials, however, was often not comprehensive, lacking details on the training and qualifications of the intervention providers and descriptions of adherence to the intervention protocol. There was also a failure to present details of the informational element of the interventions and on the background features of the care received by the control groups. While intention to treat analyses were performed, in trials with group sessions compliance was poor.52,53,55
What is already known on this topic
Postnatal depression is a major health issue affecting about 13% of all new mothers
Epidemiological studies and meta-analyses of predictive studies have consistently found that several psychosocial and psychological variables contribute to increased risk
No systematic review has examined the preventive effect of psychosocial and psychological strategies or specific intervention characteristics
What this study adds
This study did not find sufficient evidence that diverse psychosocial or psychological interventions reduce the number of women who develop postnatal depression
Interventions that target at risk women, are individually based, or initiated postnatally are more likely to be beneficial
Interpretation of results
The diversity of preventive interventions and the widely differing study end points should urge some caution in the interpretation of the pooled data. To partially address this issue, I included short, intermediate, and longer term effects where appropriate. Despite this caution and the subgrouping of end points, this review consistently showed that women who received a preventive intervention were statistically overall just as likely to experience postnatal depression as those who received standard care. It is unknown to what extent some of the heterogeneity or non-significant results are related to the measure used to assess postnatal depression. A similar non-significant effect, however, was found among those trials that incorporated the Edinburgh postnatal depression scale.
The long term consequences of postnatal depression suggest preventive approaches are warranted. Translating research on risk factors into predictive screening protocols65 and preventive interventions, however, has met with limited success, as complex interactions of biopsychosocial risk factors with individual variations need to be considered. The results from this review provide physicians and other health professionals with recommendations for future preventive trials. To further investigate postnatal depression as a public health concern, the inclusion of ethnically and socioeconomically diverse women in these research efforts is critical. In addition, all future trials should include an economic analysis of the relative costs and benefits.
I thank L Gorman, R Hagan, and C MacArthur for responding to queries.
Contributions: D Creedy assisted with assessment of trial quality and data entry, J Kavanagh assisted with the search strategy, and E Hodnett provided editorial suggestions.
Funding: None.
Competing interests: None declared.
Ethical approval: Not required.
References
- 1.Affonso DD, De AK, Horowitz JA, Mayberry LJ. An international study exploring levels of postpartum depressive symptomatology. J Psychosom Res >2000;49: 207-16. [DOI] [PubMed] [Google Scholar]
- 2.Oates MR, Cox JL, Neema S, Asten P, Glangeaud-Freudenthal N, Figueiredo B, et al. Postnatal depression across countries and cultures: a qualitative study. Br J Psychiatry Suppl >2004;46: s10-6. [DOI] [PubMed] [Google Scholar]
- 3.O'Hara M, Swain A. Rates and risk of postpartum depression—a meta-analysis. Int Rev Psychiatry >1996;8: 37-54. [Google Scholar]
- 4.Cooper PJ, Murray L. Fortnightly review. Postnatal depression. BMJ >1998;316: 1884-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper PJ, Murray L. Course and recurrence of postnatal depression. Evidence for the specificity of the diagnostic concept. Br J Psychiatry >1995;166: 191-5. [DOI] [PubMed] [Google Scholar]
- 6.Cooper P, Murray L. Prediction, detection, and treatment of postnatal depression. Arch Dis Child >1997;77: 97-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck CT. Predictors of postpartum depression: an update. Nursing Res >2001;50: 275-85. [DOI] [PubMed] [Google Scholar]
- 8.Bernazzani O, Saucier JF, David H, Borgeat F. Psychosocial predictors of depressive symptomatology level in postpartum women. J Affect Disord >1997;46: 39-49. [DOI] [PubMed] [Google Scholar]
- 9.O'Hara MW, Schlechte JA, Lewis DA, Varner MW. Controlled prospective study of postpartum mood disorders: psychological, environmental, and hormonal variables. J Abnorm Psychol >1991;100: 63-73. [DOI] [PubMed] [Google Scholar]
- 10.Gotlib IH, Whiffen VE, Wallace PM, Mount JH. Prospective investigation of postpartum depression: factors involved in onset and recovery. J Abnormal Psychology >1991;100: 122-32. [DOI] [PubMed] [Google Scholar]
- 11.Mills EP, Finchilescu G, Lea SJ. Postnatal depression—an examination of psychosocial factors. S Afr Med J >1995;85: 99-105. [PubMed] [Google Scholar]
- 12.Cooper PJ, Murray L. Postnatal depression. BMJ >1998;316: 1884-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brugha TS, Sharp HM, Cooper SA, Weisender C, Britto D, Shinkwin R, et al. The Leicester 500 project. Social support and the development of postnatal depressive symptoms, a prospective cohort survey. Psychol Med >1998;28: 63-79. [DOI] [PubMed] [Google Scholar]
- 14.Righetti-Veltema M, Conne-Perreard E, Bousquet A, Manzano J. Risk factors and predictive signs of postpartum depression. J Affect Dis >1998;49: 167-80. [DOI] [PubMed] [Google Scholar]
- 15.Dennis CL, Janssen PA, Singer J. Identifying women at-risk for postpartum depression in the immediate postpartum period. Acta Psychiatr Scand >2004;110: 338-46. [DOI] [PubMed] [Google Scholar]
- 16.Dennis CL. Treatment of postpartum depression. 2: a critical review of nonbiological interventions. J Clin Psychiatry >2004;65: 1252-65. [DOI] [PubMed] [Google Scholar]
- 17.Dennis CL. Preventing postpartum depression. I: a review of biological interventions. Can J Psychiatry >2004;49: 467-75. [DOI] [PubMed] [Google Scholar]
- 18.Dennis CL. Preventing postpartum depression. II: A critical review of nonbiological interventions. Can J Psychiatry >2004;49: 526-38. [DOI] [PubMed] [Google Scholar]
- 19.Lumley J, Austin MP, Mitchell C. Intervening to reduce depression after birth: a systematic review of the randomized trials. Int J Technol Assess Health Care >2004;20: 128-44. [DOI] [PubMed] [Google Scholar]
- 20.Dennis CL, Creedy D. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev >2004;(4): CD001134. [DOI] [PubMed]
- 21.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med >2002;21: 1539-58. [DOI] [PubMed] [Google Scholar]
- 22.Chabrol H, Teissedre F, Saint-Jean M, Teisseyre N, Roge B, Mullet E. Prevention and treatment of post-partum depression: a controlled randomized study on women at risk. Psychol Med >2002;32: 1039-47. [DOI] [PubMed] [Google Scholar]
- 23.Elliott SA, Leverton TJ, Sanjack M, Turner H, Cowmeadow P, Hopkins J, et al. Promoting mental health after childbirth: a controlled trial of primary prevention of postnatal depression. Br J Clin Psychol >2000;39: 223-41. [DOI] [PubMed] [Google Scholar]
- 24.Gordon R, Gordon K. Social factors in prevention of postpartum emotional problems. Obstet Gynecol >1960;15: 433-8. [PubMed] [Google Scholar]
- 25.Serwint JR, Wilson MH, Duggan AK, Mellits ED, Baumgardner RA, DeAngelis C. Do postpartum nursery visits by the primary care provider make a difference? Pediatrics >1991;88: 444-9. [PubMed] [Google Scholar]
- 26.Buist A, Westley D, Hill C. Antenatal prevention of postnatal depression. Arch Women's Mental Health >1999;1: 167-73. [Google Scholar]
- 27.Marks MN, Siddle K, Warwick C. Can we prevent postnatal depression? A randomized controlled trial to assess the effect of continuity of midwifery care on rates of postnatal depression in high-risk women. J Matern Fetal Neonatal Med >2003;13: 119-27. [DOI] [PubMed] [Google Scholar]
- 28.Wolman WL, Chalmers BE, Hofmeyr J, Nikodem VC. Postpartum depression and companionship in the clinical birth environment: a randomized, controlled study. Am J Obstet Gynecol >1993;168: 1388-93. [DOI] [PubMed] [Google Scholar]
- 29.Harris B, Oretti R, Lazarus J, Parkes A, John R, Richards C, et al. Randomised trial of thyroxine to prevent postnatal depression in thyroid-antibody-positive women. Br J Psychiatry >2002;180: 327-30. [DOI] [PubMed] [Google Scholar]
- 30.Harrison-Hohner J, Coste S, Dorato V, Curet LB, McCarron D, Hatton D. Prenatal calcium supplementation and postpartum depression: an ancillary study to a randomized trial of calcium for prevention of preeclampsia. Arch Women's Mental Health >2001;3: 141-6. [Google Scholar]
- 31.Hayes BA, Muller R, Bradley BS. Perinatal depression: a randomized controlled trial of an antenatal education intervention for primiparas. Birth >2001;28: 28-35. [DOI] [PubMed] [Google Scholar]
- 32.Heh SS, Fu YY. Effectiveness of informational support in reducing the severity of post-natal depression in Taiwan. J Adv Nurs >2003;42: 30-6. [DOI] [PubMed] [Google Scholar]
- 33.Llorente AM, Jensen CL, Voigt RG, Fraley JK, Berretta MC, Heird WC. Effect of maternal docosahexaenoic acid supplementation on postpartum depression and information processing. Am J Obstet Gynecol >2003;188: 1348-53. [DOI] [PubMed] [Google Scholar]
- 34.Lawrie TA, Hofmeyr GJ, De Jager M, Berk M, Paiker J, Viljoen E. A double-blind randomised placebo controlled trial of postnatal norethisterone enanthate: the effect on postnatal depression and serum hormones. Br J Obstet Gynaecol >1998;105: 1082-90. [DOI] [PubMed] [Google Scholar]
- 35.Okano T, Nagata S, Hasegawa M, Nomura J, Kumar R. Effectiveness of antenatal education about postnatal depression: a comparison of two groups of Japanese mothers. J Mental Health >1998;7: 191-8. [Google Scholar]
- 36.Rees BL. Effect of relaxation with guided imagery on anxiety, depression, and self-esteem in primiparas. J Holistic Nursing >1995;13: 255-67. [DOI] [PubMed] [Google Scholar]
- 37.Sichel DA, Cohen LS, Robertson LM, Ruttenberg A, Rosenbaum JF. Prophylactic estrogen in recurrent postpartum affective disorder. Biol Psychiatry >1995;38: 814-8. [DOI] [PubMed] [Google Scholar]
- 38.Webster J, Linnane J, Roberts J, Starrenburg S, Hinson J, Dibley L. Identify, educate and alert (IDEA) trial: an intervention to reduce postnatal depression. BJOG >2003;110: 842-6. [PubMed] [Google Scholar]
- 39.Wisner KL, Wheeler SB. Prevention of recurrent postpartum major depression. Hospital Community Psychiatry >1994;45: 1191-6. [DOI] [PubMed] [Google Scholar]
- 40.Wisner KL, Perel JM, Peindl KS, Hanusa BH, Findling RL, Rapport D. Prevention of recurrent postpartum depression: a randomized clinical trial. J Clin Psychiatry >2001;62: 82-6. [DOI] [PubMed] [Google Scholar]
- 41.Gordon NP, Walton D, McAdam E, Derman J, Gallitero G, Garrett L. Effects of providing hospital-based doulas in health maintenance organization hospitals. Obstet Gynecol >1999;93: 422-6. [DOI] [PubMed] [Google Scholar]
- 42.Hodnett ED, Lowe NK, Hannah ME, Willan AR, Stevens B, Weston JA, et al. Effectiveness of nurses as providers of birth labor support in North American hospitals: a randomized controlled trial. JAMA >2002;288: 1373-81. [DOI] [PubMed] [Google Scholar]
- 43.Lieu TA, Braveman PA, Escobar GJ, Fischer AF, Jensvold NG, Capra AM. A randomized comparison of home and clinic follow-up visits after early postpartum hospital discharge. Pediatrics >2000;105: 1058-65. [DOI] [PubMed] [Google Scholar]
- 44.Saisto T, Salmela-Aro K, Nurmi JE, Kononen T, Halmesmaki E. A randomized controlled trial of intervention in fear of childbirth. Obstet Gynecol >2001;98: 820-6. [DOI] [PubMed] [Google Scholar]
- 45.Shields N, Reid M, Cheyne H, Holmes A. Impact of midwife-managed care in the postnatal period: an exploration of psychosocial outcomes. J Reprod Infant Psychol >1997;15: 91-108. [Google Scholar]
- 46.Spinelli MG. Interpersonal psychotherapy for depressed antepartum women: a pilot study. Am J Psychiatry >1997;154: 1028-30. [DOI] [PubMed] [Google Scholar]
- 47.Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. Am J Psychiatry >2003;160: 555-62. [DOI] [PubMed] [Google Scholar]
- 48.Gorman LL. Prevention of postpartum depression in a high risk sample. Iowa City, IA: University of Iowa, >2001.
- 49.Zlotnick C, Johnson SL, Miller IW, Pearlstein T, Howard M. Postpartum depression in women receiving public assistance: pilot study of an interpersonal-therapy-oriented group intervention. Am J Psychiatry >2001;158: 638-40. [DOI] [PubMed] [Google Scholar]
- 50.Tam WH, Lee DT, Chiu HF, Ma KC, Lee A, Chung TK. A randomised controlled trial of educational counselling on the management of women who have suffered suboptimal outcomes in pregnancy. BJOG >2003;110: 853-9. [PubMed] [Google Scholar]
- 51.Armstrong KL, Fraser JA, Dadds MR, Morris J. A randomized, controlled trial of nurse home visiting to vulnerable families with newborns. J Paediatr Child Health >1999;35: 237-44. [DOI] [PubMed] [Google Scholar]
- 52.Brugha TS, Wheatley S, Taub NA, Culverwell A, Friedman T, Kirwan P, et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med >2000;30: 1273-81. [DOI] [PubMed] [Google Scholar]
- 53.Stamp GE, Williams AS, Crowther CA. Evaluation of antenatal and postnatal support to overcome postnatal depression: a randomized, controlled trial. Birth >1995;22: 138-43. [DOI] [PubMed] [Google Scholar]
- 54.Gamble J, Creedy D, Moyle W, Webster J, McAllister M, Dickson P. Effectiveness of a counseling intervention after a traumatic childbirth: a randomized controlled trial. Birth >2005;32: 11-9. [DOI] [PubMed] [Google Scholar]
- 55.Reid M, Glazener C, Murray GD, Taylor GS. A two-centred pragmatic randomised controlled trial of two interventions of postnatal support. BJOG >2002;109: 1164-70. [DOI] [PubMed] [Google Scholar]
- 56.MacArthur C, Winter HR, Bick DE, Knowles H, Lilford R, Henderson C, et al. Effects of redesigned community postnatal care on women's health 4 months after birth: a cluster randomised controlled trial. Lancet >2002;359: 378-85. [DOI] [PubMed] [Google Scholar]
- 57.Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A. Costs and effectiveness of community postnatal support workers: randomised controlled trial. BMJ >2000;321: 593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Waldenstrom U, Brown S, McLachlan H, Forster D, Brennecke S. Does team midwife care increase satisfaction with antenatal, intrapartum, and postpartum care? A randomized controlled trial. Birth >2000;27: 156-67. [DOI] [PubMed] [Google Scholar]
- 59.Gunn J, Lumley J, Chondros P, Young D. Does an early postnatal check-up improve maternal health: results from a randomised trial in Australian general practice? BJOG >1998;105: 991-7. [DOI] [PubMed] [Google Scholar]
- 60.Small R, Lumley J, Donohue L, Potter A, Waldenstrom U. Randomised controlled trial of midwife led debriefing to reduce maternal depression after operative childbirth. BMJ >2000;321: 1043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lavender T, Walkinshaw SA. Can midwives reduce postpartum psychological morbidity? A randomized trial. Birth >1998;25: 215-9. [DOI] [PubMed] [Google Scholar]
- 62.Priest SR, Henderson J, Evans SF, Hagan R. Stress debriefing after childbirth: a randomised controlled trial. Med J Aust >2003;178: 542-5. [DOI] [PubMed] [Google Scholar]
- 63.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry >1987;150: 782-6. [DOI] [PubMed] [Google Scholar]
- 64.Mrazek PJ, Haggerty RJ. Reducing risks for metal disorders—frontiers for prevention intervention research. Washington, DC: National Academy Press, >1994. [PubMed]
- 65.Austin M, Lumley J. Antenatal screening for postnatal depression: a systematic review. Acta Psychiatr Scand >2003;107: 10-7. [DOI] [PubMed] [Google Scholar]
- 66.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ >2003;326: 219. [DOI] [PMC free article] [PubMed] [Google Scholar]