Supplemental Digital Content is available in the text
Keywords: accidental falls, multiple sclerosis, wheelchair
Abstract
Falls are a serious health concern for persons with multiple sclerosis (PwMS) who use wheelchairs or scooters as their primary mode of mobility. Unfortunately, little is known about the fall prevalence and characteristics of this large segment of the multiple sclerosis (MS) community. The purpose of this study is to determine the prevalence and circumstances of falls in wheelchair and scooter users living with MS. Forty-four PwMS were recruited from research and medical centers in the United States and Asia. Participants completed a survey focusing on prevalence of falls, frequency of injurious falls, circumstances of the fall, and various quality of life indicators. A total of 44 individuals (32 females/11 males/1 not reported) aged 27 to 82 years (mean = 58 yrs) completed the survey. Seventy-five percent (n = 33) reported falling at least once in 6 months and 48% (n = 12) of those that fell sustained an injury. The majority (87.5%) of the falls occurred inside the home. Most individuals (76.7%; n = 33) reported concerns about falling and 65.9% (n = 29) limited their activities because of their concern of falling. Falls are prevalent in wheelchair and scooter users with MS. The observations highlight the need for interventions targeting this segment of the MS community.
1. Introduction
Multiple sclerosis (MS), a chronic and often disabling neurologic disease, is common among adults both in the United States and worldwide.[1] Approximately 400,000 persons are living with MS in the United States and over 2.5 million worldwide.
The disease process itself involves intermittent bursts of focal inflammation across the central nervous system.[2] The inflammatory process results in the demyelination and transection of axons throughout the central nervous system leading to conduction delays and blockage of action potentials along nerve axons.[2] As a result, muscle weakness, cognitive impairment, sensory disturbances, and a decline in postural control and gait function frequently occurs.[1]
As a result of such impairments, falls are common in persons with MS (PwMS). Approximately 50% of ambulatory PwMS report falling over a 6-month period.[3–6] These falls often result in injuries that require medical attention[4,7,8] that can potentially have dire consequences. For example, hip fractures are 4 times more likely in PwMS compared with age and sex matched peers without MS.[9] Depending on the age and sex of the individual, mortality rates can be very high.[10] Finally, physical and psychological health status (ie, health-related quality of life) reports are substantially lower among PwMS who have experienced at least one fall compared with nonfallers.[5] As a result of falls or even near falls, individuals frequently develop a fear of falling that can lead to activity curtailment, physiological deconditioning, loss of independence, and institutionalization.[11,12]
The adverse physical and psychosocial impact of falls in PwMS has led to a growing amount of research examining predictors (eg, poor balance, gait impairment, cognitive impairment, and so on[4,6,13–15]), consequences (eg, injury, fear of falling, and so on[7,8,11,16]), and prevention strategies.[17] Overall, this work has highlighted that some fall risk factors are modifiable and there is great potential to prevent falls among people with MS using targeted rehabilitation interventions.[18–21]
However, a major limitation of the research on falls and prevention strategies in PwMS is that it has almost exclusively focused on individuals who are ambulatory. Indeed, both the National MS Society's own “Free from Falls” program and the International MS falls prevention research network[22,23] excludes individuals who use a wheelchair or scooter as their primary means of mobility. A potential reason for this exclusion is the general lack of information concerning falls in this segment of the MS community. This dearth of knowledge mirrors the limited data concerning falls in other populations of wheelchair or scooter users.[24] Consequently, the purpose of this investigation was to document the prevalence and associated factors of falls in PwMS who use a wheelchair or scooter as their primary means of mobility and to examine the impact on quality of life. As a result of greater physical impairment, we hypothesize that over 50% of wheelchair and scooter users will report at least 1 fall in a 6-month period.
2. Methods
A sample of convenience of PwMS who utilized a manual or power wheelchair or scooter as their main form of mobility and self-report an inability to ambulate community distances were recruited from Sheba MS Center in Tel-Hashomer, Israel, the University of Illinois at Urbana-Champaign, IL and Shepherd Center in Atlanta, GA between May 2014 and July 2015 to participate in a survey. The participants level of neurological disability was equivalent to a score of 7.0 to 7.5 according to the Kurtzke's Expanded Disability Status Scale (EDSS) scale.[25] The local Institutional Review Boards (IRB) associated with each research center approved the study. Because of the low risk nature of the survey, a waiver of documentation of informed consent was obtained from the associated IRBs. Study participants were recruited via posting of flyers, advertisements placed in MS related periodicals and through face-to-face interactions with research staff. All interested individuals were invited to participate in the survey if they met the following inclusion criteria: 1) able to understand English or Hebrew, 2) 18-years old or older, 3) diagnosis of MS, 4) self report use of a wheelchair or scooter for the majority of their mobility, 5) self-reported inability to ambulate community distances, and 6) able to actively participate in transfers. Of note, individuals who met the above mentioned inclusion criteria and utilized ambulatory aids such as walkers or scooters for short distances in their home were not restricted from study enrollment. Participants were asked to complete either a paper survey or an online survey hosted by the University of Illinois at Urbana-Champaign that required approximately 30 minutes of their time. The paper and online surveys contained the same questions. Before being given access to the survey, participants were required to review the informed consent and indicate they understood the purpose and the risks associated with the study. Participants were also asked questions to determine if they met the inclusion criteria. Participants were not compensated for their time.
2.1. Survey development
The original survey was developed in English by 3 researchers with PhDs in rehabilitation related fields. To the best of our knowledge, there are no validated surveys available to evaluate fall frequency among wheelchair and scooter users with MS. The original survey was developed by author L.R. and critically reviewed by authors D.B and J.S. Changes were integrated into the survey and discussed by authors L.R., D.B., and J.S. until a consensus on the most appropriate questions was reached. Author A.K., a native Hebrew speaker and fluent in English, translated the survey. Please see the appendix for a copy of the survey.
2.2. Survey questions
In addition to basic demographics, study participants were asked a series of questions about their disease process, and frequency and type of mobility device use including, but not limited to, the use of wheelchairs, scooters, walkers, and canes. Participants were then asked specific questions regarding falls, including the number of falls sustained in a period of 6 months, where falls most frequently occurred, if injuries were sustained from falls, concerns about falling and activity limitations associated with concerns about falling. A fall was defined as “unintentionally coming to rest on the ground, floor, or other lower level, excluding intentional changes in position to rest on furniture, walls, or other objects”.[26]
2.3. Additional outcome assessments
Participants were then asked to complete the Fatigue Severity Scale (FSS),[27] Multiple Sclerosis Impact Scale (MSIS),[28] Multiple Sclerosis Neurophysiological Screening Questionnaire (MSNQ),[29] the Spinal Cord Injury-Fall Concerns Scale (SCI-FCS),[30] and the World Health Organization Quality of Life (Brief) (WHO-QOL-BREF) questionnaire.[31] The FSS, MSIS, and the MSNQ have been validated for use among individuals with MS. The WHO-QOL-BREF has been validated for use among wheelchair and scooter users. The SCI-FCS has not been validated among individuals with MS but assesses items frequently performed by wheelchair and scooter users. The SCI-FCS has been previously used to examine concerns about falling among wheelchair and scooter users living with MS.[32] Average SCI-FCS scores of applicable items were calculated as several participants did not perform all items evaluated on the tool. Thus, scores ranged from 1 to 4.
2.4. Statistical analysis
General exploratory analysis was performed using SPSS version 23 (SPSS, Inc., Chicago, IL) to examine the frequencies of falls and related characteristics. Because of the survey nature of the study, missing data occurred. Percentages were calculated based on the total number of participants who responded to a particular question. Differences in scores among quality of life related outcome measures were examined based on reports of a fall during the preceding 6 months. Because of the ordinal nature of the data, nonparametric Mann–Whitney tests were performed. Because of the exploratory nature of the study, no corrections were made for multiple comparisons. Finally, associations between fall frequency and various quality of life related outcomes were examined using Spearman rho correlations because of the ordinal nature of the outcome measures utilized. Partial correlations were also performed to examine the influence of the number of hours of mobility device use per week on the relationship between the number of falls sustained and the quality of life outcome measures.
3. Results
3.1. Participants
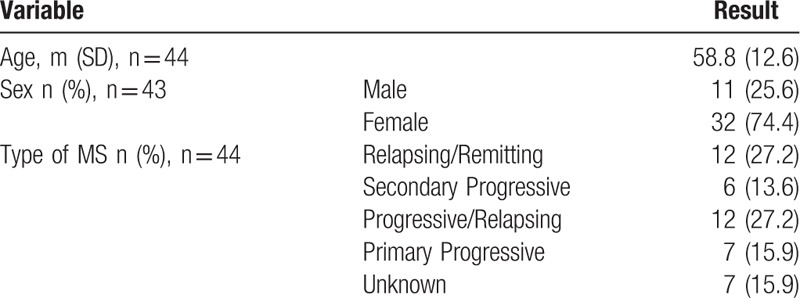
A total of 44 individuals (9 from the University of Illinois at Urbana-Champaign, 7 from Shepherd Center, and 28 from Sheba Medical Center) completed the survey. As shown in Table 1, the sample had a mean age of 58-years old (range: 27–82 yrs) and 74% were female. Relapsing/Remitting (n = 12, 27%) and progressive/relapsing (n = 12, 27%) MS were the most common types of MS reported by participants. Participants reported they used a mobility device for an average of 35.6 hours (SD = 19.3 hrs) per week.
Table 1.
Demographics.
3.2. Fall prevalence
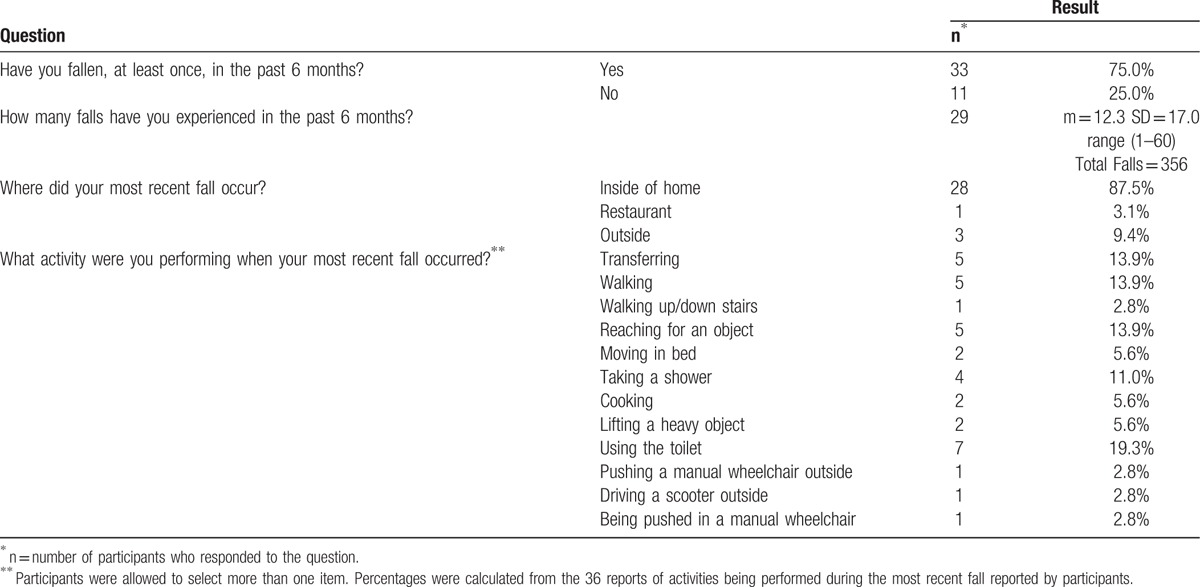
Three-quarters (75%; n = 33) of participants reported falling at least once in the previous 6 months. Among participants who have experienced a fall, an average of 12.3 (SD = 17.0, range 1–60) falls occurred in a 6-month period. The majority (87.5%) of the falls occurred inside the home whereas 9.4% occurred outside. When asked about what activities were being performed during their most recent fall, the top 4 activities reported by participants included: using the toilet (n = 7, 19.4%), transferring (n = 5, 13.9%), walking short distances (n = 5, 13.9%), and reaching for an object (n = 5, 13.9%). (Table 2)
Table 2.
Fall Prevalence, location, and action.
3.3. Consequences of falls
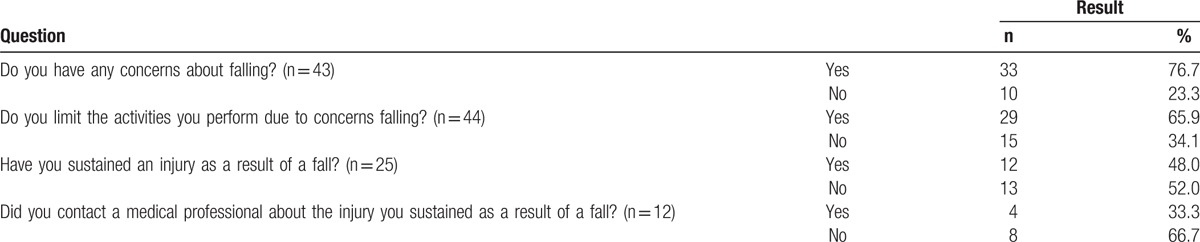
As a result of the falls that occurred, 48% (n = 12) of participants reported they sustained an injury and 4 of these participants (33.3%) reported the injury to a healthcare professional. Most participants (76.7%; n = 33) reported concerns about falling and 65.9% (n = 29) reported that they limited their activities because of their concern of falling. (Table 3) Mann-Whitney tests were performed to examine the differences in SCI-FCS scores among individuals who reported at least one fall in a 6-month period compared with those who reported no falls. No significant differences were found among SCI-FCS scores (P = 0.708, U = 44.50). Individuals who sustained no falls reported median SCI-FCS scores of 2.0 (IQR = 1.44) compared with median scores of 2.59 (IQR = 1.41) among those who sustained at least one fall.
Table 3.
Consequences of falls.
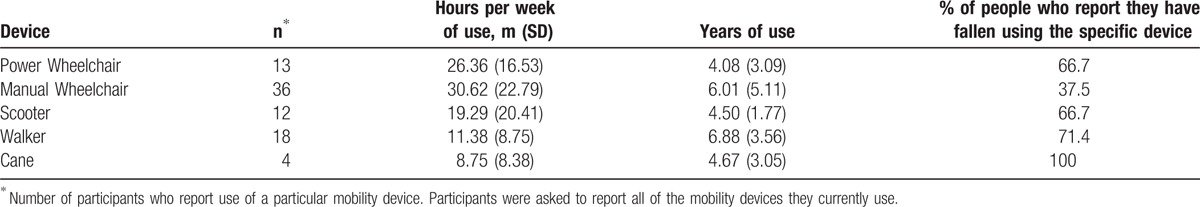
3.4. Mobility device use
A breakdown of falls while using specific devices is presented in Table 4. Because individuals living with MS frequently use a variety of devices, participants were asked to report all of the mobility devices they currently use, how many hours per week they use each device and if they have fallen using each device. The greatest number of participants (n = 36) reported use of a manual wheelchair. Participants also reported using a manual wheelchair most frequently, 30.62 hours per week. When asked if they had fallen using a particular device, 66.7% of PwMS who reported use of a power wheelchair reported falling when using a power wheelchair, 37.5% of manual wheelchair users fell when using a manual wheelchair, 66.7% of scooter users fell when using a scooter, 71.4% of walker users fell when using a walker, and 100% of cane users fell when using a cane. Please see Table 4 for additional information.
Table 4.
Mobility device use.
3.5. Impact on quality of life related measures
Mann-Whitney tests were performed to examine the difference in quality of life related outcome measures among individuals who reported at least one fall in a 6-month period compared with those who reported no falls. No significant differences were found among FSS, MSIS, MSNQ, or the WHO-QOL-BREF scores. (Table 5) Spearman's rho correlations were performed to examine associations between the number of falls in the past 6 months with quality of life indicators. Moderate significant positive correlation was found between the MSNSQ and fall frequency [rs (15) = 0.507, P = .038]. A moderate but nonsignificant negative correlation was found between the Environmental sub-section [rs (8) = –0.578, P = .08) of the WHO-QOL-BREF and fall frequency. Partial Spearman's rho correlations were performed to examine the influence of the number of hours an individual used their most frequent mobility device. This variable was found to have a minimal influence on the variables examined, as shown in Table 6.
Table 5.
Comparison of quality of life variables between fallers and nonfallers.
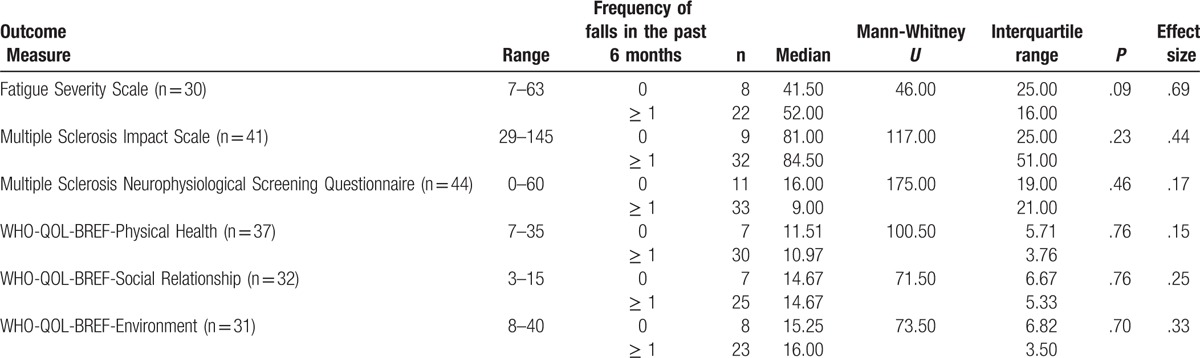
Table 6.
Correlations between number of fall and quality of life variables.

4. Discussion
This article is one of the first to examine the frequency of, consequences, and impact of falls exclusively among PwMS who self-reported use of a wheelchair or scooter as their primary mode of mobility and an inability to ambulate community distances. Results indicate that 75% of participants reported at least one fall in the past 6 months. Almost 50% (n = 12) of participants reported they sustained an injury as a result of a fall. The prevalence of falls observed in this study is higher than most other reports in PwMS. Finlayson et al[6] reported that approximately 50% of their sample reported at least one fall in a 6-month period and Nilsagard et al[33] found that 63% of the sample experienced at least one fall in a 3 month period. It is important to note that these investigations either excluded persons who utilized a wheelchair or scooter or did not report fall prevalence as a function of mobility impairment. In contrast, Matsuda et al[34] reported that between 40% and 70% of nonwalkers with MS indicate that they have fallen in the past 6 months and those over 65 had the highest prevalence of falls. Given that the current sample had a mean age of 58 years, it is possible that the elevated fall prevalence observed here results in part by the complex interaction between age and disability.[11]
4.1. Concerns about falling
Approximately 75% of participants also reported that they were concerned about falling and 65% reported they avoided doing specific activities because of their concerns. Activity avoidance has the potential to lead to social isolation and limitations in community participation. Management of such fears and activity avoidance are important, as PwMS are highly impacted by depression[35] and diminished quality of life.[36] Concerns that further impede active participation must be managed to enhance the quality of life of this substantial segment of the population. Our results are consistent with findings among ambulatory individuals. Peterson et al[37] found that 63.5% of ambulatory middle aged and older adults with MS reported a fear of falling and 82.6% limited their activities.
It is important to note that recent evidence indicates that elevated fear of falling is associated with recurrent falls in ambulatory PwMS.[16] Upon comparison of SCI-FCS scores, we did not find any significant differences between participants who have fallen compared with those who have not fallen. The data indicates that the median scores and IQR were very similar between groups. Consequently, fall management education is necessary for all PwMS who use a wheelchair or scooter, not just those who have previously sustained a fall.
4.2. Falls using specific mobility devices
Upon examination of the occurrence of falls stratified among mobility device use, fall frequency was high when participants reported use of both ambulatory and seated mobility aids. Approximately, 71.4% of participants who reported use of a walker fell when using a walker and 100% of participants who reported using a cane fell when using the cane. Use of multiple mobility devices is common and many PwMS continue to ambulate short distances in their home after being prescribed a wheelchair or scooter. Clinicians must be aware that despite the recommendation of a wheelchair or scooter to manage fall risk, many individuals continue to ambulate and sustain falls.
Falls also occur when using a wheelchair or scooter. 66.7% power wheelchair and scooter users report that they have fallen when using the device and almost 40% of manual wheelchair users report falls. Thus, clinicians must be aware that when an individual transitions to the use of a wheelchair or scooter, the risk of falls continues to be high and preventative interventions are needed.
4.3. Impact on MS related symptoms and quality of life
Results of the current study found minimal associations between fall frequency and MS related symptoms. Results indicate that there was a significant positive correlation between the number of falls experienced and the MSNSQ. The MSNSQ examines cognitive functioning among PwMS, with higher scores indicating greater involvement of cognitive impairments. Such a finding is important for caregivers of PwMS to be aware of and understand that fall risk may be increased as cognition declines. Our research also shows a moderate but nonsignificant association between WHO-QOL-BREF environmental scores and fall frequency indicating that individuals with a higher frequency of falls reported lower quality of life. The environmental subsection of the WHO-QOL-BREF examines a participant's feelings of freedom, physical safety and security, comfort with their environment and their ability to participate in and have opportunities for recreation.[31] These aspects of daily living are extremely important for overall health and wellness and prevention of depressive symptoms. Further research with a longer follow up period is necessary as quality of life is a very complex attribute to examine.[38]
4.4. Clinical application and target of further research
When providing care to PwMS who use a wheelchair or scooter as their primary means of mobility, clinicians must consider the high frequency of falls when designing their treatment protocols and must educate their clients on the high likelihood of falls and associated consequences. Clinicians also need to be aware that even when a wheelchair or scooter is recommended as a method to prevent falls or if a PwMS reports that they use a wheelchair or scooter as their primary means of mobility, PwMS may still continue to use canes or walkers. Our data indicates that a high percentage of falls occur when utilizing these devices. Clinicians must be aware of this occurrence and provide appropriate education.
Consequently, more research is needed on this topic. Limited evidenced based treatment protocols are available for clinicians to review when designing treatment plans to manage fall risk.[24] The majority of MS related rehabilitation research is focused on ambulatory individuals. As a result of differences in functional mobility, strength limitations, and assistive device use between ambulatory and wheelchair/scooter users living with MS, interventions to manage fall risk do not translate between groups. Research specific to this population is essential to provide clinicians with much needed evidenced based treatment protocols. Although our results are preliminary, focusing on the areas where falls most frequently occur is an appropriate starting point. The majority of participants reported that their most recent fall occurred at home (n = 28, 87.5%). Therefore, researchers should be diligent about inquiring and designing interventions to manage common risk factors that participants face in their own homes. As reported by study participants, the most common activity that was being performed during the most recent fall was using the toilet (n = 7, 19.4%). Using the toilet for PwMS who primarily use a wheelchair or scooter often involves a combination of urgency because of bladder dysfunction and challenges to postural control when transferring to the toilet. Among ambulatory individuals with MS, Sung et al[39] found that individuals with severe bladder dysfunction had a higher incidence of falls. Further investigation is needed to determine if bladder dysfunction, challenges to seated postural control, or a combination of the 2 are the reason for the increased incidence of falls when using the toilet. Other common activities reported that were performed during the most recent fall included transfers and reaching for objects which both involves challenges to dynamic balance. Further investigation is necessary to more fully examine the cause and circumstances surrounding falls among wheelchair and scooter users living with MS. Finally, additional research is needed to determine the most appropriate way for individuals with MS to recover after a fall. In a recent survey performed by Bisson et al[40] reports indicate that wheelchair and scooter users with MS are at a high risk for delayed initial recovery after a fall. Thus, clinicians must be aware of the potential for delayed recovery and research must be done to determine the most appropriate actions for individuals with MS to take after a fall.
4.5. Study limitations
There are limitations associated with the current study that should be considered when interpreting the results. The sample size utilized for this study was relatively small (n = 44). We however attempted to gather a wide variety of study participants from different geographic areas to obtain the most diverse population as possible. Limited research has been done to examine fall frequently among this population of individuals with MS, therefore our preliminary results are noteworthy. We also relied on self-reported results regarding inclusion criteria, fall frequency and consequences associated with falls. Participants may have misreported information. The information reported however is able to provide a general insight into the circumstances surrounding falls. Such information is important for clinicians to be aware of and will help guide future research. Finally, we utilized the SCI-FCS to objectively examine concerns about falling. This outcome measure has not been validated among individuals with MS. There are however no validated objective outcome measures currently appropriate for wheelchair and scooter users living with MS and the SCI-FCS evaluates generic activities performed by a wide variety of wheelchair and scooter users, not just those living with Spinal Cord Injury.
5. Conclusion
This article is the first to specifically examine fall frequency among wheelchair and scooter users living with MS. Results indicate that 75% (n = 33) of participants report at least one fall in the past 6 months and experienced an average of 12.3 (SD = 17.0) falls. In addition, 48% (n = 12) of participants reported an injury as a result of a fall. As a result of the high frequency of falls and significant consequences, further research to manage fall frequency is essential and must be a priority among researchers.
Supplementary Material
Footnotes
Abbreviations: EDSS = Expanded Disability Status Scale, FSS = Fatigue Severity Scale, IRB = Institutional Review Board, MS = multiple sclerosis, MSIS = Multiple Sclerosis Impact Scale, MSNQ = Multiple Sclerosis Neurophysiological Screening Questionnaire, PwMS = persons with multiple sclerosis, SCI-FCS = Spinal Cord Injury-Fall Concerns Scale, WHO-QOL-BREF = World Health Organization Quality of Life (Brief).
This study was funded by the Department of Kinesiology and Community Health at the University of Illinois at Urbana-Champaign, Champaign, IL.
The authors declare no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Noseworthy JH, Lucchinetti C, Rodriguez M, et al. Multiple sclerosis. N Engl J Med 2000;343:938–52. [DOI] [PubMed] [Google Scholar]
- [2].Bjartmar C, Trapp BD. Axonal and neuronal degeneration in multiple sclerosis: mechanisms and functional consequences. Curr Opin Neurol 2001;14:271–8. [DOI] [PubMed] [Google Scholar]
- [3].Cattaneo D, De Nuzzo C, Fascia T, et al. Risks of falls in subjects with multiple sclerosis. Arch Phys Med Rehabil 2002;83:864–7. [DOI] [PubMed] [Google Scholar]
- [4].Matsuda PN, Shumway-Cook A, Bamer AM, et al. Falls in multiple sclerosis. PM&R 2011;3:624–32. quiz 632. [DOI] [PubMed] [Google Scholar]
- [5].Coote S, Hogan N, Franklin S. Falls in people with MS who use a walking aid: prevalence, factors, and effect of balance and strengthening interventions. Arch Phys Med Rehabil 2012. [DOI] [PubMed] [Google Scholar]
- [6].Finlayson ML, Peterson EW, Cho CC. Risk factors for falling among people aged 45 to 90 years with multiple sclerosis. Arch Phys Med Rehabil 2006;87:1274–9. quiz 1287. [DOI] [PubMed] [Google Scholar]
- [7].Cameron MH, Poel AJ, Haselkorn JK, et al. Falls requiring medical attention among veterans with multiple sclerosis: a cohort study. J Rehabil Res Dev 2011;48:13–20. [DOI] [PubMed] [Google Scholar]
- [8].Peterson EW, Cho CC, von Koch L, et al. Injurious falls among middle aged and older adults with multiple sclerosis. Arch Phys Med Rehabil 2008;89:1031–7. [DOI] [PubMed] [Google Scholar]
- [9].Bazelier MT, van Staa T, Uitdehaag BM, et al. The risk of fracture in patients with multiple sclerosis: the UK general practice research database. J Bone Miner Res 2011;26:2271–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bliuc D, Nguyen ND, Nguyen TV, et al. Compound risk of high mortality following osteoporotic fracture and refracture in elderly women and men. J Bone Miner Res 2013;28:2317–24. [DOI] [PubMed] [Google Scholar]
- [11].Finlayson ML, Peterson EW. Falls, aging, and disability. Phys Med Rehabil Clin N Am 2010;21:357–73. [DOI] [PubMed] [Google Scholar]
- [12].Matsuda PN, Shumway-Cook A, Ciol MA, et al. Understanding falls in multiple sclerosis: association of mobility status, concerns about falling, and accumulated impairments. Phys Ther 2012;92:407–15. [DOI] [PubMed] [Google Scholar]
- [13].Sosnoff JJ, Socie MJ, Boes MK, et al. Mobility, balance and falls in persons with multiple sclerosis. PloS one 2011;6:e28021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gunn HJ, Newell P, Haas B, et al. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys Ther 2013;93:504–13. [DOI] [PubMed] [Google Scholar]
- [15].Kalron A, Achiron A. Postural control, falls and fear of falling in people with multiple sclerosis without mobility aids. J Neurol Sci 2013;335:186–90. [DOI] [PubMed] [Google Scholar]
- [16].Mazumder R, Lambert WE, Nguyen T, et al. Fear of falling is associated with recurrent falls in people with multiple sclerosis: a longitudinal cohort study. Int J MS Care 2015;17:164–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Sosnoff JJ, Sung J. Reducing falls and improving mobility in multiple sclerosis. Expert Rev Neurother 2015;15:655–66. [DOI] [PubMed] [Google Scholar]
- [18].Cattaneo D, Jonsdottir J, Zocchi M, et al. Effects of balance exercises on people with multiple sclerosis: a pilot study. Clin Rehabil 2007;21:771–81. [DOI] [PubMed] [Google Scholar]
- [19].Finlayson M, Peterson EW, Cho C. Pilot study of a fall risk management program for middle aged and older adults with MS. NeuroRehabilitation 2009;25:107–15. [DOI] [PubMed] [Google Scholar]
- [20].Coote S, Hogan N, Franklin S. Falls in people with multiple sclerosis who use a walking aid: prevalence, factors, and effect of strength and balance interventions. Arch Phys Med Rehabil 2013;94:616–21. [DOI] [PubMed] [Google Scholar]
- [21].Sosnoff JJ, Finlayson M, McAuley E, et al. Home-based exercise program and fall-risk reduction in older adults with multiple sclerosis: phase 1 randomized controlled trial. Clin Rehabil 2013;23:254–63. [DOI] [PubMed] [Google Scholar]
- [22].Sosnoff JJ, Finlayson M. International MS falls prevention research network: report from the front lines. Int J MS Care 2014;16:161–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Cameron M, Coote S, Sosnoff JJ. Whom to target for falls-prevention trials: recommendations from the international MS falls prevention research network. Int J MS Care 2014;16:203–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Rice LA, Ousley C, Sosnoff JJ. A systematic review of risk factors associated with accidental falls, outcome measures and interventions to manage fall risk in nonambulatory adults. Disabil Rehabil 2015;37:1697–705. [DOI] [PubMed] [Google Scholar]
- [25].Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 1983;33:1444–52. [DOI] [PubMed] [Google Scholar]
- [26].Al-Faisal W, Beattie L, Fu H, et al. WHO Global Report on Falls Prevention in Older Age, 2007. [Google Scholar]
- [27].Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 1989;46:1121–3. [DOI] [PubMed] [Google Scholar]
- [28].Hobart J, Lamping D, Fitzpatrick R, et al. The Multiple Sclerosis Impact Scale (MSIS-29): a new patient-based outcome measure. Brain 2001;124(Pt 5):962–73. [DOI] [PubMed] [Google Scholar]
- [29].Benedict RH, Cox D, Thompson LL, et al. Reliable screening for neuropsychological impairment in multiple sclerosis. Mult Scler J 2004;10:675–8. [DOI] [PubMed] [Google Scholar]
- [30].Boswell-Ruys CL, Harvey LA, Delbaere K, et al. A Falls Concern Scale for people with spinal cord injury (SCI-FCS). Spinal Cord 2010;48:704–9. [DOI] [PubMed] [Google Scholar]
- [31].Bonomi AE, Patrick DL, Bushnell DM, et al. Validation of the United States’ version of the World Health Organization Quality of Life (WHOQOL) instrument. J Clin Epidemiol 2000;53:1–2. [DOI] [PubMed] [Google Scholar]
- [32].Rice LA, Issacs Z, Ousley C, et al. Preliminary investigation of an intervention to manage fall risk and enhance functional mobility among wheeled mobility device users with multiple sclerosis. International Journal of MS Care 2017;In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Nilsagard Y, Lundholm C, Denison E, et al. Predicting accidental falls in people with multiple sclerosis: a longitudinal study. Clin Rehabil 2009;23:259–69. [DOI] [PubMed] [Google Scholar]
- [34].Matsuda PN, Verrall AM, Finlayson ML, et al. Falls among adults aging with disability. Arch Phys Med Rehabil 2015;96:464–71. [DOI] [PubMed] [Google Scholar]
- [35].Feinstein A, Magalhaes S, Richard JF, et al. The link between multiple sclerosis and depression. Nat Rev Neurol 2014;10:507–17. [DOI] [PubMed] [Google Scholar]
- [36].Rudick RA, Miller DM. Health-related quality of life in multiple sclerosis: current evidence, measurement and effects of disease severity and treatment. CNS drugs 2008;22:827–39. [DOI] [PubMed] [Google Scholar]
- [37].Peterson EW, Cho CC, Finlayson ML. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler J 2007;13:1168–75. [DOI] [PubMed] [Google Scholar]
- [38].Felce D, Perry J. Quality of life: its definition and measurement. Res Dev Disabil 1995;16:51–74. [DOI] [PubMed] [Google Scholar]
- [39].Sung JH, Motl RW, Sosnoff J. Bladder function and falls in persons with multiple sclerosis. Fourth International Symposium on Gait and Balance in Multiple Sclerosis; 2014. [Google Scholar]
- [40].Bisson EJ, Peterson EW, Finlayson M. Delayed initial recovery and long lie after a fall among middle-aged and older people with multiple sclerosis. Arch Phys Med Rehabil 2015;96:1499–505. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


