Abstract
Sepsis is one of the most important causes of death in intensive care units. Despite the fact that sepsis pathogenesis remains obscure, there is increasing evidence that oxidants and antioxidants play a key role. The imbalance of the abovementioned substances in favor of oxidants is called oxidative stress, and it contributes to sepsis process. The most important consequences are vascular permeability impairment, decreased cardiac performance, and mitochondrial malfunction leading to impaired respiration. Nitric oxide is perhaps the most important and well-studied oxidant. Selenium, vitamin C, and 3N-acetylcysteine among others are potential therapies for the restoration of redox balance in sepsis. Results from recent studies are promising, but there is a need for more human studies in a clinical setting for safety and efficiency evaluation.
1. Introduction
Sepsis is the leading cause of mortality in the intensive care units [1, 2]. Recent publications regarding the definition [3] and management of sepsis [4] underline the keen interest of clinicians. Despite the research, sepsis pathogenesis remains obscure. In the past, the widely accepted theory reported that sepsis was an uncontrolled inflammatory response to a pathogen that was rather a bystander than the real insult [5]. The failure of numerous studies using anti-inflammatory agents questioned the hypothesis of hyperinflammation [6–9].
Therapies focused until recently on macrocirculatory failure such as decreased mean arterial pressure and cardiac output. Immunohistohemical analysis revealed that cell death is minor suggesting that mechanisms other than cell death are responsible for mortality [10]. A growing body of evidence suggests that the inability of the cell to consume oxygen may play a crucial role for sepsis pathogenesis. For example, studies where supranormal oxygen delivery was targeted failed to improve patients' outcomes [11]. Furthermore, in animal studies, mucosal acidosis persisted despite the fact that mucosal perfusion did not change [12]. Since mitochondrial O2 consumption is 90% of the total body consumption, impaired O2 utilization and dysfunctional mitochondria may explain sepsis' specific characteristics. Sepsis is also characterized by excessive production of oxidants. Therefore, they may represent the generator of the abovementioned abnormalities that lead to increased mortality. In this context, redox homeostasis may play a key role, and consequently, therapies targeted to redox abnormalities may be useful for better management of septic patients.
Despite the increasing evidence that oxidative stress is a cornerstone on sepsis pathogenesis, the role of oxidative stress in sepsis may be underestimated. For example, in recent sepsis guidelines, its significance has not been highlighted. In this respect, clinicians may not be aware of the potentially pivotal role of oxidative stress in sepsis evolution. The aim of this literature review article is to point out current aspects about the topic and the evaluation of potential therapies.
2. Oxidants and Antioxidants
Redox reactions represent the basis for numerous biochemical mechanisms imperative for physiological cell function like cell signaling [13, 14]. Oxidants and antioxidants play a key role in the abovementioned mechanisms. The term antioxidant refers to a substance which donates electrons, whereas an oxidant is a substance that accepts electrons [15]. Oxidants are involved in the formation of deoxyribonucleotides, prostaglandin production, oxidation, and carboxylation and hydroxylation reactions that are essential for normal cell function. Free radicals also participate in the host defense against bacterial infections [16], the regulation of vascular tone, and cell adhesion reactions and act as a sensor for oxygen concentration [17]. Important reactive oxygen species (ROS) in sepsis pathogenesis include superoxide (O2−), hydrogen peroxide (H2O2), and hydroxyl radicals (HO). O2− and HO are free radicals since they have unpaired electrons in their molecule. Reactive nitrogen species (RNS) include the free radical nitric oxide (NO) and the nonradical peroxynitrite (ONOO−). There are several procedures involved in the genesis of oxidant molecules in health [18] and sepsis. Cells that represent the innate immune system, like neutrophils and macrophages, are responsible for the oxidative burst that takes place early in sepsis process [19, 20]. The generated ROS and RNS are important for host defense as it was demonstrated by studies with mice deficient to produce O2−, a fact associated with decreased bacterial clearance [21]. The expression of nitric oxide synthase (NOS) is enhanced by lipopolysaccharide (LPS) treatment and nuclear factor kB (NF-kB) activation, and consequently, NO concentration produced by L-arginine is increased. Thereafter, NO can be combined with O2− to form ONOO− [22]. Increased NO levels generate H2O2 in mitochondria by cytochrome c oxidase inhibition [23]. In addition, nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, cyclooxygenase, and electron transfer chain in mitochondria are sources for the increased intracellular O2− [24–26].
For the protection of cellular homeostasis, there are several enzymes or other small molecules that act as oxidant scavengers and comprise the antioxidant defense system. The main antioxidant enzymes are (i) glutathione peroxidase (GPx) which catalyzes the conversion of H2O2 into water, (ii) superoxide dismutase (SOD) which converts O2− to O2 or to the less reactive H2O2, and (iii) catalase (CAT) which also catalyzes the breakdown of H2O2. There are also other low molecular weight substances like ascorbic acid (AA), glutathione (GSH), and α-tocopherol. Among these, GSH is one of the most important redox buffers for the cells, since it can be found in all cell compartments. GSH/GSSG (glutathione disulfide, the oxidized form of GSH) is a good marker of oxidative stress. GSH can act as a cofactor for several enzymes, help in DNA repair, scavenge HO, H2O2, and lipid peroxides, and regenerate other antioxidants such as AA and tocopherols (Table 1).
Table 1.
Summary of antioxidants and their effects.
| Antioxidant | Mechanism of action |
|---|---|
| GPx | H2O2 to H2O |
| SOD | O2− to O2 |
| CAT | H2O2 to H2O and O2 |
| GSH | Antioxidant scavenger, DNA repair, cofactor for enzymes |
| AA | Acts against oxidation of lipids, proteins, and DNA |
| α-Tocopherol | Scavenger for lipid peroxidation products |
GPx: glutathione peroxidase; SOD: superoxide dismutase; CAT: catalase; GSH: glutathione; AA: ascorbic acid.
Under physiological conditions, there is a balance between the formation of oxidant substances and their removal by antioxidant scavenging compounds [27]. Oxidative stress is the imbalance between antioxidant defense and generation of oxidants leading to enhanced oxidant concentration and constitutes a mechanism of injury for many disease processes [28]. The role of oxidative stress in the pathophysiology of several common conditions like diabetes mellitus, chronic heart failure, cancer, and degenerative, neurological, and autoimmune diseases is outside the scope of this review. Oxidative imbalance has been demonstrated in several sepsis studies. Takeda et al., in an early study, found an increased thiobarbituric acid reactive substance level in septic patients suggesting increased lipid peroxidation [29]. Decreased levels of antioxidants were also detected [30].
The clinical significance of oxidative stress in sepsis is demonstrated by several studies. Cowley et al. found that sepsis survivors had greater antioxidant potential than nonsurvivors and also that it was rapidly raised to normal or supranormal levels [31]. In two other prospective observational studies, total antioxidant capacity was correlated with Acute Physiology and Chronic Health Evaluation II (APACHE II) score [32] and the presence of a greater antioxidant deficiency correlated with mortality [33]. This deficiency was strongly indicated by two markers, GSH levels and CAT activity in erythrocytes, and persisted in time. Lower plasma vitamin C levels were detected in patients with multiorgan failure [34]. Harmful mechanisms of increased oxidants level in sepsis include modification of proteins, lipids, and nucleic acids contributing to cellular injury and endothelial dysfunction. In addition, the impairment of glycocalyx and the cellular junctions between endothelial cells lead to increased vascular permeability, a cornerstone of sepsis development [35].
3. NO and Cardiovascular Dysfunction
NO is produced from L-arginine by NOS [36], an enzyme with different isoenzymes (neuronal NOS or nNOS, inducible NOS or iNOS, endothelial NOS or eNOS, and mitochondrial NOS or mtNOS). iNOS produces NO in micromolar range as opposed to the other isoforms that produce NO in nanomolar range [37]. In sepsis, NO can be produced by several cells like activated macrophages, neutrophils, lymphocytes, and others [38–40]. Various molecules such as interferon γ (IFNγ), tumor necrosis factor a (TNFa), and interleukin 1β (IL-1β) involved in the septic inflammatory process are incriminated in the induction of NO production via iNOS hyperactivity. When the cell interacts with one of these molecules, IkB in the cytoplasm is degraded, NF-kB is permitted to move to the nucleus, and therefore expression of iNOS-associated genes is enhanced [41–43].
The effects of NO can be divided into effects on cardiac performance and effects on microcirculation. NO plays a pivotal role in vasodilation and vascular hyporeactivity to vasopressors. There are several studies that indicate this relationship. The injection of LPS in iNOS-deficient mice and the wild type as control provided the evidence that iNOS mediates impairment of vascular contraction [44]. Moreover, the inhibition of NO synthesis reversed shock in dogs induced by bacterial endotoxin [45] and also in septic rats by cecal ligation [46]. NO mediates negative inotropic effects to the cardiac function. LPS treatment of failing myocardium decreased maximum inotropic response to isoprenaline. The depression of cardiac contractility was attributed to enhanced iNOS activity and release [47]. In another study by the same investigators, the negative inotropic effect on human atrial and ventricular myocardium seemed to be mediated via generation of cyclic guanosine monophosphate (cGMP) [48]. On the other hand, other studies revealed that NO has no effect on the myocardium [49] or even that low concentrations of NO are preventive of cardiac performance. In a rodent heart model, coronary flow and ventricular function were reduced by LPS, effects that were partially prevented by supplementation of NO substrate, L-arginine. These improvements were partially blocked by the administration of selective iNOS inhibitors [50]. These data lead to the assumption that NO effects on cardiac performance are concentration dependent.
Other deleterious effects include protein nitrosylation and nitration, convertion of haemoglobin (Hb) to methaemoglobin (MetHb) which leads to red blood cell lysis and thus iron availability to the pathogens, and enhance the production of IL-6 and IL-8 and activation of NF-kB [26, 51] (Table 2).
Table 2.
Summary of NO effects in sepsis.
| Positive effects of NO | |
| Preventive of cardiac contractility in low concentrations | |
| Mitochondrial proliferation | |
| Scavenger of oxygen free radicals | |
| Inhibition of oxygen free radical production | |
| Low pulmonary vascular tone | |
| Negative effects of NO | |
| Vasodilation/hyporeactivity to vasopressors | |
| Negative inotropic effect in high concentrations | |
| Inhibition of mitochondrial respiration | |
| Protein nitration/nitrosylation | |
| Methemoglobinemia | |
| Activation of NF-kB |
NO: nitric oxide; NF-kB: nuclear factor kB.
4. Mitochondria and Apoptosis
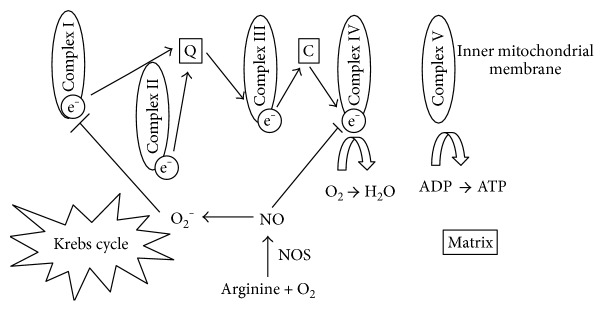
Mitochondria play a key role in redox dysregulation being at the same time sources and targets of oxidants. Oxidative phosphorylation takes place in the inner mitochondrial membrane where electron transport chain lies, consisting of five respiratory complexes (I–V). Electrons are transferred from one to another (I–IV) leading to adenosine triphosphate (ATP) generation in complex V (ATP synthase). Molecular oxygen is the final receptor of the electrons, and thus, an assessment of mitochondrial function can be performed through the measurement of oxygen consumption. The association between mitochondrial dysfunction and sepsis severity is addressed in several studies. In a fundamental one [52], skeletal muscle biopsies on 28 septic patients showed that nonsurvivors had lower ATP concentrations. Furthermore, vasopressor requirements were proportional to NO production as it was gauged by nitrite/nitrate concentrations and inversely correlated to complex I activity. Decreased ATP concentration and mitochondrial activity were also found in other human or animal studies [53, 54]. The pathogenesis of mitochondrial dysfunction is probably complex. NO seems to play a pivotal role by inhibiting the normal function of the respiratory complex IV. By binding to the specific complex, NO interrupts the normal transport of electrons and thus ATP production while at the same time the production of O2− is enhanced. The generated O2− reacts with NO leading to further mitochondrial dysfunction especially by complex I inhibition [55, 56] (Figure 1). The abovementioned mechanisms potentially explain the inability of the cells to utilize oxygen despite the adequate tissue oxygen tension. The term “cytopathic hypoxia” [57] refers to this phenomenon that eventually leads to multiorgan failure and worse outcomes. On the other hand, lower NO concentration seems to promote mitochondrial proliferation suggesting that NO effect on mitochondrial function may be concentration dependent [58].
Figure 1.
The mechanism of cytopathic hypoxia. The production of NO inhibits normal function of the respiratory complex IV interrupting the normal transport of electrons. O₂− production is enhanced and reacts with NO inhibiting complex I normal function. NO, nitric oxide; NOS, nitric oxide synthase; ADP, adenosine diphosphate; ATP, adenosine triphosphate.
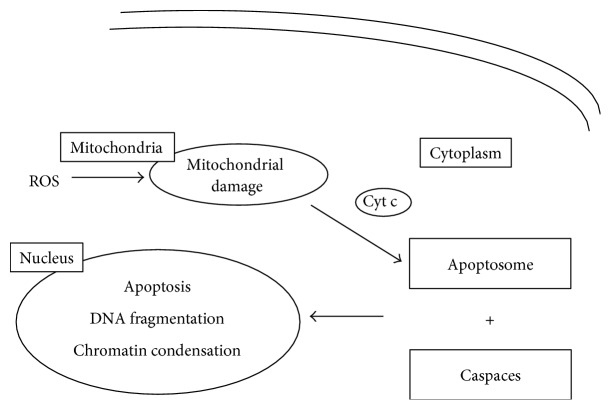
Other potential mechanisms involve protein production and apoptosis. The decreased ATP synthase gene expression and subsequently impaired protein production were demonstrated by the administration of LPS in humans [59]. Apoptosis is the programmed cell death and is involved in sepsis pathogenesis. It can be triggered in a cell through either extrinsic or intrinsic stimuli. Mitochondria play a role in both pathways but especially in the intrinsic one. Mitochondrial damage by ROS can release cytochrome c, the mediator in electron flow between complexes III and IV, to cytosol. The next step is the formation of the “apoptosome” which reacts with caspases initiating the apoptotic pathway via deoxyribonucleic acid (DNA) fragmentation and chromatin condensation [60–63] (Figure 2).
Figure 2.
Mechanism of apoptosis. Mitochondrial damage by ROS releases cytochrome C, which contributes to the formation of apoptosome. The reaction of apoptosome with caspaces initiates cell apoptosis via DNA fragmentation and chromatin condensation. ROS, reactive oxygen species; Cyt C, cytochrome C; DNA, deoxyribonucleic acid.
5. Potential Therapies
The mainstay of sepsis management is source control, antibiotic administration, and haemodynamic support, but the relationship between antioxidant status and sepsis outcomes sets also the rationale for the use of antioxidant substances for the treatment of sepsis. Several molecules and different strategies were used in a plethora of studies in the past years with sometimes conflicting results.
5.1. Selenium
Selenium is essential for the synthesis of antioxidant enzymes, like GPx, and is involved in redox signaling and other immune responses [64]. The rationale for selenium supplementation derives from the correlation between low levels of selenium and disease severity and worse clinical outcomes in critically ill patients [65]. In a single-center clinical trial conducted on 54 septic patients, high-dose selenium administration did not result in reduction of 28-day mortality but increased the activity of GPx. No effect on the level of inflammatory cytokines was noted. However, selenium administration was associated with reduced incidence of ventilator-associated pneumonia (VAP) [66]. Moreover, in a recent multicenter randomized controlled trial (RCT), high-dose intravenous administration of sodium selenite was combined with procalcitonin-guided antimicrobial therapy in order to improve sepsis outcome. Both interventions failed to improve 28-day mortality [67]. In the most recent meta-analysis [68] after the review of 21 RCTs, the investigators concluded that parenteral supplementation of selenium in critically ill patients as a single agent or combined with other antioxidants had no effect on mortality, infections, length of stay, or ventilator days. The only significant effect was the reduction of infections in patients that were nonseptic at the initiation of therapy. In conclusion, even if there is a rationale for selenium administration, clinical trials failed to demonstrate benefits. Further research may reveal new insights in the role of selenium in sepsis pathophysiology.
5.2. Vitamin C
AA is the redox form of vitamin C and acts as a natural antioxidant. Plasma AA in patients with multiorgan failure was significantly lower [34], whereas low concentrations were inversely correlated with increased lipid peroxides [69] a marker of increased oxidative stress. Results from animal models demonstrated that AA ameliorates edema and hypotension and improves arteriolar responsiveness and capillary blood flow [70–73]. Experiments in healthy volunteers after induction of systemic inflammation by low doses of E. coli endotoxemia revealed that the hyporeactivity can be corrected by high doses of vitamin C, suggesting that oxidative stress may represent an important target for inflammation-induced impaired vascular function [74]. In a phase I safety trial of intravenous AA in patients with severe sepsis, infusion was safe and well tolerated [75]. In a retrospective analysis of the combination of hydrocortisone, vitamin C, and thiamine for the treatment of severe sepsis and septic shock, hospital mortality was 8.5% in the treatment group compared to 40.4% in the control group (p < 0.001). The propensity-adjusted odds of mortality in the patients treated with the vitamin C protocol was 0.13 (95% CI 0.04–0.48, p = 0.02). The sequential organ failure assessment score (SOFA score) decreased in all patients in the treatment group with none developing progressive organ failure. The duration of vasopressors was also smaller for the treatment group [76]. The very promising results of this study render the need for prospective randomized trials imperative for the determination of the role of vitamin C in sepsis treatment.
5.3. N-Acetylcysteine (NAC)
GSH is an important molecule recognized not only as an antioxidant but also as a mediator of immune and inflammatory pathways. GSH function is potentially enhanced by the administration of NAC, which has also itself an antioxidant and immunomodulatory activity [77–82]. Studies in humans demonstrated that the administration of NAC can significantly increase hepatosplanchnic blood flow attributed to the increase of cardiac index [83] and can augment neutrophil phagocytosis in patients diagnosed with sepsis, systemic inflammatory response syndrome (SIRS), or multiple trauma [84]. On the other hand, there are studies that demonstrate no influence on outcomes and the level of cytokines [85]. Sometimes, sepsis-induced organ failure was even aggravated [86]. The conflicting results may be due to a limited number of patients. Findings need to be confirmed in larger clinical trials.
5.4. Mitochondria-Targeted Antioxidants
Several strategies were used in order to reduce oxidative stress generated in mitochondria. The ability of lipophilic cations to accumulate in the mitochondria makes them good candidates for clinical studies. MitoQ (ubiquinone attached to a triphenylphosphonium cation) has been shown to protect mammalian cells from hydrogen peroxide-induced apoptosis [87, 88]. In another study, the effects of MitoQ were tested at first in vitro in an endothelial cell model of sepsis and afterwards in vivo in a rat model of sepsis. In vitro, MitoQ decreased oxidative stress and protected mitochondria from damage as indicated by a lower rate of ROS formation and by maintenance of the mitochondrial membrane potential. In vivo, MitoQ treatment resulted in lower levels of biochemical markers of acute liver and renal dysfunction [89]. The hypothesis that the administration of MitoQ would prevent endotoxin-induced reductions in cardiac mitochondrial and contractile function was tested in adult rodents. Endotoxin induced reductions in mitochondrial state 3 respiration rates, the respiratory control ratio, and ATP generation. These effects were ameliorated in the MitoQ-treated animals [90]. There are other substances conjucated to triphenylphosphonium cation as well, like vitamin E (MitoVitE), or ebselen, a selenium-containing compound with peroxidase activity (MitoPeroxidase) [91, 92]. Despite their promising properties, data on human studies are lacking.
Another option is the use of SOD mimetics. SOD mimetic M40401 improved vascular reactivity to vasopressors, reduced cytokine production, and improved mortality in a rat model of septic shock [93]. The ability of another SOD mimetic, the MnIIITE-2-PyP5+, to enter the mitochondria in vivo at levels sufficient to exert its antioxidant action was established by another study in rats [94]. These results encourage the development of SOD mimetics as therapeutic agents for sepsis.
TEMPOL was also used in animal studies with promising results [95, 96], but human studies are lacking. Antiapoptotic properties and ROS scavenging may explain its beneficial action.
5.5. NOS Inhibitors
The crucial role of NO in sepsis development and organ dysfunction led to the implementation of therapeutic strategies capable of reducing NO levels. NOS inhibition can be nonselective or selective for iNOS, which is predominantly synthesized during inflammation. In animal studies, nonselective NOS inhibition improved haemodynamics but increased mortality [97, 98]. The use of nonselective NOS inhibitors in patients with septic shock was terminated early because of increased mortality [99]. The inhibition of eNOS may explain the negative results of the study. The finding that the overexpression of eNOS is beneficial in septic animals [100, 101] led to the hypothesis that it is the excessive NO production by iNOS that is harmful and stimulated a research for selective iNOS inhibitors. Treatment with the selective iNOS inhibitor aminoguanidine inhibited the LPS-induced bacterial translocation by ameliorating intestinal hyperpermeability [102]. The rate of oxygen consumption was significantly restored in endotoxemic rats treated with aminoguanidine as compared with vehicle-treated endotoxemic rats [103]. Furthermore, in a porcine model of bacteremia where selective iNOS blockade was used, sepsis-induced plasma nitrate/nitrite concentrations were inhibited, hypotension was prevented without affecting cardiac output, and progressive deterioration in ileal mucosal microcirculation was blunted without mucosal acidosis [104]. An interesting alternative is ketanserin, a serotonin receptor antagonist. Several studies suggest that the administration of ketanserin is beneficial in septic animals. Mechanisms involved are the restoration of baroflex function [105] and the inhibition of iNOS expression via the MEK/ERK pathway [106]. The administration of ketanserin in septic patients resulted in improved microcirculatory perfusion assessed by direct visualization of the microcirculation with sidestream dark-field imaging [107]. The promising results deserve further evaluation in randomized trials.
5.6. Melatonin
Melatonin is the major hormone secreted by pineal gland predominantly at night. Melatonin has significant anti-inflammatory and antiapoptotic effects, but it can also act as an antioxidant scavenger for radical oxygen and nitrogen species [108, 109]. There are several animal studies depicting these beneficial antioxidant properties of melatonin in LPS or cecal ligation and puncture- (CLP-) induced septic shock [110–112]. Another important finding is the protection of mitochondrial dysfunction. Melatonin administration decreased mitochondrial NOS activity and inhibition of complexes I and IV in LPS-treated rats [113]. Furthermore, the results from another study suggest that melatonin can also prevent mitochondrial damage from the inducible isoform of mitochondrial NOS in septic mice [114]. Finally, it can restore mitochondrial production of ATP [115]. When healthy volunteers received melatonin before the administration of LPS, several markers of inflammation and oxidative stress were reduced [116]. In another study, melatonin treatment in septic newborns resulted in lower concentrations of lipid peroxidation products and other favorable outcomes [117]. In conclusion, melatonin has beneficial effects in sepsis that encourage the development of human studies since relevant data are lacking.
6. Conclusion
Oxidative stress mechanisms in sepsis are highly complicated. ROS and RNS play a pivotal role in sepsis evolution, but their specific role and importance remain obscure. Nevertheless, hyperpermeability, hypotension induced by reduced vascular tone, and mitochondrial impairment of respiration are key elements for multiorgan failure and thus mortality in septic patients. Several therapies were tested in clinical trials. Results are not sufficient for the implementation of these therapies in a clinical setting. An explanation may be that animal models do not completely resemble human sepsis. Further research is needed to answer questions about the underline mechanisms. Nevertheless, the increasing insight may alter our perception in sepsis development and management.
Acknowledgments
The authors are grateful to Lili Mousiou (English literature graduate) for the English language editing of the manuscript.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Vincent J. L., Sakr Y., Sprung C. L., et al. Sepsis in European intensive care units: results of the SOAP study. Critical Care Medicine. 2006;34(2):344–353. doi: 10.1097/01.CCM.0000194725.48928.3A. [DOI] [PubMed] [Google Scholar]
- 2.Angus D. C., Linde-Zwirble W. T., Lidicker J., Clermont G., Carcillo J., Pinsky M. R. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Critical Care Medicine. 2001;29(7):1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Singer M., Deutschman C. S., Seymour C. W., et al. The third international consensus definitions for sepsis and septic shock (sepsis-3) The Journal of the American Medical Association. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rhodes A., Evans L. E., Alhazzani W., et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Medicine. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 5.Thomas L. Germs. The New England Journal of Medicine. 1972;287(11):553–555. doi: 10.1056/NEJM197209142871109. [DOI] [PubMed] [Google Scholar]
- 6.Abraham E., Wunderink R., Silverman H., et al. Efficacy and safety of monoclonal antibody to human tumor necrosis factor alpha in patients with sepsis syndrome. A randomized, controlled, double-blind, multicenter clinical trial. TNF-alpha MAb sepsis study group. The Journal of the American Medical Association. 1995;273(12):934–941. [PubMed] [Google Scholar]
- 7.Sprung C. L., Annane D., Keh D., et al. Hydrocortisone therapy for patients with septic shock. The New England Journal of Medicine. 2008;358(2):111–124. doi: 10.1056/NEJMoa071366. [DOI] [PubMed] [Google Scholar]
- 8.Fisher C. J., Jr., Dhainaut J. F., Opal S. M., et al. Recombinant human interleukin 1 receptor antagonist in the treatment of patients with sepsis syndrome. Results from a randomized, double-blind, placebo-controlled trial. Phase III rhIL-1ra Sepsis Syndrome Study Group. The Journal of the American Medical Association. 1994;271(23):1836–1843. doi: 10.1001/jama.1994.03510470040032. [DOI] [PubMed] [Google Scholar]
- 9.Bone R. C., Fisher C. J., Jr., Clemmer T. P., Slotman G. J., Metz C. A., Balk R. A. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. The New England Journal of Medicine. 1987;317(11):653–658. doi: 10.1056/NEJM198709103171101. [DOI] [PubMed] [Google Scholar]
- 10.Hotchkiss R. S., Swanson P. E., Freeman B. D., et al. Apoptotic cell death in patients with sepsis, shock, and multiple organ dysfunction. Critical Care Medicine. 1999;27(7):1230–1251. doi: 10.1097/00003246-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Gattinoni L., Brazzi L., Pelosi P., et al. A trial of goal-oriented hemodynamic therapy in critically ill patients. The New England Journal of Medicine. 1995;333(16):1025–1032. doi: 10.1056/NEJM199510193331601. [DOI] [PubMed] [Google Scholar]
- 12.VanderMeer T. J., Wang H., Fink M. P. Endotoxemia causes ileal mucosal acidosis in the absence of mucosal hypoxia in a normodynamic porcine model of septic shock. Critical Care Medicine. 1995;23(7):1217–1226. doi: 10.1097/00003246-199907000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Jones D. P. Radical-free biology of oxidative stress. American Journal of Physiology. Cell Physiology. 2008;295(4):C849–C868. doi: 10.1152/ajpcell.00283.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang J., Wang X., Vikash V., et al. ROS and ROS-mediated cellular signaling. Oxidative Medicine and Cellular Longevity. 2016;2016:18. doi: 10.1155/2016/4350965.4350965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kohen R., Nyska A. Oxidation of biological systems: oxidative stress phenomena, antioxidants, redox reactions, and methods for their quantification. Toxicologic Pathology. 2002;30(6):620–650. doi: 10.1080/01926230290166724. [DOI] [PubMed] [Google Scholar]
- 16.Webster N. R., Nunn J. F. Molecular structure of free radicals and their importance in biological reactions. British Journal of Anaesthesia. 1988;60(1):98–108. doi: 10.1093/bja/60.1.98. [DOI] [PubMed] [Google Scholar]
- 17.Droge W. Free radicals in the physiological control of cell function. Physiological Reviews. 2002;82(1):47–95. doi: 10.1152/physrev.00018.2001. [DOI] [PubMed] [Google Scholar]
- 18.Meo S. D., Reed T. T., Venditti P., Victor V. M. Role of ROS and RNS sources in physiological and pathological conditions. Oxidative Medicine and Cellular Longevity. 2016;2016:44. doi: 10.1155/2016/1245049.1245049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chanock S. J., Benna J. e., Smith R. M., Babior B. M. The respiratory burst oxidase. The Journal of Biological Chemistry. 1994;269(40):24519–24522. [PubMed] [Google Scholar]
- 20.Robinson J. M., Badwey J. A. Production of active oxygen species by phagocytic leukocytes. Immunology Series. 1994;60:159–178. [PubMed] [Google Scholar]
- 21.Gao X. P., Standiford T. J., Rahman A., et al. Role of NADPH oxidase in the mechanism of lung neutrophil sequestration and microvessel injury induced by Gram-negative sepsis: studies in p47phox-/- and gp91phox-/- mice. Journal of Immunology. 2002;168(8):3974–3982. doi: 10.4049/jimmunol.168.8.3974. [DOI] [PubMed] [Google Scholar]
- 22.Brown G. C. Regulation of mitochondrial respiration by nitric oxide inhibition of cytochrome c oxidase. Biochimica et Biophysica Acta (BBA) - Bioenergetics. 2001;1504(1):46–57. doi: 10.1016/S0005-2728(00)00238-3. [DOI] [PubMed] [Google Scholar]
- 23.Poderoso J. J., Carreras M. C., Lisdero C., Riobo N., Schopfer F., Boveris A. Nitric oxide inhibits electron transfer and increases superoxide radical production in rat heart mitochondria and submitochondrial particles. Archives of Biochemistry and Biophysics. 1996;328(1):85–92. doi: 10.1006/abbi.1996.0146. [DOI] [PubMed] [Google Scholar]
- 24.Virdis A., Colucci R., Fornai M., et al. Cyclooxygenase-2 inhibition improves vascular endothelial dysfunction in a rat model of endotoxic shock: role of inducible nitric-oxide synthase and oxidative stress. The Journal of Pharmacology and Experimental Therapeutics. 2005;312(3):945–953. doi: 10.1124/jpet.104.077644. [DOI] [PubMed] [Google Scholar]
- 25.Jacobi J., Kristal B., Chezar J., Shaul S. M., Sela S. Exogenous superoxide mediates pro-oxidative, proinflammatory, and procoagulatory changes in primary endothelial cell cultures. Free Radical Biology and Medicine. 2005;39(9):1238–1248. doi: 10.1016/j.freeradbiomed.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 26.Andrades M. E., Morina A., Spasic S., Spasojevic I. Bench-to-bedside review: sepsis - from the redox point of view. Critical Care. 2011;15(5):p. 230. doi: 10.1186/cc10334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gutteridge J. M., Mitchell J. Redox imbalance in the critically ill. British Medical Bulletin. 1999;55(1):49–75. doi: 10.1258/0007142991902295. [DOI] [PubMed] [Google Scholar]
- 28.Poljsak B., Suput D., Milisav I. Achieving the balance between ROS and antioxidants: when to use the synthetic antioxidants. Oxidative Medicine and Cellular Longevity. 2013;2013:11. doi: 10.1155/2013/956792.956792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Takeda K., Shimada Y., Amano M., Sakai T., Okada T., Yoshiya I. Plasma lipid peroxides and alpha-tocopherol in critically ill patients. Critical Care Medicine. 1984;12(11):957–959. doi: 10.1097/00003246-198411000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Goode H. F., Cowley H. C., Walker B. E., Howdle P. D., Webster N. R. Decreased antioxidant status and increased lipid peroxidation in patients with septic shock and secondary organ dysfunction. Critical Care Medicine. 1995;23(4):646–651. doi: 10.1097/00003246-199504000-00011. [DOI] [PubMed] [Google Scholar]
- 31.Cowley H. C., Bacon P. J., Goode H. F., Webster N. R., Jones J. G., Menon D. K. Plasma antioxidant potential in severe sepsis: a comparison of survivors and nonsurvivors. Critical Care Medicine. 1996;24(7):1179–1183. doi: 10.1097/00003246-199607000-00019. [DOI] [PubMed] [Google Scholar]
- 32.Chuang C. C., Shiesh S. C., Chi C. H., et al. Serum total antioxidant capacity reflects severity of illness in patients with severe sepsis. Critical Care. 2006;10(1, article R36) doi: 10.1186/cc4826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karapetsa M., Pitsika M., Goutzourelas N., Stagos D., Tousia Becker A., Zakynthinos E. Oxidative status in ICU patients with septic shock. Food and Chemical Toxicology. 2013;61:106–111. doi: 10.1016/j.fct.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 34.Borrelli E., Roux-Lombard P., Grau G. E., et al. Plasma concentrations of cytokines, their soluble receptors, and antioxidant vitamins can predict the development of multiple organ failure in patients at risk. Critical Care Medicine. 1996;24(3):392–397. doi: 10.1097/00003246-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Rubio-Gayosso I., Platts S. H., Duling B. R. Reactive oxygen species mediate modification of glycocalyx during ischemia-reperfusion injury. American Journal of Physiology. Heart and Circulatory Physiology. 2006;290(6):H2247–H2256. doi: 10.1152/ajpheart.00796.2005. [DOI] [PubMed] [Google Scholar]
- 36.Knowles R. G., Moncada S. Nitric oxide synthases in mammals. The Biochemical Journal. 1994;298(Part 2):249–258. doi: 10.1042/bj2980249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moncada S., Palmer R. M., Higgs E. A. Nitric oxide: physiology, pathophysiology, and pharmacology. Pharmacological Reviews. 1991;43(2):109–142. [PubMed] [Google Scholar]
- 38.Forman H. J., Torres M. Redox signaling in macrophages. Molecular Aspects of Medicine. 2001;22(4-5):189–216. doi: 10.1016/S0098-2997(01)00010-3. [DOI] [PubMed] [Google Scholar]
- 39.Carreras M. C., Pargament G. A., Catz S. D., Poderoso J. J., Boveris A. Kinetics of nitric oxide and hydrogen peroxide production and formation of peroxynitrite during the respiratory burst of human neutrophils. FEBS Letters. 1994;341(1):65–68. doi: 10.1016/0014-5793(94)80241-6. [DOI] [PubMed] [Google Scholar]
- 40.Valdez L. B., Boveris A. Nitric oxide and superoxide radical production by human mononuclear leukocytes. Antioxidants & Redox Signaling. 2001;3(3):505–513. doi: 10.1089/15230860152409130. [DOI] [PubMed] [Google Scholar]
- 41.Xie Q. W., Kashiwabara Y., Nathan C. Role of transcription factor NF-kappa B/Rel in induction of nitric oxide synthase. The Journal of Biological Chemistry. 1994;269(7):4705–4708. [PubMed] [Google Scholar]
- 42.Pantano C., Reynaert N. L., van der Vliet A., Janssen-Heininger Y. M. Redox-sensitive kinases of the nuclear factor-kappaB signaling pathway. Antioxidants & Redox Signaling. 2006;8(9-10):1791–1806. doi: 10.1089/ars.2006.8.1791. [DOI] [PubMed] [Google Scholar]
- 43.Abraham E. Nuclear factor-kappaB and its role in sepsis-associated organ failure. The Journal of Infectious Diseases. 2003;187(Supplement 2):S364–S369. doi: 10.1086/374750. [DOI] [PubMed] [Google Scholar]
- 44.Gunnett C. A., Chu Y., Heistad D. D., Loihl A., Faraci F. M. Vascular effects of LPS in mice deficient in expression of the gene for inducible nitric oxide synthase. The American Journal of Physiology. 1998;275(2) Part 2:H416–H421. doi: 10.1152/ajpheart.1998.275.2.H416. [DOI] [PubMed] [Google Scholar]
- 45.Kilbourn R. G., Jubran A., Gross S. S., et al. Reversal of endotoxin-mediated shock by NG-methyl-L-arginine, an inhibitor of nitric oxide synthesis. Biochemical and Biophysical Research Communications. 1990;172(3):1132–1138. doi: 10.1016/0006-291X(90)91565-A. [DOI] [PubMed] [Google Scholar]
- 46.Hollenberg S. M., Cunnion R. E., Zimmerberg J. Nitric oxide synthase inhibition reverses arteriolar hyporesponsiveness to catecholamines in septic rats. The American Journal of Physiology. 1993;264(2) Part 2:H660–H663. doi: 10.1152/ajpheart.1993.264.2.H660. [DOI] [PubMed] [Google Scholar]
- 47.Flesch M., Kilter H., Cremers B., et al. Effects of endotoxin on human myocardial contractility involvement of nitric oxide and peroxynitrite. Journal of the American College of Cardiology. 1999;33(4):1062–1070. doi: 10.1016/S0735-1097(98)00660-3. [DOI] [PubMed] [Google Scholar]
- 48.Flesch M., Kilter H., Cremers B., et al. Acute effects of nitric oxide and cyclic GMP on human myocardial contractility. The Journal of Pharmacology and Experimental Therapeutics. 1997;281(3):1340–1349. [PubMed] [Google Scholar]
- 49.Toth I., Heard S. O. Nitric oxide does not mediate lipopolysaccharide-induced myocardial depression in guinea pigs. Critical Care Medicine. 1997;25(4):684–688. doi: 10.1097/00003246-199704000-00021. [DOI] [PubMed] [Google Scholar]
- 50.Price S., Mitchell J. A., Anning P. B., Evans T. W. Type II nitric oxide synthase activity is cardio-protective in experimental sepsis. European Journal of Pharmacology. 2003;472(1-2):111–118. doi: 10.1016/S0014-2999(03)01826-0. [DOI] [PubMed] [Google Scholar]
- 51.Vincent J. L., Zhang H., Szabo C., Preiser J. C. Effects of nitric oxide in septic shock. American Journal of Respiratory and Critical Care Medicine. 2000;161(6):1781–1785. doi: 10.1164/ajrccm.161.6.9812004. [DOI] [PubMed] [Google Scholar]
- 52.Brealey D., Brand M., Hargreaves I., et al. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet. 2002;360(9328):219–223. doi: 10.1016/S0140-6736(02)09459-X. [DOI] [PubMed] [Google Scholar]
- 53.Gasparetto A., Corbucci G. G., Candiani A., Gohil K., Edwards R. H. Effect of tissue hypoxia and septic shock on human skeletal muscle mitochondria. Lancet. 1983;2(8365–8366):p. 1486. doi: 10.1016/S0140-6736(83)90823-1. [DOI] [PubMed] [Google Scholar]
- 54.Llesuy S., Evelson P., Gonzalez-Flecha B., et al. Oxidative stress in muscle and liver of rats with septic syndrome. Free Radical Biology and Medicine. 1994;16(4):445–451. doi: 10.1016/0891-5849(94)90121-X. [DOI] [PubMed] [Google Scholar]
- 55.Liaudet L., Soriano F. G., Szabo C. Biology of nitric oxide signaling. Critical Care Medicine. 2000;28(4 Supplement):N37–N52. doi: 10.1097/00003246-200004001-00005. [DOI] [PubMed] [Google Scholar]
- 56.Frost M. T., Wang Q., Moncada S., Singer M. Hypoxia accelerates nitric oxide-dependent inhibition of mitochondrial complex I in activated macrophages. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 2005;288(2):R394–R400. doi: 10.1152/ajpregu.00504.2004. [DOI] [PubMed] [Google Scholar]
- 57.Fink M. P. Bench-to-bedside review: cytopathic hypoxia. Critical Care. 2002;6(6):491–499. doi: 10.1186/cc1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nisoli E., Clementi E., Paolucci C., et al. Mitochondrial biogenesis in mammals: the role of endogenous nitric oxide. Science. 2003;299(5608):896–899. doi: 10.1126/science.1079368. [DOI] [PubMed] [Google Scholar]
- 59.Calvano S. E., Xiao W., Richards D. R., et al. A network-based analysis of systemic inflammation in humans. Nature. 2005;437(7061):1032–1037. doi: 10.1038/nature03985. [DOI] [PubMed] [Google Scholar]
- 60.Murphy M. P. How mitochondria produce reactive oxygen species. The Biochemical Journal. 2009;417(1):1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kapralov A. A., Kurnikov I. V., Vlasova I. I., et al. The hierarchy of structural transitions induced in cytochrome c by anionic phospholipids determines its peroxidase activation and selective peroxidation during apoptosis in cells. Biochemistry. 2007;46(49):14232–14244. doi: 10.1021/bi701237b. [DOI] [PubMed] [Google Scholar]
- 62.Orrenius S., Gogvadze V., Zhivotovsky B. Mitochondrial oxidative stress: implications for cell death. Annual Review of Pharmacology and Toxicology. 2007;47:143–183. doi: 10.1146/annurev.pharmtox.47.120505.105122. [DOI] [PubMed] [Google Scholar]
- 63.Kroemer G., Galluzzi L., Brenner C. Mitochondrial membrane permeabilization in cell death. Physiological Reviews. 2007;87(1):99–163. doi: 10.1152/physrev.00013.2006. [DOI] [PubMed] [Google Scholar]
- 64.Fairweather-Tait S. J., Bao Y., Broadley M. R., et al. Selenium in human health and disease. Antioxidants & Redox Signaling. 2011;14(7):1337–1383. doi: 10.1089/ars.2010.3275. [DOI] [PubMed] [Google Scholar]
- 65.Manzanares W., Biestro A., Galusso F., et al. Serum selenium and glutathione peroxidase-3 activity: biomarkers of systemic inflammation in the critically ill? Intensive Care Medicine. 2009;35(5):882–889. doi: 10.1007/s00134-008-1356-5. [DOI] [PubMed] [Google Scholar]
- 66.Chelkeba L., Ahmadi A., Abdollahi M., et al. The effect of parenteral selenium on outcomes of mechanically ventilated patients following sepsis: a prospective randomized clinical trial. Annals of Intensive Care. 2015;5(1):p. 29. doi: 10.1186/s13613-015-0071-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bloos F., Trips E., Nierhaus A., et al. Effect of sodium selenite administration and procalcitonin-guided therapy on mortality in patients with severe sepsis or septic shock: a randomized clinical trial. JAMA Internal Medicine. 2016;176(9):1266–1276. doi: 10.1001/jamainternmed.2016.2514. [DOI] [PubMed] [Google Scholar]
- 68.Manzanares W., Lemieux M., Elke G., Langlois P. L., Bloos F., Heyland D. K. High-dose intravenous selenium does not improve clinical outcomes in the critically ill: a systematic review and meta-analysis. Critical Care. 2016;20(1):p. 356. doi: 10.1186/s13054-016-1529-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Galley H. F., Howdle P. D., Walker B. E., Webster N. R. The effects of intravenous antioxidants in patients with septic shock. Free Radical Biology and Medicine. 1997;23(5):768–774. doi: 10.1016/S0891-5849(97)00059-2. [DOI] [PubMed] [Google Scholar]
- 70.Tyml K., Li F., Wilson J. X. Delayed ascorbate bolus protects against maldistribution of microvascular blood flow in septic rat skeletal muscle. Critical Care Medicine. 2005;33(8):1823–1828. doi: 10.1097/01.CCM.0000172548.34622.DE. [DOI] [PubMed] [Google Scholar]
- 71.Wu F., Wilson J. X., Tyml K. Ascorbate protects against impaired arteriolar constriction in sepsis by inhibiting inducible nitric oxide synthase expression. Free Radical Biology and Medicine. 2004;37(8):1282–1289. doi: 10.1016/j.freeradbiomed.2004.06.025. [DOI] [PubMed] [Google Scholar]
- 72.Shen K. P., Lo Y. C., Yang R. C., Liu H. W., Chen I. J., Wu B. N. Antioxidant eugenosedin-A protects against lipopolysaccharide-induced hypotension, hyperglycaemia and cytokine immunoreactivity in rats and mice. The Journal of Pharmacy and Pharmacology. 2005;57(1):117–125. doi: 10.1211/0022357055137. [DOI] [PubMed] [Google Scholar]
- 73.Wilson J. X. Mechanism of action of vitamin C in sepsis: ascorbate modulates redox signaling in endothelium. BioFactors. 2009;35(1):5–13. doi: 10.1002/biof.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pleiner J., Mittermayer F., Schaller G., Marsik C., MacAllister R. J., Wolzt M. Inflammation-induced vasoconstrictor hyporeactivity is caused by oxidative stress. Journal of the American College of Cardiology. 2003;42(9):1656–1662. doi: 10.1016/j.jacc.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 75.Fowler A. A., 3rd, Syed A. A., Knowlson S., et al. Phase I safety trial of intravenous ascorbic acid in patients with severe sepsis. Journal of Translational Medicine. 2014;12:p. 32. doi: 10.1186/1479-5876-12-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Marik P. E., Khangoora V., Rivera R., Hooper M. H., Catravas J. Hydrocortisone, vitamin C and thiamine for the treatment of severe sepsis and septic shock: a retrospective before-after study. Chest. 2017;151(6):1229–1238. doi: 10.1016/j.chest.2016.11.036. [DOI] [PubMed] [Google Scholar]
- 77.Meydani S. N., Wu D., Santos M. S., Hayek M. G. Antioxidants and immune response in aged persons: overview of present evidence. The American Journal of Clinical Nutrition. 1995;62(6 Supplement):1462S–1476S. doi: 10.1093/ajcn/62.6.1462S. [DOI] [PubMed] [Google Scholar]
- 78.Aruoma O. I., Halliwell B., Hoey B. M., Butler J. The antioxidant action of N-acetylcysteine: its reaction with hydrogen peroxide, hydroxyl radical, superoxide, and hypochlorous acid. Free Radical Biology and Medicine. 1989;6(6):593–597. doi: 10.1016/0891-5849(89)90066-X. [DOI] [PubMed] [Google Scholar]
- 79.Victor V. M., Guayerbas N., Garrote D., Rio M. D., Fuente M. D. l. Modulation of murine macrophage function by N-acetylcysteine in a model of endotoxic shock. BioFactors. 1999;10(4):347–357. doi: 10.1002/biof.5520100405. [DOI] [PubMed] [Google Scholar]
- 80.Victor V. M., Fuente M. D. l. N-Acetylcysteine improves in vitro the function of macrophages from mice with endotoxin-induced oxidative stress. Free Radical Research. 2002;36(1):33–45. doi: 10.1080/10715760210160. [DOI] [PubMed] [Google Scholar]
- 81.Fuente M. D. l., Victor V. M. Ascorbic acid and N-acetylcysteine improve in vitro the function of lymphocytes from mice with endotoxin-induced oxidative stress. Free Radical Research. 2001;35(1):73–84. doi: 10.1080/10715760100300611. [DOI] [PubMed] [Google Scholar]
- 82.Zhang H., Spapen H., Nguyen D. N., Benlabed M., Buurman W. A., Vincent J. L. Protective effects of N-acetyl-L-cysteine in endotoxemia. The American Journal of Physiology. 1994;266(5) Part 2:H1746–H1754. doi: 10.1152/ajpheart.1994.266.5.H1746. [DOI] [PubMed] [Google Scholar]
- 83.Rank N., Michel C., Haertel C., et al. N-Acetylcysteine increases liver blood flow and improves liver function in septic shock patients: results of a prospective, randomized, double-blind study. Critical Care Medicine. 2000;28(12):3799–3807. doi: 10.1097/00003246-200012000-00006. [DOI] [PubMed] [Google Scholar]
- 84.Heller A. R., Groth G., Heller S. C., et al. N-Acetylcysteine reduces respiratory burst but augments neutrophil phagocytosis in intensive care unit patients. Critical Care Medicine. 2001;29(2):272–276. doi: 10.1097/00003246-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 85.Emet S., Memis D., Pamukcu Z. The influence of N-acetyl-L-cystein infusion on cytokine levels and gastric intramucosal pH during severe sepsis. Critical Care. 2004;8(4):R172–R179. doi: 10.1186/cc2866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Spapen H. D., Diltoer M. W., Nguyen D. N., Hendrickx I., Huyghens L. P. Effects of N-acetylcysteine on microalbuminuria and organ failure in acute severe sepsis: results of a pilot study. Chest. 2005;127(4):1413–1419. doi: 10.1378/chest.127.4.1413. [DOI] [PubMed] [Google Scholar]
- 87.Kelso G. F., Porteous C. M., Coulter C. V., et al. Selective targeting of a redox-active ubiquinone to mitochondria within cells: antioxidant and antiapoptotic properties. The Journal of Biological Chemistry. 2001;276(7):4588–4596. doi: 10.1074/jbc.M009093200. [DOI] [PubMed] [Google Scholar]
- 88.Dhanasekaran A., Kotamraju S., Kalivendi S. V., et al. Supplementation of endothelial cells with mitochondria-targeted antioxidants inhibit peroxide-induced mitochondrial iron uptake, oxidative damage, and apoptosis. The Journal of Biological Chemistry. 2004;279(36):37575–37587. doi: 10.1074/jbc.M404003200. [DOI] [PubMed] [Google Scholar]
- 89.Lowes D. A., Thottakam B. M., Webster N. R., Murphy M. P., Galley H. F. The mitochondria-targeted antioxidant MitoQ protects against organ damage in a lipopolysaccharide-peptidoglycan model of sepsis. Free Radical Biology and Medicine. 2008;45(11):1559–1565. doi: 10.1016/j.freeradbiomed.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 90.Supinski G. S., Murphy M. P., Callahan L. A. MitoQ administration prevents endotoxin-induced cardiac dysfunction. American Journal of Physiology. Regulatory, Integrative and Comparative Physiology. 2009;297(4):R1095–R1102. doi: 10.1152/ajpregu.90902.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Filipovska A., Kelso G. F., Brown S. E., Beer S. M., Smith R. A., Murphy M. P. Synthesis and characterization of a triphenylphosphonium-conjugated peroxidase mimetic. Insights into the interaction of ebselen with mitochondria. The Journal of Biological Chemistry. 2005;280(25):24113–24126. doi: 10.1074/jbc.M501148200. [DOI] [PubMed] [Google Scholar]
- 92.Smith R. A., Porteous C. M., Gane A. M., Murphy M. P. Delivery of bioactive molecules to mitochondria in vivo. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(9):5407–5412. doi: 10.1073/pnas.0931245100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Macarthur H., Couri D. M., Wilken G. H., et al. Modulation of serum cytokine levels by a novel superoxide dismutase mimetic, M40401, in an Escherichia coli model of septic shock: correlation with preserved circulating catecholamines. Critical Care Medicine. 2003;31(1):237–245. doi: 10.1097/00003246-200301000-00037. [DOI] [PubMed] [Google Scholar]
- 94.Spasojevic I., Chen Y., Noel T. J., et al. Mn porphyrin-based superoxide dismutase (SOD) mimic, MnIIITE-2-PyP5+, targets mouse heart mitochondria. Free Radical Biology and Medicine. 2007;42(8):1193–1200. doi: 10.1016/j.freeradbiomed.2007.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Fink M. P., Macias C. A., Xiao J., et al. Hemigramicidin-TEMPO conjugates: novel mitochondria-targeted anti-oxidants. Biochemical Pharmacology. 2007;74(6):801–809. doi: 10.1016/j.bcp.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 96.Macias C. A., Chiao J. W., Xiao J., et al. Treatment with a novel hemigramicidin-TEMPO conjugate prolongs survival in a rat model of lethal hemorrhagic shock. Annals of Surgery. 2007;245(2):305–314. doi: 10.1097/01.sla.0000236626.57752.8e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Teale D. M., Atkinson A. M. L-canavanine restores blood pressure in a rat model of endotoxic shock. European Journal of Pharmacology. 1994;271(1):87–92. doi: 10.1016/0014-2999(94)90268-2. [DOI] [PubMed] [Google Scholar]
- 98.Cobb J. P., Natanson C., Hoffman W. D., et al. N omega-amino-L-arginine, an inhibitor of nitric oxide synthase, raises vascular resistance but increases mortality rates in awake canines challenged with endotoxin. The Journal of Experimental Medicine. 1992;176(4):1175–1182. doi: 10.1084/jem.176.4.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lopez A., Lorente J. A., Steingrub J., et al. Multiple-center, randomized, placebo-controlled, double-blind study of the nitric oxide synthase inhibitor 546C88: effect on survival in patients with septic shock. Critical Care Medicine. 2004;32(1):21–30. doi: 10.1097/01.CCM.0000105581.01815.C6. [DOI] [PubMed] [Google Scholar]
- 100.Yamashita T., Kawashima S., Ohashi Y., et al. Resistance to endotoxin shock in transgenic mice overexpressing endothelial nitric oxide synthase. Circulation. 2000;101(8):931–937. doi: 10.1161/01.CIR.101.8.931. [DOI] [PubMed] [Google Scholar]
- 101.Ichinose F., Buys E. S., Neilan T. G., et al. Cardiomyocyte-specific overexpression of nitric oxide synthase 3 prevents myocardial dysfunction in murine models of septic shock. Circulation Research. 2007;100(1):130–139. doi: 10.1161/01.RES.0000253888.09574.7a. [DOI] [PubMed] [Google Scholar]
- 102.Unno N., Wang H., Menconi M. J., et al. Inhibition of inducible nitric oxide synthase ameliorates endotoxin-induced gut mucosal barrier dysfunction in rats. Gastroenterology. 1997;113(4):1246–1257. doi: 10.1053/gast.1997.v113.pm9322519. [DOI] [PubMed] [Google Scholar]
- 103.King C. J., Tytgat S., Delude R. L., Fink M. P. Ileal mucosal oxygen consumption is decreased in endotoxemic rats but is restored toward normal by treatment with aminoguanidine. Critical Care Medicine. 1999;27(11):2518–2524. doi: 10.1097/00003246-199911000-00032. [DOI] [PubMed] [Google Scholar]
- 104.Matejovic M., Krouzecky A., Martinkova V., et al. Selective inducible nitric oxide synthase inhibition during long-term hyperdynamic porcine bacteremia. Shock. 2004;21(5):458–465. doi: 10.1097/00024382-200405000-00010. [DOI] [PubMed] [Google Scholar]
- 105.Liu C., Zhang G. F., Song S. W., et al. Effects of ketanserin on endotoxic shock and baroreflex function in rodents. The Journal of Infectious Diseases. 2011;204(10):1605–1612. doi: 10.1093/infdis/jir609. [DOI] [PubMed] [Google Scholar]
- 106.Liu C., Zhang X., Zhou J. X., et al. The protective action of ketanserin against lipopolysaccharide-induced shock in mice is mediated by inhibiting inducible NO synthase expression via the MEK/ERK pathway. Free Radical Biology and Medicine. 2013;65:658–666. doi: 10.1016/j.freeradbiomed.2013.07.045. [DOI] [PubMed] [Google Scholar]
- 107.Vellinga N. A., Veenstra G., Scorcella C., et al. Effects of ketanserin on microcirculatory alterations in septic shock: an open-label pilot study. Journal of Critical Care. 2015;30(6):1156–1162. doi: 10.1016/j.jcrc.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 108.Srinivasan V., Mohamed M., Kato H. Melatonin in bacterial and viral infections with focus on sepsis: a review. Recent Patents Endocrine Metabolic Immune Drug Discovery. 2012;6(1):30–39. doi: 10.2174/187221412799015317. [DOI] [PubMed] [Google Scholar]
- 109.Srinivasan V., Pandi-Perumal S. R., Spence D. W., Kato H., Cardinali D. P. Melatonin in septic shock: some recent concepts. Journal of Critical Care. 2010;25(4):656.e1–656.e6. doi: 10.1016/j.jcrc.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 110.Carrillo-Vico A., Lardone P. J., Naji L., et al. Beneficial pleiotropic actions of melatonin in an experimental model of septic shock in mice: regulation of pro-/anti-inflammatory cytokine network, protection against oxidative damage and anti-apoptotic effects. Journal of Pineal Research. 2005;39(4):400–408. doi: 10.1111/j.1600-079X.2005.00265.x. [DOI] [PubMed] [Google Scholar]
- 111.Wu J. Y., Tsou M. Y., Chen T. H., Chen S. J., Tsao C. M., Wu C. C. Therapeutic effects of melatonin on peritonitis-induced septic shock with multiple organ dysfunction syndrome in rats. Journal of Pineal Research. 2008;45(1):106–116. doi: 10.1111/j.1600-079X.2008.00567.x. [DOI] [PubMed] [Google Scholar]
- 112.Sewerynek E., Melchiorri D., Reiter R. J., Ortiz G. G., Lewinski A. Lipopolysaccharide-induced hepatotoxicity is inhibited by the antioxidant melatonin. European Journal of Pharmacology. 1995;293(4):327–334. doi: 10.1016/0926-6917(95)90052-7. [DOI] [PubMed] [Google Scholar]
- 113.Escames G., Leon J., Macias M., Khaldy H., Acuna-Castroviejo D. Melatonin counteracts lipopolysaccharide-induced expression and activity of mitochondrial nitric oxide synthase in rats. The FASEB Journal. 2003;17(8):932–934. doi: 10.1096/fj.02-0692fje. [DOI] [PubMed] [Google Scholar]
- 114.Escames G., Lopez L. C., Tapias V., et al. Melatonin counteracts inducible mitochondrial nitric oxide synthase-dependent mitochondrial dysfunction in skeletal muscle of septic mice. Journal of Pineal Research. 2006;40(1):71–78. doi: 10.1111/j.1600-079X.2005.00281.x. [DOI] [PubMed] [Google Scholar]
- 115.Lopez L. C., Escames G., Ortiz F., Ros E., Acuna-Castroviejo D. Melatonin restores the mitochondrial production of ATP in septic mice. Neuro Endocrinology Letters. 2006;27(5):623–630. [PubMed] [Google Scholar]
- 116.Alamili M., Bendtzen K., Lykkesfeldt J., Rosenberg J., Gogenur I. Melatonin suppresses markers of inflammation and oxidative damage in a human daytime endotoxemia model. Journal of Critical Care. 2014;29(1):184.e9–184.e13. doi: 10.1016/j.jcrc.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 117.Gitto E., Karbownik M., Reiter R. J., et al. Effects of melatonin treatment in septic newborns. Pediatric Research. 2001;50(6):756–760. doi: 10.1203/00006450-200112000-00021. [DOI] [PubMed] [Google Scholar]